Abstract
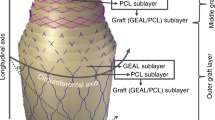
Surgical treatment of vascular disease has become common, creating the need for a readily available, small-diameter vascular graft. However, the use of synthetic materials is limited to grafts larger than 5–6 mm because of the frequency of occlusion observed with smaller-diameter prosthetics. An alternative to synthetic materials would be a biomaterial that could be used in the design of a tissue-engineered graft. We demonstrate that a small-diameter (4 mm) graft constructed from a collagen biomaterial derived from the submucosa of the small intestine and type I bovine collagen has the potential to integrate into the host tissue and provide a scaffold for remodeling into a functional blood vessel. The results obtained using a rabbit arterial bypass model have shown excellent hemostasis and patency. Furthermore, within three months after implantation, the collagen grafts were remodeled into cellularized vessels that exhibited physiological activity in response to vasoactive agents.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Report of a working party of the British Cardiac Society: coronary angioplasty in the United Kingdom. Br. Heart J. 66, 325–331 (1991).
Heart and Stroke Facts: Statistical Supplement, American Heart Association. http://www.americanheart.org/statistics. (1996).
Callow, A.D. in Biologic and synthetic vascular prosthesis. 11–26, (ed. Stanley, J.) (Grune and Stratton, New York; 1986).
Edwards, W.S., Holdefer, W.F. & Motashemi, M. The importance of proper caliber of lumen in femoral popliteal artery reconstruction. Surg. Gynecol. & Obstet. 122, 37–42 (1966).
Brewster, D.C. & Rutherford, R.B. Prosthetic Grafts. Vaxcular Surgury. (ed. W.B. Saunders) 492–521, (Philadelphia; 1995).
Stephen, M., Loewenthal, J., Little, J.M., May, J. & Sheil, A.G.R. Autogenous veins and velour Dacron in femoropopliteal arterial bypass. Surgery 81, 314–318 (1977).
O'Donnell, T.F. et al. Correlation of operative findings with angiographic and non-invasive hemodynamic factors associated with failure of PTFE grafts. J. Vasc. Surg. 1, 136–48 (1984).
Gundry, S.R. & Behrendt, D.M. A comparison of fibrin glue, albumin and blood as agents to pretreat porous grafts. J. Surg. Res. 43, 75–77 (1987).
Kottke-Marchant, K., Anderson, J.M., Umemura, Y. & Marchant, R.E. Effect of coating on the in vitro blood compatibility of Dacron arterial prostheses. Biomaterials 10, 14–17 (1989).
Park, K.D. et al. Heparin immobilization onto segmented polyurethane urea surfaces. J. Biomed. Mater. Res. 22, 977–980 (1988).
Zarge, J.L., Huang, P. & Greisler, H.P. in Principles of tissue engineering (eds Lanza, R., Langer, R., & Chick, W.) 349–364 (R.G. Landes Company, Georgetown, TX; 1997).
Herring, M.B., Gardner, A.L. & Glover, J. A single-staged technique for seeding vascular grafts with autogenous endothelium. Surgery 84, 498–502 (1987).
Williams, S.K., Jarrell, B.E. & Kleinert, L.B. Endothelial cell transplantation onto porcine arteriovenous grafts evaluated using a canine model. J. Invest. Surg. 7, 503–517 (1994).
Pasic, M. et al. Superior late patency of small-diameter Dacron grafts seeded with omental microvascular cells: an experimental study. Ann. Thorac. Surg. 58, 677–682 (1994).
Bowlin, G.L. & Rittgers, S.E. Electrostatic endothelial cell seeding technique for small diameter vascular prostheses: feasibility testing. Cell Transplant. 6, 623–629 (1997).
Weinberg, C.B. & Bell, E. A blood vessel model constructed from collagen and cultured vascular cells. Science 231, 397–399 (1986).
Matsuda, T. & Miwa, H. A hybrid vascular model biomimicking the hierarchic structure of arterial wall. J. Thorac. Cardiovasc. Surg. 110, 988–997 (1995).
Ziegler, T., Robinson, K.A., Alexander, R.W. & Nerem, R.M. Co-culture of endothelial and smooth muscle cells in a flow environment: an improved culture model of the vascular wall? Cells Mater. 5, 115–124 (1995).
Tranquillo, R.T., Girton, T.S., Bromberek, B.A., Triebes, T.G. & Mooradian, D.L. Magnetically-oriented tissue-equivalent tubes. Biomaterials 17, 349–353 (1996).
L'Heureux, N., Paquet, S., Germain, L., Labbe, R. & Auger, F.A. A completely biological tissue-engineered human blood vessel. FASEB J. 12, 47–56 (1998).
Niklason, L.E. et al. Functional arteries grown in vitro. Science 284, 489–493 (1999).
Lawler, M.R., Foster, J.H. & Scott, H.W. Evaluation of canine intestinal submucosa as a vascular substitute. Am. J. Surg. 122, 517–519 (1971).
Egusa, S. Replacement of inferior vena cava and abdominal aorta with the autogenous segment of small intestine. Acta Med. 22, 153–165 (1968).
Matsumoto, T., Holmes, R.H. & Burdick, C.D. The fate of the inverted segment of small bowel used for the replacement of major veins. Surgery 60, 739–743 (1966).
Badylak, S.F., Lantz, G.C., Coffey, A. & Geddes, L.A. Small intestinal submucosa as a large diameter vascular graft in the dog. J. Surg. Res. 47, 74–80 (1989).
Lantz, G.C., Badylak, S.F., Coffey, A.C., Geddes, L.A. & Blevins, W.E. Small intestinal submucosa as a small-diameter arterial graft in the dog. J. Invest. Surg. 3, 217–227 (1990).
Termin, P.L., Carr, R.M., O'Neil, K.D. & Connolly, R.J. Thrombogenicity of intestinal submucosa: results of canine ex vivo shunt and acute rabbit implant studies. AAMI Cardiovascular Science and Technology Conference Proceedings, Washington D.C.; (1993).
Hardin-Young, J., Carr, R.M., Downing, G., Condon, K. & Termin, P.L. Modification of native collagen reduces antigenicity but preserves cell compatibility. Biotechnol. Bioeng. 49, 675–682 (1996).
Kim, K.M., Herrera, G.A. & Battarbee, H.D. Role of glutaraldehyde in calcification of porcine aortic valve fibroblasts. Am. J. Pathol. 154, 671–675 (1999).
Abraham, G.A., Carr, R.M., Kemp, P.D. & Baker, L. Chemical Cleaning of Biological Material. PCT publication no. WO 98/49969 (1998).
Falanga, V. et al. Rapid healing of venous ulcers and lack of clinical rejection with an allogeneic cultured human skin equivalent. Arch. Dermatol. 134, 293–299 (1998).
Davies, M., Ramkumar, V., Gettys, T.W. & Hagen, P.-O. The expression and function of G-proteins in experimental intimal hyperplasia. J. Clin. Invest. 94, 1680–1689 (1994).
Davies, PF . Flow-mediated endothelial mechanotransduction. Physiol. Rev. 75, 519–560 (1995).
Mills, I. & Sumpio, B.E. in Tissue engineering of prosthetic vascular grafts (eds Zilla P. & Griesler, H.P.) 425–438, (R.G. Landes Co, Austin, TX; 1999).
Levesque, M.J. & Nerem, R.M. The study of rheological effects on vascular endothelial cells in culture. Biorheology 26, 345–357 (1989).
Davids, L., Dower T. & Zilla, P. in Tissue engineering of prosthetic vascular grafts (eds Zilla P. & Griesler, H.P.). 3–45, (R.G. Landes Co, Austin, TX; 1999).
O' Malley, M.K. et al. Contraction and sensitivity to norephinephrine after endothelial denudation is inhibited by prazosin. Surgery 99, 36–43 (1986).
Kemp, P.D., Carr, R.M. & Maresh, J.G. Collagen constructs. US patent no. 5,256,418 (1993).
Cramer, R., Moore, R. & Amplatz, K. Reduction of surgical complication rate by the use of a hypothrombogenic catheter coating. Radiology 109, 585–588 (1973).
Acknowledgements
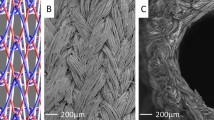
We would like to thank Jeffrey Crews, Rachel Brothers, Kim Medeiros, and Dan O'Reilly of Organogenesis for assistance with the histology, Dr. Joseph Laning for immunological analyses and Dr. Einar Svendsen of the GADE Institute, University of Bergen, Bergen, Norway, for the scanning electron microscopy.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huynh, T., Abraham, G., Murray, J. et al. Remodeling of an acellular collagen graft into a physiologically responsive neovessel. Nat Biotechnol 17, 1083–1086 (1999). https://doi.org/10.1038/15062
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/15062
This article is cited by
-
Current challenges and future trends in manufacturing small diameter artificial vascular grafts in bioreactors
Cell and Tissue Banking (2020)
-
Fabrication and Testing of Electrospun Polyurethane Blended with Chitosan Nanoparticles for Vascular Graft Applications
Cardiovascular Engineering and Technology (2018)
-
Stem Cell Sources and Graft Material for Vascular Tissue Engineering
Stem Cell Reviews and Reports (2018)
-
Engineered electrospun polyurethane and castor oil nanocomposite scaffolds for cardiovascular applications
Journal of Materials Science (2017)