Abstract
The human chromosome X is closely associated with congenital disorders and mental retardation (MR), because it contains a significantly higher number of genes than estimated from the proportion in the human genome. We constructed a high-density and high-resolution human chromosome X array (X-tiling array) for comparative genomic hybridization (CGH). The array contains a total of 1,001 bacterial artificial chromosome (BACs) throughout chromosome X except pseudoautosomal regions and two BACs specific for Y. In four hybridizations using DNA samples from healthy males, the ratio of each spotted DNA was scattered between −3SD and 3SD, corresponding to a log2 ratio of −0.35 and 0.35, respectively. Using DNA samples from patients with known congenital disorders, our X-tiling array was proven to discriminate one-copy losses and gains together with their physical sizes, and also to estimate the percentage of a mosaicism in a patient with mos 45,X[13]/46,X,r(X)[7]. Furthermore, array-CGH in a patient with atypical Schinzel-Giedion syndrome disclosed a 1.1-Mb duplication at Xq22.3 including a part of the IL1RAPL2 gene as a likely causative aberration. The results indicate our in-house X-tiling array to be useful for the identification of cryptic copy-number aberrations containing novel genes responsible for diseases such as congenital disorders and X-linked MR.
Similar content being viewed by others
Introduction
The human chromosome X is involved in a number of genetic diseases and has been suggested to contain a significantly higher number of gene mutations of which can cause mental retardation (MR), developmental delays, and other congenital disorders (Zechner et al. 2001). According to an on-line database (Ensembl version 39, Jun 2006, http://www.ensembl.org/Homo_sapiens/mapview?chr=X), the chromosome X includes 879 known and 107 novel protein-coding genes, which are 4.16% of all human protein-coding genes. Among 1,346 entries for MR in online-Mendelian inheritance in man (OMIM, http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?db=OMIM), 340 (25.3%) are mapped on the chromosome X. Moreover, among 277 entries for “congenital anomaly”, 77 (27.8%) are mapped on chromosome X, likewise 51 (36.1%) of 141 entries for “multiple congenital anomaly” and 336 (25.5%) of 1,320 entries for “congenital disorder” are on the chromosome X. The frequency of each is apparently higher than that estimated from the proportion of genes on chromosome X.
Since many of the genes associated with X-linked MR (XLMR) and other X-linked conditions have been identified from studies of microscopically visible X-chromosomal abnormalities, such as chromosomal translocation breakpoints and deletions, conventional cytogenetics has been often applied to examinations of unknown congenital disorders. However, due to its limited resolution (5–10 Mb), there is a strong need for more sensitive and comprehensive assays for the identification of genes related to X-linked conditions. A recently developed array-based comparative genomic hybridization (array-CGH) technique has enabled a high-throughput analysis of genomic copy-number aberrations with a resolution limited by the size of the clones used and the distance between each of them (Pinkel et al. 1998; Inazawa et al. 2004). Nowadays, array-CGH has become the method of choice for the quantitative detection of chromosomal copy-number abnormalities with precise position and size in tumors as well as in genetic diseases. Using either a bacterial artificial chromosome (BAC)-based array or oligonucleotide-based array, cryptic chromosomal copy-number aberrations and subtle genomic rearrangements at breakpoints of translocation with copy-number changes have been detected in patients with nonspecific congenital disorders, including idiopathic MR and dysmorphic features (Veltman et al. 2004; Cowell et al. 2005; Hayashi et al. 2005; Kok et al. 2005; Rosenberg et al. 2005; Sanlaville et al. 2005; Schoumans et al. 2005; Tyson et al. 2005).
In order to investigate genomic copy-number aberrations in human diseases, we have developed various BAC-based genomic arrays (Inazawa et al. 2004). Here, we report the construction of a full coverage chromosome X array (MCG X-tiling array), containing 1,001 BAC/PACs (P1-derived artificial chromosome) throughout the chromosome X besides peudoautosomal regions and regions showing cross-hybridization with the chromosome Y. The performance of our MCG X-tiling array was validated by hybridization of four pairs of DNAs from healthy males. Further, we tested subjects with X-linked or unknown genetic disorders including congenital anomalies suspected to have some cryptic genomic aberrations on chromosome X using our MCG X-tiling array.
Materials and methods
Subjects
The subjects for our MCG X-tiling array analyses were as follows; (1) Four healthy males for the validation of each clone spotted on the X-tiling array (2) Three patients (Patient 1–3, Table 1) with known genomic aberrations on chromosome X for the evaluation of performance (3) One patient (Patient 4, Table 1) with Schinzel-Giedion syndrome (SGS, MIM %269150), who had a submicroscopic duplication at Xq22.3 detected by another of our in-house CGH-arrays. In this patient, we performed more detailed examination of the duplication by using the X-tiling array.
Genomic DNA from each subject was isolated from peripheral blood lymphocytes or lymphoblastoid cell lines (LCL) established by Epstein-Bar virus transformation as described (Saito-Ohara et al. 2002). DNA samples were obtained from all of the patients or their parents and also healthy volunteers with prior written consent from each patient and approval by the local ethics committee.
Clinical features
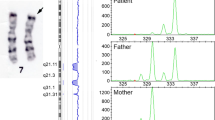
Patient 1 was a boy diagnosed with atypical severe Duchenne muscular dystrophy (DMD), having several features of Pelizaeus-Merzbacher disease (PMD); profound mental retardation, early-onset muscle weakness and nystagmus as described in our previous report (Saito-Ohara et al. 2002). His karyotype was 46,Y,inv(X)(p21.2q22.2), and that of his mother was 46,X,inv(X)(p21.2q22.2) (Fig. 1a). Detailed molecular cytogenetic analysis studies revealed that he had two cryptic copy-number aberrations at the breakpoints of his inv(X); a deletion including a part of DMD at Xp21.2 and a duplication including PLP1 at Xq22, respectively (Saito-Ohara et al. 2002). Patient 2 was a girl whose karyotype was 46,X,del(X)(p11.4p22.2) (Fig. 1b), but who had no symptoms of Turner syndrome. Patient 3 was a girl who had a mosaicism, mos 45,X[13]/46,X,r(X)(p21?q21?)[7], though GTG-banding could not reveal the precise breakpoints involved (Fig. 1c). Patient 4 was a girl born in the 37th week of gestation to non-consanguineous parents. Her birth weight was 3,304 g. She was diagnosed with Schinzel-Giedion syndrome (SGS; MIM %269150) based on facial anomalies (hirsutism, frontal bossing, midface dysplasia, hypertelorism, low-set ears, and micrognathia), genital anomalies, bilateral hydronephrosis, and the malformation of several bones (short sclerotic skull base, broad ribs, and hypoplastic pubic bones). She was also diagnosed with Hirschsprung disease based on abdominal bloating and acetylcholinesterase staining of rectal biopsy. At present, 14 months of age, she shows severe developmental delay, cannot hold her neck-up, does not reveal tracking, and can speak only bubbling. Her karyotype was 46,XX (data not shown).
A Partial karyotype of R-banded X chromosomes in the mother of Patient 1: left is an intact X chromosomes and right is inv(X)(p21.2q22.2). Arrows indicate breakpoints at the inv(X). B GTG-banded chromosomes X of Patient 2: an arrow indicates the breakpoint involved in 46,X,del(X)(p11.4p22.2). C GTG-banded chromosomes X of Patient 3: the breakpoint of r(X)(p21?q21?) could not be clearly identified by conventional cytogenetics
Cytogenetic analysis
Analyses of GTG-banded metaphase chromosomes were performed with cultured peripheral blood lymphocytes using standard methods. In Patient 1, R-banded metaphase chromosomes were prepared by the thymidine synchronization and bromodeoxyuridine (BrdU) release technique as described (Inazawa et al. 1993).
Preparation of the array
The array was constructed using BAC/PAC clones from the chromosomes X and Y selected according to information in the genomic database (http://www.genome.ucsc.edu/; freeze May 2004). Genomic target DNAs were isolated from 50-ml bacterial cultures using the Plasmid mini kit (Qiagen, Tokyo, Japan) following the instructions of the manufacturer with minor modifications. The chromosomal position of each BAC/PAC clone was confirmed by fluorescence in situ hybridization (FISH) as described below. After being restricted with the DpnI, HaeIII, and RsaI enzymes, the DNA was combined, ligated to the adaptor, purified with nucleospin extract (Macherey-Nagel, Düren, Germany), and stored at −20°C (“immortalization” of target genomic DNA). Three nanograms of immortalized DNA was amplified by two rounds of adaptor polymerase chain reaction (PCR) (Tanabe et al. 2003) using an amino-linked primer, and purified with Microcon (Millipore, Billerica, Mass., USA). Purified amino-linked PCR products were dissolved in printing solution and spotted in duplicate at a concentration of 750 ng/μl on slides for amino-linked oligonucleotides (Matsunami Glass, Osaka, Japan) with a Geneshot ink-jet spotter (NGK Insulators, Aichi, Japan).
Array-CGH analysis
Hybridizations were performed as described elsewhere (Hayashi et al. 2005; Takada et al. 2005) with minor modifications. Briefly, 0.375 μg of test and reference genomic DNA was labeled with Alexa Fluor 555 and 647, respectively, using a BioPrime Plus Array CGH Indirect Genomic Labeling system (Invitrogen, Carlsbad, Calif., USA), and co-hybridized with Cot-1 DNA to X-tiling slides in a hybridization machine, HYBRIMASTER HS-300eTAC (ALOKA, Tokyo, Japan). After hybridization, the slides were scanned with a GenePix 4000B (Axon Instruments, Foster City, Calif., USA). Acquired images were analyzed with GenePix Pro 6.0 imaging software (Axon Instruments). Fluorescence ratios were normalized so that the mean of the middle third of log2ratios across the array was zero. The thresholds for copy-number gain and loss were set at log2 ratios of 0.35 and −0.35, respectively, as described below.
When a MCG whole genome array-4500 which contained 4,523 BAC clones covering the entire genome at intervals of approximately 0.7 Mb was employed (Inazawa et al. 2004; Hayashi et al. 2005), 1.5 μg instead of 0.375 μg of genomic DNA was used for hybridization.
FISH
Metaphase chromosomes were prepared from normal male lymphocytes and from patients’ lymphocytes using the standard method. FISH analyses were performed as described elsewhere (Hayashi et al. 2005) using a BAC located around the region of interest as probes.
Quantitative real-time PCR
In order to define the region with copy-number aberrations detected by array-CGH, quantitative real-time PCR experiments were performed with an ABI Prism 7900 sequence-detection system using SYBR Green PCR Master Mix (Applied Biosystems, Foster City, Calif., USA) according to the manufacturer’s instructions as described previously (Takada et al. 2005). The designed primer sequences in five exons of the IL1RAPL2 gene, two exons of the PLP1 gene, one exon of the FMR2 gene as a normal copy-number control are listed in Table 2. Each assay was performed in triplicate.
Assays for X-chromosome inactivation
The pattern of X-chromosome inactivation in a female was first evaluated using an androgen receptor (AR) X-inactivation assay (Kubota et al. 1999) with minor modifications (Honda et al. 2007). Briefly, DNA modified with sodium bisulfite was amplified with primers specific for methylated or unmethylated DNA sequences in the human AR locus, where methylation status corresponded with X-inactivation. Products of two different sizes were gained from the paternal and maternal alleles because of the polymorphism of the triplet repeat, and their peak images were measured using a 3130 Genetic analyzer (Applied Biosystems) with GeneMapper Software v4.0 (Applied Biosystems). An imbalance of chromosome X inactivation (skewing) was judged based on the ratio of the amount of PCR product from the paternal versus maternal allele.
For a patient showing an imbalance of X-inactivation by PCR, we evaluated X-inactivation in metaphase chromosomes from LCL using the BrdU-labeling technique in late S-phase (Inazawa et al. 1993). Those chromosomes were used for FISH to show the affected chromosome X as described (Panasiuk et al. 1997; Honda et al. 2007).
Results
Validation of the clones on the X-tiling array and decision of thresholds
According to the information in the genomic database (http://www.genome.ucsc.edu/; freeze May 2004), we selected BAC and PAC clones almost fully covering the entire chromosome X except pseudoautosomal regions and regions showing similarity with the chromosome Y. We performed FISH using all the picked clones, and eliminated clones which hybridized to unexpected chromosomal regions, showed multiple signals, and contained repetitive sequences judged by visual inspection of signal patterns in metaphase as well as interphase chromosomes. Through this process, we selected a total of 1,003 BAC/PAC clones including 1,001 from chromosome X together with two from chromosome Y as a reference.
In order to validate each of the clones on the MCG X-tiling array, we performed array-CGH using the same DNA for both the test and reference. Each DNA was extracted from peripheral blood mononuclear cells of four healthy males, thus this trial was performed four times. Since the normalized and log2-translated ratios follow a normal distribution, standard deviation (SD) can be used to define thresholds (Vermeesch et al. 2005). We performed four hybridizations to confirm that all ratios were contained between −3SD and +3SD (Fig. 2a). Also, −3SD and +3SD correspond to 0.78 and 1.27 as the primary ratio, and to −0.35 and 0.35 as the log2 ratio, respectively.
a Validation of the MCG X-tiling array using identical genomic DNA for both the test and reference. Genomic DNA was isolated from four healthy males. Clones are order according to the UCSC mapping position (http://www.genome.ucsc.edu/; freeze May 2004). Each spot represents test over reference value after normalization and log2 transformation in each BAC clone. Dotted horizontal lines indicate −3SD and +3SD, which correspond to −0.35 (open arrowhead) and 0.35 (filled arrowhead) as a log2 ratio, respectively. The vertical gray bar indicates a centromere’s position. b Histogram of the ratios obtained for the four control hybridizations. Thresholds for copy-number gain and loss were set at a log2 ratio of −0.35 and 0.35, respectively
Applicability of the X-tiling array
In order to validate the use of our X-tiling array to detect copy-number aberrations, we hybridized DNA from the patients with known aberrations on the chromosome X, which were already confirmed by a conventional GTG banding technique. These tests included the detection of one-copy deletion and duplication (Patient 1), estimation of the physical distance involved in genomic aberrations (Patient 2), and evaluation of the proportion of a mosaicism (Patient 3).
In Patient 1, one-copy deletion and duplication were detected correctly, since our X-tiling array revealed a 0.8-Mb deletion at Xp21.2-p21.1 and 1.3-Mb duplication at Xq22.1-q22.2 (Fig. 3a; Table 1).
Validation of the use of the X-tiling array to detect known copy-number aberrations. Each clone is plotted in the same manner as in Fig. 1. Vertical gray bars indicate positions of centromeres. a Results of X-tiling array for Patient 1. A 0.8-Mb deletion at Xp21.2-p21.1 (filled arrowhead) and 1.3-Mb duplication at Xq22.1-q22.2 (open arrowhead) were detected (Table 1). b Results of X-tiling array for Patient 2. A 24.2-Mb deletion at Xp22.3-p22.11 (closed arrow) is estimated from the reduced ratios of 124 clones in a female patient with partial monosomy of chromosome X (Table 1). c Results of X-tiling array for Patient 3 with mos 45,X[13]/46,X,r(X)(p21?q21?)[7]. In the array CGH, DNA from a normal male was employed as a reference. The genomic region of r(X) was detected (closed arrow) by regular hybridization (blue) and dye-swap hybridization (red) on the MCG X-tiling array. The 65-Mb normal diploid region from Xp11.22 to Xq24 (Table 1) was due to the sum of her intact X and r(X) with 1.25 as a primary ratio. Since the DNA of a healthy male was used as a normal control, both 45,X and the deleted region of the ring chromosome would reveal a primary ratio of 1.0 and the intact region of the ring, a ratio of 2.0. In fact, the average primary ratio in the intact region was about 1.25, which meant that 45,X occupied about 75%. Therefore, we presumed that the percentage of the ring chromosome was about 25%, which is similar to the percentage determined by conventional cytogenetics
In Patient 2, we detected a 24.2-Mb deletion at Xp22.3-p22.11 (Fig. 3b), clearly indicating that our array can confer useful information on physical distance together with a precise location through our X-tiling array at a single copy level even for microscopically detectable chromosomal copy-number aberrations. The proximal breakpoint was between clones RP11-326H11 and RP11-79B3 (Fig. 3b; Table 1).
In Patient 3, in order to evaluate the proportion of the mosaicism in mos 45, X[13]/46,X,r(X)(p21?q21?)[7] as well as to determine the precise breakpoints involved in the r(X) on our array platform, we performed an X-tiling array analysis with DNA from a healthy male as a normal control in a dye-swap hybridization manner. We detected a 65-Mb normal diploid region from Xp11.22 to Xq24 (Fig. 3c; Table 1) due to her intact X and r(X) with 1.25 as a primary ratio. Since the expected primary ratio was 2.0 on the assumption that all lymphocytes were 46,X,r(X) and 1.0 on the assumption that all lymphocytes were 45,X, the percentage of lymphocytes bearing 46,X,r(X) was estimated at 25% in the normal diploid, which is consistent with the results of the conventional cytogenetic analysis.
Application of MCG X-tiling for unknown congenital disorders
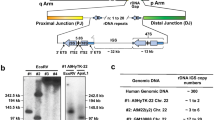
In Patient 4, we had detected a duplication of approximately 1.0–1.8 Mb at Xq22.3 using the MCG Whole Genome Array−4500. In order to define the aberration more precisely, an X-tiling array analysis was performed and revealed an approximately 1.1-Mb-wide duplication between RP11-230E14 and RP11-829N22 at Xq22.2-Xq22.3 (Fig. 4a; Table 1), including a part of the IL1RAPL2 gene. FISH analyses confirmed the partial duplication of IL1RAPL2 (Fig. 4b), and additional FISH analyses in parents of the patient revealed no duplication of this region (data not shown), indicating that the aberration is de novo and might be causative. To determine the precise extent of this duplicated region, a quantitative real-time PCR was performed using primer pairs for exons 3, 6, 7, 8, and 11 of IL1RAPL2. Exons 3 and 6 showed a pattern of three copies, whereas exons 7, 8 and 11 were present as two copies in the proband (Fig. 4c), suggesting that the boundary of the IL1RAPL2 duplication is located between exons 6 and 7 (Fig. 4d). We next assessed X-chromosomal inactivation status using a methylation-specific PCR for bisulfite-converted DNA (Kubota et al. 1999; Honda et al. 2007), and could estimate clearly the status of the X-inactivation (Fig. 4e). We then determined the inactivated allele by FISH using BrdU-labeled metaphases. In 12 of 20 metaphases, an allele harboring duplication at Xq22.2-Xq22.3 showed late-replication indicative of an inactivated X (Fig. 4f). Although we tried to evaluate the expression level of IL1RAPL2 by RT-PCR, unfortunately we detected no PCR product because of an extremely low expression level of this gene in lymphocytes (data not shown).
The result of genomic analyses of Patient 4 with Schinzel-Giedion syndrome (SGS). a X-tiling array analysis using genomic DNA from the proband and a normal female as test and reference samples, respectively. Each clone is plotted in the same manner as in Fig. 2. A black arrow indicates the duplicated clones, and her detailed copy-number karyotype is described in Table 1. b FISH using BACs specific for Xq22.3 (RP11-539A6, green) and Xp22.33 (RP11-95C16, red) as a control. A green signal was duplicated on one allele (arrow). Inset; enlarged X chromosomes, the right shows dup(X), and the left is a normal X. c Real-time quantitative PCR analysis for the proband (filled circles) and a normal female (open circles) as test and reference samples, respectively, in each exon of IL1RAPL2. A ratio of 1 indicates that the target sequences are present as two copies. Notably, the genomic sequences were present as three copies at exons 3 and 6, but two copies at exons 7, 8 and 11 in the proband. d A map of the duplicated region. Each clone is aligned according to the UCSC Genome Browser (assembled on May 2004; http://www.genome.ucsc.edu/). Open rectangles indicate duplicated BAC clones, and filled rectangles indicate clones with a normal copy-number. Open closed arrow indicates the duplicated region. The horizontal thick bar indicates the IL1RAPL2 gene and vertical lines and numbers indicate exons and exon numbers, respectively. e Result of a methylation-specific PCR assay. The X-axis represents product size and the Y-axis represents the fluorescent intensity of electrophoretic bands. The upper panel shows peak patterns derived using primers specific for methylated alleles, revealing that the size of the peak was 216 bp (filled arrowhead), whereas the lower panel shows patterns derived using primers specific for unmethylated alleles, revealing the size of the peak to be 213 bp (open arrowhead). f Result of FISH using BrdU-labeled metaphase chromosomes. The duplicated allele showed late-replication revealing inactivation (filled arrowhead), whereas the intact allele showed early-replication revealing activation (open arrowhead). Each signal for FISH is the same as in Fig. 4b. Inset; enlarged X chromosomes, the right is an inactivated X, and the left is an activated X
Discussion
We have constructed a high-density and high-resolution human chromosome X array for CGH and used it to investigate genomic aberrations in patients with congenital anomalies, developmental delays, and MR. In the process of constructing this X-tiling array, we first validated whether each BAC contains genomic DNA from the chromosome X by FISH on metaphase chromosomes. Since Bejjani et al. (2005) reported that 7% of the clones used for the construction of their BAC-based genomic array were mismapped in publicly available human genome databases, we picked out 1,250 BAC/PAC clones assigned to chromosome X from a genome database and with each of these performed FISH to choose clones sufficient for our criteria described above (data not shown). Finally, we selected 1,001 BAC/PAC clones correctly hybridized to the chromosome X and two hybridized to the chromosome Y.
Inefficient hybridization of each spot due to the low complexity of a sequence, high repeat content, or lack of enough DNA gives a high signal/noise ratio in an array-CGH analysis (Bauters et al. 2005). In our four hybridizations using identical DNA for both the test and reference, each of the clones showed a similar signal ratio and all values were within the range −3SD to +3SD corresponding to −0.35 and 0.35 as a log2 ratio, respectively, after normalization, suggesting that all clones might have appropriate hybridization capacity providing sufficient signal intensity for analysis.
Next, we validated the potential of the array by performing hybridizations in patients with known genomic aberrations. As shown in Fig. 3, our array was able to detect one-copy deletion and duplication (Fig. 3a) with a precise estimation of their extent (Fig. 3b). In addition, our array detected the genomic copy-number aberration and its precise breakpoint regions even in a mosaicism of r(X) in a girl. Indeed, although conventional cytogenetics revealed that the breakpoints were probably involved in regions Xp21 and Xq21, our X-tiling array CGH clearly showed the precise breakpoints of the r(X) to be Xp11.22 and Xq24, respectively, together with the base-position around each of the breaks according to the information in a genomic database (http://www.genome.ucsc.edu/; freeze May 2004) (Fig. 3c). Further, by comparing the detected ratio with the expected ratio, we could also estimate a substantial proportion of the r(X) in her mosaicism. These results indicate that our X-tiling array can detect genomic copy-number aberrations in a highly sensitive, specific, and quantitative manner with a good resolution.
An array-CGH analysis using the X-tiling array could be applied to patients with disorders of X-linked inheritance, those with diseases suspected to be associated with sex chromosome-linked inheritance, and patients with some chromosome X aberrations detected by other methods, e.g., conventional karyotypic analysis and genomic arrays other than the X-tiling array.
In Patient 4, we detected a duplication of approximately 1.1 Mb at Xq22.3 in a girl diagnosed as having SGS with Hirschsprung disease. The duplication involved exons 1–6 of the IL1RAPL2 gene (Fig. 4c, d), and X-inactivation was not skewed (Fig. 4e, f). IL1RAPL2 is a close homologue of IL1RAPL1 (Sana et al. 2000), and the two share 65% amino acid identity (Jin et al. 2000). IL1RAPL2 is expressed strongly in the central nervous system not only in adulthood but also in the fetal period (Ferrante et al. 2001), and partial or whole microdeletions of IL1RAPL1 in patients with XLMR have been reported (Carrié et al. 1999). More recently, a truncating mutation of IL1RAPL1 was reported to be responsible for XLMR in a MRX21 family (Tabolacci et al. 2006). However, no aberration of IL1RAPL2 at the nucleotide or chromosome level has been reported in any congenital anomalies, developmental disorders, or MR. In our patient, the duplication disrupts IL1RAPL2 within one of the two duplicons, which might be associated with the generation of its aberrant transcript or the dosage aberration, resulting in MR and/or other phenotypes. Although SGS has been suggested to be an autosomal recessive (AR) model of inheritance (Schinzel et al. 1978; Antich et al. 1995), the findings for our patient do not support an AR-type inheritance. However, the majority of cases of SGS are sporadic and this syndrome is an extremely rare disorder with fewer than 30 patients reported to date (Minn et al. 2002; Jones et al. 2006), and the recurrence in only 1 of the 20 families does not firmly sustain an AR inheritance pattern (Culic et al. 1996). Therefore, a subset of SGS may possibly show some other inheritance pattern, like Cornelia de Lange syndrome (CDLS, MIM 122470), which has two causative genes and two inheritance patterns, autosomal dominant and X-linked recessive (Krantz et al. 2004; Tonkin et al. 2004; Musio et al. 2006). However, it is difficult to explain the various phenotypes of the patient based only on the aberration of IL1RAPL2.
Here, we described several applications of our MCG X-tiling array to the CGH analysis of the human genome. Although several genomic structural aberrations, such as a balanced translocation without a genomic copy-number aberration or parental disomy, cannot be detected by BAC array-based CGH, the method has the potential to uncover hidden genomic copy-number aberrations behind unknown congenital abnormalities, developmental delays, and MR when used together with other cytogenetic techniques. Indeed, candidate regions associated with XLMR, distinctive of copy-number variation (CNV) (Redon et al. 2006), have emerged on our in-house X-tiling array during the cause of our on-going study for screening cryptic chromosome aberrations in a cohort of Japanese families with XLMR.
Reference
Antich J, Manzanares R, Camarasa F, Krauel X, Vila J, Cusi V (1995) Schinzel-Giedion syndrome: report of two sibs. Am J Med Genet 59:96–99
Bauters M, Van Esch H, Marynen P, Froyen G (2005) X chromosome array-CGH for the identification of novel X-linked mental retardation genes. Eur J Med Genet 48:263–275
Bejjani BA, Saleki R, Ballif BC et al (2005) Use of targeted array-based CGH for the clinical diagnosis of chromosomal imbalance: is less more? Am J Med Genet 134:259–267
Carrié A, Jun L, Bienvenu T et al (1999) A new member of the IL-1 receptor family highly expressed in hippocampus and involved in X-linked mental retardation. Nat Genet 23:25–31
Cowell JK, LaDuca J, Rossi MR, Burkhardt T, Nowak NJ, Matsui S (2005) Molecular characterization of the t(3;9) associated with immortalization in the MCF10A cell line. Cancer Genet Cytogenet 163:23–29
Culic V, Resic B, Oorthuys JW, Overweg-Plandsoen WC, Hennekam RC (1996) A Croatian patient of the Schinzel-Giedion syndrome. Genet Couns 7:21–25
Ferrante MI, Ghiani M, Bulfone A, Franco B (2001) IL1RAPL2 maps to Xq22 and is specifically expressed in the central nervous system. Gene 275:217–221
Hayashi S, Kurosawa K, Imoto I, Mizutani S, Inazawa J (2005) Detection of cryptic chromosome aberrations in a patient with a balanced t(1;9)(p34.2;p24) by array-based comparative genomic hybridization. Am J Med Genet 139:32–36
Honda S, Hayashi S, Kato M et al (2007) Clinical and molecular cytogenetic characterization of two patients with non-mutational aberrations of the FMR2 gene. Am J Med Genet (in press)
Inazawa J, Saito H, Ariyama T, Abe T, Nakamura Y (1993) High-resolution cytogenetic mapping of 342 new cosmid markers including 43 RFLP markers on human chromosome 17 by fluorescence in situ hybridization. Genomics 17:153–162
Inazawa J, Inoue J, Imoto I (2004) Comparative genomic hybridization (CGH)-arrays pave the way for identification of novel cancer-related genes. Cancer Sci 95:559–563
Jin H, Gardner RJ, Viswesvaraiah R, Muntoni F, Roberts RG (2000) Two novel members of the interleukin-1 receptor gene family, one deleted in Xp22.1-Xp21.3 mental retardation. Eur J Hum Genet 8:87–94
Jones KL (2006) SMITH’s recognizable patterns of human malformation. Elsevier Saunders, Philadelphia, pp 250–251
Kok K, Dijkhuizen T, Swart YE et al (2005) Application of a comprehensive subtelomere array in clinical diagnosis of mental retardation. Eur J Med Genet 48:250–262
Krantz ID, McCallum J, DeScipio C et al (2004) Cornelia de Lange syndrome is caused by mutations in NIPBL, the human homolog of Drosophila melanogaster Nipped-B. Nat Genet 36:631–635
Kubota T, Nonoyama S, Tonoki H et al (1999) A new assay for the analysis of X-chromosome inactivation based on methylation-specific PCR. Hum Genet 104:49–55
Minn D, Christmann D, De Saint-Martin A et al (2002) Further clinical and sensorial delineation of Schinzel-Giedion syndrome: report of two patients. Am J Med Genet 109:211–217
Musio A, Selicorni A, Focarelli M.L et al (2006) X-linked Cornelia de Lange syndrome owing to SMC1L1 mutations. Nat Genet 38:528–530
Panasiuk B, Midro AT, Zadrozna-Tolwinska B (1997) Earlier finishing of Xp21.2 subband replication of the inactive X chromosome in Rett syndrome girl but not in her 47,XXX mother. Clin Genet 52:120–125
Pinkel D, Segraves R, Sudar D et al (1998) High resolution analysis of DNA copy number variation using comparative genomic hybridization to microarrays. Nat Genet 20:207–211
Redon R, Ishikawa S, Fitch KR et al (2006) Global variation in copy number in the human genome. Nature 444:444–454
Rosenberg C, Knijnenburg J, Chauffaille Mde L et al (2005) Array CGH detection of a cryptic deletion in a complex chromosome rearrangement. Hum Genet 116:390–394
Saito-Ohara F, Fukuda Y, Ito M et al (2002) The Xq22 inversion breakpoint interrupted a novel Ras-like GTPase gene in a patient with Duchenne muscular dystrophy and profound mental retardation. Am J Hum Genet 71:637–645
Sana TR, Debets R, Timans JC, Bazan JF, Kastelein RA (2000) Computational identification, cloning, and characterization of IL-1R9, a novel interleukin-1 receptor-like gene encoded over an unusually large interval of human chromosome Xq22.2-q22.3. Genomics 69:252–262
Sanlaville D, Lapierre JM, Turleau C et al (2005) Molecular karyotyping in human constitutional cytogenetics. Eur J Med Genet 48:214–231
Schinzel A, Giedion A (1978) A syndrome of severe midface retraction, multiple skull anomalies, clubfeet, and cardiac and renal malformations in sibs. Am J Med Genet 1:361–375
Schoumans J, Ruivenkamp C, Holmberg E, Kyllerman M, Anderlid BM, Nordenskjold M (2005) Detection of chromosomal imbalances in children with idiopathic mental retardation by array based comparative genomic hybridisation (array-CGH). J Med Genet 42:699–705
Tabolacci E, Pomponi MG, Pietrobono R, Terracciano A, Chiurazzi P, Neri G (2006) A truncating mutation in the IL1RAPL1 gene is responsible for X-linked mental retardation in the MRX21 family. Am J Med Genet 140:482–487
Takada H, Imoto I, Tsuda HS et al (2005) Screening of DNA copy-number aberrations in gastric cancer cell lines by array-based comparative genomic hybridization. Cancer Sci 96:100–110
Tanabe C, Aoyagi K, Sakiyama T et al (2003) Evaluation of a whole-genome amplification method based on adaptor-ligation PCR of randomly sheared genomic DNA. Genes Chromosomes Cancer 38:168–176
Tonkin ET, Wang TJ, Lisgo S, Bamshad MJ, Strachan T (2004) NIPBL, encoding a homolog of fungal Scc2-type sister chromatid cohesion proteins and fly Nipped-B, is mutated in Cornelia de Lange syndrome. Nat Genet 36:636–641
Tyson C, Harvard C, Locker R et al (2005) Submicroscopic deletions and duplications in individuals with intellectual disability detected by array-CGH. Am J Med Genet 139:173–185
Veltman JA, Yntema HG, Lugtenberg D et al (2004) High resolution profiling of X chromosomal aberrations by array comparative genomic hybridisation. J Med Genet 41:425–432
Vermeesch JR, Melotte C, Froyen G et al (2005) Molecular karyotyping: array CGH quality criteria for constitutional genetic diagnosis. J Histochem Cytochem 53:413–422
Zechner U, Wilda M, Kehrer-Sawatzki H, Vogel W, Fundele R, Hameister H (2001) A high density of X-linked genes for general cognitive ability: a run-away process shaping human evolution? Trends Genet 17:697–701
Acknowledgements
We are grateful to Dr. Masahiro Ito and Dr. Fumiko Saito-Ohara for a useful discussion on a patient with DMD and PMD. We also thank Ms. Ayako Takahashi and Ms. Rumi Mori for their technical assistance. This study was supported by Grants-in-Aid for Scientific Research on Priority Areas and 21st Century Center of Excellence Program for Molecular Destruction and Reconstitution of Tooth and Bone from the Ministry of Education, Culture, Sports, Science, and Technology, Japan; and by a Grant-in-Aid from Core Research for Evolutional Science and Technology (CREST) of the Japan Science and Technology Corporation (JST).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hayashi, S., Honda, S., Minaguchi, M. et al. Construction of a high-density and high-resolution human chromosome X array for comparative genomic hybridization analysis. J Hum Genet 52, 397–405 (2007). https://doi.org/10.1007/s10038-007-0127-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-007-0127-4
Keywords
This article is cited by
-
A novel intragenic deletion in OPHN1 in a Japanese patient with Dandy-Walker malformation
Human Genome Variation (2018)
-
Concomitant microduplications of MECP2 and ATRX in male patients with severe mental retardation
Journal of Human Genetics (2012)
-
Novel intragenic duplications and mutations of CASK in patients with mental retardation and microcephaly with pontine and cerebellar hypoplasia (MICPCH)
Human Genetics (2012)
-
Commentary on ‘Identification of a microdeletion at Xp22.13 in a Taiwanese family presenting with Nance–Horan syndrome’
Journal of Human Genetics (2011)
-
Clinical application of array-based comparative genomic hybridization by two-stage screening for 536 patients with mental retardation and multiple congenital anomalies
Journal of Human Genetics (2011)