Abstract
Cell-free fetal DNA (cffDNA) in the supernatant of amniotic fluid, which is usually discarded, can be used as a sample for prenatal diagnosis. For rapid prenatal diagnosis of frequent chromosome abnormalities, for example trisomies 13, 18, and 21, and monosomy X, using cffDNA, we have developed a targeted microarray-based comparative genomic hybridization (CGH) panel on which BAC clones from chromosomes 13, 18, 21, X, and Y were spotted. Microarray-CGH analysis was performed for a total of 13 fetuses with congenital anomalies using cffDNA from their uncultured amniotic fluid. Microarray CGH with cffDNA led to successful molecular karyotyping for 12 of 13 fetuses within 5 days. Karyotypes of the 12 fetuses (one case of trisomy 13, two of trisomy 18, two of trisomy 21, one of monosomy X, and six of normal karyotype) were later confirmed by conventional chromosome analysis using cultured amniocytes. The one fetus whose molecular-karyotype was indicated as normal by microarray CGH actually had a balanced translocation, 45,XY,der(14;21)(q10;q10). The results indicated that microarray CGH with cffDNA is a useful rapid prenatal diagnostic method at late gestation for chromosome abnormalities with copy-number changes, especially when combined with conventional karyotyping of cultured amniocytes.
Similar content being viewed by others
Introduction
Karyotyping of cultured fetal cells is the standard method for prenatal diagnosis of chromosomal abnormalities. It usually requires 10–14 days to receive a result, however, and may have some problems, e.g. occasional failure of cell culture, wrong karyotype because of artifacts during cell culture, and psuedomosaicism associated with maternal-cell contamination. The recently developed microarray-based comparative genomic hybridization (microarray CGH) does not require dividing cells and enables rapid, automated, high-throughput screening of chromosome abnormalities (Pollack et al. 1999). In this system, DNA from bacteria-derived artificial chromosome (BAC) that had been precisely mapped to regions in the human genome was amplified by the degenerated oligonucleotide primed (DOP)-PCR method and used as target DNA on the microarray (Telenius et al. 1992). Consequently, microarray CGH made rapid whole-chromosome analysis possible in a single experiment, compared with thousands of experiments using independent fluorescence in-situ hybridization (FISH) (Lapierre et al. 2000; Oostlander et al. 2004; Lau and Leung 2005).
Cell-free fetal DNA (cffDNA) in amniotic fluid obtained by amniocentesis is usually ignored and discarded; it is, however, becoming an attractive sample for prenatal diagnosis (Bianchi 2000; Bianchi and Lo 2001; Watanagara and Bianchi 2004; Hahn et al. 2005; Lo 2005). A recent report pointed out that cffDNA from amniotic fluid is a potential sample for microarray-based diagnosis, because its performance in hybridization is similar to that of cellular DNA (Larrabee et al. 2004). However, its accuracy, reproducibility, analytical and clinical validity, and clinical utility have not been well demonstrated. Little is known about whether microarray CGH with cffDNA is a rapid and effective analytical method for diagnosis of unbalanced chromosomal aberrations, or how to use the method in uncultured amniotic fluid. In clinical medicine, situations often arise which involve pregnancies requiring a rapid prenatal diagnosis for appropriate fetal management, for example those with fetal multiple anomalies detected by ultrasound examination at late gestation (Drummond et al. 2003; Nyberg and Souter 2000; Yang et al. 2005). In this situation, utilization of cffDNA from crude amniotic fluid may make it possible to shorten the testing time for molecular karyotyping. Also, as common chromosomal abnormalities during perinatal care were trisomy 13, 18, and 21, and monosomy X, a targeted microarray based CGH panel of these chromosomes could be efficient.
In this study, we investigated whether targeted microarray-CGH analysis using cffDNA in uncultured amniotic fluid can be used for rapid screening for common chromosomal abnormalities.
Materials and methods
Subjects and DNA preparation
Seven fetuses with congenital anomalies in the 15–17th weeks of gestation and six such fetuses in the 32–34th weeks were included in this study. Fresh amniotic fluid (30 mL) was obtained by transabdominal amniocentesis. Two-thirds of the amniotic fluids were used for 400-band-level G-banding chromosome analysis and the remaining 10 mL were for microarray-CGH assay. The 13 fetuses included one case of trisomy 13, two of trisomy 18, two of trisomy 21, one of monosomy X, one of balanced translocation, three of a normal XY karyotype, and three cases of a normal XX karyotype, all of which were diagnosed by conventional karyotyping of their cultured amniocytes. Study procedures were approved by the Committee for the Ethical Issues on Human Genome and Gene Analysis in Nagasaki University, and written informed consent was obtained from all families.
Fresh amniotic fluid (10 mL) was centrifuged at 350g for 10 min, and the supernatant was centrifuged again at 13,500g for 20 min to remove any remaining cells (Bianchi et al. 2001). The cffDNA was extracted from the second supernatant using the DNA extraction kit (Qiagen, Hilden, Germany). All samples contained at least 800–1,250 ng cffDNA. The performance of the cffDNA in hybridization to microarrays was similar to that of control DNA obtained from a karyotypically normal male adult.
Degenerate oligonucleotide primed (DOP) PCR
Degenerate oligonucleotide primed-PCR was performed to amplify target clone DNA using three different 5′-aminolabeled PCR primers described elsewhere (Harada et al. 2004). PCR was cycled 30 times at 94°C for 30 s, at linear ramping of 37–72°C over 10 min, and at 72°C for 1 min. Successfully amplified PCR products, usually 0.2–2 kb in size, were used for subsequent experiments. Each 100 μL PCR product obtained by use of the three primers was mixed with the same volume of 4× print buffer (1 mol L−1 sodium phosphate/0.001% N-lauroyl sarcosine, pH 8.5) and concentrated to a final volume of 30 μL using Microcon 100 (Millipore, Bedford, MA, USA). The products were mixed with DMSO and ddH2O to a final concentration of 1× print buffer/20% DMSO and were ready for prints.
Microarray CGH
Fifty BAC clones (ten clones each on chromosomes 13, 18, 21, X, and Y) selected from the UCSC genome browser were used as target DNA for microarray (Table 1). Their chromosomal location was confirmed by FISH in our laboratory (Miyake et al. 2006). The target clone DNA amplified by DOP-PCR was spotted in triplicate on to CodeLinkTM activated slides (Amersham Bioscience, Buckinghamshire, UK) using Stampman (Nippon Laser and Electronics Laboratory, Nagoya, Japan) with a center-to-center distance of 1 mm between adjacent spots. The same triplicate-spot panel was prepared in duplicate as blocks A and B on the same slide. The slides were then pretreated, denatured, and stored in a desiccator until use.
The procedure used for microarray-CGH analysis has been described elsewhere (Harada et al. 2004; Miyake et al. 2006). Briefly, the 800 ng digested subject DNA was labeled with Cy3, and control DNA with Cy5 (CGH 1). Reverse labeling (patient DNA with Cy5, and control DNA with Cy3) was also performed (CGH 2). EcoRI-digested genomic DNA was labeled with Cy5- or Cy3-dCTP by random prime labeling. Differently labeled DNA was combined with hybridization buffer (50% formamide, 10% dextran sulfate, 0.1% Tween 20, 2× SSC, 10 mmol L−1 Tris–HCl, pH 7.4). After prehybridization with herring sperm DNA and human CotI DNA using an in situ frame (Eppendorf, Hamburg, Germany) surrounding each block on a slide in a hybridization chamber (Genetix, New Milton, UK), labeled probe mixtures of CGH1 and CGH2 were simultaneously applied to blocks A and B, respectively. Slides were incubated at 37°C for 72 h with gentle shaking (5 rpm), and then washed once with solution A (1× PBS with 0.05% Tween 20), twice with solution B (2× SSC with 50% formamide) at 43°C for 15 min, and finally with solution A at room temperature for 10 min twice, with shaking, at room temperature.
Slides were scanned with GenePix 4000B (Axon Instruments, Union City, CA, USA) and analyzed with GenePix Pro 4.0 software (Axon Instruments). The subject-to-control DNA ratio for the microarray-CGH was calculated from data from a single-slide experiment, using the “ratio of means” formula. Average normalized inter-locus fluorescence ratio (ANILFR) was calculated for each CGH (Mantripragada et al. 2003). On the basis of results from a previous study, the normal ANILFR range was defined as average within ±2SD (Harada et al. 2004).
Results
Microarray CGH with Cy-3 labeled cffDNA from a 46,XX fetus and with Cy-5 labeled male control DNA revealed the high subject-to-control (Cy3-to-Cy-5) ratio for X-chromosome BAC clones and the markedly reduced ratio for Y-chromosome clones (Fig. 1a). The reverse test (Cy-5 labeled subject and Cy-3 labeled control) revealed the opposite hybridization pattern (Fig. 1b). These CGH patterns of the fetus well reflected her two X chromosomes and no Y chromosome. When signal intensities for the X and Y chromosome markers of cffDNA from a 46,XY male fetus were compared with those of the male control DNA, no significant difference was observed (Figs. 1c, d). Likewise, microarray CGH with cffDNA from two fetuses which were confirmed later to have trisomy 18 or trisomy 21 revealed the increased subject-to-control ratio for clones of chromosomes 18 and 21, respectively (data not shown). The CGH with cffDNA from a male fetus with a balanced translocation [45,XY,der(14;21)(q10;q10)mat] revealed no different signal intensity from a karyotypically normal male fetus (Fig. 1e).
Microarray-CGH data for female and male cffDNA from uncultured amniotic fluid obtained in the 15–17th gestational weeks, each hybridized separately to arrayed BAC-clones, together with reference DNA from a karyotypically normal adult male. a Cy-3-labeled female cffDNA (subject), and Cy-5-labeled male reference DNA (control). b Reverse-labeled female cffDNA and male reference DNA. Signal intensity for Y chromosomal clones was infinity, because the normal XX female fetus has no Y chromosome. c Cy-3-labeled male cffDNA and Cy-5-labeled male reference DNA. d Reverse-labeled male cffDNA and male reference DNA. e Cy-3-labeled cffDNA from a male fetus with balanced translocation [45,XY,der(14;21)(q10;q10)mat] and Cy-5-labeled male reference DNA. Vertical axis shows the CGH ratio (Cy-3/Cy-5) value at each locus, and horizontal axis (left to right) 50 BAC clones (ten clones on each chromosome) located to chromosome 13, 18, 21, X, and Y
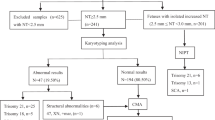
We also used the microarray-CGH method for diagnosis of six fetuses with congenital abnormalities that were detected by ultrasound examination at late gestation. A 40-year-old primigravida woman at 33 weeks’ gestation was referred to our hospital because of her fetus’s intrauterine growth retardation (IUGR), polyhydramnios, ventricular septal defect, and an enlarged cisterna magna. The woman also had a severe threatened premature labor and a tocolytic treatment was started. Decompression by amniocentesis was done at 34 weeks’ gestation to prevent premature labor, and targeted microarray CGH was performed with cffDNA from amniotic fluid. Because the subject-to-control ratio was increased only for all clones of chromosome 18, the ratio was normal for other autosomal clones (Fig. 2a), and XX patterns were apparent, the fetus was diagnosed to be a girl with trisomy 18. Her karyotype was later confirmed to be 47,XX,+18 by chromosome analysis in her cultured amniocytes. Likewise, two fetuses were successfully diagnosed by the microarray CGH to have trisomy 13 and trisomy 21, respectively, because their cffDNA revealed increased subject-to-control ratio for clones of chromosomes 13 and 21 (Figs. 2b, c). The cffDNA of another case had a decreased ratio for Y-chromosomal clones only and a normal ratio for X-chromosomal clones (Fig. 2d), compared with the ratios for a normal control male, indicating that the fetus had monosomy X. Karyotypes of all these three cases were confirmed later by chromosome analysis of their amniotic cells. The remaining two fetuses were diagnosed to be karyotypically normal by the targeted microarray-based CGH, the results being concordant with results from subsequent karyotyping (data not shown).
Microarray-CGH data for cffDNA from uncultured amniotic fluid in the 32–34th gestational weeks of fetuses with numerical chromosome aberrations, each hybridized separately to array clones, together with Cy-5-labeled normal male reference DNA. a–d Cy-3-labeled cffDNA from female fetuses with trisomy 18, trisomy 13, trisomy 21, and monosomy X, respectively. The vertical axis shows the CGH ratio (Cy3/Cy5) value for each locus and the horizontal axis shows ten clones each on chromosomes 13, 18, 21, X, and Y
Discussion
With the development of obstetric ultrasound examinations for a perinatal care, fetal anomalies are often found without the objective of diagnosis (Drummond et al. 2003; Yang et al. 2005). Most such findings do not suggest a specific chromosome region as a target for prenatal diagnosis. In the current microarray-CGH study with cffDNA from uncultured amniotic fluid, we successfully detected abnormal karyotypes in fetuses tested as little as 5 days after amniocentesis. Microarray CGH as a diagnostic tool for chromosome abnormalities has several advantages over conventional and/or FISH-based karyotyping. It enables rapid and comprehensive detection of copy-number changes (deletions or duplications) in the genome in a single experiment (Lapierre at al. 2000; Barrett et al. 2001; Oostlander et al. 2004). In addition, when cffDNA is used as a sample, cell culture is not required. Although inter-phase FISH and quantitative fluorescent PCR (QF-PCR) are also rapid prenatal diagnostic methods, they are applied to limited chromosomal regions at one time. However, BAC-based microarray CGH has some drawbacks. Because its resolving power depends on the number of clones printed and the genomic distance between the clones, a microdeletion or microduplication may be overlooked if the clones printed are less dense. Furthermore, microarray CGH cannot detect balanced rearrangements and diploid/tetraploid mosaics (Amiel et al. 2002; Oostlander et al. 2004). In fact, chromosome abnormalities we have successfully diagnosed were all copy-number changes, and a balanced translocation [45,XY,der(14;21)(q10;q10)] in one fetus could not be diagnosed by this method.
Although the supernatant of the amniotic fluid is usually discarded and ignored as a sample for prenatal chromosomal diagnosis, it contains cffDNA and can be used for genetic testing of the fetus. The reliability, validity, and utility of cffDNA for prenatal diagnosis were very similar to those of DNA isolated from cultured amniocytes from the same fetus (Larrabee et al. 2004). Because conventional karyotyping using amniocytes is still invaluable, microarray CGH-based molecular karyotyping with cffDNA should be run in parallel with conventional prenatal karyotyping.
In conclusion, the results of this study indicated that cffDNA in crude amniotic fluid can be used as a sample for microarray-CGH-based prenatal diagnosis of chromosome abnormality. Microarray-CGH with cffDNA enables rapid and comprehensive analysis of copy-number genome changes (Vermeesh et al. 2005). Because of drawbacks of the method, however, it should conducted in combination with conventional karyotyping. The cffDNA also occurs in the maternal circulation. If this technique is applied to cffDNA from the maternal plasma (Masuzaki et al. 2004), it will become a major non-invasive prenatal screening test for fetal chromosome abnormalities.
References
Amiel A, Bouaron N, Kidron D, Sharony R, Gaber E, Fejgin MD (2002) CGH in the detection of confined placental mosaicism (CPM) in placentas of abnormal pregnancies. Prenat Diagn 22:752–758
Barrett IJ, Lomax BL, Loukianova T, Tang SS, Lestou VS, Kalousek DK (2001) Comparative genomic hybridization: a new tool for reproductive pathology. Arch Pathol Lab Med 125:81–84
Bianchi DW (2000) Fetal cells in the mother: from genetic diagnosis to diseases associated with fetal cell microchimerism. Eur J Obstet Gynecol Reprod Biol 92:103–108
Bianchi DW, LeShane ES, Cowan JM (2001) Large amounts of cell-free fetal DNA are present in amniotic fluid. Clin Chem 47:1867–1869
Bianchi DW, Lo YM (2001) Fetomaternal cellular and plasma DNA trafficking: the Yin and the Yang. Ann NY Acad Sci 945:119–131
Drummond CL, Gomes DM, Senat MV, Audibert F, Dorion A, Ville Y (2003) Prenat. Diagn 23:1068–1072
Harada N, Hatchwell E, Okamoto N, Tsukahara M, Kurosawa K, Kawame H, Kondoh T, Ohashi H, Tsukino R, Kondoh Y, Shimokawa O, Ida T, Nagai T, Fukushima Y, Yoshiura K, Niikawa N, Matsumoto N (2004) Subtelomere specific microarray based comparative genomic hybridisation: a rapid detection system for cryptic rearrangements in idiopathic mental retardation. J Med Genet 41:130–136
Hahn S, Huppertz B, Holzgreve W (2005) Fetal cells and cell free fetal nucleic acids in maternal blood: new tools to study abnormal placentation? Placenta 26:515–526
Lapierre JM, Cacheux V, Luton D, Collot N, Oury JF, Aurias A, Tachdjian G (2000) Analysis of uncultured amniocytes by comparative genomic hybridization: a prospective prenatal study. Prenat Diagn 20:123–131
Larrabee PB, Johnson KL, Pestova E, Lucas M, Wilber K, LeShane ES, Tantravahi U, Cowan JM, Bianchi DW (2004) Microarray analysis of cell-free fetal DNA in amniotic fluid: a prenatal molecular karyotype. Am J Hum Genet 75:485–491
Lau TK, Leung TN (2005) Genetic screening and diagnosis. Curr Opin Obstet Gynecol 17:163–169
Lo YM (2005) Recent advances in fetal nucleic acids in maternal plasma. J Histochem Cytochem 53:293–296
Mantripragada KK, Buckley PG, Benetkiewicz M, de Bustos C, Hirvela C, Jarbo C, Bruder CEG, Wensman H, Mathiesen T, Nyberg G, Papi L, Collins VP, Ichimura K, Evans G, Dumanski JP (2003) High-resolution profiling of an 11 Mb segment of human chromosome 22 in sporadic schwannoma using array-CGH. Inter J Oncol 22:615–622
Masuzaki H, Miura K, Yoshimura S, Yoshiura K, Ishimaru T (2004) Detection of cell free placental DNA in maternal plasma: direct evidence from three cases of confined placental mosaicism. J Med Genet 41:289–292
Miyake N, Shimokawa O, Harada N, Sosonkina N, Okubo A, Kawara H, Okamoto N, Kurosawa K, Kawame H, Iwakoshi M, Kosho T, Fukushima Y, Makita Y, Yokoyama Y, Yamagata T, Kato M, Hiraki Y, Nomura M, Yoshiura K, Kishino T, Ohta T, Mizuguchi T, Niikawa N, Matsumoto N (2006) BAC array CGH reveals genomic aberrations in idiopathic mental retardation. Am J Med Genet 140:205–211
Nyberg DA, Souter VL (2000) Sonographic markers of fetal aneuploidy. Clin Perinatol 27:761–789
Oostlander AE, Meijer GA, Ylstra B (2004) Microarray-based comparative genomic hybridization and its applications in human genetics. Clin Genet 66:488–495
Pollack JR, Perou CM, Alizadeh AA, Eisen MB, Pergamenschikov A, Williams CF, Jeffrey SS, Botstein D, Brown PO (1999) Genome-wide analysis of DNA copy-number changes using cDNA microarrays. Nat Genet 23:41–46
Telenius H, Carter NP, Bebb CE, Nordenskjold M, Ponder BA, Tunnacliffe A (1992) Degenerate oligonucleotide-primed PCR: general amplification of target DNA by a single degenerate primer. Genomics 13:718–725
Vermeesch JR, Melotte C, Froyen G, Van Vooren S, Dutta B, Maas N, Vermeulen S, Menten B, Speleman F, De Moor B, Van Hummelen P, Marynen P, Fryns JP, Devriendt K (2005) Molecular karyotyping: array CGH quality criteria for constitutional genetic diagnosis. J Histochem Cytochem 53:413–422
Wataganara T, Bianchi DW (2004) Fetal cell-free nucleic acids in the maternal circulation: new clinical applications. Ann NY Acad Sci 1022:90–99
Yang JH, Chung JH, Shin JS, Choi JS, Ryu HM, Kim MY (2005) Prenatal diagnosis of trisomy 18: report of 30 cases. Prenat Diagn 25:119–122
Acknowledgments
We thank Dr Joseph Wagstaff for his help and valuable advice. K.M., H.M., N.M., and N.N. were supported in part by Grants-in-Aid for Scientific Research (Nos. 16591670, 17591748, 16390101, and 13854024, respectively) from the Ministry of Education, Sports, Culture, Science and Technology of Japan, and N.N. was supported by SORST from Japan Science and Technology Agency (JST).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miura, S., Miura, K., Masuzaki, H. et al. Microarray comparative genomic hybridization (CGH)-based prenatal diagnosis for chromosome abnormalities using cell-free fetal DNA in amniotic fluid. J Hum Genet 51, 412–417 (2006). https://doi.org/10.1007/s10038-006-0376-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10038-006-0376-7
Keywords
This article is cited by
-
Noninvasive fetal trisomy detection by multiplexed semiconductor sequencing: a barcoding analysis strategy
Journal of Human Genetics (2016)
-
Mosaic pregnancy after transfer of a “euploid” blastocyst screened by DNA microarray
Journal of Ovarian Research (2013)
-
Proteomic profile determination of autosomal aneuploidies by mass spectrometry on amniotic fluids
Proteome Science (2008)
-
Guidelines for molecular karyotyping in constitutional genetic diagnosis
European Journal of Human Genetics (2007)
-
Identification of origin of unknown derivative chromosomes by array-based comparative genomic hybridization using pre- and postnatal clinical samples
Journal of Human Genetics (2007)