Abstract
The compound 5-(4-methoxyarylimino)-2-N-(3,4-dichlorophenyl)-3-oxo-1,2,4-thiadiazolidine (P3-25) is known to possess anti-bacterial, anti-fungal, anti-tubercular, and local anesthetic activities. We studied the anti-tumorigenic activity of P3-25 and the role of nuclear transcription factor kappaB (NF-κB) in this process. In constitutive NF-κB-expressing cells, treatment with P3-25 inhibited the expression of NF-κB-dependent reporter gene, adhesion molecules, and cyclooxygenase. It downregulated phosphorylation of p65 by inhibiting upstream kinases, such as protein kinase A and casein kinase II, but did not alter NF-κB DNA-binding activity. Alone, P3-25 induced apoptosis in NF-κB-expressing and doxorubicin-resistant breast cancer cells, and in the presence of other chemotherapeutic agents, it potentiated apoptosis. Overall, our results suggest that P3-25 exerts antitumorigenic activity by inhibiting phosphorylation of p65, the transcriptionally active subunit of NF-κB by inhibiting its upstream kinases, and potentiates apoptosis mediated by chemotherapeutic agents. These results suggest novel approaches for designing of anticancer drugs for combination chemotherapy.
Similar content being viewed by others
Main
Nuclear transcription factor kappa B (NF-κB) has a role in oncogenesis and its regulation is important in cancer therapy. Overexpression, amplification, and rearrangements of different genes related to NF-κB have been observed in tumors.1 NF-κB is activated in response to various inflammatory stimuli including cytokines, mitogens, bacterial products, viral proteins, and apoptosis-inducing agents.2, 3 Although the primary level of NF-κB activation lies in the removal of the inhibitory subunit of NF-κB (inhibitory subunit of kappa B (IκBα)), the phosphorylation of p65 is required to recruit the transcriptional apparatus and to stimulate expression of several genes including cyclin D1, adhesion molecules, cyclooxygenase (Cox)-2, and matrix metalloproteinases. The activity of casein kinase II (CKII), known to be induced by several growth stimuli, is elevated in a variety of human cancers.4 Cytoplasmic NF-AT (cytoplasmic nuclear factor of activated T cells (NF-Atc)) is phosphorylated by CKII and translocated into the nucleus.5 RelA (p65) is phosphorylated at multiple serine residues such as Ser529,6, 7 Ser536,8 and Ser276 9 by CKII, IκB kinase (IKK), and protein kinase A (PKA)/mitogen and stress-activated protein kinase (MSK), respectively. PKA catalytic subunit binds with IκBα of NF-κB/IκB complex and remains inactive. When IκB is degraded, PKA becomes activated and phosphorylates p65 at Ser276.10 PKA activates another transcription factor cyclic AMP responsive element-binding protein (CREB) directly or via p38 MAPK and MSK1 pathways.11
Higher activity of NF-κB is a common characteristic of many tumor cells.1, 2, 12, 13 HuT-78, a cutaneous lymphoid T cell line that constitutively expresses NF-κB, is resistant to TNF-induced apoptosis.14, 15 Constitutive activity of IKK, mediated by different factors like interleukin-1, epidermal growth factor, heregulin, and so on, has been shown in constitutive NF-κB-expressing cells.16 BAY 11-7082 (BAY) is known to inhibit IKK, and thereby inhibits IκBα phosphorylation and NF-κB activation.17, 18 Constitutive expression of NF-κB leads to activation of several factors involved in cell cycle progression and cell differentiation for cancer metastasis. Inhibiting NF-κB activity in tumor cells dramatically reduced the cell growth in vitro and in vivo.19 NF-κB, possibly through the activation of the antiapoptotic genes, plays a key role in the protection of cells against inducers of apoptosis including chemotherapeutic drugs.13 Several mechanisms including increased expression of NF-κB proteins, mutations and/or deletions in IκBα gene, and increased IκBα turnover, and so on, are involved in NF-κB activation in tumor cells.1, 20 In spite of the growing evidence of the important role of NF-κB in tumorigenesis and its resistance to chemotherapy, only few attempts have been made to understand the mechanisms of the constitutive activity of NF-κB in tumor cells and its regulation for successful therapy.
The thiazolidones and thiadiazolie have drawn considerable attention for their anti-bacterial,21 anti-fungal,21 and anti-inflammatory 22 activities. Considering these effects and NF-κB's role in inflammation and tumor biology, newer derivatives of 1,2,4-thiadiazolidines, including 3-oxo-1,2,4-thiadiazolidines,23 were synthesized by using the oxidative debenzylation technique and their biological effects were studied.24 The dichlorophenyl derivatives of 1,2,4-thiadiazolidine were shown to inhibit TNF-induced activation of NF-κB through the inhibition of IKK activation.25
The aim of this study is to understand the molecular mechanisms underlying the resistance against chemotherapeutic agents due to basal NF-κB activation in different cancer cells. We have tested the role of upstream kinases for p65 phosphorylation and, thereby, the NF-κB-dependent genes transcription in those tumor cells that constitutively expressed NF-κB. Our results indicate that NF-κB is constitutively activated in different tumor cells such as HuT-78, HT-29, DU145, and PC3, but not Jurkat cell lines. The high level of phosphorylated p65 and its upstream kinases such as PKA and CKII in those cells led to the activation of several NF-κB-dependent genes. In this report, first the time we provide evidence that the dimethyl form of 1,2,4 thiadiazolidine inhibited PKA and CKII activities and consequently decreased phosphorylation of p65 and this resulted in the downregulation of transcription of several NF-κB-dependent genes involved in cell proliferation and metastasis. This compound potentiated cell death, mediated by chemotherapeutic agents in those constitutive NF-κB-expressing cells. Taken together, this study helps to understand the importance of phosphorylation of p65 in constitutive NF-κB-expressing cells for its tumorigenic activities. Downregulation of these kinases leads to the potentiation of apoptotic responses mediated by chemotherapeutic agents, which may help to further design oxo-1,2,4-thiadiazolidine compounds as potential antitumor drugs for combination therapy.
Results
In this study, we examined the effect of 5-(4-methoxyarylimino)-2-N-(3,4-dichlorophenyl)-3-oxo-1,2,4-thiadiazolidine (designated as P3-25 throughout the study) in NF-κB-expressing cells on phosphorylation of p65 and DNA-binding activity of NF-κB. Cell lines such as HuT-78, HT-29, DU145, and PC3 have constitutive activity of NF-κB. Jurkat cells, pulsed with 10 pM TNF for 1 h (indicated as Jkt/TNF), maintained high NF-κB activity for at least the duration of the experiments. All these cells were used as NF-κB-expressing cells for the entire study. P3-25 was chemically synthesized in the laboratory as described previously24 and was used as a solution in DMSO at 10 mM concentration. Further dilution was carried out in cell culture medium. The concentrations and duration of exposure of P3-25 employed in these studies had no effect on cytolysis as detected by the lactate dehydrogenase (LDH) assay from culture supernatant of treated cells (Culture supernatant from 100 nM P3-25-treated HuT-78 cells for 0, 6, 12, and 24 h when incubated with substrate solution (0.23 M sodium pyruvate and 5 mM NADH in 0.1 M phosphate buffer, pH 7.5) showed 1.214±0.102, 1.202±0.092, 1.192±0.124, and 1.172±0.114 absorbances, respectively, at 340 nm).
P3-25 blocks NF-κB-dependent reporter gene expression
NF-κB-expressing tumor cells, Jurkat, HuT-78, HT-29, DU145, and PC3 cells were cotransfected with a reporter plasmid containing an NF-κB-binding site (wild or mutant type) cloned upstream of heat-stable secretory alkaline phosphatase (SEAP) designated as NF-κB-SEAP or NF-κB(mut)-SEAP and green fluorescent protein (GFP) constructs for 3 h using SuperFect reagent (Qiagen, Germany). Cells were cultured for 12 h. Transfection efficiencies for Jurkat, HuT-78, HT-29, DU145, and PC3 cells were found to be 24, 25, 28, 27, and 29%, respectively, measured by GFP-positive cell count. Jurkat cells, stimulated with TNF (10 pM) for 1 h (Jkt/TNF), were cultured for 12 h with other cells. Then the cells were treated with P3-25 for different time periods or 2% DMSO for 12 h. The SEAP activity was assayed in culture supernatant. Results, expressed as fold increase in activity over the nontransfected control, in Figure 1a showed that Jkt/TNF, HuT-78, HT-29, DU145, and PC3 cells induced an 8–9-fold increase in SEAP activity, indicating the activation of NF-κB-dependent SEAP reporter gene. Treatment with DMSO (2% for 12 h, control) did not interfere with the basal SEAP activity in these cells. NF-κB(mut)-SEAP-transfected cells showed no basal SEAP activity in all these cells. P3-25 treatment decreased the basal activity of SEAP in a time-dependent manner in all these cells, suggesting P3-25-mediated downregulation of NF-κB-dependent reporter gene in different cell types.
P3-25 inhibits reporter gene expression dependent on NF-κB-, but not AP-1, and also NF-κB DNA-binding activity in NF-κB-expressing cells. (a) Jurkat, HuT-78, HT-29, DU145, and PC3 cells were transfected with Qiagen superfect transfection reagent for 3 h with plasmids for NF-κB promoter (either wild or mutant) DNA that had been linked to SEAP (NF-κB-SEAP or NF-κB(mut)-SEAP) and GFP. After washing, Jurkat cells were stimulated with 10 pM TNF and then all cells were cultured for 12 h. The GFP-positive cells were counted and transfection efficiency was calculated. Cells were treated with P3-25 (100 nM) for different times or 2% DMSO for 12 h and culture supernatant was assayed for SEAP activity. The results are represented as fold of activation over the nontransfected control. (b) Jkt/TNF (Jurkat cells were stimulated with 10 pM TNF for 1 h), HuT-78, HT-29, DU145, and PC3 cells were treated with P3-25 (100 nM) for different times or 2% DMSO (for Jkt/TNF and HuT-78 cells) for 12 h. The nuclear extracts were prepared and assayed for NF-κB by the gel shift assay. (c) Supershift of NF-κB band. Nuclear extracts, prepared from HuT-78 or DU145 cells, were incubated with different antibodies and cold NF-κB (wild or mutant, 200 ng each) oligonucleotides for 15 min and then assayed for NF-κB. (d) HuT-78 and DU145 cells, transfected with Qiagen superfect transfection reagent for 3 h with plasmids for AP-1 promoter DNA that linked to luciferase reporter gene and GFP, were cultured for 12 h. GFP-positive cells were counted. Cells were treated with P3-25 (100 nM) for different times and curcumin (10 μ M) or 2% DMSO for 12 h and the pellet was extracted and assayed for luciferase activity
P3-25 does not inhibit DNA-binding activity of NF-κB
NF-κB-expressing cells were treated with 100 nM P3-25 for different times and then the DNA-binding activity of NF-κB was measured by a gel shift assay from nuclear extracts. TNF-induced NF-κB binding decreased partially on treatment with P3-25 in a time-dependent manner without interfering with the basal DNA-binding activity of NF-κB (Figure 1b). These data suggest that P3-25 decreases the expression of NF-κB-dependent reporter gene without altering constitutive NF-κB DNA binding.
Nuclear extracts from HuT-78 or DU145 cells were incubated with antibodies (Abs) to p50 and p65 alone or in combination, and then the gel shift assay was conducted to study the specificity and composition of the retarded band. Abs to either subunit of NF-κB shifted the band to a higher molecular weight (Figure 1c), thus suggesting that the retarded complex consisted of both p50 and p65 subunits. Neither preimmune serum nor irrelevant Abs such as anti-c-Rel had any effect on the mobility of NF-κB. This complex completely disappeared in the presence of a 50-fold molar excess of cold NF-κB and was unable to bind with mutant oligonucleotides, indicating its specificity.
P3-25 does not inhibit AP-1-dependent reporter gene expression
HuT-78 and DU145 cells were transfected with plasmids for AP-1 promoter DNA that linked to luciferase (AP-1-Luciferase) and GFP for 3 h. Cells were cultured for 12 h and transfection efficiency determined by GFP-positive cell count was found to be 26 and 27% for HuT-78 and DU145 cells, respectively. Cells were treated with P3-25 for different time periods and with curcumin or DMSO for 12 h. The luciferase activity was assayed in cell extracts. Results, expressed as fold activity over the vector-transfected cells, showed that P3-25 partially inhibited the basal activation of luciferase activity in HuT-78 or DU145 cells (Figure 1d). Curcumin potently inhibited the basal activation of luciferase activity, and DMSO did not interfere in the basal luciferase activity in these cells.
P3-25 blocks ICAM1 and Cox-2 expression
Jkt/TNF, HuT-78, HT-29, DU145, and PC3 cells were treated with P3-25 (100 nM) for different time periods and the amounts of NF-κB-dependent gene products, intercellular adhesion molecule (ICAM) 1 and Cox-2, were analyzed by Western blot technique. The amounts of ICAM1 (Figure 2a) and Cox-2 (Figure 2b) were found to decrease with increasing time of incubation with P3-25. These cells, transfected with Cox-2-luciferase and GFP constructs, showed decreased luciferase activity on treatment with P3-25 in a time-dependent manner (Figure 2c). The amounts of mRNA of Cox-2 and ICAM1 decreased with increasing time of P3-25 treatment in HuT-78 and DU145 cells (Figure 2d and e). Treatment for 12 h with BAY, a selective inhibitor of IκBα kinase (IKK) decreases NF-κB, which completely inhibited the basal expression of ICAM1 or Cox-2, Cox-2-dependent expression of luciferase, and basal levels of Cox-2 or ICAM1 mRNA. All these data suggest that P3-25 downregulates the expression of NF-κB-dependent genes.
P3-25 inhibits expression of ICAM1 and Cox-2. (a and b) Jkt/TNF, HuT-78, HT-29, DU145, and PC3 cells were treated with P3-25 (100 nM) for different times at 37°C. Jkt/TNF and HuT-78 cells were separately treated with 5 μ M BAY 11-7082 (designated as BAY) for 12 h. ICAM1 (a) or Cox-2 (b) was detected from whole-cell extract proteins (100 μg) by Western blot. Tubulin was detected by reprobing both blots. (c) All these cells were cotransfected with vector, Cox-2-Luciferase, and GFP constructs using SuperFect reagent for 3 h. Cells were washed, cultured for 12 h, and counted for GFP-positive cells. Luciferase activity was assayed from whole-cell extracts prepared from P3-25- (for different times) or BAY- (for 12 h) treated cells, considering vector alone value as one fold. (d and e) HuT-78 or DU145 cells were treated with 100 nM P3-25 for different times or 5 μ M BAY for 12 h. Total RNA was isolated and Cox-2, ICAM1, and actin were detected by RT-PCR followed by PCR using Cox-2, ICAM1, and actin-specific primers at 305, 447, and 496 bp bands, respectively
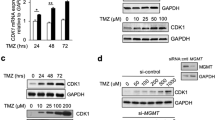
P3-25 induces cell death
NF-κB-expressing cells were treated with P3-25 for 72 h and then cell viability was tested by the MTT (3-(4,5-dimethyl-2-thiozolyl)-2,5-diphenyl-2H-tetrazolium bromide) assay. The cell viability decreased with increasing concentrations of P3-25 in NF-κB-expressing cells (Figure 3a). Treatment with BAY alone showed 25–35% and in combination with P3-25 (100 nM) showed it 70–80% cell death in these cell types. HuT-78 cells were treated with different concentrations of P3-25 or 5 μ M BAY and the cell viability was tested by the ‘Live & Dead’ cell assay. The percentage of dead cells (in red color) increased in a dose-dependent manner on treatment with P3-25 (Figure 3b). These results suggest that P3-25 induces cell death in NF-κB-expressing cells.
P3-25 induces apoptosis. (a) Jkt/TNF, HuT-78, HT-29, DU145, or PC3 cells (5000/well of 96-well plate), cultured for 12 h, were treated with varying concentrations of P3-25 or 5 μ M BAY for 72 h at 37°C, CO2 incubator in triplicate. Then MTT was assayed and absorbance was taken at 570 nm. The results are expressed as inhibition of cell viability measured from the values of mean absorbance of triplicate samples. (b) HuT-78 cells were treated with varying concentrations of P3-25 or 5 μ M BAY for 72 h and percentage of dead cells (red color) were counted using the ‘Live & Dead’ cell assay kit and indicated in mean percentage in bracket from triplicate assays. (c) HuT-78, HT-29, DU145, and PC3 cells were treated with 100 nM P3-25 for different times or 5 μ M BAY for 12 h. Cell extract (0.5 mg) protein, obtained from the pellet by three times freeze–thaw method with water, was used to measure malondialdehyde by TBA-SDS buffer. The data represented increased production of TBA-reactive substances in percentage from one out of three independent experiments. (d) HuT-78, DU145, or PC3 cells were treated with 100 nM P3-25 for different times at 37°C. Cell extracts were prepared and 50 μg proteins were used to detect PARP
P3-25 induces lipid peroxidation and poly-(ADP)-ribose polymerase cleavage
We also examined the effect on lipid peroxidation and poly ADP-ribose polymerase (PARP) cleavage under conditions of P3-25-induced cell death. Constitutive NF-κB-expressing cells were treated with 100 nM P3-25 for different times or 5 μ M BAY for 12 h and then lipid peroxidation was assayed in whole-cell extracts. Treatment with P3-25 induced lipid peroxidation in HuT-78, HT-29, DU145, and PC3 cells in a time-dependent manner (Figure 3c). Cells treated with BAY did not increase lipid peroxidation significantly. P3-25 treatment induced PARP cleavage, as 116 kDa PARP cleaved into 85 kDa protein fragment in a time-dependent manner (Figure 3d). The same blot when reprobed with anti-tubulin antibody showed an equal intensity of bands in different lanes suggesting equal loading of extract proteins. These data suggest that P3-25 is a potent inducer of apoptosis for NF-κB-expressing cells.
P3-25 inhibits PKAα or CKII but not IKK activity
The Jkt/TNF, HuT-78, HT-29, DU145, and PC3 cells were treated with 100 nM P3-25 for different times and then activities of IKK, PKAα, and CKII were measured. The IKK activity marginally decreased in Jkt/TNF cells at 6 h of treatment by P3-25. In other cells, high basal activity of IKK remained unaltered on P3-25 treatment (Figure 4a). BAY-treated Jkt/TNF or HuT-78 cells showed complete inhibition of IKK activity. The activity of PKAα, assayed either by in vitro phosphorylation of GST-p65 protein (Figure 4b) or by kemptide as substrate, decreased in all these cell types (Figure 4c). Pretreatment with BAY did not have an effect on PKA activity in Jkt/TNF or HuT-78 cells. The protein concentrations of PKAα remained unchanged in these cells after P3-25 treatment. The activity of CKII decreased on P3-25 treatment in a time-dependent manner in these cells without altering the amounts of its protein (Figure 4d). BAY treatment did not decrease the activity of CKII in Jkt/TNF or HuT-78 cells. All these constitutively NF-κB-expressing cells had high basal IKK, PKAα, and CKII activities. These results indicate that the treatment of these cells with P3-25 decreases activities of PKAα or CKII, but not of IKK.
P3-25 inhibits activities of PKAα, CKII, NF-AT, and CREB, but not of IKK in NF-κB-expressing cells. Jkt/TNF, HuT-78, HT-29, DU145, and PC3 cells were treated with 100 nM P3-25 for different times. Jkt/TNF and HuT-78 cells were treated with 5 μ M BAY for 6 h. (a) The whole-cell extracts (300 μg) protein was immunoprecipitated with anti-IKKα and IKKβ (1 μg each) antibodies and kinase assayed using GST-IκBα as substrate. The IKKα was assayed from 100 μg protein extract by Western blot. (b–d) The whole-cell extracts (400 μg protein) were immunoprecipated with anti-PKAα or -CKII antibody (1 μg each) and immune complex was used to assay PKAα (b) or CKII (d) using GST-p65 protein (3 μg/lane) as substrate. The levels of PKAα or CKII were assayed from the extract (100 μg protein) by Western blot. The anti-PKAα-immunoprecipitated samples were assayed for PKAα activity using kemptide as substrate (c). (e) The whole-cells extracts (100 μg) from HuT-78 and DU145 were analyzed in 10% SDS-PAGE and detected for phospho-p65 (Ser276 or Ser536) using specific phospho-p65 (Ser276) (e1) or -p65 (Ser536) (e2) antibody. Blots were reprobed with anti-p65 antibody. (f) HuT-78 cells were treated without or with 100 nM P3-25 for 6 h and extracts were immunoprecipitated against anti-PKAα (f1) or CKII (f2) antibody and one half of immunoprecipitated beads were incubated with a mixture containing GST or GST-p65 substrate and ATP. Samples were analyzed in 10% SDS-PAGE followed by Western blots against anti-GST antibody (upper panels). These blots were reprobed with anti-p65 (C-terminal) antibody (middle panels). The other half of immunoprecipitated beads was used for PKAα or CKII assay using GST or GST-p65 substrate and the same extract (100 μg protein) was tested for amounts of PKAα or CKII presented by Western blots (lower panels). (g) HuT-78 and DU145 cells were treated with 100 nM P3-25 for different times and NF-AT was assayed from the nuclear extract (g1). HuT-78 and DU145 cells, transfected with vector, NF-AT-luciferase, and GFP constructs for 3 h by Qiagen SuperFect reagent were cultured for 12 h and GFP-positive cells were counted. Cells were treated with 100 nM P3-25 for different times or 2% DMSO for 24 h. The cell extracts were assayed for luciferase activity. Luciferase activity was expressed as fold of activation (g2), considering vector-transfected cells value as one. (h) HuT-78 and DU145 cells were treated with 100 nM P3-25 for different times or 2% DMSO for 6 h. Nuclear extract (10 μg protein) was assayed for CREB by the gel shift assay. CREB was assayed in presence of 200 ng unlabeled (cold) oligonucleotide
P3-25 decreases phospho-p65 levels
The concentrations of phospho-p65 were measured in whole-cell extracts using anti-phospho-p65 (Ser276) or -phospho-p65 (Ser536) antibody by Western blot in HuT-78 and DU145, after treatment with BAY for 6 h or P3-25 for different time intervals. Both forms of phospho-p65 decreased with increasing time of P3-25 incubation (Figure 4e1 and e2). BAY did not affect phospho-p65 in any of these cells. Upon reprobing those blots with anti-p65 antibody, the amounts of p65 protein were found to be unchanged.
PKAα or CKII does not phosphorylate GST
The extracts of HuT-78 cells, untreated or treated with P3-25 for 6 h, were immunoprecipitated with anti-PKAα or -CKII antibody. The concentration of GST was determined by Western blot technique from one half of immunoprecipitated beads incubated with GST or GST-p65 substrate in the presence of ATP. Bands appeared at 93 kDa (for full length p65 fused with GST), 45 kDa (for IgG, light chain), and 28 kDa (for GST alone) positions for those samples immunoprecipitated with anti-PKAα or -CKII antibody (Figure 4f1 and f2, upper panels). The p65 bands appeared at 93 kDa position by reprobing the same blot (Figure 4f1 and f2, middle panels). The other half of the immunoprecipitated beads, used for assay of PKAα or CKII in vitro, showed no phosphorylation of GST but phosphorylated GST-p65. Treatment with P3-25 inhibited this phosphorylation (Figure 4f1 and f2, lower panels). These results suggest that the PKAα or CKII phosphorylates in vitro GST-p65 (full length), but not GST alone.
P3-25 inhibits NF-ATc or CREB activity
As P3-25 treatment decreased activities of PKAα and CKII, the DNA-binding activities of NF-AT and CREB were measured from nuclear extracts obtained from P3-25-treated HuT-78 and DU145 cells. NF-AT DNA-binding activity decreased with increasing time of P3-25 treatment (Figure 4g1). The luciferase activity decreased in NF-AT-luciferase construct-transfected HuT-78 and DU145 cells with increasing time of P3-25 treatment (Figure 4g2), suggesting P3-25-mediated downregulation of NF-AT. Similarly, CREB DNA-binding activity also decreased with increasing time of P3-25 treatment in HuT-78 and DU145 cells (Figure 4h). Collectively, these results indicate the inhibition of PKAα- and CKII-mediated cellular activities on treatment of cells with P3-25.
P3-25 inhibits expression of NF-κB-dependent reporter gene and activation of PKAα and induces cell death in Jurkat cells
So far, all experiments were carried out in NF-κB-expressing cells. The effect of P3-25 was also tested in cells such as Jurkat cells that showed very low expression of NF-κB and PKAα activity. Jurkat and HuT-78 cells were treated with P3-25 for different time periods and then the DNA-binding activity of NF-κB was assayed. Treatment with P3-25 did not affect DNA binding by NF-κB in HuT-78 cells, but decreased PKAα activity (Figure 5a). A marginal activation of PKAα was observed in Jurkat cells, which was inhibited by P3-25 in a time-dependent manner. It also inhibited the marginal activation of NF-κB-dependent SEAP activity in Jurkat cells transfected with NF-κB-SEAP construct (Figure 5b). As shown earlier, P3-25 inhibited NF-κB-dependent SEAP activity in HuT-78 cells in a time-dependent manner (Figure 5b). The cell viability, tested by MTT dye uptake, was decreased in a time-dependent manner in both Jurkat and HuT-78 cells (Figure 5c). The results suggest that P3-25 also exerts its effect in cell lines having low activity of NF-κB.
P3-25 inhibits marginal activation of PKAα and induces cell death in Jurkat cells. Jurkat and HuT-78 cells were treated with 100 nM P3-25 for different times and DNA-binding activity of NF-κB was assayed from nuclear extracts, and PKAα activation was assayed from whole-cell extracts by using GST-p65 in vitro (a). Jurkat and Hut-78 cells were transfected with NF-κB-SEAP, IκBα-DN, and GFP constructs. Cells were treated with P3-25 for different times; SEAP activity was assayed and indicated as fold activation (b). Cells were treated in triplicate with 100 nM P3-25 for different times and cell viability was assayed by MTT uptake (c)
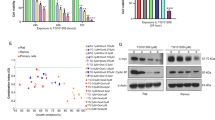
P3-25 potentiates cell death mediated by chemotherapeutic agents
HuT-78, HT-29, DU145, and PC3 cells were treated with 100 nM P3-25 for 4 h and then with chemotherapeutic agents, doxorubicin, taxol, cisplatin, or vincristine (1 μ M each), for 72 h. Cell viability was assayed by the MTT assay. Alone, P3-25 or the chemotherapeutic agents induced about 60% cell death in these cell types. P3-25-pretreated cells showed almost 90% cell death in combination with doxorubicin, taxol, cisplatin, or vincristine (Figure 6a). It appears that P3-25 exerts an additive effect on cell death. P3-25 alone or in combination with different chemotherapeutic agents showed almost similar cell viability in HuT-78 cells as detected by the ‘Live & Dead’ cell assay (Figure 6b).
P3-25 potentiates apoptosis mediated by chemotherapeutic agents. (a) HuT-78, HT-29, DU145, and PC3 cells (5 × 103/well of 96-well plate), incubated for 12 h, were treated with 100 nM P3-25 for 4 h followed by doxorubicin, taxol, cisplatin, or vincristine (1 μ M each) for 72 h at 37°C, in a CO2 incubator. Then, MTT uptake was assayed by absorbance at 570 nm. Inhibition of cell viability was calculated from the mean absorbance values of triplicate samples. (b) HuT-78 cells were treated with 100 nM P3-25 for 4 h followed by treatment with doxorubicin, taxol, or cisplatin (1 μ M each) for 72 h. The number of dead cells (red color) were counted using the ‘Live & Dead’ cell assay kit and indicated in percentage in brackets. (c) PC3 cells were pretreated with 100 nM P3-25 for 4 h and then treated with doxorubicin, taxol, cisplatin, or vincristine (1 μ M each) for 72 h. The cell extracts (50 μg protein) were used to detect PARP by Western blot. The blot was reprobed to detect tubulin by Western blot. (d) DU145 cells were pretreated with varying concentrations of P3-25 for 4 h and then treated with doxorubicin, cisplatin, or taxol (1 μ M each) for 72 h. The PARP was detected from cells extract. Blot was reprobed to detect tubulin by Western blot. (e) Jkt/TNF, HuT-78, HT-29, DU145, and PC3 cells were treated with 100 nM P3-25 for 4 h and then treated with cisplatin (1 μ M) for 72 h. The PARP was detected from the extracts (50 μg proteins) by Western blot. The tubulin was detected after reprobing with anti-tubulin antibody from the same blot
PC3 and DU145 cells were treated with P3-25 (100 nM) for 4 h followed by incubation with doxorubicin, taxol, cisplatin, or vincristine (1 μ M each) for 72 h. The PARP cleavage was detected by Western blot. These agents and P3-25 alone increased the cleaved fragment of PARP at 85 kDa. In P3-25-pretreated cells, the intensity of cleaved fragment increased more than with agents alone in PC3 (Figure 6c) and DU145 cells (Figure 6d), indicating an additive effect in combination with chemotherapeutic agents. The cisplatin-mediated cleavage of PARP protein also showed an additive effect when Jkt/TNF, HuT-78, HT-29, DU145, and PC3 cells were pretreated with P3-25 (Figure 6e). The equal intensity of tubulin from those blots indicated equal loading of the proteins for different treatments. These data suggest that P3-25 shows an additive effect in combination with different chemotherapeutic agents on cell death.
P3-25 downregulates the activation of NF-κB-dependent genes, PKA- or CKII-dependent p65 phosphorylation, IKK activity, and cell death in doxorubicin-resistant MCF-7 cells
Doxorubicin-resistant MCF-7 cells differ from the wild-type cells in having higher expression of caspase 3 and tissue transglutaminase.26 We tested the sensitivity of these cells to P3-25 with respect to the properties of expression of NF-κB-dependent genes – activities of PKAα, CKII, and IKK, and apoptosis. The increased activities of NF-κB-dependent SEAP (Figure 7a) and Cox-2-lucifearse (Figure 7d) in doxorubicin-resistant cells were progressively downregulated with time of incubation in the presence of P3-25. The levels of ICAM1 (Figure 7b) and Cox-2 (Figure 7c) also decreased with time of incubation in doxorubicin-resistant cells. The high basal activities of PKAα and CKII, but not of IKK, observed in doxorubicin-resistant cells, decreased on treatment with P3-25 in a time-dependent manner (Figure 7d). Both methods of MTT assay (Figure 7e) and PARP cleavage (Figure 7f) indicated time-dependent cytotoxicity of P3-25 in doxorubicin-resistant cells. Thus, P3-25 acts by the inhibiting activation of NF-κB-dependent genes and cell death mediated by it follows a pathway different from that of doxorubicin.
P3-25 inhibits the expression of NF-κB-dependent genes, activation of PKA or CKII, and induces apoptosis in doxorubicin-resistant MCF-7 cells. (a) Doxorubicin-resistant MCF-7 cells, cultured in the presence of 2 μ M doxorubicin, transfected with vector, NF-κB-SEAP, and GFP constructs were cultured for 12 h. GFP-positive cells were counted. Cells were treated with P3-25 (100 nM) for different times and the culture supernatant was assayed for SEAP activity. The results represented as fold of activation over the vector-transfected cells. (b) Doxorubicin-resistant cells, cultured in the presence of 2 μ M doxorubicin, were treated with 100 nM P3-25 for different times. The amounts of ICAM1 and Cox-2 were measured from cell extracts by Western blot. As loading control, tubulin was detected by reprobing both blots. (c) Doxorubicin-resistant cells, cotransfected with Cox-2-Luciferase and GFP constructs, were cultured for 12 h and treated with 100 nM P3-25 for different times. Luciferase activity assayed from whole-cell extracts. (d) Doxorubicin-resistant cells were treated with P3-25 for different times and PKAα or CKII was assayed from cell extracts using GST-p65 as substrate; IKK was assayed using GST-IκBα as substrate. From the same extracts, the levels of PKAα, CKII, or IKKα were detected by Western blot. (e) Doxorubicin-resistant cells were treated with 100 nM P3-25 for different times and then cell viability was assayed by MTT dye uptake. Results are represented as inhibition of cell viability in percentage. (f) Doxorubicin-resistant cells were treated with 100 nM P3-25 for different times and PARP was detected from cell extracts by Western blot. The same blot was reprobed for tubulin
Discussion
The present study reinforces the concept that high levels of NF-κB and expression of genes dependent on it confer viability in tumor cells. Indeed, these are the likely factors in the development of their resistance against chemotherapeutic drugs. High basal activities of PKA, CKII, and IKK result in the constitutive expression of NF-κB and other genes involved in tumorigenesis. The thiadiazolidine derivative P3-25, known to block TNF-induced NF-κB activation,25 also blocked the expression of NF-κB-dependent genes without interfering with the consensus DNA-binding activity in NF-κB-expressing cells; it was also found that P3-25 is a potent inhibitor of upstream kinases PKAα and CKII required for phosphorylation of p65. These important findings suggested that P3-25 achieves these effects by controlling phosphorylation activities of upstream kinases and, thereby, expression of NF-κB-dependent genes.
Most of the tumor cells have basal activity of NF-κB. Cells lacking NF-κB cannot survive for long, as NF-κB is required for the function of normal cell cycle. Although the activities of PKAα and NF-κB were very low in Jurkat cells, downregulation of this low basal activity of PKAα and expression of NF-κB-dependent SEAP gene were observed on treatment with P3-25. Involvement of any other pathway in P3-25-mediated cell death in low NF-κB-expressing cells needs further investigation.
Our results indicate that activation of NF-κB-dependent genes is linked with apoptosis. How constitutively NF-κB-expressing cells overcome the apoptotic effect, mediated by several apoptotic inducers including chemotherapeutic agents, is not well understood. Several genes regulated by the activation of NF-κB, including those of the zinc-finger protein A20,27 manganese superoxide dismutase, 28, 29 and cIAP2 (cellular inhibitor for apoptosis), 30 are known to be involved in the inhibition of apoptosis. It is possible that these genes are constitutively expressed in different cancer cells, thus leading to inhibition of apoptosis. Mice, lacking the NF-κB p65 gene, die early in embryonic development from massive cellular death of hepatic parenchyma.31 The antiapoptotic role of NF-κB was also supported by the observation that embryonic fibroblasts from IκB-knockout mice are resistant to TNF.32 Similarly, transfection of a dominant negative form of IκBα complememtary DNA (cDNA) (IκBα-DN) prevented the TNF-induced cell death.33, 34 A sustained level of IKKs is required for constitutive activation of NF-κB.35, 36 Although BAY completely inhibited IKK activity in NF-κB-expressing cells, it showed 30% cell death alone at 72 h of treatment. Lipid peroxidation is an important marker of cell death, which occurs by excessive production of ROS mainly via the mitochondrial pathway. BAY induced cell death by inhibiting IKK and thereby NF-κB without inducing lipid peroxidation, which indicates that BAY may not use the mitochondrial pathway to induce apoptosis. P3-25 and BAY in combination induced almost 75% cell death, indicating that P3-25 works in some way other than inhibition of IKK. In this study, we show that PKAα and CKII are involved in cell survival in NF-κB-expressing or chemotherapeutically resistant cells, and are downregulated by P3-25, thus leading to cell death. How P3-25 downregulates PKAα and CKII needs to be studied further. Several reports indicate that constitutive or induced NF-κB gives resistance to apoptosis stimulated by a wide variety of agents.29, 37, 38, 39 It is possible that the cytotoxic effect of P3-25 on tumor cells is mediated through its suppression of NF-κB. Surprisingly, the NF-κB DNA-binding ability was not altered by P3-25 in constitutively NF-κB-expressing cells. The upstream kinase IKK complex, involved in the activation of NF-κB, was not inhibited by P3-25.
Several genes involved in tumor promotion, such as those of cytokines, Cox-2, metalloproteases, urinary plasminogen activator, and cell surface adhesion molecules, are regulated by NF-κB.40, 41, 42 By blocking expression of NF-κB-dependent gene, P3-25 plays a critical role in exhibiting anticarcinogenic and anti-inflammatory effects. Inhibiting NF-κB by adenoviral IκBα or proteasome inhibitors was found to overcome resistance induced after chemotherapy.37 Therefore, the ability of P3-25 to suppress NF-κB could be exploited by combination with chemotherapy, as recurrence of tumor is common in cancer patients after chemotherapy.
Aspirin was found to be beneficial for preventing colon cancer because of its ability to suppress Cox-2 through NF-κB.43 Similarly, P3-25 may also be beneficial for colon cancer as it inhibits NF-κB-dependent gene expression and the products required for metastasis. NF-κB-inhibitory activity of P3-25 may also have applications for various tumors and may also be useful for other diseases including inflammation and arthritis, where its activation has been shown to mediate pathogenesis.
Materials and Methods
Materials
Glycine, 4-methyl umbelliferyl phosphate, paclitaxol, doxorubicin, cisplatin, vincristine, MTT, kemptide, and anti-tubulin antibody were obtained from Sigma-Aldrich Chemicals (St Louis, MO, USA). Penicillin, streptomycin, neomycin, RPMI-1640 medium, and fetal bovine serum (FBS) were obtained from Life Technologies. Antibodies against p65, IKKα, IKKβ, PKAα, ICAM1, PARP, CKII, and Cox-2 and double-stranded CREB and NF-ATc oligonucleotides were purchased from Santa Cruz Biotechnology, Inc. (Santa Cruz, CA, USA). The ‘Live & Dead’ cell assay kit was obtained from Molecular Probes (Eugene, OR, USA). Plasmids for NF-κB-SEAP, NF-κB(mut)-SEAP, Cox-2-Luciferase, and GFP were kindly supplied by Professor BB Aggarwal of the University of Texas MD Anderson Cancer Center (Houston, TX, USA). P3-25 was prepared from 1-(4-methoxyaryl) thiocarbamide as described previously.25
Cell lines
The cell lines used in this study were as follows: Jurkat (T cell), HuT-78 (modified T cell), HT-29 (colorectal adenocarcinoma), DU145 (prostatic adenocarcinoma), and PC3 (prostatic adenocarcinoma). These cells were obtained from the American Type Culture Collection (Manassas, VA, USA). Doxorubicin-resistant MCF-7 cells were obtained from Professor Kapil Mehta, MD Anderson Cancer Center, Houston, USA. Cells were cultured in RPMI-1640 medium containing 10% FBS, penicillin (100 U/ml), and streptomycin (100 μg/ml). All cells were free from mycoplasma, as detected by the Gen-Probe mycoplasma rapid detection kit (Fisher Scientific, PA, USA).
NF-κB, NF-AT, or CREB activation assay
Activation of NF-κB was determined by EMSA.29 Briefly, cells, after different treatments, were used to prepare cytoplasmic and nuclear extracts. Nuclear extract proteins (8 μg) were incubated with 32P end-labeled double-stranded NF-κB oligonucleotide of HIV-LTR, 5′-TTGTTACAAGGGACTTTCCGCTGGGGACTTTCCAGGGAGGCGTGG-3′, for 30 min at 37°C, and the DNA–protein complex was separated from free oligonucleotide on 6.6% native PAGE. Similarly, NF-AT and CREB binding were assayed using specific double-stranded labeled oligonucleotides. The visualization of radioactive bands was carried out in a PhosphorImager (Fuji, Japan).
NF-κB-dependent SEAP reporter gene assay
Cells were transiently transfected with Qiagen SuperFect transfection reagent (Hilden, Germany) with reporter plasmid containing NF-κB-binding site cloned upstream of heat-stable SEAP designated as NF-κB-SEAP and GFP (0.5 μg. each) constructs for 3 h and cultured for 12 h. GFP-positive cells were counted and indicated for transfection efficiency. Cells were treated with P3-25 for different times. Cell culture-conditioned medium (25 μl) was analyzed for SEAP activity essentially as per the Clontech protocol (Palo Alto, CA) and reported as fold activation with respect to vector-transected cells, as described previously.44
Cox-2-, AP-1-, or NF-AT-dependent luciferase gene transcription assay
The expression of Cox-2-, AP-1-, or NF-AT-dependent luciferase reporter gene was carried out as described previously.45 Cells were transiently transfected with SuperFect transfection reagent containing 0.5 μg of each reporter plasmid containing Cox-2-, AP-1-, or NF-AT-binding site cloned upstream of luciferase (designated as Cox-2-, AP-1-, or NF-AT-Luciferase, respectively) and GFP constructs. After 3 h of transfection, cells were washed and cultured for 12 h followed by treatment with P3-25 for different times. GFP-positive cells were counted. The cell pellets were extracted with lysis buffer (part of the Luciferase assay kit from Promega) and the extracts were incubated with the firefly luciferin (substrate, Promega). Light emission was monitored with a Luminometer and values were calculated as fold of activation over vector-transfected value.
Detection of ICAM1 and Cox2 by semiquantitative RT-PCR
After treatment, total RNA was extracted using TRIzol (Gibco BRL) and 1 μg of total RNA was reverse-transcribed using poly-T oligonucleotide and M-MuLV reverse transcriptase (Invitrogen). The PCR was performed using primers for ICAM1 (5′-AGGGAGGCTCCGTGCTGGTGA-3′, sense primer and 5′-TCAGTGCGGCACGAGAAATTG-3′, antisense primer),46 Cox-2 (5′-TTCAAATGAGATTGTGGGAAAAT-3′, sense primer and 5′-AGATCATCTCTGCCTGAGTATCTT-3′, antisense primer),47 and actin. Following PCR, the amplicons were analyzed by gel electrophoresis with ethidium bromide staining.
IKK assay
The IKK assay was performed by a method described previously.44 Briefly, IKK complex from whole-cell extract (300 μg) was precipitated with anti-IKKα and anti-IKKβ antibodies (1 μg each), followed by incubation with protein A/G-Sepharose beads (Pierce, Rockford, IL). After 2 h of incubation, the beads were washed with lysis buffer and assayed for IKK activity using 2 μg of GST-IκBα (aa 1–54) substrate protein.
Purification of GST-p65 and assay of PKAα and CKII
A GST-p65 (1656 bp) full-length fusion protein was prepared as follows. A double stranded cDNA encoding the p65 full-length flanked by a 5′ BamHI restriction and 3′ stop codon with a XhoI restriction site was synthesized by PCR using the HeLa cDNA library as template and the following oligonucleotide primers: 5′-ATCGGGGATCCGBATGGACGAA CTGTTCCCCCTCATC-3′ and 5′-TAGACTCTCGAGTTAGGAGCTGATCTGACTCAGCAG GG-3′. The amplified product was purified and ligated into BamHI- and XhoI-digested vector pET41b (Novagen). The GST-p65 protein was expressed in expression strain Rossetta (Novagen).
The whole-cell extracts from different treatments were immunoprecipitated with anti-PKAα or -CKII antibody (1 μg each). The immune complex was washed, incubated with 3 μg of GST-p65 substrate protein and 32P-ATP in kinase assay buffer for 30 min at 37°C, and analyzed in 8% SDS-PAGE. The gel was dried and exposed to phosphorimager screen and radioactive bands were detected in PhosphorImager. Immunoprecipitated PKA from cell extracts was incubated with 20 μl of substrate cocktail containing 100 μ M kemptide. The reaction was started by adding 5 μl of the mixture containing 0.5 mM ATP and 10 μCi of 32P-ATP. After incubation, the mixture was spotted onto a streptavidin-coated membrane, washed repeatedly, dried, and counted in a Beta Counter with scintillation fluid.
Cytotoxicity assay
MTT assay
The cytotoxicity was measured by the MTT assay.44 Briefly, cells (1 × 104 cells/well of 96-well plate), cultured for 12 h, were treated with different agents for 72 h and thereafter 25 μl of MTT solution (5 mg/ml in PBS) was added. After 2 h of incubation, 100 μl extraction buffer (20% SDS in 50% dimethylformamide) was added. After an overnight incubation at 37°C, absorbance was red at 570 nm.
Live & dead assay
The cytotoxicity was determined by the Live/Dead assay 44 (Molecular Probes, Eugene, OR, USA). Briefly, after different treatment, 1 × 105 cells were stained with ‘Live & Dead’ cell assay reagent (5 μ M ethidium homodimer, 5 μ M calcein-AM). Red (as dead) and blue (as live) cells were analyzed under a fluorescence microscope (Labophot-2, Nikon, Tokyo, Japan).
Western blot of PARP
Apoptosis was examined by proteolytic cleavage of PARP.14 Briefly, 50 μg whole-cell extracts were resolved on 7.5% SDS-PAGE, electrotransferred onto a nitrocellulose membrane, blotted with mouse anti-PARP antibody, and then detected by chemiluminescence (Amersham Pharmacia Biotech, NJ, USA).
Determination of lipid peroxidation
Lipid peroxidation was determined by measuring thiobarbituric acid-reactive malondialdehyde (MDA), an end product of peroxidation of polyunsaturated fatty acids, as described previously.15, 25
Abbreviations
- BAY:
-
BAY 11-7082
- CKII:
-
casein kinase II
- Cox-2:
-
cyclooxygenase 2
- CREB:
-
cyclic AMP responsive element-binding protein
- GFP:
-
green fluorescent protein
- ICAM:
-
intercellular adhesion molecules
- IKK:
-
inhibitory subunit of kappa B (IκBα) kinase
- MTT:
-
3-(4,5-dimethyl-2-thiozolyl)-2,5-diphenyl-2H-tetrazolium bromide
- NF-ATc:
-
cytoplasmic nuclear factor of activated T cells
- NF-κB:
-
nuclear transcription factor kappa B
- P3-25:
-
5-(4-methoxyarylimino)-2-N-(3,4-dichlorophenyl)-3-Oxo-1,2,4-thiadiazolidine
- PARP:
-
poly ADP-ribose polymerase
- PKA:
-
protein kinase A
- SEAP:
-
secretory alkaline phosphatase
References
Rayet B, Gelinas C . Aberrant rel/nfkb genes and activity in human cancer. Oncogene 1999; 18: 6938–6947.
Karin M, Greten FR . NF-kappaB: linking inflammation and immunity to cancer development and progression. Nat Rev Immunol 2005; 5: 749–759.
Baeuerle PA, Baichwal VR . NF-κB as a frequent target for immuno-suppressive and anti-inflammatory molecules. Adv Immunol 1997; 65: 111–137.
Izeradjene K, Douglas L, Delaney A, Houghton JA . Influence of casein kinase II in tumor necrosis factor-related apoptosis-inducing ligand-induced apoptosis in human rhabdomyosarcoma cells. Clin Canc Res 2005; 10: 6650–6660.
Porter CM, Havens MA, Clipstone NA . Identification of amino acid residues and protein kinases involved in the regulation of NFATc subcellular localization. J Biol Chem 2000; 275: 3543–3551.
Wang D, Westerheide SD, Hanson JL, Baldwin Jr AS . Tumor necrosis factor α-induced phosphorylation of RelA/p65 on Ser529 is controlled by casein kinase II. J Biol Chem 2000; 275: 32592–32597.
Chantome A, Pance A, Gauthier N, Vandroux D, Chenu J, Solary E et al. Casein kinase II-mediated phosphorylation of NF-kappaB p65 subunit enhances inducible nitric-oxide synthase gene transcription in vivo. J Biol Chem 2004; 279: 23953–23960.
Sakurai H, Chiba H, Miyoshi H, Sugita T, Toriumi W . IκB kinases phosphorylate NF-κB p65 subunit on serine 536 in the transactivation domain. J Biol Chem 1999; 274: 30353–30356.
Vermeulen L, Wilde GD, Damme PV, Berghe WV, Haegeman G . Transcriptional activation of the NF-kappaB p65 subunit by mitogen- and stress-activated protein kinase-1 (MSK1). EMBO J 2003; 22: 1313–1324.
Zhong H, Voll RE, Ghosh S . Phosphorylation of NF-kappa B p65 by PKA stimulates transcriptional activity by promoting a novel bivalent interaction with the coactivator CBP/p300. Mol Cell 1998; 1: 661–671.
Delghandi MP, Johannessen M, Moens U . The camp signaling pathway activates CREB through PKA, p38 and MSK1 in NIH 3T3 cells. Cell Sig 2005; 17: 1343–1351.
Wang CY, Cusack Jr JC, Liu R, Baldwin Jr AS . Control of inducible chemoresistance: enhanced anti-tumor therapy through increased apoptosis by inhibition of NF-kappaB. Nat Med 1999; 5: 412–417.
Barkett M, Gilmore TD . Control of apoptosis by Rel/NF-kappaB transcription factors. Oncogene 1999; 18: 6910–6924.
Manna SK, Aggarwal BB . Lipopolysaccharide inhibits TNF-induced apoptosis: role of nuclear factor-B activation and reactive oxygen intermediates. J Immunol 1999; 162: 1510–1518.
Sreenivasan Y, Sarkar A, Manna SK . Mechanism of cytosine arabinoside mediated apoptosis: role of Rel A (p65) dephosphorylation. Oncogene 2003; 22: 4356–4369.
Bhat-Nakshatri P, Sweeney CJ, Nakshatri H . Identification of signal transduction pathways involved in constitutive NF-kappaB activation in breast cancer cells. Oncogene 2002; 21: 2066–2078.
Dai Y, Rahmani M, Dent P, Grant S . Blockade of histone deacetylase inhibitor-induced RelA/p65 acetylation and NF-kappaB activation potentiates apoptosis in leukaemia cells through a process mediated by oxidative damage, XIAP downregulation, and c-Jun-N-terminal kinase 1 activation. Mol Cell Biol 2005; 25: 5429–5444.
Hammer EB, Irminger JC, Rickenbach K, Parnaud G, Ribaux P, Bosco D et al. Activation of NF-kappaB by extracellular matrix is involved in spreading and glucose-stimulated insulin secretion of pancreatic beta cells. J Biol Chem 2005; 280: 30630–30637.
Duffey DC, Chen Z, Dong G, Ondrey FG, Wolf JS, Brown K et al. Expression of a dominant-negative mutant inhibitor-kappaBalpha of nuclear factor-kappaB in human head and neck squamous cell carcinoma inhibits survival, proinflammatory cytokine expression, and tumor growth in vivo. Cancer Res 1999; 59: 3468–3474.
Krappmann D, Emmerich F, Kordes U, Scharschmidt E, Dorken B, Scheidereit C . Molecular mechanisms of constitutive NF-kappaB/Rel activation in Hodgkin/Reed–Sternberg cells. Oncogene 1999; 18: 943–953.
Abdel-Halin AM, Abdel-Aziz RM, El-Dein HS, El-Kafrawy AF . Synthesis and biological activity of some 2-[pyrimidin-2-yl] imino-thiazoalidin-4-one. Ind J Heteroc Chem 1994; 4: 45–50.
Geard C, Bernard B, Bertin E, Cristina De A, Simon LC, Dumas M et al. Synthesis and biological activity of nitro heterocycles analogous to mega zol, a tryopanocidal lead. J Med Chem 2003; 46: 427–440.
Choubey AK, Tripathi AK, Singh R . Synthesis, antifungal and antibacterial activities of some new 2-benzylideneamino-5-arylimino-3-oxo-1, 2, 4-thiadiazolidines. Ind J Chem 1998; 37B: 145–150.
Manna P, Singh R, Narang KK, Manna SK . Synthesis, antifungal, antitumor and anti-inflammatory activities of some new 5-substitutedarylimino-2-N-p-tolylsulphonyl-3-oxo-1, 2, 4-thiadiazolidines. Ind J Heterocycl Chem 2004; 13: 249–252.
Manna P, Narang KK, Manna SK . 1, 2, 4-thiadiazolidine derivative inhibits nuclear transcription factor-κB and its dependent genes activation but induces apoptosis. Int J Cancer 2005; 113: 549–560.
Devarajan E, Chen J, Multani AS, Pathak S, Sahin AA, Mehta K . Human breast cancer MCF-7 cell line contains inherently drug-resistant subclones with distinct genotypic and phenotypic features. Int J Oncol 2002; 20: 913–920.
Heyninck K, Beyaert R . A20 inhibits NF-kappaB activation by dual ubiquitin-editing functions. Trends Biochem Sci 2005; 20: 1–4.
Djavaheri-Mergny M, Javelaud D, Wietzerbin J, Besancon F . NF-kappaB activation prevents apoptotic oxidative stress via an increase of both thioredoxin and MnSOD levels in TNFalpha-treated Ewing sarcoma cells. FEBS Lett 2004; 578: 111–115.
Manna SK, Zhang HJ, Yan T, Oberley LW, Aggarwal BB . Overexpression of Mn-superoxide dismutase suppresses TNF induced apoptosis and activation of nuclear transcription factor-B and activated protein-1. J Biol Chem 1998; 273: 13245–13254.
Hübinger G, Schneider C, Stöhr D, Ruff H, Kirchner D, Schwänen C et al. CD30-induced up-regulation of the inhibitor of apoptosis genes cIAP1 and cIAP2 in anaplastic large cell lymphoma cells. Exper Hematol 2004; 32: 382–389.
Beg AA, Sha, WC, Bronson RT, Ghosh S, Baltimore D . Embryonic lethality and liver degeneration in mice lacking the RelA component of NF-kappa B. Nature 1995; 376: 167–170.
Beg AA, Baltimore D . An essential role for NF-kappaB in preventing TNF-alpha-induced cell death. Science 1996; 274: 782–784.
Van Antwerp DJ, Martin SJ, Kafri T, Green DR, Verma IM . Suppression of TNF-alpha-induced apoptosis by NF-kappaB. Science 1996; 274: 787–789.
Wang CY, Mayo MW, Baldwin Jr AS . TNF- and cancer therapy-induced apoptosis: potentiation by inhibition of NF-kappaB. Science 1996; 274: 784–787.
Gasparian AV, Yao YJ, Kowalczyk D, Lyakh LA, Karseladze A, Slaga TJ et al. The role of IKK in constitutive activation of NF-κB transcription factor in prostatecarcinoma cells. J Cell Sci 2002; 115: 141–151.
Broemer M, Krappmann D, Scheidereit C . Requirement of Hsp90 activity for IkB kinase (IKK) biosynthesis and for constitutive and inducible IKK and NF-κB activation. Oncogene 2004; 23: 5378–5386.
Li Y, Ahmed F, Ali S, Philip PA, Kucuk O, Sarkar FH . Inactivation of nuclear factor kappaB by soy isoflavone genistein contributes to increased apoptosis induced by chemotherapeutic agents in human cancer cells. Cancer Res 2005; 65: 6934–6942.
Sors A, Jean-Louis F, Pellet C, Laroche L, Dubertret L, Courtois G et al. Down-regulating constitutive activation of the NF-{kappa}B canonical pathway overcomes the resistance of cutaneous T cell lymphoma to apoptosis. Blood 2006; 107: 2354–2363.
Dong G, Chen Z, Kato T, Van Waes C . The host environment promotes the constitutive activation of nuclear factor-κB and proinflammatory cytokine expression during metastatic tumor progression of murine squamous cell carcinoma. Cancer Res 1999; 59: 3495–3504.
VonKnethen A, Callsen D, Brune B . Superoxide attenuates macrophage apoptosis by NF-κB and AP-1 activation that promotes cyclooxygenase-2 expression. J Immunol 1997; 163: 2858–2866.
Lee JY, Moon SK, Hwang CW, Nam KS, Kim YK, Yoon HD et al. A novel function of benzyl isothiocyanate in vascular smooth muscle cells: the role of ERK1/2, cell cycle regulation, and matrix metalloproteinase-9. J Cell Physiol 2005; 203: 493–500.
Ruegg C, Mariotti A . Vascular integrins: pleiotropic adhesion and signaling molecules in vascular homeostasis and angiogenesis. Cell Mol Life Sci 2003; 60: 1135–1157.
Esaki M, Matsumoto T, Yao S, Nakamura S, Hirahashi M, Yao T et al. Immunohistochemical characteristics of duodenal adenomas in familial adenomatous polyposis with special reference to cell kinetics. Hum Pathol 2005; 36: 66–73.
Sarkar A, Sreenivasan Y, Ramesh GT, Manna SK . Beta-D-glucoside suppresses TNF-induced activation of nuclear transcription factor kappaB but potentiates apoptosis. J Biol Chem 2004; 279: 33768–33781.
Manna SK, Ramesh GT . Interleukin-8 induces nuclear transcription factor-kB through TRAF6-dependent pathway. J Biol Chem 2005; 280: 7010–7021.
Scholzen TE, Sunderkotter C, Kalden DH, Brzoska T, Fastrich M, Fisbeck T et al. Alpha-melanocyte stimulating hormone prevents lipopolysaccharide-induced vasculitis by down-regulating endothelial cell adhesion molecule expression. Endocrinol 2003; 144: 360–370.
Wu A-W, Gu J, Li Z-F, Ji J-F, Xu G-W . Cox-2 expression and tumor angiogenesis in colorectal cancer. World J Gastroenterol 2004; 10: 2323–2326.
Acknowledgements
The Department of Biotechnology (DBT), Govt of India, supported this work. We duly acknowledge the University Grants Commission, New Delhi, for providing a fellowship to PM, the Department of Science and Technology (DST) for providing SEARC Fast Track proposal for Young Scientists grant to SM, and the Council for Scientific and Industrial Research (CSIR), New Delhi, for providing a fellowship to AS. We thank Drs S Mahalingam, G Ramakrishna, A Sardesai, S Khosla, T Ramasarma, and J Gowrishankar for critically and carefully reading the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by C Borner
Rights and permissions
About this article
Cite this article
Manna, S., Manna, P. & Sarkar, A. Inhibition of RelA phosphorylation sensitizes apoptosis in constitutive NF-kappaB-expressing and chemoresistant cells. Cell Death Differ 14, 158–170 (2007). https://doi.org/10.1038/sj.cdd.4401929
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4401929
Keywords
This article is cited by
-
The diverse and complex roles of NF-κB subunits in cancer
Nature Reviews Cancer (2012)
-
Cyclooxygenase 2-dependent and independent activation of Akt through casein kinase 2α contributes to human bladder cancer cell survival
BMC Urology (2011)
-
RETRACTED ARTICLE: Late phase activation of nuclear transcription factor kappaB by doxorubicin is mediated by interleukin-8 and induction of apoptosis via FasL
Breast Cancer Research and Treatment (2010)
-
Downregulation of Inflammatory Responses by Novel Caffeic Acid Ester Derivative by Inhibiting NF-kappa B
Journal of Clinical Immunology (2009)