Key Points
-
Marijuana (cannabis) is the most commonly abused illicit psychoactive drug.
-
In one recent study, about 50% of dental students in the UK had used illicit drugs, including marijuana.
-
Medical uses of marijuana include symptomatic relief of chronic pain, multiple sclerosis and depression, arthritis and neuropathy.
-
An oromucosal spray has been developed from the major components of cannabis designed to relieve pain especially in multiple sclerosis.
-
Oral stinging and white lesions may result from using the spray.
Abstract
Background An oromucosal spray has been developed from the major components of marijuana (cannabis), including tetrahydrocannabinol (THC) and cannabidiol (CBD), in alcohol with a peppermint flavouring, designed to be administered as a spray under the tongue or on the buccal mucosa to relieve pain in multiple sclerosis. Although the available evidence indicates its efficacy in this respect, some patients develop oral burning sensation, stinging or white lesions, probably burns.
Objective To investigate the oral side-effects of oromucosal cannabis spray in multiple sclerosis (MS) patients.
Design A small open observational study.
Subjects and methods A series of nine patients with MS who had been using a marijuana oromucosal spray for at least four weeks, were asked to attend for oral examination. Patients were asked whether they had ever experienced symptoms (dryness; bad taste; stinging) associated with use of the spray. A standard oral examination was carried out using a dental light, and the presence of any mucosal lesions recorded. Where mucosal lesions were present, patients were advised to discontinue the spray and re-attend after four weeks for re-examination. For ethical reasons, biopsies were not undertaken at the first visit.
Results Of nine patients invited to participate, eight attended. All admitted to a stinging sensation on using the oromucosal cannabis spray, and four had visible oral mucosal white lesions in the floor of the mouth.
Conclusions Although the white lesions observed were almost certainly burns, resolving or improving on discontinuation of use of the medication, the high alcohol concentration of the oromucosal cannabis spray raises concern in relation to chronic oral use.
Similar content being viewed by others
Introduction
Marijuana (cannabis) is the most commonly abused illicit psychoactive drug. The real extent of marijuana use is unclear but, for example, even about 50% of dental students in the UK in one recent study had used illicit drugs, including marijuana.1
Derived from Cannabis sativa or Cannabis indica, the main active chemical of this recreational drug is THC (delta-9-tetrahydrocannabinol), which binds to central nervous system (CNS) receptors, influencing pleasure, memory, thought, concentration, sensory and time perception, and coordinated movement.
Medical use of marijuana in UK and other countries has reported benefits especially in management of chronic pain, multiple sclerosis and depression, arthritis and neuropathy.2,3 In the USA, 36 states and the District of Columbia have had statutes that address the issue within the past 26 years, but several of those states have either repealed the laws or allowed them to sunset and, since 1996, 11 states have enacted laws that allow individuals to use marijuana with a physician's consent,4 though the Federal Government still maintains strict prohibitions. However, the US Supreme Court has considered sympathetically, cases involving people who smoke marijuana to alleviate their illnesses.
In 1971 the World Health Organization (WHO) pronounced cannabis medically useless and its use was regulated in many countries including the UK. However, the UK law appears to be relaxing and a Select Committee of the House of Lords subsequently argued that more research was necessary, in view of anecdotal reports of the efficacy of cannabis in controlling pain and tremor, particularly in multiple sclerosis (MS).
There are three main forms of cannabis: marijuana, hash and hash oil, all of which contain the main psychoactive constituent THC. Marijuana is most commonly smoked, but it can be added to foods. Recently, a mouth spray has been developed from the major components of marijuana, including THC and cannabidiol (CBD), in alcohol with a peppermint flavour (Sativex® oromucosal spray, GW Pharmaceuticals, UK). This is designed to be administered as a spray under the tongue or on the buccal mucosa. Canada became, in April 2005, the first country to approve this oromucosal spray, a move that could shift the medical marijuana debate in the US and elsewhere. The drug is available in Canadian pharmacies, principally for the treatment of pain from MS, marketed by Germany's Bayer HealthCareAG.
The drug has had no licence for use in the UK, and a licence was refused by the Medicines and Healthcare Products Regulatory Agency (MHRA), but the UK Home Office Minister has agreed to its use in special circumstances. Sativex® thus remains a controlled drug in line with stated government policy, but can be obtained from doctors who have a Home Office license. These physicians can prescribe it on a named patient basis, the system available for the use of unlicensed medicines: in accordance with the Medicines Act, a medicine which has yet to be licensed in the UK may be prescribed and supplied in response to an unsolicited request to fulfil the special needs of an individual patient under a physician's direct personal responsibility.
The oromucosal marijuana spray appeared, in a UK randomised controlled trial, to be effective in reducing central neuropathic pain and sleep disturbance in MS.5 The drug was significantly superior to placebo in reducing the mean intensity of pain and sleep disturbance, and was generally well tolerated, although more patients than those using placebo reported dizziness, dry mouth, and somnolence.5 The oromucosal marijuana spray has also been used in rheumatoid arthritis, when a significant analgesic effect was observed and disease activity was significantly suppressed.6,7 At least five randomised controlled trials have now confirmed its efficacy in a range of conditions.8,9,10
We encountered a chair-bound patient with MS requiring restorative dental care who, on examination, had evidence of symptomless white lesions in the floor of mouth/ventrum of tongue, with no obvious causal factors, apart from use of the cannabis oromucosal spray. We thus undertook an open observational study of a small series of such patients.
Patients and methods
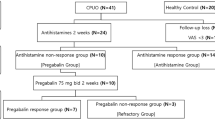
A small open observational study was conducted on a series of nine patients with multiple sclerosis (MS) using a marijuana oromucosal spray as part of a UK trial on its efficacy in MS pain, which had local Ethics Committee approval. None of the patients were using topical oral medicaments apart from dentifrices.
The oromucosal spray (Sativex® oromucosal spray, GW Pharmaceuticals, UK) delivers 2.7 mg of THC and 2.5 mg of CBD, and patients gradually self-titrate to a recommended maximum of 48 sprays in 24 hours. The spray contains approximately 50% v/v alcohol, in a propylene glycol base, and each 100 μl actuation contains up to 0.04 g alcohol.
Patients, all of whom had been using the spray for at least four weeks, were asked to attend for oral examination. Patients were asked whether they had ever experienced symptoms (dryness; bad taste; stinging) associated with use of the spray. A standard oral examination was carried out using a dental light, and the presence of any mucosal lesions recorded. Where mucosal lesions were present, the patient was advised to discontinue the spray and re-attend after four weeks for re-examination. For ethical reasons, biopsies were not undertaken at the first visit.
Results
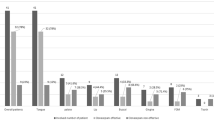
The results are shown in Table 1. Of nine patients invited to participate, eight attended (five female). All admitted to a stinging sensation on using the oromucosal cannabis spray, but none complained of dryness or bad taste and only four had oral mucosal white lesions in the floor of mouth. The lesions in three were clinically very obvious (Fig. 1), but in one were equivocal. The lesions were soft white homogeneous lesions which did not remove with gauze, clinically resembling a sublingual keratosis or a burn. All lesions visibly resolved or decreased by a second visit. Biopsies were therefore not undertaken.
Discussion
The oromucosal spray developed from the major components of marijuana, including tetrahydrocannabinol (THC) and cannabidiol (CBD), in alcohol with a peppermint flavouring, is designed to be administered as a spray under the tongue or on the buccal mucosa to relieve pain in multiple sclerosis. Although the available evidence indicates its efficacy in this respect, some patients develop a sensation of dry mouth5 or a bad taste8 but also – as shown here – stinging and/or mucosal white lesions, probably burns, in a minority. Dry mouth is also a consequence of cannabis and cannabinoids used in other forms.11 Four of eight patients developed oral white lesions which resolved on cessation of spray use, suggesting they were chemical burns. The high alcohol concentration raises concern in relation to chronic oral use and it would therefore be wise to warn against continued spraying on to sore or damaged mucosa, advise that regular oral inspection is mandatory in chronic users and to move to formulation with non-alcohol solutions, despite the lack of evidence implicating alcohol-containing mouthwashes in oral cancer.12
Marijuana in other forms, by comparison with other 'recreational' drugs, could be rated to be a relatively safe drug13 but can have adverse effects.14 THC from cannabis enters the bloodstream and exerts its effects on the body via interaction with endogenous receptors. On the CNS, adverse effects can include depression, anxiety and personality disturbances. Marijuana can impair memory and learning, distort perception, cause difficulty in thinking and problem solving and impair coordination, and may trigger psychoses – development of which is often delayed, almost 50% of patients receiving a diagnosis more than a year after seeking treatment for a cannabis-induced psychosis.15 Marijuana can also have systemic effects, affecting blood pressure and heart rate and lowering the oxygen-carrying capacity of blood: the risk of myocardial infarction may more than quadruple in the first hour after using it. Babies born to women who used marijuana during pregnancies displayed abnormal responses to visual stimuli, tremulousness and a high-pitched cry.
Smoking marijuana frequently leads to respiratory illnesses such as infections, daily cough and sputum production, and obstructed airways. There have been case reports of upper respiratory tract cancers in young adults who smoke cannabis, but evidence from the few epidemiological cohort studies and case-control studies is inconsistent.16 Patients using marijuana may develop oral leukoplakia,17 although tobacco use may contribute to this, and there was concern from some case reports that cannabis use may predispose to oral cancer,18,19 though a large population-based study in USA has essentially discounted this.20 Cannabis smoke may be less carcinogenic than that from tobacco.21
Cannabis abusers also generally have poorer oral health than non-users, have xerostomia, with an increased risk of dental caries and periodontal diseases, and may be prone to oral infections, possibly aggravated by an immunosuppressive effect22,23 (Table 2). Dental treatment of patients using cannabis can result in acute anxiety, dysphoria and paranoiac thoughts, and epinephrine-containing local analgesics may prolong the tachycardia induced by cannabis.24,25
The oromucosal spray developed from marijuana (cannabis) may relieve pain in some chronic diseases, but some patients develop an oral burning sensation, stinging or white lesions, probably burns. Dryness and bad taste have also been recorded. Patients should therefore be sensitised to these effects in relation to chronic oral use. Although the lesions in this study were almost certainly burns due to the alcohol, resolving or improving on discontinuation of use of the medication, the high alcohol concentration used orally raises concern in relation to chronic use, as alcohol may itself have carcinogenic potential, since alcohol may be metabolised by the oral flora to acetaldehyde.26 It is possible that some other constituent such as peppermint (piperitone) might contribute, but the only published report on the oral adverse effects of this was related to orofacial granulomatosis.27
Orofacial lesions are common in people who use psychoactive substances28 and may be seen in topical marijuana use.
References
Newbury-Birch D, Lowry R J, Kamali F . The changing patterns of drinking, illicit drug use, stress, anxiety and depression in dental students in a UK dental school: a longitudinal study. Br Dent J 2002; 192: 646–649.
Gorter R W, Butorac M, Cobian E P, van der Sluis W. Medical use of cannabis in the Netherlands. Neurology 2005; 64: 917–919.
Ware M A, Adams H, Guy G W . The medicinal use of cannabis in the UK: results of a nationwide survey. Int J Clin Pract 2005; 59: 291–295.
Varma P . Public health issue brief: medical marijuana: year end report-2004. Issue Brief Health Policy Track Serv 2004; 31: 1–9.
Rog D J, Nurmikko T J, Friede T, Young C A . Randomized, controlled trial of cannabis-based medicine in central pain in multiple sclerosis. Neurology 2005; 65: 812–819.
Blake D R, Robson P, Ho M, Jubb R W, McCabe C S . Preliminary assessment of the efficacy, tolerability and safety of a cannabis-based medicine (Sativex) in the treatment of pain caused by rheumatoid arthritis. Rheumatology (Oxford) 2005; 45: 50–52.
Wright S, Ware M, Guy G . The use of a cannabis-based medicine (Sativex) in the treatment of pain caused by rheumatoid arthritis. Rheumatology (Oxford) 2006; 45: 781.
Perras C . Sativex for the management of multiple sclerosis symptoms. Issues Emerg Health Technol 2005; 72: 1–4.
Perez J . Combined cannabinoid therapy via an oromucosal spray. Drugs Today (Barc) 2006; 42: 495–503.
Barnes M P . Sativex: clinical efficacy and tolerability in the treatment of symptoms of multiple sclerosis and neuropathic pain. Expert Opin Pharmacother 2006; 7: 607–615.
Berlach D M, Shir Y, Ware M A . Experience with the synthetic cannabinoid nabilone in chronic noncancer pain. Pain Med 2006; 7: 25–29.
Cole P, Rodu B, Mathisen A . Alcohol-containing mouthwash and oropharyngeal cancer: a review of the epidemiology. J Am Dent Assoc 2003; 134: 1079–1087.
Iversen L . Long-term effects of exposure to cannabis. Curr Opin Pharmacol 2005; 5: 69–72.
Kalant H . Adverse effects of cannabis on health: an update of the literature since 1996. Prog Neuropsychopharmacol Biol Psychiatry 2004; 28: 849–863.
Arendt M, Rosenberg R, Foldager L, Perto G, Munk-Jorgensen P. Cannabis-induced psychosis and subsequent schizophrenia-spectrum disorders: follow-up study of 535 incident cases. Br J Psychiatry 2005; 187: 510–515.
Hall W, Christie M, Currow D . Cannabinoids and cancer: causation, remediation, and palliation. Lancet Oncol 2005; 6: 35–42.
Darling M R, Arendorf T M . Review of the effects of cannabis smoking on oral health. Int Dent J 1992; 42: 19–22.
Donald P J . Marijuana smoking – possible cause of head and neck carcinoma in young patients. Otolaryngol Head Neck Surg 1986; 94: 517–521.
Firth NA . Marijuana use and oral cancer: a review. Oral Oncol 1997; 33: 398–401.
Rosenblatt K A, Daling J R, Chen C, Sherman K J, Schwartz S M . Marijuana use and risk of oral squamous cell carcinoma. Cancer Res 2004; 64: 4049–4054.
Melamede R . Cannabis and tobacco smoke are not equally carcinogenic. Harm Reduct J 2005; 2: 21.
Cho C M, Hirsch R, Johnstone S . General and oral health implications of cannabis use. Aust Dent J 2005; 50: 70–74.
Darling M R, Arendorf T M . Effects of cannabis smoking on oral soft tissues. Community Dent Oral Epidemiol 1993; 21: 78–81.
Gregg J M, Campbell R L, Levin K J, Ghia J, Elliott R A . Cardiovascular effects of cannabinol during oral surgery. Anesth Analg 1976; 55: 203–213.
Horowitz L G, Nersasian R R . A review of marijuana in relation to stress-response mechanisms in the dental patient. J Am Dent Assoc 1978; 96: 983–986.
Pikkarainen P H, Baraona E, Jauhonen P, Seitz H K, Lieber C S . Contribution of oropharynx microflora and of lung microsomes to acetaldehyde in expired air after alcohol ingestion. J Lab Clin Med 1981; 97: 631–636.
Patton D W, Ferguson M M, Forsyth A, James J . Oro-facial granulomatosis: a possible allergic basis. Br J Oral Maxillofac Surg 1985; 23: 235–242.
Thavarajah R, Rao A, Raman U, Rajasekaran S T, Joshua E R H, Kannan R . Oral lesions of 500 habitual psychoactive substance users in Chennai, India. Arch Oral Biol 2006; 51: 512–519.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Scully, C. Cannabis; adverse effects from an oromucosal spray. Br Dent J 203, E12 (2007). https://doi.org/10.1038/bdj.2007.749
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bdj.2007.749