Abstract
Type 2 diabetes is a chronic metabolic disorder, where failure to maintain normal glucose homoeostasis is associated with, and exacerbated by, obesity and the concomitant-elevated free fatty acid concentrations typically found in these patients. Hyperglycaemia and hyperlipidaemia together contribute to a decline in insulin-producing β-cell mass through activation of the transcription factors nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) and signal transducer and activator of transcription (STAT)-1. There are however a large number of molecules potentially able to modulate NF-κB and STAT1 activity, and the mechanism(s) by which glucolipotoxicity initially induces NF-κB and STAT1 activation is currently poorly defined. Using high-density microarray analysis of the β-cell transcritptome, we have identified those genes and proteins most sensitive to glucose and fatty acid environment. Our data show that of those potentially able to activate STAT1 or NF-κB pathways, tumour necrosis factor receptor (TNFR)-5 is the most highly upregulated by glucolipotoxicity. Importantly, our data also show that the physiological ligand for TNFR5, CD40L, elicits NF-κB activity in β-cells, whereas selective knockdown of TNFR5 ameliorates glucolipotoxic induction of STAT1 expression and NF-κB activity. This data indicate for the first time that TNFR5 signalling has a major role in triggering glucolipotoxic islet cell death.
Similar content being viewed by others
Main
In 2011, it was estimated that there were 347 million people worldwide living with diabetes.1 Moreover, the incidence of diabetes continues to grow at an alarming rate, with the figure in 2030 projected to be more than double that reported in 2000.2 There are a limited number of options to treat type 2 diabetes (T2D), and furthermore oral and injectable medications often become less effective over time. Thus, there is an urgent need to better understand the causes of diabetes, and to identify new targets for the development of novel treatment strategies.
Hyperglycaemia and hyperlipidaemia together contribute to the gradual loss of β-cell function that has been observed in patients with T2D. In addition to the failure of compensatory hypersecretion to overcome insulin resistance, reduction in β-cell mass through increased apoptosis is a key component of T2D.3, 4 Increased metabolic stress results in the activation of the transcription factors nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB)5, 6 and signal transducer and activator of transcription (STAT)-1.7 These then trigger the synthesis of a number of β-cell proteins, including the cytokine interleukin (IL)-1β.8 This is then released from the cell, whereupon it is able to bind the β-cell surface IL-1 receptor and amplify both NF-κB activation and the subsequent cytokine response that is driven through activation of nucleotide-binding oligomerization domain receptor family, pyrin domain containing 3 inflammasomes.5 In addition, inflammasome activation can also lead to caspase-1-mediated cell death through a process termed pyroptosis, which both fragments DNA and leads to pore formation in the plasma membrane.9
As well as these IL-1β-mediated cytokine response pathways, a number of chemokines are also synthesised and released by β-cells following glucolipotoxic activation of NF-κB.5 These serve to attract circulating immune cells, which then infiltrate the pancreas and are specifically drawn towards β-cells.10, 11 Here these immune cells release their own cocktail of cytokines. Along with glucolipotoxicity-induced β-cell IL-1β release, this localised toxic milieu effectively destroys β-cells.
Although we know many of the events resulting from NF-κB activation, the initial trigger of glucolipotoxic NF-κB activation remains poorly defined. Endoplasmic reticulum (ER) stress is one mechanism that has been proposed to initiate this response.12 However, as ER stress is typically induced by an increase in the synthesis of client proteins, this is more likely to occur in response to increased transcriptional activity and the resulting increase in protein synthesis and ER throughput. Hence, ER stress is more likely to be a consequence rather than cause of the increased transcriptional activity and/or islet inflammation. There are some exceptions, such as Wolfram syndrome where there is a coding mutation in the protein wolframin that is thought to regulate ER Ca2+ flux and thereby ensure protein fidelity and the degradation of misfolded proteins.13 However, as this and similar genetic disorders are relatively rare they are unlikely to contribute to ER stress in the majority of people with T2D.
Oxidative stress is another mechanism commonly championed, as the initial driver of gluco-or lipotoxic NF-κB activation in β-cells. This is also questionable, however, since reactive oxygen species (ROS) trigger a rapid spike in intracellular Ca2+ that results in transient exocytosis of insulin.14, 15 Indeed, there is increasing evidence to suggest that ROS are essential for normal β-cell function, including insulin secretion.16 Furthermore, some anti-oxidants potently inhibit glucose-stimulated insulin secretion, not enhance it.17 This may help explain why levels of the H2O2-inactivating enzymes glutathione peroxidase and catalase are particularly low in β-cells, when compared, for example, with expression level in the liver.18 This does not mean that β-cells are incapable of sustaining damage from excessive oxidative stress. However, given the routine high glycolytic throughput of β-cells and the general tolerance of β-cells against levels of ROS that would be damaging to other cells, it would seem incongruous were glucolipotoxicity to exert a disproportionately damaging effect upon pancreatic function.
To more accurately define the initial mechanisms triggering glucolipotoxicity-induced β-cell dysfunction, we used a combination of microarray expression profiling, independent quantitative PCR analysis, western blotting, confocal microscopy, and NF-κB activity assays to identify those genes and proteins, whose expression is most sensitive to glucose and fatty acid environment. Our data indicate that of the genes most likely to be associated with cell death pathways, tumour necrosis factor receptor (TNFR)-5 (also known as CD40) is the most highly upregulated and is able to induce STAT1 and NF-κB activation. Importantly, this pattern of upregulation was not restricted to rat insulinoma cells alone, but also isolated mouse islets from high-fat-fed mice and human islets, indicating that this may represent a conserved cell death activation mechanism.
Results
To better understand the mechanisms by which chronic exposure to high glucose and fatty acids alters cellular function, we incubated INS-1 rat pancreatic β-cell insulinoma cells for 72 h in Roswell Park Memorial Institute (RPMI)-1640 media and media supplemented with 28 mM glucose, 200 μM oleic acid, and 200 μM palmitic acid. Total RNA was isolated and hybridised to Affymetrix rat microarray chips (Santa Clara, CA, USA). Approximately 10% of INS-1 transcripts underwent a twofold or greater change in expression that was statistically significant (Supplementary Appendix Table 1). This included genes linked to apoptosis and related signalling pathways, biological oxidation, nucleic acid processing, and repair (Figure 1). To better understand how altered function in these genes correlates with human disease, we employed Metacore analysis algorithms (https://portal.genego.com) to identify the 25 diseases most closely associated with our data set. Table 1 indicates the degree of significance, along with enrichment expressed as the ratio of the number of genes that would be expected to be associated to each specific disease by chance (shown in green) compared with the number of the differentially expressed genes enriched in our data set (shown in red).
Effect of glucolipotoxicity on β-cell ontology. Comparative analysis of gene expression from INS-1 cells incubated for 72 h in RPMI-1640 media supplemented with or without 28 mM glucose, plus 200 μM oleic acid, and 200 μM palmitic acid. Data are compiled from six independent microarray analyses (three per experimental group). Reactome pathway analysis (http://www.reactome.org) identified 13 significant biological functions/pathways (P<0.05)
For molecules linked to inflammation and apoptosis, we found changed expression in a number of tumour necrosis receptor (TNFR) superfamily members and associated factors. Of these TNFRSF5, the gene encoding TNFR5 was found to be the most highly upregulated with 2.23-fold expression (P<0.01; Table 2). To validate these results, we performed independent quantitative real-time PCR (qRT-PCR) analysis of TNFRSF5, as well as the genes encoding TNFR1 and TNFR6 (also known as Fas) that have previously been shown to mediate cytokine-induced islet inflammation and apoptosis. Again, we observed significant increase in TNFRSF5 expression (3.62-fold; P<0.01) induced by high glucose and fatty acid environment (Table 2). TNFRSF1A was also upregulated by greater than twofold, but variable response meant that this was not deemed statistically significant in the samples examined. TNFRSF6 by contrast was only modestly upregulated, with this not found to be statistically significant in the PCR experiments. As a consequence, we focused our investigation on TNFR5 for the remainder of this study.
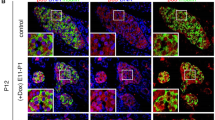
Although our data indicate significant upregulation in TNFRSF5 gene expression in β-cells exposed to a glucolipotoxic environment, mRNA does not always equate to protein. Therefore, we incubated INS-1 cells for 72 h in RPMI-1640 supplemented with either 28 mM glucose, 200 μM oleic acid, or 200 μM palmitic acid, both individually and in combination, and immunoblotted with anti-TNFR5 polyclonal antibody. The combination of glucose and fatty acids induced the strongest (two- to threefold; P<0.01) upregulation in TNFR5 protein (Figure 2a), although fatty acids or glucose alone also induced upregulation albeit by a more modest increase. These data are supported by immunofluorescence experiments (Figure 2b), in which there was a strong increase in TNFR5 intensity (green) in INS-1 cells incubated for 72 h in the presence of high glucose and fatty acids. Thus, a parallel increase in protein levels assessed both by western blot an immunofluorescence was detected under glucolipotoxic conditions.
TNFR5 protein expression in INS-1 β-cells, high-fat-fed mouse islets, and human islets. (a) INS-1 cells incubated for 72 h in RPMI-1640 media supplemented with or without 28 mM glucose, 200 μM oleic acid, and 200 μM palmitic acid. Immunoblots were conducted using anti-TNFR5 primary antibody (Santa Cruz Biotechnology, Dallas, TX, USA) and Li-Cor IR secondary antibody (Lincoln, NE, USA), and are representative of three independent experiments. (b) Imuunofluorescence of INS-1 cells fixed in 4% paraformaldehyde for 30 min, then permeabilized with 0.1% Triton X-100. Samples were treated with anti-DAPI (blue; Life Technologies Ltd., Paisley, UK) or anti-TNFR5 primary antibody (green), and incubated with secondary antibody conjugated to fluorescence dye (AF488; Life Technologies Ltd.). Images were taken with a Leica epi-fluo microscope (Wetzlar, Germany) using either a 20 × objective (upper panels) or 40 × objective (lower panels), and in each case are representative of three independent experiments. (c) C57Bl/6 mice were fed a high-fat or standard rodent diet for 10 weeks. Islets of mice were extracted and digested with collagenase, RNA extracted, reverse transcribed, and qRT-PCR analysis performed. Data were analysed using the ΔΔCT method from four independent experiments. (d) Human islets were cultured 24 h with or without 0.5 mM palmitate. RNA was extracted, reverse transcribed, and qRT-PCR analysis performed. Data were analysed using the ΔΔCT method from six independent experiments. *P<0.05
INS-1 tissue culture cells offer a consistent response to experimental manipulation, which makes them an ideal choice for microarray analysis where large numbers of repeat experiments are costly. However, as transformed β-cell lines are not always fully representative of primary β-cell biology, it becomes important to determine whether these findings are indicative of whole animal physiology. Therefore, C57Bl/6 mice were fed a high-fat diet for 10 weeks, resulting in impaired glucose tolerance, diminished insulin secretion, and reduced islet size. Pancreas was removed and total RNA extracted from isolated islets. In line with our INS-1 cell data, qRT-PCR analysis of extracted RNA showed a twofold increase in TNFRSF5 expression in the high-fat-fed mice relative to lean controls (Figure 2c). To determine whether our data were also reflective of human physiology, we next isolated islets post-mortem from human donors. These islets were incubated for 24 h in RPMI-1640 supplemented +/− 0.5 mM palmitate, total RNA extracted, and qRT-PCR performed. Despite the shorter incubation period, we again observed statistically significant upregulation of TNFRSF5 (1.4-fold; P<0.05; Figure 2d), indicative of a similar pattern of upregulation of TNFRSF5 in rodent and human islets.
To identify wider TNFR5 pathway interactions, non-biased network analysis was performed using the MetaCore integrated knowledge database of pathways (https://portal.genego.com). The gene content from microarray analysis files was used as the input list for generation of biological networks, using the analyse network algorithm with default settings. This is a variant of the shortest paths algorithm with main parameters of (1) relative enrichment with the uploaded data and (2) relative saturation of networks with canonical pathways. CD40L signalling through TNFR5 came out as the top ranked of all upregulated networks irrespective of cellular function. A further major finding from this analysis was the central involvement of Janus kinase (JAK)/STAT signalling pathways (Figure 3). As JAK/STAT signalling is often also linked to additional cytokine signalling through interferon (IFN)-γ-related pathways, we were able to assess the likely validity of these predictions by going back to our original data set and determining whether IFN-related genes showed changed expression. Of the six genes that came through our bioinformatic filter with statistically significant data, all six were upregulated. Furthermore, upregulation of all six genes was further confirmed by independent PCR analysis and shown to be statistically significant (P<0.001; Supplementary Appendix Table 2).
Network analysis of TNFR5 signalling. MetaCore (http://genego.com) was used to build a network from significantly upregulated genes in INS-1 cells subjected to glucolipotoxicity. The most significant biological network (P<0.001) included positive regulation of cellular, biological, and metabolic processes linked to TNFR5 and JAK/STAT signalling. Details of network objects and interactions are provided in the Metacore legend (Supplementary Appendix Figure 1). Thick cyan lines indicate the fragments of canonical pathways. Upregulated genes are marked with red circles
To gain more detailed understanding of the contribution of TNFR5 in triggering glucolipotoxic STAT1 and NF-kB responses, we selectively modulated TNFR5 expression and activity, and determined the resulting effect on STAT1 and NF-κB. INS-1 cells were transfected with either scramble sequence or short interfering RNA (siRNA) specifically directed against TNFR5, then incubated for a further 72 h in media supplemented with or without 28 mM glucose, 200 μM oleic acid, and 200 μM palmitic acid. Although the scramble sequence had no effect upon TNFR5 expression, the selective oligonucleotide brought down expression of TNFR5 by 96.0 +/− 1.0% in cells cultured in standard RPMI-1640, and by 97.8 +/− 1.3% in cells cultured in RPMI-1640 supplemented high glucose and fatty acids (Figure 4a). We then went on to determine STAT1 expression in these cells. Culturing cells for 72 h in media supplemented with high glucose and fatty acids resulted in STAT1 expression more than doubling (Figure 4b). However in cells where TNFR5 had been knocked down (siRNA lanes), STAT1 expression decreased by 61.0 +/− 4.0% in cells cultured in standard RPMI-1640 media (left panel), and by 54.6 +/− 2.9% in cells cultured in RPMI-1640 supplemented with high glucose and fatty acids (right panel).
Effect of TNFR5 on STAT1 expression. (a) INS-1 cells were either mock-transfected, transfected with scramble sequence RNA (ssRNA), or with specific interfering oligonucleotide (siRNA). Cells were then incubated for 72 h in RPMI-1640 media supplemented with or without 28 mM glucose, plus 200 μM oleic acid, and 200 μM palmitic acid. Immunoblots were conducted using anti-TNFR5 primary antibody (Santa Cruz Biotechnology). Alpha-tubulin was used for normalisation of the data. TNFR5 protein expression fold-changes are expressed as mean±S.E.M. of data obtained from three different experiments. (b) INS-1 cells were either mock-transfected, transfected with ssRNA, or with siRNA oligonucleotide. Cells were then incubated for 72 h in RPMI-1640 media supplemented with or without 28 mM glucose, plus 200 μM oleic acid, and 200 μM palmitic acid. Immunoblots were conducted using anti-STAT1 primary antibody (Cell Signalling Technology, Beverly, MA, USA). Alpha-tubulin was used for normalisation of the data. Protein expression fold-changes are expressed as mean±S.E.M. from data obtained from three different experiments. *P<0.05, **P< 0.01, ***P< 0.001
We next investigated how glucolipotoxicity and TNFR5 activity affect NF-κB expression, localisation, and activity. Following 72 h incubation in media supplemented with 28 mM glucose and 200 μM fatty acids, we observed a 73.5 +/− 5.7% increase in NF-κB expression (Figure 5a). Similarly, 6 h exposure of INS-1 cells to 1 μg/ml CD40L (the physiological activator of TNFR5) resulted in increased translocation of the NF-κB p65 subunit to the nucleus (Figure 5b). Although this is consistent with NF-κB activation by TNFR5, we nonetheless sought to confirm this using a quantitative ELISA assay that we have previously used to determine NF-κB activity in nuclear extracts isolated from cells of patients with autoinflammatory fevers.19, 20, 21 Using this assay, we were also able to compare NF-κB activity in β-cells treated with high glucose, TNFα, or CD40L. As can be seen (Figure 5c), 72 h incubation of INS-1 cells in 28 mM glucose resulted in an increased level of NF-κB activity similar to that observed, following 2 h exposure of cells to 100 ng/ml of TNFα. However, under low-glucose conditions where TNFR5 expression is not upregulated beyond basal, 6 h exposure to 1 μg/ml CD40L nevertheless still succeeded in eliciting half-maximal induction of NF-κB activity.
Effect of TNFR5 signalling on NF-κB expression, localization, and activity. (a) INS-1 cells were incubated for 72 h in RPMI-1640 media supplemented with or without 28 mM glucose, plus 200 μM oleic acid, and 200 μM palmitic acid (GLT). Immunoblots were conducted using using anti-NF-κB p65 subunit primary antibody (Santa Cruz Biotechnology). Beta-actin was used for normalization of the data. Data presented are representative of three independent experiments. (b) INS-1 cells were cultured onto coverslips and incubated with CD40 ligand (1 μg/ml) for 6 h. Cells were then fixed and stained with anti-NF-κB p65 polycolonal antibody (green) and DAPI (blue). Images were taken with a Leica EpiFluo microscope with a 63 × objective (representative image of three independent experiments). p65 translocation to the nucleus was quantified using Image J. (c) INS-1 rat pancreatic β-cells were cultured in RPMI-1640 media supplemented with glucose, TNF, or CD40 at the indicated concentrations and for the duration stated. NF-κB subunit activity was detected using TransAm ELISA kit (Active Motif, Rixensart, Belgium) directed against NFκB p65 subunits. Absorbance was measured at 450 nm, with a reference wavelength of 655 nm. All experimental data were gathered from a series of three independent experiments. (d) INS-1 cells were either mock-transfected, transfected with ssRNA, or with siRNA oligonucleotide, and cells then incubated for 72 h in RPMI-1640 media. NF-kB activity was quantified as outlined above. Experimental data were gathered from a series of five independent experiments. *P<0.05
The above experiments detail how glucolipotoxicity influences TNFR5 expression and activity. They do not however tell us whether the increased NF-κB activation is dependent upon TNFR5, or is instead simply coincidental to increased TNFR5 expression and activity. To address this point, we again knocked down TNFR5 expression, then measured NF-κB activity in mock-transfected cells, cells transfected with scramble sequence, and cells transfected with selective oligonucleotide. Although we were only able to achieve a much more modest knockdown of TNFR5 in this particular series of experiments (58.3 +/− 16.9%), this still significantly ablated NF-κB activity by 46.7 +/− 8.2%.
Discussion
Using an unbiased high-density microarray screen, we have been able to determine the effect of high glucose and fatty acid environment on thousands of genes simultaneously. Among the top 25 hits, our, data indicates the presence of disease association with both endocrine and metabolic disorders, which suggests the presence of pathways with known T2D and obesity aetiology in man. Interestingly, the molecules differentially expressed in this study were also found to be important in other diseases. Of those diseases were a number of brain disorders. This may reflect the pancreas being a highly innervated organ that shares a number of molecular similarities with brain at the level of transcriptome and proteome, the roots to which likely lie in the fact that the pancreas contains ancestral precursors of both pancreatic and neural crest origin.22 The data also indicate changed expression of genes associated with pathways common to many forms of neoplasm. Epidemiologic evidence suggests that people with diabetes are at significantly higher risk for many forms of cancer.23 Furthermore several studies indicate an association between diabetes and risk of liver, pancreatic, endometrial, colon/rectum, breast, and bladder cancer. Although common risk factors such as age, obesity, physical inactivity, and smoking undoubtedly contribute to the increased cancer risk in diabetic patients, hyperinsulinemia may also increase the likelihood of developing cancer due to insulin being a growth factor with metabolic and mitogenic effects. Its action in malignant cells is also favoured by mechanisms acting at both the receptor and post-receptor level.24
In agreement with the data presented here, it has previously been shown that both human and murine pancreatic β-cells express functional TNFR5.25, 26 Our observation that exposure of β-cells to high levels of glucose and/or fatty acids results in a two- to fourfold increase in expression of TNFR5 may therefore have clinical implications. However, without ligand activation increased receptor expression is unlikely to have a significant deleterious impact on functional β-cell mass. The pro-apoptotic response to glucose and lipids is not restricted to islet cells alone though. Previous work has shown that Indian subjects with diabetes have approximately three times higher soluble cluster of differentiation 40 ligand (sCD40L) levels in their plasma than individuals with normal glucose tolerance.27 The same study also found that plasma sCD40L levels were also elevated in people with impaired glucose tolerance, metabolic syndrome, and insulin resistance. Other researchers reported similar findings in a subsequent study in Europeans with T2D.28 Interestingly, this latter publication also reported a significant decrease in platelet TNFR5 signalling following sustained reduction in haemoglobin A1C, indicating that the process may be reversible. A positive correlation between glycaemic control and sCD40L level has also recently been reported in patients with type 1 diabetes.29
Our predictive pathway analysis indicates the potential for TNFR5 to regulate a wide range of cellular functions, including those that direct the ultimate fate of the β-cell – namely life and regeneration through cell proliferation (STAT5 and MAP3K) and cell cycle (cyclins and associated kinases), or cell death (Bcl-2 and B-cell lymphoma-extra large). At the heart of each of these pathways, however, lies NF-κB and/or STAT1. Therefore, the combination of high sCD40L levels found in diabetes and the upregulated expression of functional β-cell receptor shown here suggests that TNFR5 signalling may be responsible for much of the glucolipotoxicty-induced NF-κB activity in humans. Furthermore, given that NF-κB5, 6 and STAT17 activity are known to subsequently lead to islet cell death, we hypothesise that TNFR5 signalling likely represents a major cause of islet cell death in people with poorly controlled glucose homoeostasis and chronically elevated levels of glucose and fatty acids.
As glucolipotoxic induction of both STAT1 and NF-κB expression and activity can be prevented by downregulation of TNFR5 expression this has major potential therapeutic implications, not least as it might be possible to enhance islet cell survival through targeted disruption of TNFR5 pathways. Anti-TNFR5 strategies have previously been employed as a general immunosuppressant strategy following transplantation, and also to treat people suffering from lupus and several types of cancer. Intervention has not always met with success however, as there are a number of reports where anti-CD40L monoclonal antibodies have been shown to induce thromboembolic events.30, 31, 32, 33 Importantly, these dangerous side effects have not been observed when the receptor, rather than ligand, is targeted. Indeed, there are now numerous highly promising clinical trials taking place, involving different anti-TNFR5 monoclonal antibodies.34, 35 Of these, those employing antagonistic anti-TNFR5 antibodies are of particular relevance to our current study. Lucatumumab is one such example that has been found to be well tolerated,36 at least in moderate and intermediate strength doses.37 Importantly, it has also been shown to prevent induction of NF-κB activity in multiple myeloma cells.38 This strategy would need to be modified for the treatment of diabetes though, as immune cell interactions with the Fc region of cell-bound lucatumumab could potentially lead to either opsonisation of β-cells or antibody-dependent cell cytotoxicity. Phage display technology may provide an alternative solution however, facilitating the generation of antibody fragments containing the key heavy and light chain antigen recognition sites, although lacking the Fc region of the full molecule. This is an area that clearly warrants future research.
Materials and Methods
Materials
Antibodies were obtained from Santa Cruz Biotechnology Inc., Cell Signalling Technology, and Li-Cor Bioscience. Unless otherwise stated, all other chemicals were purchased from Sigma Aldrich (St. Louis, MO, USA) or VWR International Ltd (Lutterworth, UK).
Cell culture and islet isolation
INS-1 β-cells was cultured in RPMI-1640 media supplemented where indicated with 28 mM glucose, 200 μM oleic acid, or 200 μM palmitic acid for 72 h as detailed previously.39 C57Bl/6 mice (Charles River, UK) were fed a high-fat (60% fat-58Y1; Test Diets, St. Lois, MO, USA) or standard rodent diet for 10 weeks. Pancreas was surgically removed and digested in Hank's buffered salt solution containing collagenase P (1 mg/ml) and DNAse I (0.15 mg/ml; both Roche Diagnostics, Burgess Hill, UK). All animal experiments were conducted in accordance with the UK Home Office Animals (Scientific Procedures) Act, 1986, with local ethical committee approval. Human islets were isolated from non-diabetic multiorgan donors as previously detailed,40 with approval of the local ethics committee and with written informed consent from family members. In both cases, islets were hand-picked into RPMI-1640 and immediately lysed for RNA or protein experiments.
Quantitative RT-PCR
Cells were trypsinised, washed with cold phosphate-buffered saline (PBS) and lysed in RNAeasy QTL lysis buffer. Total RNA was prepared from lysed cells using RNeasy kit (Qiagen, Hilden, Germany) according to manufacturers recommended procedures (Qiagen). cDNA was generated from RNA using a standard RT kit (Promega, Madison, WI, USA). qRT-PCR reactions were performed using Maxima SYBR Green/ROX qPCR Master Mix (ThermoFisher Scientific, Loughborough, UK) and the following primers: rat CD40 forward primer GTCGGATTCTTCTCCAATG; rat CD40 reverse primer ACAGAGGGTATCAGTCTGAC; mouse CD40 forward primer TGGTCATTCCTGTCGTGATG; and mouse CD40 reverse primer GGCTCTGTCTTGGCTCATCT. Human islet experiments were performed as previously described,41 with CD40 oligonucleotide obtained from assay-on-demand gene expression products (Applied Biosystems, Foster City, CA, USA). Target gene mRNA was quantified and normalised for β-actin using an ABI7700 bioanalyzer (Applied Biosystems). Data were analysed using the ΔΔCT method.
Affymetrix arrays
Quality and integrity of extracted RNA was assessed using an Agilent Bioanalyser 2100 (Agilent Technologies, Santa Clara, CA, USA). A measure of 10 μg total RNA was converted into double-stranded cDNA using Superscript Reverse Transcriptase kit (Life Technologies Ltd.), following manufacturer’s T7-(dT)-based recommendation. T7 RNA polymerase was then used to convert the cDNA to biotin-labelled cRNA. cRNA generated with T7 polymerase was chemically fragmented, then hybridized overnight at 45 °C to Affymetrix high-density GeneChip Rat Genome 230 2.0 arrays (Affymetrix), each containing 31 000 probe set, analysing over 30 000 transcripts and variants from over 28 000 well-substantiated rat genes following Affymetrix Expression Analysis Technical Manual procedures. Chips were then washed and stained with streptavidin-phycoerythrin (SAPE). Signals were amplified by incubation with biotinylated anti-streptavidin antibody (Vector Laboratories, Burlingame, CA, USA) followed by a final SAPE staining step. Fluorescent pixel intensities for each probe were determined using a confocal laser scanner (GeneArray Scanner, Affymetrix), processed, quantified, background adjusted, and scaled using Affymetrix Microarray Suite 5.0 software (Affymetrix). Further MAS 5.0 analysis (Affymetrix) of scaled intensity data generated the absolute analysis for each probe, as well as comparative expression reading between two GeneChip arrays (Affymetrix). Condition-to-condition differential expression profile analysis was carried out using Genomics Suite (Partek Incorporated, St.Louis, MO, USA). Principal component analysis was applied to identify any independent sources of variation in the data.
Pathway identification and visualisation
For comprehensive analysis of biological pathways in which transcripts were differentially expressed we combined expression data from the microarray analysis with information in Reactome version 29, (http://www.reactome.org), a knowledgebase of biological pathways.42 To visualise the networks, we used MetaCore (http://genego.com) integrated knowledge database and software suite. Data analysis tools were used to generate high-resolution images of networks, with details of network objects and interactions provided in the Metacore legend (Supplementary Appendix Figure 1).
Western blotting
INS-1 cells were lysed and protein separated by SDS-PAGE. Protein was then transferred to nitrocellulose as described previously.39 Protein was detected using either anti-STAT1 (Cell Signalling Technology), anti-TNFR5, or anti-NF-κB p65 primary antibody (Santa Cruz Biotechnology), and Li-Cor IR secondary antibody. Antibody binding was detected using the LI-COR Fc Dual-Mode Imaging System (LI-COR).
Immunofluoresence
Cells were seeded in 12-well plates onto coverslips for 72 h in different media conditions, then fixed in 4% paraformaldehyde in PBS for 30 min and subsequently washed three times in PBS and store at +4 °C overnight. The following day, cells were permeabilized by with 0.1% Triton X-100 in PBS for 5 min, washed in 0.1% Triton in PBS, then incubated in primary antibody for 2 h at room temperature. Coverslips were then washed three times in PBS+Triton X-100 and then incubated with secondary antibody conjugated to fluorescence dye (AF488, ThermoFisher Scientific) for 1 h at room temperature. Images have been taken using a Leica DM5000 epi-fluo microscope.
Gene silencing
INS-1 cells were cultured to 40–50% confluency. siRNA oligonucleotide was combined with diluted lipofectamine RNAi max and mixed gently. After 25 min at room temp, the solution was mixed with RPMI and serum, but without antibiotics. This was then added to cells for 24 h, after which it was replaced with complete RPMI. Knockdown was detected 48–72 h after transfection by western blot.
NF-κB activity
TransAM NF-κB Family Kits (Active Motif, Rixensart, Belgium) were utilised for the study of specific NF-κB subunit pathways. In brief, oligonucleotide containing an NF-κB consensus-binding site was immobilized onto 96-well plates. The binding of NF-κB to its consensus sequence was detected by adding 30 μl of complete binding buffer to each well and 1 μg of nuclear extract diluted in complete lysis buffer was then added per well. The plates were sealed and incubated for 1 h at room temp with mild agitation. Each well was then washed three times with 200 μl 1 × wash buffer. Antibody directed against one of NF-κB p65 subunit was bound to the protein-oligonucleotide complex and detected following addition of secondary antibody, conjugated to horse radish peroxidase. Developing solution was added and the plate was incubated for 2–10 min at room temperature. Absorbance was then measured, using a spectrophotometer (Perkin Elmer-Wallac, Milan, Italy) Victor-1420 multi-label counter at 450 nm with a reference wavelength of 655 nm.
Statistical analysis
Results are expressed as mean±S.E.M. (n=3 or more independent experiments). Parameters were compared using unpaired Student's t-test and a P-value of<0.05 was considered significant.
Abbreviations
- ER:
-
endoplasmic reticulum
- IFN:
-
interferon
- IL:
-
interleukin
- JAK:
-
Janus kinase
- NF-κB:
-
nuclear factor kappa-light-chain-enhancer of activated B cells
- PBS:
-
phosphate-buffered saline
- qRT-PCR:
-
quantitative real-time PCR
- ROS:
-
reactive oxygen species
- RPMI:
-
Roswell Park Memorial Institute
- sCD40L:
-
soluble cluster of differentiation 40 ligand
- siRNA:
-
short interfering RNA
- STAT:
-
signal transducer and activator of transcription
- T2D:
-
type 2 diabetes
- TNFR:
-
tumour necrosis factor receptor
References
Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ et al. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 2011; 378: 31–40.
Wild S, Roglic G, Green A, Sicree R, King H . Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004; 27: 1047–1053.
Mathis D, Vence L, Benoist C . beta-Cell death during progression to diabetes. Nature 2001; 414: 792–798.
Rhodes CJ . Type 2 diabetes-a matter of beta-cell life and death? Science 2005; 307: 380–384.
Donath MY, Boni-Schnetzler M, Ellingsgaard H, Ehses JA . Islet inflammation impairs the pancreatic β-cell in type 2 diabetes. Physiology 2009; 24: 325–331.
Novotny GW, Lundh M, Backe MB, Christensen DP, Hansen JB, Dahllöf MS et al. Transcriptional and translational regulation of cytokine signaling in inflammatory β-cell dysfunction and apoptosis. Arch Biochem Biophys 2012; 528: 171–184.
Moore F, Naamane N, Colli ML, Bouckenooghe T, Ortis F, Gurzov EN et al. STAT1 is a master regulator of pancreatic β-cell apoptosis and islet inflammation. J Biol Chem 2011; 286: 929–941.
Maedler K, Sergeev P, Ris F, Oberholzer J, Joller-Jemelka HI, Spinas GA et al. Glucose-induced beta cell production of IL-1beta contributes to glucotoxicity in human pancreatic islets. J Clin Invest 2002; 110: 851–860.
Kepp O, Galluzzi L, Zitvogel L, Kroemer G . Pyroptosis - a cell death modality of its kind? Eur J Immunol 2010; 40: 627–630.
Ehses JA, Perren A, Eppler E, Ribaux P, Pospisilik JA, Maor-Cahn R et al. Increased number of islet-associated macrophages in type 2 diabetes. Diabetes 2007; 56: 2356–2370.
Donath MY, Schumann DM, Faulenbach M, Ellingsgaard H, Perren A, Ehses JA . Islet inflammation in type 2 diabetes: from metabolic stress to therapy. Diabetes Care 2008; 31: S161–S164.
Harding HP, Ron D . Endoplasmic reticulum stress and the development of diabetes: a review. Diabetes 2002; 51 (Suppl 3): S455–S461.
Inoue H, Tanizawa Y, Wasson J, Behn P, Kalidas K, Bernal-Mizrachi E et al. A gene encoding a transmembrane protein is mutated in patients with diabetes mellitus and optic atrophy (Wolfram syndrome). Nat Genet 1998; 20: 143–148.
Janjic D, Maechler P, Sekine N, Bartley C, Annen AS, Wolheim CB . Free radical modulation of insulin release in INS-1 cells exposed to alloxan. Biochem Pharmacol 1999; 57: 639–648.
Maechler P, Wollheim. CB . Mitochondrial glutamate acts as a messenger in glucose-induced insulin exocytosis. Nature 1999; 402: 685–689.
Pi J, Bai Y, Zhang Q, Wong V, Floering LM, Daniel K et al. Reactive oxygen species as a signal in glucose-stimulated insulin secretion. Diabetes 2007; 56: 1783–1791.
Llanos P, Contreras-Ferrat A, Barrientos G, Valencia M, Mears D, Hidalgo C . Glucose-dependent insulin secretion in pancreatic β-cell islets from male rats requires Ca2+ release via ROS-stimulated ryanodine receptors. PLoS One 2015; 10: e0129238.
Tiedge M, Lortz S, Drinkgern J, Lenzen S . Relation between antioxidant enzyme gene expression and antioxidative defense status of insulin-producing cells. Diabetes 1997; 46: 1733–1742.
Nedjai B, Hitman GA, Yousaf N, Chernajovsky Y, Stjernberg-Salmela S, Pettersson T et al. Abnormal tumor necrosis factor receptor I cell surface expression and NF-κB activation in tumor necrosis factor receptor-associated periodic syndrome. Arthritis Rheum 2008; 58: 273–283.
Nedjai B, Hitman GA, Quillinan N, Coughlan RJ, Church LD, McDermott MF et al. Proinflammatory action of the antiinflammatory drug infliximab in TNF-receptor associated periodic syndrome. Arthritis Rheum 2009; 60: 619–625.
Nedjai B, Hitman GA, Church LD, Minden K, Whiteford ML, McKee S et al. Differential cytokine secretion resulting from p65 and c-Rel NF-κB subunit signaling in peripheral blood mononuclear cells of TNFR-associated periodic fever syndrome patients. Cell Immunol 2011; 268: 55–59.
Arntfield M, van der Kooy D . The adult mammalian pancreas contains separate precursors of pancreatic and neural crest developmental origins. Stem Cells Dev 2013; 22: 2145–2157.
Tsugane S, Inoue M . Insulin resistance and cancer: epidemiological evidence. Cancer Sci 2010; 101: 1073–1079.
Cannata D, Fierz Y, Vijayakumar A, LeRoith D . Type 2 diabetes and cancer: what is the connection? Mt Sinai J Med 2010; 77: 197–213.
Klein D, Barbé-Tuana F, Pugliese A, Ichii H, Garza D, Gonzalez M et al. A functional CD40 receptor is expressed in pancreatic beta cells. Diabetologia 2005; 48: 268–276.
Klein D, Timoneri F, Ichii H, Ricordi C, Pastori RL . CD40 activation in human pancreatic islets and ductal cells. Diabetologia 2008; 51: 1853–1861.
Gokulakrishnan K, Deepa R, Mohan V, Gross MD . Soluble P-selectin and CD40L levels in subjects with prediabetes, diabetes mellitus, and metabolic syndrome—the Chennai Urban Rural Epidemiology Study. Metabolism 2006; 55: 237–242.
Neubauer H, Setiadi P, Günesdogan B, Pinto A, Börgel J, Mügge A . Influence of glycaemic control on platelet bound CD40-CD40L system, P-selectin and soluble CD40 ligand in Type 2 diabetes. Diabet Med 2010; 27: 384–390.
El-Asrar MA, Adly AA, Ismail EA . Soluble CD40L in children and adolescents with type 1 diabetes: relation to microvascular complications and glycemic control. Pediatr Diabetes 2012; 13: 616–624.
Kirk AD, Knechtle SJ, Vincenti FG, Nadeau KC . Preliminary results of the use of humanized anti-CD154 in human renal allotransplantation. Am J Transplant 2001; 1 (suppl 1): 191.
Boumpas DT, Furie R, Manzi S, Illei GG, Wallace DJ, Balow JE et al. BG9588 Lupus Nephritis Trial Group. short course of BG9588 (anti-CD40 ligand antibody) improves serologic activity and decreases hematuria in patients with proliferative lupus glomerulonephritis. Arthritis Rheum 2003; 48: 719–727.
Sidiropoulos PI, Boumpas DT . Lessons learned from anti-CD40L treatment in systemic lupus erythematosus patients. Lupus 2004; 13: 391–397.
Pree I, Wekerle T . New approaches to prevent transplant rejection: co-stimulation blockers anti-CD40L and CTLA4Ig. Drug Discov Today 2006; 3: 41–47.
Goldwater R, Keirns J, Blahunka P, First R, Sawamoto T, Zhang W et al. A phase 1, randomized ascending single-dose study of antagonist anti-human CD40 ASKP1240 in healthy subjects. Am J Transplant 2013; 13: 1040–1046.
Hassan SB, Sørensen JF, Olsen BN, Pedersen AE . Anti-CD40-mediated cancer immunotherapy: an update of recent and ongoing clinical trials. Immunopharmacol Immunotoxicol 2014; 36: 96–104.
Bensinger W, Maziarz RT, Jagannath S, Spencer A, Durrant S, Becker PS et al. A phase 1 study of lucatumumab, a fully human anti-CD40 antagonist monoclonal antibody administered intravenously to patients with relapsed or refractory multiple myeloma. Br J Haematol 2012; 159: 58–66.
Byrd JC, Kipps TJ, Flinn IW, Cooper M, Odenike O, Bendiske J et al. Phase I study of the anti-CD40 humanized monoclonal antibody lucatumumab (HCD122) in relapsed chronic lymphocytic leukemia. Leuk Lymphoma 2012; 53: 2136–2142.
Tai YT, Li X, Tong X, Santos D, Otsuki T, Catley L et al. Human anti-CD40 antagonist antibody triggers significant antitumor activity against human multiple myeloma. Cancer Res 2005; 65: 5898–5906.
Marshall C, Hitman GA, Cassell PG, Turner MD . Effect of glucolipotoxicity and rosiglitazone upon insulin secretion. Biochem Biophys Res Comm 2007; 356: 756–762.
Marselli L, Suleiman M, Masini M, Campani D, Bugliani M, Syed F et al. Are we overestimating the loss of beta cells in type 2 diabetes? Diabetologia 2014; 57: 362–365.
Bugliani M, Liechti R, Cheon H, Suleiman M, Marselli L, Kirkpatrick C et al. Microarray analysis of isolated human islet transcriptome in type 2 diabetes and the role of the ubiquitin-proteasome system in pancreatic beta cell dysfunction. Mol Cell Endocrinol 2013; 367: 1–10.
Matthews L, Gopinath G, Gillespie M, Caudy M, Croft D, de Bono B et al. Reactome knowledgebase of human biological pathways and processes. Nucleic Acids Res 2009; 37: D619–D622.
Acknowledgements
This study was funded by Diabetes UK, NovoNordisk UK Research Foundation, and St. Bartholomew’s & The Royal London Charitable Foundation grant awards.
Author contributions
MBa researched the data and reviewed/edited the manuscript. BWO researched the data and reviewed/edited the manuscript. CM researched the data. CT researched the data. KH researched the data and reviewed/edited the manuscript. TAJ researched the data and reviewed/edited the manuscript. MBu researched the data and reviewed/edited the manuscript. BN researched the data. PWC researched the data and reviewed/edited the manuscript. JK researched the data. MMY reviewed/edited the manuscript. GRB researched the data and reviewed the manuscript. PM contributed to the discussion and reviewed/edited the manuscript. GAH reviewed the experimental data and reviewed/edited the manuscript. MDT conceived and designed the study and wrote the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by A Stephanou
Supplementary Information accompanies this paper on Cell Death and Disease website
Rights and permissions
Cell Death and Disease is an open-access journal published by Nature Publishing Group. This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Bagnati, M., Ogunkolade, B., Marshall, C. et al. Glucolipotoxicity initiates pancreatic β-cell death through TNFR5/CD40-mediated STAT1 and NF-κB activation. Cell Death Dis 7, e2329 (2016). https://doi.org/10.1038/cddis.2016.203
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cddis.2016.203
This article is cited by
-
Salusin-β contributes to oxidative stress and inflammation in diabetic cardiomyopathy
Cell Death & Disease (2017)