Abstract
Effective management of breast cancer depends on early diagnosis and proper monitoring of patients’ response to therapy. However, these goals are difficult to achieve because of the lack of sensitive and specific biomarkers for early detection and for disease monitoring. Accumulating evidence in the past several years has highlighted the potential use of peripheral blood circulating nucleic acids such as DNA, mRNA and micro (mi)RNA in breast cancer diagnosis, prognosis and for monitoring response to anticancer therapy. Among these, circulating miRNA is increasingly recognized as a promising biomarker, given the ease with which miRNAs can be isolated and their structural stability under different conditions of sample processing and isolation. In this review, we provide current state-of-the-art of miRNA biogenesis, function and discuss the advantages, limitations, as well as pitfalls of using circulating miRNAs as diagnostic, prognostic or predictive biomarkers in breast cancer management.
Similar content being viewed by others
Facts
-
Micro (mi)RNAs are small RNA species whose expression is often dysregulated in cancer.
-
MiRNAs are present in the circulation of cancer patients and can potentially be used for disease monitoring.
-
Large proportion of circulating miRNAs in cancer patients do not originate from tumors but rather reflect the body’s homeostatic response.
Open Questions
-
Are circulating miRNAs disease specific?
-
What is the best approach for sample processing and detection of circulating miRNAs in breast cancer patients?
-
What is the best normalization approach when quantifying circulating miRNAs?
Breast cancer is one of the most common malignant diseases in the world, with an estimated 1.5 million new cases per year.1 The incidence has been decreasing in the developed world;2 however, it remains a common cause of death in the USA and UK; Caucasian women have an estimated lifetime risk of 1 in 9.3
There are numerous risk factors for breast cancer, including age, family history, obesity and exposure to hormones and therapeutic radiation.4 Models used to estimate breast cancer risk vary depending on population characteristics; however, with the exception of hormone prophylaxis, such models are not suitable for individual patient management. The two most common types of breast cancer are ductal and lobular carcinoma. An important issue for treatment is selecting the right therapeutic modality, which is largely dependent on disease subtype. Breast cancer is currently molecularly classified based on expression of sex hormone receptors and human epidermal growth factor receptor (HER)2, which can determine diagnostic approach and treatment choice.5 However, other methods of classification that are based on global gene expression are gaining momentum.6 Molecular data – for instance, from oncotype DX breast cancer assays in lymph node-negative breast cancer – have increased our understanding of the mechanisms of chemotherapy and hormone resistance, such as the role of mutations in estrogen receptor (ER)1 in resistance to endocrine therapy.7
Micro (mi)RNAs
MiRNAs are short, single-stranded RNA sequences (usually 19–23 nucleotides (nts)) derived from ~70-nt precursors that control gene expression in a variety of physiological and developmental processes, thus having a critical role in post-transcriptional regulation of gene expression in a broad range of biological systems.8, 9, 10, 11 In humans, a single miRNA has several dozens or even hundreds of mRNA targets. Over 60% of human protein-coding genes are predicted to contain miRNA-binding sites in their 3′-untranslated region (3′-UTR).12 According to the miRBase database (www.mirbase.org), there are >2500 mature miRNA sequences in the human genome.13, 14 MiRNAs mediate the repression of target mRNAs by base paring to complementary sequences in the 3′-UTR, causing transcript destabilization, translational repression or both15 (Figure 1). Recent studies have reported that miRNAs also modulate gene expression by binding to other regions, including protein-coding exons,16, 17, 18 and can even induce gene expression in mammalian cells.19
Schema depicting miRNA biogenesis and function. Primary miRNA transcript (pri-miRNA) is transcribed by RNA polymerase II/III in the nucleus, forming an elongated RNA hairpin structure that is subsequently cleaved by Drosha into a small stem-loop structure of ~70 nt, (pre-miRNA). Pre-miRNA is exported from the nucleus into the cytoplasm by exportin-5 and the loop is cleaved after the pre-miRNA is loaded onto Dicer, producing a double-stranded structure of miRNA and antisense miRNA*. The latter is typically degraded, whereas the long (~22 nt) mature miRNA strand is incorporated into the miRNA-induced silencing complex (mRISC), leading to mRNA degradation or translational repression. Mature miRNA levels are regulated via binding to ceRNAs such circular (c)RNAs, pseudogenes, and lncRNAs, which act as a sponge to prevent miRNA binding to target mRNAs
MiRNA Biogenesis and Maturation
The biogenesis of mature miRNA involves a series of biological processes (Figure 1), for review see Winter et al.20 A primary miRNA transcript (pri-miRNA) is first transcribed in the nucleus by RNA polymerase II (or sometime by RNA polymerase III), which is subsequently cleaved by Drosha into a 70-nt known as precursor miRNA (pre-miRNA).21, 22, 23 The pre-miRNA is exported from the nucleus to the cytoplasm by exportin-524, 25 and loaded onto Dicer; the loop is then cleaved, producing a double-stranded structure composed of miRNA and antisense miRNA*.26 The latter is usually degraded, whereas the long (~22 nt) mature miRNA strand is incorporated into the miRNA-induced silencing complex,27, 28 leading to gene silencing via mRNA cleavage or translational repression depending on the degree of complementarity between the miRNA and target mRNA transcript29, 30, 31, 32 (Figure 1). It was recently reported that miRNAs can switch from translational repression to induction.19
Regulation of miRNAs by Competing Endogenous (ce)RNAs
Although miRNAs exert their functions via direct binding to miRNA response elements (MREs) in target mRNAs, they are themselves subject to regulation when they bind to MRE-containing non-coding RNA transcripts, known as ceRNAs (Figure 1). Pseudogenes mostly originate from gene duplication and mutation and therefore lack the ability to produce functional protein.33 One class of pseudogenes is generated via mRNA retrotransposition (processed pseudogenes);34 for example, phosphatase and tensin homolog pseudogene (PTENP)1 contains many of the 3′-UTR MREs sites found in PTEN and is frequently lost in human cancer. PTENP1 was found to regulate PTEN levels by sequestering its regulatory miRNAs, including miR-19b and miR-20a.35
Long non-coding (lnc)RNAs are a class of RNA molecules that are longer than 200 nts. Although several lncRNAs, including X-inactive specific transcript and H19, were described decades ago, their role in gene regulation has only recently become known. For instance, the lncRNA homeobox (HOX) transcript antisense RNA (HOTAIR) was shown to interact with polycomb repressive complex 2, which is required to suppress HOXD gene expression.36 In addition, lncRNAs can function as decoys to sequester miRNAs and prevent their binding to target transcripts; for example, HOTAIR was found to regulate the expression of HER2 by acting as a miR-331-3p sponge in gastric cancer.37
Circular (circ)RNAs are ceRNAs generated via direct ligation of 5′ and 3′ ends of linear RNA as an intermediate during RNA splicing.38 CircRNAs are more stable than the linear molecule and may therefore be more efficient miRNA sponges (Figure 1). For example, ciRS-7 and sex-determining region Y act as sponges for miR-7 in neurons and miR-138 in testicular tissue.39
Methods for Detecting Circulating miRNAs
Accurate quantification of circulating miRNAs in body fluids poses a number of challenges because of their low abundance and small size. However, various tools have recently been developed that overcome these obstacles, with each having advantages and limitations (Table 1). Quantitative reverse transcriptase real-time (qRT-)PCR is a widely used and highly sensitive method that requires only small amounts of input RNA.40 A major limitation of qRT-PCR is that it is oftentimes used to quantify the levels of a defined set of miRNAs (usually <700); as such, it cannot be used for high-throughput profiling. Microarray platforms are an alternative method for detecting circulating miRNA. The advantage of this method is the ability to simultaneously detect large numbers of circulating miRNAs;41 disadvantages include a low dynamic range and inability to detect novel (i.e., unannotated) miRNA species. Next-generation sequencing is another technology for detecting circulating miRNAs based on deep sequencing.42 This method has the advantage of being able to detect both annotated and unannotated miRNAs, although it requires large amounts of starting material and generates copious amounts of data that must be analyzed using complex bioinformatics tools. Direct quantification of circulating miRNAs in bodily fluids has become possible using the NanoString nCounter platform,43 which is based on a novel digital molecular barcoding technology that enables quantification of the exact copy number of miRNA species in a biological sample.44 However, a major limitation of this platform is that it currently can only detect up to 800 human miRNAs per slide. Given the strengths and shortcomings of each platform, selecting the appropriate one will largely depend on the available resources, type of sample, and the question being addressed.
Sample Selection and Processing
Levels of circulating miRNAs are influenced by sample type and RNA extraction method. Serum and plasma are the most commonly used sample types for circulating miRNA detection. Hemolysis can affect the abundance of circulating miRNAs;45, 46 therefore, samples with obvious hemolysis should be routinely excluded from miRNA profiling studies.41 We have found serum to be a better sample choice for circulating miRNA studies as it is less prone to hemolysis than plasma. In addition, as miRNAs usually exist in the circulation bound to other proteins or in apoptotic bodies or exosomes, it is important to choose an RNA isolation method that will extract all miRNAs present in the desired biological fraction, such as TRIzol reagent or column-based techniques.
Role of miRNAs in Breast Cancer
Dysregulation of miRNAs is linked to many human diseases including myocardial infarction and cardiovascular diseases,47, 48 diabetes, obesity49, 50, 51 and cancer.52 Various mechanisms such as DNA amplification, deletion and mutations relating to miRNA loci, epigenetic silencing or inhibition of specific miRNA processing can lead to altered miRNA expression in human cancers53 In this section, we describe the best-known examples of breast cancer-associated miRNAs, focusing on their involvement in various aspects of breast cancer (Figure 2).
Transcriptome–miRNA interaction networks in breast cancer. Schematic representation of the interaction of commonly altered miRNAs in breast cancer and their identified mRNA targets regulating EMT/metastasis, stemness, growth and survival of breast cancer cells. ↑ indicated miRNA or gene is upregulated, whereas (↓) indicate miRNA or gene is downregulated in BC tissue. Yellow filled miRNA ovals indicate miRNAs whose expression is also altered in the circulation based on current review. RHOC, Ras homolog family member C; HOXD10, homeobox D 10; KLF4, Kruppel-like factor 4; PDCD4, programmed cell death 4; SOX4, SRY (sex-determining region Y)-box 4; TNC, Tenascin-C; FHOD1, Formin homology 2 domain containing 1; PPM1F, protein phosphatase, Mg2+/Mn2+ Dependent 1F; ZEB1, zinc-finger E-box binding homeobox 1; ZEB2, zinc-finger E-box binding homeobox 2; VEGFA, vascular endothelial growth factor A; LIN28B, Lin-28 homolog B; RAS, RAS viral oncogene homolog; HMGA2, high mobility group AT-Hook 2; BMI1, BMI1 proto-oncogene, polycomb ring finger; ID4, inhibitor of DNA binding 4, HLH protein; PTEN, phosphatase and tensin homolog; BRCA1, BRCA1, DNA repair associated; BCL2, BCL2, apoptosis regulator; SIRT1, sirtuin 1; ERBB3, Erb-B2 receptor tyrosine kinase 3
In humans, let-7 is overexpressed in differentiated epithelial tissues and is oftentimes downregulated during tumorogenesis; it is known to target LIN28 mRNA and is itself a target of negative feedback regulation by LIN28.44, 52 LIN28 protein expression is upregulated in many tumors, including breast cancer.54 Let-7 was found to regulate breast cancer tumor-initiating cells (T-IC) through targeting HRAS and HMGA2.55 The miR-200 family is recognized as having a tumor-suppressor role. The family consists of five members organized as two clusters – cluster I (miR-200b/200a/429) and cluster II (miR-200c/141) on chromosomes 1 and 12, respectively,56 which are suppressed during epithelial-to-mesenchymal transition (EMT), an initiating step in metastasis that is associated with increased breast cancer cell motility and invasiveness.57, 58 MiR-200 family members were found to regulate BMI1 expression in breast cancer T-IC and suppress EMT by inhibiting zinc-finger E-box binding homeobox (ZEB)1 and ZEB2.59, 60 These findings were supported by another study showing that modulation of miR-200c in breast cancer cells affects cell migration and invasion.61 In addition, miR-200c regulates transforming growth factor β-induced stress fiber formation independently of the ZEB/E–cadherin axis by targeting the actin-regulatory proteins formin homology 2 domain containing (FHOD)1 and protein phosphatase, Mg2+/Mn2+-dependent (PPM)1F.61 MiR-10b was first discovered as an oncogenic miRNA in metastatic breast cancer cell lines;62 miR-10b level has been linked to malignancy in advanced-stage cancer of various types. Its expression was also upregulated in metastatic as compared with matched primary tumors.63 MiR-10b directly targets the HOXD10 and Krüppel-like factor 4 genes.62, 64 MiR-21 is an oncogenic miRNA that inhibits several tumor-suppressor genes and thus promotes cell growth and invasion and tumor metastasis. MiR-21 is one of the most highly expressed miRNAs in breast cancer, and its upregulation is associated with tumor progression and poor prognosis.65, 66 MiR-21 has several targets including tropomyosin 1α and programmed cell death (PDCD)4.66, 67 MiR-21 also targets PTEN68 to promote MCF-7 breast cancer cell growth,69 as well as the tumor suppressors acidic nuclear phosphoprotein 32 family member A and SWI/SNF-related matrix-associated actin-dependent regulator of chromatin subfamily A member 4.70 MiR-335, which is oftentimes silences in breast cancer, inhibits metastasis by targeting the transcription factor Sry-box 4 and extracellular matrix protein tenascin-C.71, 72 The tumor-suppressor function of miR-335 involves reducing cell viability and promoting apoptosis by simultaneously regulating the BRCA1 activators insulin-like growth factor 1, ER-α, and specificity protein 1 and the repressor inhibitor of differentiation 4.73 MiR-301 acts as an oncomiR in breast cancer via regulation of forkhead box F2, B-cell lymphoma 2-binding component 3, PTEN and collagen 2A1.74
MiR-155 is another oncogenic miRNA that regulates multiple signaling pathways related to cell growth and survival;75 it is known to target BRCA1, a human breast cancer susceptibility gene76, 77 that is involved in DNA repair and cell cycle progression. Other genes associated with breast cancer progression such as suppressor of cytokine signaling 1 and forkhead box O3a are negatively regulated by miR-155.78 MiR-34a is oftentimes downregulated in breast cancer, which promotes breast cancer growth and survival through upregulation of SIRT1 and BCL2 proteins.79, 80 miR-205 is frequently downregulated in metastatic breast cancer. Loss of miR-205 promoted breast cancer cell growth and invasion through upregulation of Erb-B2 receptor tyrosine kinase 3, vascular endothelial growth factor A, ZEB1 and ZEB2 proteins.81, 82, 83
Circulating miRNAs as Disease Biomarkers
Cell-free circulating miRNAs usually exist bound to ribonucleoprotein complexes or high-density lipoprotein or they are released from cells in lipid vesicles, microvesicles, exosomes or apoptotic bodies (Figure 3).84, 85, 86, 87 Lipid vesicles and exosomes have critical roles in cell–cell communication.87, 88 Thus, circulating miRNAs may reflect homeostatic response of the organism, as well as signs of disease progression. Circulating miRNAs have been detected in the peripheral blood circulation and other body fluids.89, 90, 91 Owing to their stability and resistance to endogenous RNase activity, these miRNAs have been proposed as diagnostic and prognostic biomarkers for diseases, such as cancer, diabetes mellitus and neurological disorders.92, 93, 94, 95 Table 2 summarizes the frequently upregulated circulating miRNAs in human cancers. Elevated levels of miR-21 and -210 in the serum have been reported in patients with diffuse large B-cell lymphoma; the former is associated with relapse-free survival.96 Increased serum levels of various miRNAs have been linked to different human cancers – for instance, miR-141 in prostate cancer;91 miR-25 and miR-223 in lung cancer;89 miR-21, miR-92, miR-93, miR-126 and miR-29a in ovarian cancer;97 miR-92 and miR-17-3p in colorectal cancer;98 miR-92a in acute leukemia;99 miR-210, miR-21, miR-155 and miR-196a in pancreatic cancer;100, 101 miR-184 in squamous cell carcinoma of the tongue;102 and miR-500 in hepatocellular carcinoma.103
Sources and forms of circulating miRNAs. MiRNAs can be released via an active process in the form of exosomes (<100 nM) through the course of exocytosis (a process that involves fusion of the multivesicular body (MVBs) with the plasma membrane) or as microvesicles (100–1000 nM, through outward budding from the plasma membrane). Alternatively, miRNAs can be released as a result of necrosis or apoptosis (programmed cell death). Cell-free circulating miRNAs usually exist bound to ribonucleoprotein complexes (such as Argonaute-2), or high-density lipoprotein (HDL). Circulating miRNAs are also found within lipid microvesicles and exosomes
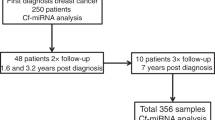
A large number of studies have reported the usefulness of miRNAs as diagnostic, prognostic, or predictive biomarkers for breast cancer. Table 3 list characteristics of the studies including number of patients included, verification of miRNAs identified using alternative methods and confirmation of the findings in an independent cohort of patients. As seen in Table 3, studies varied in their quality based on these quality criteria. In the following sections, we will discuss how circulating miRNAs have been used in the context of breast cancer biology as diagnostic, prognostic and predictive biomarkers.
Circulating miRNAs as diagnostic biomarkers
Heneghan and colleagues104 assessed the diagnosis potential of a panel of seven cancer-associated miRNAs in the circulation of patients with various cancer types. The authors found that let-7a and miR-10b and -155 levels were upregulated in the majority of cancer patients, whereas circulating miR-195 level distinguished those with breast cancer from other cancer types and from normal control with a sensitivity of 88% and a specificity of 91%. The sensitivity was further increased to 94% when using a combination of circulating levels of miR-195, let-7a and miR-155. Another study explored the diagnostic potential of a panel of circulating miRNAs targeting PTEN tumor suppressor using qRT-PCR in a cohort of breast cancer patients. The preoperative levels of circulating miR-20a and -21 were higher in patients with breast cancer and benign disease compared with healthy controls, whereas levels of circulating miR-214 were able to discriminate between malignant and benign tumors and healthy subjects.105 Cuk et al.106 explored the diagnostic potential of a seven circulating miRNA panel (miR-127-3p, miR-148b, miR-376a, miR-376c, miR-409-3p, miR-652 and miR-801) in two cohorts of breast cancer patients. The authors observed elevated levels of these miRNAs in the circulation from breast cancer patients. MiR-127-3p, miR-148b, miR-409-3p, miR-652 and miR-801 were detected in breast cancer stages I and II, suggesting that they can be used for early diagnosis. In another study, miRNA expression profiling using plasma samples from breast cancer patients and healthy controls revealed 43 miRNAs that were differentially expressed between the two groups, with patients exhibiting higher miR-148b, miR-133a and miR-409-3p levels. miR-148b and miR-133a were also detected in breast cancer cell lines, suggesting their tumor origin.107 A recent study performed global profiling of circulation miRNA in patients with ER-positive early-stage breast cancer and age-matched healthy controls. The authors identified a panel of nine miRNAs (miR-15a, miR-18a, miR-107, miR-133a, miR-139-5p, miR-143, miR-145, miR-365 and miR-425) that can discriminate between patients with breast cancer and healthy controls. This panel was subsequently validated in a second cohort of patients with early-stage breast cancer.108 A study using the Taqman low-density array platform comparing patients with early breast cancer and healthy controls found that circulating miR-484 level was higher in patients with breast cancer, which was validated in a second cohort of patients with early-stage breast cancer.109 Although several of the aforementioned studies included a modest number of patients, Shimomura et al.110 conducted microarray expression profiling using sera from a cohort of 1280 patients with breast cancer, 2836 controls, 451 from patients with other cancer types and 63 from patients with non-breast benign diseases. The authors divided the samples into training and validation cohorts and identified a panel of five miRNAs (miR-1246, miR-1307-3p, miR-4634, miR-6861-5p and miR-6875-5p) that discriminated between patients with breast cancer and those with other cancer types and controls. In another study, serum miR-155, miR-19a, miR-181b and miR-24 levels were elevated in patients with early-stage breast cancer relative to healthy subjects at the time of diagnosis, and were higher in high-risk as compared with low-risk patients. Interestingly, miR-155, miR-181b and miR-24 expression declined after surgical resection whereas that of miR-19a decreased post-therapy.111
However, one limitation of the above-mentioned studies is that the origin of detected circulating miRNAs has not been verified and in particular, the contribution of breast cancer tissue to the identified circulating miRNAs is not known. A number of studies examined the association between the expression of selected miRNA panels in breast cancer tissues and their correlation with circulating miRNAs. For instance, global profiling of miRNA expression in breast cancer tumor tissue, normal tissue and serum samples obtained from patients and from healthy controls revealed significant deregulation in the expression level of several miRNAs in both tissue and circulation. In particular, miR-1, miR-92a, miR-133a and miR-133b were the most prominently upregulated diagnostic markers in breast cancer sera, which was subsequently validated in an independent cohort of patients with breast cancer.112 Matamala et al.113 performed global miRNA expression profiling using paraffin-embedded tissue from patients with breast cancer and samples from healthy controls; in two independent cohorts of breast cancer versus control, they identified and validated four miRNAs (miR-505-5p, miR-125b-5p, miR-21-5p and miR-96-5p) that were significantly overexpressed in tissue and circulation of pretreated patients with breast cancer. In another study, Li et al.114 assessed the expression of Let-7c in breast cancer tissue compared with adjacent para-carcinoma control tissue. The authors reported significant downregulation in Let-7c in breast cancer. The tissue findings were subsequently verified using sera of patients with breast cancer that revealed lower levels of let-7c compared with serum levels in healthy controls. Wang et al.115 assessed the diagnostic potential of circulating miR-182 in breast cancer patients. High serum levels of circulating miR-182 measured by qRT-PCR were detected in breast cancer patients as compared with healthy controls and miR-182 was also overexpressed in breast cancer tissue, suggesting that it is potential use as a diagnostic biomarker. Although in the above-mentioned studies a good concordance was observed in miRNAs profile detected in breast cancer tumor tissue and in the circulation, some studies suggested a non-tumor origin of circulating miRNAs. Waters and colleagues116 used a murine model of breast cancer to assess changes in circulating miRNA expression during tumor progression. Of particular interest, circulating miR-138 was upregulated in the murine xenograft model of breast cancer, whose upregulated expression was subsequently validated in the sera from patients with breast cancer. Interestingly, the authors did not observe any change in miR-138 levels in breast cancer tissues itself.
miRNA expression profiling of breast cancer tissue revealed that several miRNAs exhibited expression pattern associated with breast cancer molecular subtype, ER status or other pathological features.117, 118 Therefore, a number of studies assessed potential utilization of circulating miRNAs in breast cancer disease stratification. In one study, Zhu et al.119 assessed the expression of circulating miR-16, miR-145 and miR-155 in a cohort of breast cancer patients compared with those in healthy controls. Although there was no difference in the expression of this miRNA panel in breast cancer, miR-155 was found to be highly expressed in progesterone (PR)-positive patients. Wang and colleagues120 correlated the expression of selected panel of miRNAs in breast cancer tissues and matched serum samples. The authors observed miR-21, miR-106a and miR-155 levels to be elevated, whereas those of miR-126, miR-199a and miR-335 to be reduced in tumor specimens relative to normal tissue. Interestingly, circulating levels of miR-21, miR-126, miR-155, miR-199a and miR-335 were associated with histological tumor grade and sex hormone receptor expression. Recently our group isolated and performed an enrichment step before global expression profiling of circuiting miRNAs in breast cancer patients compared with normal controls. We identified a novel panel of nine circulating miRNAs (miR-4270, miR-1225-5p, miR-188-5p, miR-1202, miR-4281, miR-1207-5p, miR-642b-3p, miR-1290 and miR-3141) that was upregulated in patients with breast cancer, and whose expression was correlated with cancer stage and molecular subtype.41
Circulating miRNAs as prognostic biomarkers
Circulating miRNAs can also serve as prognostic biomarkers in breast cancer patients (Table 3). A prognostic biomarker should indicate patient’s outcome, for example, disease recurrence or disease progression, independent of treatment received. In one study, serum levels of melanoma-associated antigen-A1, -A2, -A3 and -A12 and CCCTC-binding factor-like mRNA, as well as that of let-7b were higher in patients with invasive breast cancer compared with those with non-invasive tumors, benign breast disease or healthy controls. In this study, miR-202 overexpression was positively correlated with reduced overall survival.121 In another study, Mangolini and colleagues122 used droplet digital PCR to assess the prognostic value of a five circulating miRNA (miR-10b-5p, miR-145-5p, miR-148b-3p, miR-425-5p and miR-652-3p) panel chosen based on prior circulating miRNA expression profiling study. The authors reported that serum levels of miR-148b-3p and miR-652-3p were lower, whereas higher expression of miR-10b-5p correlated with poor prognosis in two cohorts of breast cancer patients. A recent study investigated the prognostic value of circulating miRNAs in patients with primary triple-negative breast cancer (TNBC). The authors conducted genome-wide miRNA expression profiling using serum from TNBC patients, which revealed a four-miRNA signature (miR-18b, miR-103, miR-107 and miR-652) that could predict tumor relapse and overall survival.123
Several studies has also investigated the potential correlation between miRNA profile expression in the circulation and in breast cancer metastastic tissue and their possible use to diagnose generalized metastatic disease. Based on the observation that miR-10b and miR-373 are overexpressed in breast cancer lymph node metastases, circulating levels of miR-10b and miR-373 were assessed in the sera for their potential utilization as biomarker for detecting breast cancer lymph node metastases. The authors reported higher levels of miR-10b and miR-373 in plasma from preoperative breast cancer patients with lymph node metastasis compared with patients without metastasis and normal controls.124 In another study, serum levels of four breast cancer-associated miRNAs (miR-10b, miR-34a, mi-R141 and miR-155) were measured in patients with primary or metastatic breast cancer, and healthy controls using qRT-PCR. Increased expression of circulating miR-34a was correlated with tumor stage, whereas upregulation of miR-10b, miR-34a and miR-155 was associated with the presence of metastases.125 Shaker et al.126 assessed the expression of four miRNAs in the sera of female patients with breast cancer and healthy controls and reported increased levels of miR-29b-2, miR-155, miR-197 and miR-205 in patients with breast cancer and the levels of these miRNAs correlated with tumor grade (T3 versus T2) and the presence of lymph node metastases (N3 versus N2), whereas expression of only miR-155 and miR-205 correlated with the presence of distant metastases. miRNA expression profiling performed on breast cancer tissue, serum samples from patients with early-stage breast cancer and healthy controls revealed that the level of miR-92a was reduced whereas that of miR-21 was increased in the tissue and serum of patients with early-stage breast cancer relative to controls. Furthermore, serum miR-92a and -21 levels were correlated with tumor size and the presence of lymph node metastases.127 In addition, miRNA profiling of recurrent, non-recurrent and healthy controls identified 22 miRNAs, which were subsequently validated in an independent cohort of non-recurrent and recurrent breast cancer patients’ sera. Upregulation of miR-21-5p, miR-375, miR-205-5p and miR-194-5p and downregulation of miR-382-5p, miR-376c-3p and miR-411-5p have been linked to breast cancer recurrence.128 Another study has reported an association between the expression of cell-free exosomal miRNAs circulating in serum and the molecular subtypes of breast cancer. The authors measured the expression levels of six circulating miRNAs (miR-10b, miR-17, miR-34a, miR-93, miR-155 and miR-373) in the sera of patients with primary (M0), and metastatic (M1) breast cancer and those of healthy controls. The authors observed significant differences in the expression levels of circulating miR-34a, miR-93 and miR-373 between the patients with M0 breast cancer and healthy controls, whereas the levels of miR-17 and miR-155 were significantly higher in the M0 compared with those in the M1 group. Elevated levels of miR-373 were associated with HER2-negative status of the primary tumor, whereas levels of miR-17 and miR-34a correlated with PR or ER status.129
Circulating miRNAs as predictive biomarkers
Only few studies have investigated the value of circulating miRNAs in breast cancer patients as predictive biomarkers for treatment response. In one study, expression of four breast cancer-associated miRNAs (miR-10b, miR-34a, miR-125b and miR-155) was profiled in the sera from breast cancer patients with invasive ductal carcinoma and preoperative neoadjuvant chemotherapy before treatment and normal controls. Among the studied miRNAs, only miR-125b exhibited higher expression level in non-responder breast cancer patients suggesting possible correlation between miR-125b expression in the circulation and breast cancer chemotherapeutic resistance.130 In an independent study, Wu and colleagues42 performed deep sequencing of circulating miRNAs on pre-treatment sera obtained from a cohort of stages II–III locally advanced breast cancer patients who received neoadjuvant chemotherapy followed by surgical resection of the tumor. The authors observed that reduced level of miR-375 and elevated levels of miR-122 were able to discriminate between relapsed and non-relapsed patients, whereas elevated levels of miR-375, miR-184, miR-1299 and miR-196a and reduced levels of miR-381, miR-410 and miR-1246 were observed in good responder to neoadjuvant chemotherapy. The authors subsequently validated miR-122 in a second cohort of stages II–III BC patients and demonstrated significant association between elevated expression of circulating miR-122 and patient relapse, suggesting potential utilization of miR-122 and miR-375 in predicting response to chemotherapy in BC patients and relapse. Sun and colleagues131 used qRT-PCR to assess the expression of miR-155 in the sera from breast cancer patients compared with healthy individuals and reported elevated circulating levels of miR-155 in breast cancer. Interestingly, the levels of miR-155 in the serum decreased after surgery and four cycles of chemotherapy suggesting potential utilization of miR-155 as an indicator for treatment response.
Limitations of Using miRNAs as Breast Cancer Biomarkers
The establishment of an accurate and reliable panel of circulating miRNAs for breast cancer diagnosis, prognosis and prediction of treatment response, is challenging at nearly every step from sample collection and processing to data analysis.132 A major limitation to using circulating miRNAs as biomarkers is their low abundance, which hampers their detection using standard miRNA profiling techniques such as microarrays. Modified approaches have been proposed as a solution: for example, we recently developed a new strategy that relies on miRNA isolation and enrichment before global expression profiling.41 Another important issue is sample selection and processing. The majority of studies use serum, or plasma. We found that serum is a better choice to avoid drawbacks of excluding a large number of samples because of the presence of hemolysis. Notably, circulating miRNA levels are higher in serum than in plasma, implying potential interference by platelet and white blood cell during sample preparation.133 It is therefore important to use the same type of material (for patients and controls), avoid samples showing signs of hemolysis and use a standardized protocol of sample collect and processing. Patient selection and classification is a critical issue for clinical studies. A number of studies have reported fluctuations in circulating miRNA levels in response to chemotherapy.134, 135, 136 To eliminate this problem, patients’ treatment regimen must be considered, or else blood samples must be collected before chemotherapy. Another important factor is the choice of platform for measurement of miRNA level. It is clear that the majority of studies listed in Table 3 are qRT-PCR-based. Although this method is more sensitive and less costly than others, a major limitation is the inability to detect novel miRNAs; indeed, most studies used a pre-existing circulating miRNA panel or screened for miRNAs that have been detected in tissue. Finally, there is a lack of reliable housekeeping circulating miRNAs for normalization of expression levels, which can change with physiological and pathological status. As such, other approaches for normalization have been used, such as using equal amounts of starting material (serum or plasma)41 or a synthetic spike-in control, which was found to be more reliable than endogenous miRNAs for data normalization.137
As observed in the above appraisal of the published studies, there is a minimal overlap in the identified miRNA panels among different studies, which reflects a complex biology of miRNA expression in BC patient’s circulation. Breast cancer is a heterogeneous group of diseases with diverse biological behaviors that correspond to heterogeneous cancer tissue structure and gene expression profile. The discrepancy in the identified circulating miRNA signatures reported by different groups, may be caused by the heterogeneity of the disease and its clinical presentation. The variability may also be caused by the significant contribution of many tissues to the circulating miRNAs. Circulating exosomes and microvesicles are carrier of miRNAs in the circulation and their content and biological functions are dependent on their cell of origin;138 a potential solution to obtain a breast cancer-specific profile is to enrich tumor-specific miRNAs through isolation of circulating microvesicles using markers specific to the tissue of origin. For instance, epithelial cell adhesion molecule (EpCAM)-positive microvesicles were isolated from ovarian cancer for miRNA profiling.139
Conclusions
Circulating miRNAs hold a great promise as diagnostic, prognostic or predictive biomarkers in the clinical management of patients with breast cancer. In our review of the current state of knowledge in the field, we observed little consistency with respect to the circulating miRNA panels identified by different research groups, hence currently we do not have clinically useful panel of circulating miRNA to be used in the oncology practice. This is in part because of variations in patient selection and techniques used to isolate and measure circulating miRNAs, their low abundance, the effects of therapy, and concurrent diseases, inadequate sample sizes, inadequate statistical analysis, and insufficient numbers of validation studies testing their clinical utilization. A number of issues related to sample collection, method of measurements and normalization are still in need for standardization and streamlining, whereas a number of approaches are currently under development to enhance detection sensitivity and specificity and improve the clinical applications of miRNAs. Multi-center global profiling studies may provide useful data for identifying diagnostic, prognostic, or predictive circulating miRNA panels. Although these issues may hamper the clinical use of miRNA profiling in clinical practice, their use as research tools to understand and possibly target cancer cells and cancer stem cells are currently rich areas for clinical investigation.
References
Siegel RL, Miller KD, Jemal A . Cancer statistics 2015 CA Cancer J Clin 2015; 65: 5–29.
Youlden DR, Cramb SM, Dunn NA, Muller JM, Pyke CM, Baade PD . The descriptive epidemiology of female breast cancer: an international comparison of screening, incidence, survival and mortality. Cancer Epidemiol 2012; 36: 237–248.
International Agency for research on Cancer. GLOBOCAN Cancer Fact Sheets: Breast cancer http://globocan.iarc.fr/old/FactSheets/cancers/breast-new.asp Accessed 10 October 2016.
Jorgensen KJ, Kalager M, Barratt A, Baines C, Zahl PH, Brodersen J et al. Overview of guidelines on breast screening: why recommendations differ and what to do about it. Breast 2016; 31: 261–269.
Charles L, Loprinzi FRA, Martee L, Hensley JTR ASCO SEP. 3rd edn. American Society of Clinical Oncology, Alexandria, VA, USA, 2013.
Ellsworth RE, Blackburn HL, Shriver CD, Soon-Shiong P, Ellsworth DL . Molecular heterogeneity in breast cancer: state of the science and implications for patient care. Semin Cell Dev Biol 2016; 64: 65–72.
Paik S, Shak S, Tang G, Kim C, Baker J, Cronin M et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N Engl J Med 2004; 351: 2817–2826.
Baek D, Villen J, Shin C, Camargo FD, Gygi SP, Bartel DP . The impact of microRNAs on protein output. Nature 2008; 455: 64–71.
Lim LP, Lau NC, Garrett-Engele P, Grimson A, Schelter JM, Castle J et al. Microarray analysis shows that some microRNAs downregulate large numbers of target mRNAs. Nature 2005; 433: 769–773.
Selbach M, Schwanhausser B, Thierfelder N, Fang Z, Khanin R, Rajewsky N . Widespread changes in protein synthesis induced by microRNAs. Nature 2008; 455: 58–63.
Bushati N, Cohen SM . microRNA functions. Annu Rev Cell Dev Biol 2007; 23: 175–205.
Friedman RC, Farh KK, Burge CB, Bartel DP . Most mammalian mRNAs are conserved targets of microRNAs. Genome Res 2009; 19: 92–105.
Carthew RW, Sontheimer EJ . Origins and mechanisms of miRNAs and siRNAs. Cell 2009; 136: 642–655.
Davis BN, Hata A . Regulation of microRNA biogenesis: a miRiad of mechanisms. Cell Commun Signal 2009; 7: 18.
Filipowicz W, Bhattacharyya SN, Sonenberg N . Mechanisms of post-transcriptional regulation by microRNAs: are the answers in sight? Nat Rev Genet 2008; 9: 102–114.
Forman JJ, Legesse-Miller A, Coller HA . A search for conserved sequences in coding regions reveals that the let-7 microRNA targets Dicer within its coding sequence. Proc Natl Acad Sci USA 2008; 105: 14879–14884.
Hausser J, Landthaler M, Jaskiewicz L, Gaidatzis D, Zavolan M . Relative contribution of sequence and structure features to the mRNA binding of Argonaute/EIF2C-miRNA complexes and the degradation of miRNA targets. Genome Res 2009; 19: 2009–2020.
Hendrickson DG, Hogan DJ, McCullough HL, Myers JW, Herschlag D, Ferrell JE et al. Concordant regulation of translation and mRNA abundance for hundreds of targets of a human microRNA. PLoS Biol 2009; 7: e1000238.
Vasudevan S, Tong Y, Steitz JA . Switching from repression to activation: microRNAs can up-regulate translation. Science 2007; 318: 1931–1934.
Winter J, Jung S, Keller S, Gregory RI, Diederichs S . Many roads to maturity: microRNA biogenesis pathways and their regulation. Nat Cell Biol 2009; 11: 228–234.
Lee Y, Ahn C, Han J, Choi H, Kim J, Yim J et al. The nuclear RNase III Drosha initiates microRNA processing. Nature 2003; 425: 415–419.
Lee Y, Kim M, Han J, Yeom KH, Lee S, Baek SH et al. MicroRNA genes are transcribed by RNA polymerase II. EMBO J 2004; 23: 4051–4060.
Zeng Y, Yi R, Cullen BR . Recognition and cleavage of primary microRNA precursors by the nuclear processing enzyme Drosha. EMBO J 2005; 24: 138–148.
Lund E, Guttinger S, Calado A, Dahlberg JE, Kutay U . Nuclear export of microRNA precursors. Science 2004; 303: 95–98.
Yi R, Qin Y, Macara IG, Cullen BR . Exportin-5 mediates the nuclear export of pre-microRNAs and short hairpin RNAs. Genes Dev 2003; 17: 3011–3016.
Ding XC, Weiler J, Grosshans H . Regulating the regulators: mechanisms controlling the maturation of microRNAs. Trends Biotechnol 2009; 27: 27–36.
Bosse GD, Simard MJ . A new twist in the microRNA pathway: not Dicer but Argonaute is required for a microRNA production. Cell Res 2010; 20: 735–737.
Hutvagner G, Simard MJ . Argonaute proteins: key players in RNA silencing. Nat Rev Mol Cell Biol 2008; 9: 22–32.
Giraldez AJ, Mishima Y, Rihel J, Grocock RJ, Van Dongen S, Inoue K et al. Zebrafish MiR-430 promotes deadenylation and clearance of maternal mRNAs. Science 2006; 312: 75–79.
Pillai RS, Bhattacharyya SN, Artus CG, Zoller T, Cougot N, Basyuk E et al. Inhibition of translational initiation by Let-7 MicroRNA in human cells. Science 2005; 309: 1573–1576.
Zeng Y, Cullen BR . Sequence requirements for micro RNA processing and function in human cells. RNA 2003; 9: 112–123.
Doench JG, Petersen CP, Sharp PA . siRNAs can function as miRNAs. Genes Dev 2003; 17: 438–442.
Li WH, Gojobori T, Nei M . Pseudogenes as a paradigm of neutral evolution. Nature 1981; 292: 237–239.
Vanin EF . Processed pseudogenes: characteristics and evolution. Annu Rev Genet 1985; 19: 253–272.
Poliseno L, Salmena L, Zhang J, Carver B, Haveman WJ, Pandolfi PP . A coding-independent function of gene and pseudogene mRNAs regulates tumour biology. Nature 2010; 465: 1033–1038.
Rinn JL, Kertesz M, Wang JK, Squazzo SL, Xu X, Brugmann SA et al. Functional demarcation of active and silent chromatin domains in human HOX loci by noncoding RNAs. Cell 2007; 129: 1311–1323.
Liu XH, Sun M, Nie FQ, Ge YB, Zhang EB, Yin DD et al. Lnc RNA HOTAIR functions as a competing endogenous RNA to regulate HER2 expression by sponging miR-331-3p in gastric cancer. Mol Cancer 2014; 13: 92.
Lasda E, Parker R . Circular RNAs: diversity of form and function. RNA 2014; 20: 1829–1842.
Hansen TB, Jensen TI, Clausen BH, Bramsen JB, Finsen B, Damgaard CK et al. Natural RNA circles function as efficient microRNA sponges. Nature 2013; 495: 384–388.
Kroh EM, Parkin RK, Mitchell PS, Tewari M . Analysis of circulating microRNA biomarkers in plasma and serum using quantitative reverse transcription-PCR (qRT-PCR). Methods 2010; 50: 298–301.
Hamam R, Ali AM, Alsaleh KA, Kassem M, Alfayez M, Aldahmash A et al. microRNA expression profiling on individual breast cancer patients identifies novel panel of circulating microRNA for early detection. Sci Rep 2016; 6: 25997.
Wu X, Somlo G, Yu Y, Palomares MR, Li AX, Zhou W et al. De novo sequencing of circulating miRNAs identifies novel markers predicting clinical outcome of locally advanced breast cancer. J Transl Med 2012; 10: 42.
Oikonomopoulos A, Polytarchou C, Joshi S, Hommes DW, Iliopoulos D . Identification of circulating microRNA signatures in Crohn's disease using the Nanostring nCounter technology. Inflamm Bowel Dis 2016; 22: 2063–2069.
Alajez NM, Shi W, Wong D, Lenarduzzi M, Waldron J, Weinreb I et al. Lin28b promotes head and neck cancer progression via modulation of the insulin-like growth factor survival pathway. Oncotarget 2012; 3: 1641–1652.
Kirschner MB, Kao SC, Edelman JJ, Armstrong NJ, Vallely MP, van Zandwijk N et al. Haemolysis during sample preparation alters microRNA content of plasma. PLoS ONE 2011; 6: e24145.
McDonald JS, Milosevic D, Reddi HV, Grebe SK, Algeciras-Schimnich A . Analysis of circulating microRNA: preanalytical and analytical challenges. Clin Chem 2011; 57: 833–840.
Eulalio A, Mano M, Dal Ferro M, Zentilin L, Sinagra G, Zacchigna S et al. Functional screening identifies miRNAs inducing cardiac regeneration. Nature 2012; 492: 376–381.
Quiat D, Olson EN . MicroRNAs in cardiovascular disease: from pathogenesis to prevention and treatment. J Clin Invest 2013; 123: 11–18.
Cao L, Lin EJ, Cahill MC, Wang C, Liu X, During MJ . Molecular therapy of obesity and diabetes by a physiological autoregulatory approach. Nat Med 2009; 15: 447–454.
Hilton C, Neville MJ, Karpe F . MicroRNAs in adipose tissue: their role in adipogenesis and obesity. Int J Obes (Lond) 2012; 37: 325–332.
Dehwah MA, Xu A, Huang Q . MicroRNAs and type 2 diabetes/obesity. J Genet Genomics 2012; 39: 11–18.
Croce CM . Causes and consequences of microRNA dysregulation in cancer. Nat Rev Genet 2009; 10: 704–714.
Alajez NM, Lenarduzzi M, Ito E, Hui AB, Shi W, Bruce J et al. MiR-218 suppresses nasopharyngeal cancer progression through downregulation of survivin and the SLIT2-ROBO1 pathway. Cancer Res 2011; 71: 2381–2391.
Viswanathan SR, Powers JT, Einhorn W, Hoshida Y, Ng TL, Toffanin S et al. Lin28 promotes transformation and is associated with advanced human malignancies. Nat Genet 2009; 41: 843–848.
Yu F, Yao H, Zhu P, Zhang X, Pan Q, Gong C et al. let-7 regulates self renewal and tumorigenicity of breast cancer cells. Cell 2007; 131: 1109–1123.
Altuvia Y, Landgraf P, Lithwick G, Elefant N, Pfeffer S, Aravin A et al. Clustering and conservation patterns of human microRNAs. Nucleic Acids Res 2005; 33: 2697–2706.
Huber MA, Azoitei N, Baumann B, Grunert S, Sommer A, Pehamberger H et al. NF-kappaB is essential for epithelial-mesenchymal transition and metastasis in a model of breast cancer progression. J Clin Invest 2004; 114: 569–581.
Yang J, Mani SA, Donaher JL, Ramaswamy S, Itzykson RA, Come C et al. Twist, a master regulator of morphogenesis, plays an essential role in tumor metastasis. Cell 2004; 117: 927–939.
Shimono Y, Zabala M, Cho RW, Lobo N, Dalerba P, Qian D et al. Downregulation of miRNA-200c links breast cancer stem cells with normal stem cells. Cell 2009; 138: 592–603.
Korpal M, Lee ES, Hu G, Kang Y . The miR-200 family inhibits epithelial-mesenchymal transition and cancer cell migration by direct targeting of E-cadherin transcriptional repressors ZEB1 and ZEB2. J Biol Chem 2008; 283: 14910–14914.
Jurmeister S, Baumann M, Balwierz A, Keklikoglou I, Ward A, Uhlmann S et al. MicroRNA-200c represses migration and invasion of breast cancer cells by targeting actin-regulatory proteins FHOD1 and PPM1F. Mol Cell Biol 2012; 32: 633–651.
Ma L, Teruya-Feldstein J, Weinberg RA . Tumour invasion and metastasis initiated by microRNA-10b in breast cancer. Nature 2007; 449: 682–688.
Baffa R, Fassan M, Volinia S, O'Hara B, Liu CG, Palazzo JP et al. MicroRNA expression profiling of human metastatic cancers identifies cancer gene targets. J Pathol 2009; 219: 214–221.
Rowland BD, Peeper DS . KLF4, p21 and context-dependent opposing forces in cancer. Nat Rev Cancer 2006; 6: 11–23.
Frankel LB, Christoffersen NR, Jacobsen A, Lindow M, Krogh A, Lund AH . Programmed cell death 4 (PDCD4) is an important functional target of the microRNA miR-21 in breast cancer cells. J Biol Chem 2008; 283: 1026–1033.
Zhu S, Si ML, Wu H, Mo YY . MicroRNA-21 targets the tumor suppressor gene tropomyosin 1 (TPM1). J Biol Chem 2007; 282: 14328–14336.
Qian B, Katsaros D, Lu L, Preti M, Durando A, Arisio R et al. High miR-21 expression in breast cancer associated with poor disease-free survival in early stage disease and high TGF-beta1. Breast Cancer Res Treat 2009; 117: 131–140.
Wickramasinghe NS, Manavalan TT, Dougherty SM, Riggs KA, Li Y, Klinge CM . Estradiol downregulates miR-21 expression and increases miR-21 target gene expression in MCF-7 breast cancer cells. Nucleic Acids Res 2009; 37: 2584–2595.
Si ML, Zhu S, Wu H, Lu Z, Wu F, Mo YY . miR-21-mediated tumor growth. Oncogene 2007; 26: 2799–2803.
Schramedei K, Morbt N, Pfeifer G, Lauter J, Rosolowski M, Tomm JM et al. MicroRNA-21 targets tumor suppressor genes ANP32A and SMARCA4. Oncogene 2011; 30: 2975–2985.
Png KJ, Yoshida M, Zhang XH, Shu W, Lee H, Rimner A et al. MicroRNA-335 inhibits tumor reinitiation and is silenced through genetic and epigenetic mechanisms in human breast cancer. Genes Dev 2011; 25: 226–231.
Tavazoie SF, Alarcon C, Oskarsson T, Padua D, Wang Q, Bos PD et al. Endogenous human microRNAs that suppress breast cancer metastasis. Nature 2008; 451: 147–152.
Heyn H, Engelmann M, Schreek S, Ahrens P, Lehmann U, Kreipe H et al. MicroRNA miR-335 is crucial for the BRCA1 regulatory cascade in breast cancer development. Int J Cancer 2011; 129: 2797–2806.
Shi W, Gerster K, Alajez NM, Tsang J, Waldron L, Pintilie M et al. MicroRNA-301 mediates proliferation and invasion in human breast cancer. Cancer Res 2011; 71: 2926–2937.
Faraoni I, Antonetti FR, Cardone J, Bonmassar E . miR-155 gene: a typical multifunctional microRNA. Biochim Biophys Acta 2009; 1792: 497–505.
O'Donovan PJ, Livingston DM . BRCA1 and BRCA2: breast/ovarian cancer susceptibility gene products and participants in DNA double-strand break repair. Carcinogenesis 2010; 31: 961–967.
Szabo CI, King MC . Inherited breast and ovarian cancer. Hum Mol Genet 1995; 4 Spec No: 1811–1817.
Jiang S, Zhang HW, Lu MH, He XH, Li Y, Gu H et al. MicroRNA-155 functions as an OncomiR in breast cancer by targeting the suppressor of cytokine signaling 1 gene. Cancer Res 2010; 70: 3119–3127.
Yamakuchi M, Ferlito M, Lowenstein CJ . miR-34a repression of SIRT1 regulates apoptosis. Proc Natl Acad Sci USA 2008; 105: 13421–13426.
Li L, Yuan L, Luo J, Gao J, Guo J, Xie X . MiR-34a inhibits proliferation and migration of breast cancer through down-regulation of Bcl-2 and SIRT1. Clin Exp Med 2013; 13: 109–117.
Wu H, Zhu S, Mo YY . Suppression of cell growth and invasion by miR-205 in breast cancer. Cell Res 2009; 19: 439–448.
Iorio MV, Casalini P, Piovan C, Di Leva G, Merlo A, Triulzi T et al. microRNA-205 regulates HER3 in human breast cancer. Cancer Res 2009; 69: 2195–2200.
Gregory PA, Bert AG, Paterson EL, Barry SC, Tsykin A, Farshid G et al. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat Cell Biol 2008; 10: 593–601.
Vickers KC, Palmisano BT, Shoucri BM, Shamburek RD, Remaley AT . MicroRNAs are transported in plasma and delivered to recipient cells by high-density lipoproteins. Nat Cell Biol 2011; 13: 423–433.
Valadi H, Ekstrom K, Bossios A, Sjostrand M, Lee JJ, Lotvall JO . Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol 2007; 9: 654–659.
Pegtel DM, Cosmopoulos K, Thorley-Lawson DA, van Eijndhoven MA, Hopmans ES, Lindenberg JL et al. Functional delivery of viral miRNAs via exosomes. Proc Natl Acad Sci USA 2010; 107: 6328–6333.
Turchinovich A, Weiz L, Burwinkel B . Extracellular miRNAs: the mystery of their origin and function. Trends Biochem Sci 2012; 37: 460–465.
Al-toub M, Vishnubalaji R, Hamam R, Kassem M, Aldahmash A, Alajez NM . CDH1 and IL1-beta expression dictates FAK and MAPKK-dependent cross-talk between cancer cells and human mesenchymal stem cells. Stem Cell Res Ther 2015; 6: 135.
Chen X, Ba Y, Ma L, Cai X, Yin Y, Wang K et al. Characterization of microRNAs in serum: a novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res 2008; 18: 997–1006.
Gilad S, Meiri E, Yogev Y, Benjamin S, Lebanony D, Yerushalmi N et al. Serum microRNAs are promising novel biomarkers. PLoS ONE 2008; 3: e3148.
Mitchell PS, Parkin RK, Kroh EM, Fritz BR, Wyman SK, Pogosova-Agadjanyan EL et al. Circulating microRNAs as stable blood-based markers for cancer detection. Proc Natl Acad Sci USA 2008; 105: 10513–10518.
Chin LJ, Slack FJ . A truth serum for cancer—microRNAs have major potential as cancer biomarkers. Cell Res 2008; 18: 983–984.
Guay C, Regazzi R . Circulating microRNAs as novel biomarkers for diabetes mellitus. Nat Rev Endocrinol 2013; 9: 513–521.
Gandhi R, Healy B, Gholipour T, Egorova S, Musallam A, Hussain MS et al. Circulating microRNAs as biomarkers for disease staging in multiple sclerosis. Ann Neurol 2013; 73: 729–740.
Khoo SK, Petillo D, Kang UJ, Resau JH, Berryhill B, Linder J et al. Plasma-based circulating MicroRNA biomarkers for Parkinson's disease. J Parkinson's Dis 2012; 2: 321–331.
Lawrie CH, Gal S, Dunlop HM, Pushkaran B, Liggins AP, Pulford K et al. Detection of elevated levels of tumour-associated microRNAs in serum of patients with diffuse large B-cell lymphoma. Br J Haematol 2008; 141: 672–675.
Resnick KE, Alder H, Hagan JP, Richardson DL, Croce CM, Cohn DE . The detection of differentially expressed microRNAs from the serum of ovarian cancer patients using a novel real-time PCR platform. Gynecol Oncol 2009; 112: 55–59.
Ng EK, Chong WW, Jin H, Lam EK, Shin VY, Yu J et al. Differential expression of microRNAs in plasma of patients with colorectal cancer: a potential marker for colorectal cancer screening. Gut 2009; 58: 1375–1381.
Tanaka M, Oikawa K, Takanashi M, Kudo M, Ohyashiki J, Ohyashiki K et al. Down-regulation of miR-92 in human plasma is a novel marker for acute leukemia patients. PLoS ONE 2009; 4: e5532.
Ho AS, Huang X, Cao H, Christman-Skieller C, Bennewith K, Le QT et al. Circulating miR-210 as a novel hypoxia marker in pancreatic cancer. Transl Oncol 2010; 3: 109–113.
Wang J, Chen J, Chang P, LeBlanc A, Li D, Abbruzzesse JL et al. MicroRNAs in plasma of pancreatic ductal adenocarcinoma patients as novel blood-based biomarkers of disease. Cancer Prevent Res 2009; 2: 807–813.
Wong TS, Ho WK, Chan JY, Ng RW, Wei WI . Mature miR-184 and squamous cell carcinoma of the tongue. Sci World J 2009; 9: 130–132.
Yamamoto Y, Kosaka N, Tanaka M, Koizumi F, Kanai Y, Mizutani T et al. MicroRNA-500 as a potential diagnostic marker for hepatocellular carcinoma. Biomarkers 2009; 14: 529–538.
Heneghan HM, Miller N, Kelly R, Newell J, Kerin MJ . Systemic miRNA-195 differentiates breast cancer from other malignancies and is a potential biomarker for detecting noninvasive and early stage disease. Oncologist 2010; 15: 673–682.
Schwarzenbach H, Milde-Langosch K, Steinbach B, Muller V, Pantel K . Diagnostic potential of PTEN-targeting miR-214 in the blood of breast cancer patients. Breast Cancer Res Treat 2012; 134: 933–941.
Cuk K, Zucknick M, Madhavan D, Schott S, Golatta M, Heil J et al. Plasma microRNA panel for minimally invasive detection of breast cancer. PLoS ONE 2013; 8: e76729.
Shen J, Hu Q, Schrauder M, Yan L, Wang D, Medico L et al. Circulating miR-148b and miR-133a as biomarkers for breast cancer detection. Oncotarget 2014; 5: 5284–5294.
Kodahl AR, Lyng MB, Binder H, Cold S, Gravgaard K, Knoop AS et al. Novel circulating microRNA signature as a potential non-invasive multi-marker test in ER-positive early-stage breast cancer: a case control study. Mol Oncol 2014; 8: 874–883.
Zearo S, Kim E, Zhu Y, Zhao JT, Sidhu SB, Robinson BG et al. MicroRNA-484 is more highly expressed in serum of early breast cancer patients compared to healthy volunteers. BMC Cancer 2014; 14: 200.
Shimomura A, Shiino S, Kawauchi J, Takizawa S, Sakamoto H, Matsuzaki J et al. Novel combination of serum microRNA for detecting breast cancer in the early stage. Cancer Sci 2016; 107: 326–334.
Sochor M, Basova P, Pesta M, Dusilkova N, Bartos J, Burda P et al. Oncogenic microRNAs: miR-155, miR-19a, miR-181b, and miR-24 enable monitoring of early breast cancer in serum. BMC Cancer 2014; 14: 448.
Chan M, Liaw CS, Ji SM, Tan HH, Wong CY, Thike AA et al. Identification of circulating microRNA signatures for breast cancer detection. Clin Cancer Res 2013; 19: 4477–4487.
Matamala N, Vargas MT, Gonzalez-Campora R, Minambres R, Arias JI, Menendez P et al. Tumor microRNA expression profiling identifies circulating microRNAs for early breast cancer detection. Clin Chem 2015; 61: 1098–1106.
Li XX, Gao SY, Wang PY, Zhou X, Li YJ, Yu Y et al. Reduced expression levels of let-7c in human breast cancer patients. Oncol Lett 2015; 9: 1207–1212.
Wang PY, Gong HT, Li BF, Lv CL, Wang HT, Zhou HH et al. Higher expression of circulating miR-182 as a novel biomarker for breast cancer. Oncol Lett 2013; 6: 1681–1686.
Waters PS, Dwyer RM, Brougham C, Glynn CL, Wall D, Hyland P et al. Impact of tumour epithelial subtype on circulating microRNAs in breast cancer patients. PLoS ONE 2014; 9: e90605.
Blenkiron C, Goldstein LD, Thorne NP, Spiteri I, Chin SF, Dunning MJ et al. MicroRNA expression profiling of human breast cancer identifies new markers of tumor subtype. Genome Biol 2007; 8: R214.
Iorio MV, Ferracin M, Liu CG, Veronese A, Spizzo R, Sabbioni S et al. MicroRNA gene expression deregulation in human breast cancer. Cancer Res 2005; 65: 7065–7070.
Zhu W, Qin W, Atasoy U, Sauter ER . Circulating microRNAs in breast cancer and healthy subjects. BMC Res Notes 2009; 2: 89.
Wang F, Zheng Z, Guo J, Ding X . Correlation and quantitation of microRNA aberrant expression in tissues and sera from patients with breast tumor. Gynecol Oncol 2010; 119: 586–593.
Joosse SA, Muller V, Steinbach B, Pantel K, Schwarzenbach H . Circulating cell-free cancer-testis MAGE-A RNA, BORIS RNA, let-7b and miR-202 in the blood of patients with breast cancer and benign breast diseases. Br J Cancer 2014; 111: 909–917.
Mangolini A, Ferracin M, Zanzi MV, Saccenti E, Ebnaof SO, Poma VV et al. Diagnostic and prognostic microRNAs in the serum of breast cancer patients measured by droplet digital PCR. Biomark Res 2015; 3: 12.
Kleivi Sahlberg K, Bottai G, Naume B, Burwinkel B, Calin GA, Borresen-Dale AL et al. A serum microRNA signature predicts tumor relapse and survival in triple-negative breast cancer patients. Clin Cancer Res 2015; 21: 1207–1214.
Chen W, Cai F, Zhang B, Barekati Z, Zhong XY . The level of circulating miRNA-10b and miRNA-373 in detecting lymph node metastasis of breast cancer: potential biomarkers. Tumour Biol 2013; 34: 455–462.
Roth C, Rack B, Muller V, Janni W, Pantel K, Schwarzenbach H . Circulating microRNAs as blood-based markers for patients with primary and metastatic breast cancer. Breast Cancer Res 2010; 12: R90.
Shaker O, Maher M, Nassar Y, Morcos G, Gad Z . Role of microRNAs -29b-2, -155, -197 and -205 as diagnostic biomarkers in serum of breast cancer females. Gene 2015; 560: 77–82.
Si H, Sun X, Chen Y, Cao Y, Chen S, Wang H et al. Circulating microRNA-92a and microRNA-21 as novel minimally invasive biomarkers for primary breast cancer. J Cancer Res Clin Oncol 2013; 139: 223–229.
Huo D, Clayton WM, Yoshimatsu TF, Chen J, Olopade OI . Identification of a circulating MicroRNA signature to distinguish recurrence in breast cancer patients. Oncotarget 2016; ; 7: 55231–55248.
Eichelser C, Flesch-Janys D, Chang-Claude J, Pantel K, Schwarzenbach H . Deregulated serum concentrations of circulating cell-free microRNAs miR-17, miR-34a, miR-155, and miR-373 in human breast cancer development and progression. Clin Chem 2013; 59: 1489–1496.
Wang H, Tan G, Dong L, Cheng L, Li K, Wang Z et al. Circulating MiR-125b as a marker predicting chemoresistance in breast cancer. PLoS ONE 2012; 7: e34210.
Sun Y, Wang M, Lin G, Sun S, Li X, Qi J et al. Serum microRNA-155 as a potential biomarker to track disease in breast cancer. PLoS ONE 2012; 7: e47003.
Witwer KW . Circulating microRNA biomarker studies: pitfalls and potential solutions. Clin Chem 2015; 61: 56–63.
Wang K, Yuan Y, Cho JH, McClarty S, Baxter D, Galas DJ . Comparing the MicroRNA spectrum between serum and plasma. PLoS ONE 2012; 7: e41561.
Diener Y, Walenda T, Jost E, Brummendorf TH, Bosio A, Wagner W et al. MicroRNA expression profiles of serum from patients before and after chemotherapy. Genomics Data 2015; 6: 125–127.
Hansen TF, Carlsen AL, Heegaard NH, Sorensen FB, Jakobsen A . Changes in circulating microRNA-126 during treatment with chemotherapy and bevacizumab predicts treatment response in patients with metastatic colorectal cancer. Br J Cancer 2015; 112: 624–629.
Ponomaryova AA, Morozkin ES, Rykova EY, Zaporozhchenko IA, Skvortsova TE, Dobrodeev capital AC et al. Dynamic changes in circulating miRNA levels in response to antitumor therapy of lung cancer. Exp Lung Res 2016; 42: 95–102.
Li Y, Kowdley KV . Method for microRNA isolation from clinical serum samples. Anal Biochem 2012; 431: 69–75.
Mathivanan S, Lim JW, Tauro BJ, Ji H, Moritz RL, Simpson RJ . Proteomics analysis of A33 immunoaffinity-purified exosomes released from the human colon tumor cell line LIM1215 reveals a tissue-specific protein signature. Mol Cell Proteomics 2010; 9: 197–208.
Taylor DD, Gercel-Taylor C . MicroRNA signatures of tumor-derived exosomes as diagnostic biomarkers of ovarian cancer. Gynecol Oncol 2008; 110: 13–21.
Acknowledgements
The authors thank the Deanship of Scientific Research at King Saud University (research group no. RG-1438-032) for funding this work. The funder had no role in the preparation of the manuscript or decision to publish.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by M Agostini
Rights and permissions
Cell Death and Disease is an open-access journal published by Nature Publishing Group. This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Hamam, R., Hamam, D., Alsaleh, K. et al. Circulating microRNAs in breast cancer: novel diagnostic and prognostic biomarkers. Cell Death Dis 8, e3045 (2017). https://doi.org/10.1038/cddis.2017.440
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2017.440
This article is cited by
-
MicroRNA signatures differentiate types, grades, and stages of breast invasive ductal carcinoma (IDC): miRNA-target interacting signaling pathways
Cell Communication and Signaling (2024)
-
Searching for the “Holy Grail” of breast cancer recurrence risk: a narrative review of the hunt for a better biomarker and the promise of circulating tumor DNA (ctDNA)
Breast Cancer Research and Treatment (2024)
-
Circulating tumour cells for early detection of clinically relevant cancer
Nature Reviews Clinical Oncology (2023)
-
SOX9 is a target of miR-134-3p and miR-224-3p in breast cancer cell lines
Molecular and Cellular Biochemistry (2023)
-
Novel polymorphism rs12402181 in the mature sequence of hsa-miR-3117-3p has a protective effect against breast cancer development by affecting miRNA processing and function
3 Biotech (2023)