Summary:
Considerable evidence in preclinical models as well as in human transplantation now suggests that donor-derived natural killer (NK) cells can contribute to alloimmune recognition of recipient residual tumour cells. This makes the NK cell population an attractive target for in vitro or in vivo manipulations, in order to improve the antitumour effect of allogeneic transplantation. However, conditions in which allogeneic donor cells are collected vary; several reports have emphasised the different phenotypic and functional properties of T cells derived from marrow, cord blood or mobilised peripheral blood grafts; others have demonstrated different clinical outcomes following blood or marrow transplantation after myeloablative conditioning regimens. NK cells have been examined in this setting; the availability of new tools to study the expression of a variety of surface antigens that are involved in the control of NK cell activity offered us an opportunity to extensively characterise the phenotypic properties of NK cells from donors, before and after administration of pharmacological doses of rhG-CSF used for haematopoietic progenitor mobilisation. Our study suggests that rhG-CSF does not reproducibly alter blood NK cell phenotype in normal individuals, and thus that donor-derived cells are fully equipped to exert their potential antitumour effect.
Similar content being viewed by others
Main
Allogeneic transplantation is now widely accepted as an efficient modality of immune intervention to treat patients with poor-prognosis malignancies.1 The graft-versus-leukaemia or graft-versus-tumour (GVT) effect has been well recognised, and involves recognition of residual host tumour cells by donor-derived immune effectors. A number of lines of evidence suggests that T cells play a prominent role: graft-versus-host disease (GVHD) lesions are infiltrated with donor-derived T cells. T-cell depletion results in a sharp diminution in the frequency and severity of GVHD, at the expense of an increase in relapse rate;2 most attempts at manipulating the T-cell compartment have provided equivalent observations, suggesting that the highly desirable goal to dissociate GVHD and GVL through these means will be difficult to achieve.
More recent evidences suggest that natural killer (NK) cells may also contribute to allorecognition of host tumour cells. In murine models, NK cells from fully allogeneic donors support GVT effect, while they do not trigger GVHD following T-cell-depleted transplantation.3 In humans, the experience with haploidentical transplantation has provided a setting to demonstrate that NK cells that are activated as a result of ‘Killer Immunoglobulin like Receptor (KIR) ligand incompatibility’ between donor and recipient contribute to the eradication of residual acute myeloid leukaemia cells, and an improved disease-free survival.4,5 This was further supported by the demonstration that these NK cells can eradicate human leukemic cells that were previously xeno-transplanted in NOD-SCID, and that activated murine NK cells can be used as part of the conditioning regimen to eradicate endogenous haematopoiesis in a murine model of transplantation.5 While the advantage of ‘KIR ligand incompatibility’ was not systematically demonstrated in other transplantation contexts,6,7,8 the positive results observed in recipients of haploidentical transplants have aroused considerable interest in the manipulation of NK cells.
The molecular mechanisms that preside over NK cell activation are increasingly being understood. Key players in this phenomenon are two groups of membrane receptors. NK receptors (NKR) comprise two structurally distinct types of molecules: the CD94/CD159a (NKG2A) heterodimer binds MHC class E molecules on target cells, while KIR molecules constitute a highly polymorphic group of molecules that bind various HLA-A, -B and -C antigens.9 KIR and NKG2 molecules are classified as inhibiting and activating receptors, depending on their intracytoplasmic and trans-membrane domains, while polymorphism in the extracellular domain specifies the recognition of different HLA-A, -B or -C antigens.10 Inhibitory receptors are usually dominant over their activating counterparts, and one of the NKR fundamental roles is to prevent NK cell activation. Another important set of molecules is natural cytotoxicity receptors (NCR): NKp30, NKp44 and NKp46, recognise mostly unidentified ligands and, as a consequence, activate NK cell cytotoxicity.11 In addition, the lectin-like molecule NKG2D participates in NK cell activation; ligands for NKG2-D were recently identified: these are stress molecules such as MIC-A, MIC-B or ULBP/RAET, which are induced on target cells in various situations, including viral infection12 and tumour transformation.13 NK cells express other functionally relevant antigens, including CD16, one of the Fcγ receptors. Low or high levels of the CD56 membrane antigen on CD3− cells distinguish between cytokine secreting and cytotoxic NK cells, respectively.14 NK cells express Pen5 or CD162R, a glycosylated variant of the PSGL-1 molecule that acts as a ligand for selectins.15 They also express costimulatory molecules as well as cytokine receptors. Following activation, cytotoxic NK cells exert their activity through the perforin–granzyme pathway, and induce apoptosis in target cells.
Physicians, who perform allogeneic transplantations, now have the choice of various types of grafts and collection procedures. The use of cord blood (CB) provides a graft with small numbers of haematopoietic progenitors, and thus restricts its use mostly for children. For adults, the use of allogeneic bone marrow (BM) grafts remained the ‘gold standard’, up to a recent period, when the substitution of allogeneic blood cell graft was evaluated, following a myeloablative regimen. The use of either type of graft in this setting produced clearly distinct results: allogeneic aphereses produce a more rapid neutrophil and platelet recovery than marrow grafts, as a consequence of a higher content in CD34+ progenitors. Consequences on GVHD incidence, relapse rate and survival remain controversial,16,17 although a recent meta-analysis of several clinical trials (European Haematology Association Annual Meeting, EHA 8, Geneva, 11–14 June, 2004. Abstract # 265. Allogenic peripheral blood stem cell transplant vs bone marrow transplant in the management of haematological malignancies: an individual patient meta-analysis of nine randomised trials. By the Stem Cell Trialists' group) suggest that allogeneic peripheral blood (PB) cells produce a higher incidence of chronic GVHD as a consequence of a higher content in lymphocytes and – at least for patients at high risk of relapse – produce a better antileukaemic effect and lower rate of relapse.18
In this context, it is important to determine what are the consequences on lymphocyte populations of the use of pharmacological doses of rhG-CSF to mobilise haematopoietic progenitors in donors. Most published reports19,20,21,22,23,24 have focused on T-cell phenotype or function, and suggest that rhG-CSF may truly be an immunomodulator in addition to being a mobilisation agent. Manipulation of the NK cell compartment will require an assessment of the consequences of rhG-CSF exposure on this cell population.
In a previous report,25 we validated a protocol for a detailed phenotypic analysis of donor NK cells, using cryopreserved samples of marrow or blood grafts, and a set of murine monoclonal antibodies directed mostly to NKR. We here present a follow-up of this study, in which we prospectively analysed fresh blood and apheresis samples obtained from normal donors before and after they received rhG-CSF for mobilisation of haematopoietic progenitors.
Materials and methods
Donors and samples
A total of 28 normal donors were sequentially studied for NK cell phenotype. After informed consent, cell samples were sequentially obtained following rhG-CSF administration (apheresis #1, #2), or at a distance from a mobilisation treatment (PB before rhG-CSF infusion, PB, or samples of donor lymphocyte infusion, DLI, obtained before rhG-CSF infusion or between 2 and 28 months after the first rhG-CSF infusion). rhG-CSF (Lenograstim, Chugai, Paris) was given as per institutional protocol (10 μg/kg/day, rounded to a unique daily dose of 600 μg, for 6 days). Aphereses were performed after injections #4 and #5 (apheresis #1, #2, respectively). Owing to the high number of parameters to be studied and the limited number of cells available for each sample, not all parameters were studied on each sample.
As controls, 25 BM samples were obtained during collection for allogeneic transplantation. In total, 25 discarded CB were obtained from the French Network of Cord Blood Banks (RFSP, CB were discarded because of insufficient volume or insufficient number of haematopoietic progenitors, as per procedure). All grafts were analysed for their content of nucleated cells and lymphoid subpopulations by flow cytometry, using standard procedures at our institution.26
For NK cell phenotype studies, EDTA anticoagulated samples were obtained from cell therapy products (aphereses, BM, CB and DLI), or were obtained from the donor through vein puncture (PB). Mononuclear cells were recovered after Ficoll density gradient centrifugation and processed for flow cytometry analysis within 24 h.
Antibodies and flow cytometry
The following mouse mAb were used in this study: PE-conjugated anti-CD56 (IgG1, N901), anti-CD158a/h (IgG1, EB6), anti-CD158b1/b2/j (IgG1, GL183), anti-CD158e1/e2 (IgG1, Z27), anti-CD158i (IgG2a, FES172), anti-CD94 (IgG2a, HP3B1), anti-CD159a (IgG2b, Z199), anti-NKG2D (IgG1, 149810), anti-NKp30 (IgG1, Z25), anti-NKp46 (IgG1, BAB281), anti-TCRVα24 (IgG1, C15), uncoupled anti-CD162R (IgM, 5H10.21.5)+PE-conjugated goat-anti-mouse IgM (polyclonal), FITC-conjugated anti-CD3 (IgG1, UCHT1), PC5-conjugated anti-CD16 (IgG1, 3G8) and anti-CD56 (IgG1, N901). These mAb and their isotype-matched negative control mAb were purchased from Beckman Coulter Immunotech (Marseille, France) except for NKG2D mAb, purchased from R&D systems (Lille, France). It is important to note that, except for FES172 – anti-CD158i – which recognises a KIR identified only as an activating receptor, antibodies directed against other KIR molecules (anti-CD158a/h, anti-CD158b1/b2/j and anti-CD158e1/e2) do not discriminate between activating and inhibiting isoforms of the molecules. For intracellular staining, the following PE-coupled mAb were used: anti-perforin mAb (IgG2b, δG9), purchased from Becton Dickinson Pharmingen (San Diego, USA) and anti-granzyme B (IgG1, GB11) from Serotech (Oxford, UK).
NK cells were identified as CD3−//CD56/CD16+ or CD3−/CD56+ cells, with low FSC and SSC, using three-colour flow cytometry and FITC-labelled anti-CD3, PC5-labelled anti-CD56 and anti-CD16 mAbs. Subsequently, we separately analysed the CD56bright and CD56dim NK cell subsets for NCR (NKp30, NKp46), NKG2D, CD162R, perforin and granzyme B expression; cells were labelled with specific PE-labelled anti-NK mAb, FITC-labelled anti-CD3 and PC5-labelled anti-CD56 mAb (CD16 mAb was no longer utilised in this set of experiments). The pelleted cells were analysed with a FACSCalibur flow cytometer (Becton Dickinson Immunocytometry System). Data were analysed using the CellQuest™ software (BD). At least 10 000 events were collected in the CD3−//CD16+/CD56+ (NKR phenotype) or CD3+/CD56+ lymphocyte gate. Absolute NK cell numbers were computed from the total numbers of viable mononuclear cells, the percentage of lymphocytes in the graft sample and the percentage of NK cells within the lymphocyte gate.
Intracellular perforin and granzyme B were detected on EDTA anti-coagulated samples, using the IntraPrep permeabilisation reagent (Beckman-Coulter-Immunotech) following the manufacturer's recommendations. Briefly, fresh mononuclear cells were first stained with PE-labelled anti-CD56 and FITC-labelled anti-CD3 (or isotype-matched negative control) mAbs, in PBS supplemented with 5% foetal calf serum. After washing, pelleted cells were fixed and permeabilised, before intracellular staining with PE-conjugated anti-granzyme B or anti-perforin mAbs. Data acquisition and analysis were performed as described above.
For NCR, NKG2D, perforin and granzyme B, we calculated a ‘specific fluorescence intensity (sMFI)’13 for total NK, CD56bright and CD56dim NK cells sequentially obtained from normal donors. We defined sMFI as the ratio of the MFI of the considered population (NK, CD56bright and CD56dim NK cells) stained with a given relevant mAb, over the MFI of the same population stained with the appropriate isotypic control mAb.
Statistical analyses
Comparisons between unpaired values were carried out using either the Student t-test or the Mann–Wittney U-test, depending on the numbers of observations. Descriptive statistics and comparisons were computed with the Statview® software for Macintosh computers.
Results
Variations in NK cell number and phenotype in CB, adult BM and adult PB
As previously described,25 the absolute numbers of NK cells defined as CD3−//CD16+/CD56+ cells, differ in CB, BM or adult PB cell therapy products. This is mostly the result of a higher number of cells in aphereses than in BM and CB. The percentage of NK cells within the lymphocyte subpopulation in CB is approximately twice the value observed for BM (P=0.0108) and apheresis samples (P=0.0066), NK cell frequency being similar in adult cell therapy products (Figure 1a). However, the low cellular content of CB units results in a lower absolute number of NK cells in this type of allogeneic graft. The relative proportion of CD56dim and CD56bright NK cells is not statistically different in the three types of graft (Figure 1b). The CD162R molecule is expressed on fewer NK cells in BM than in mobilised PB (P=0.0109), with intermediate values for CB. Among NKR, CD94+ and CD159a+ (NKG2A) were expressed at significantly higher levels on CB NK cells than on adult counterparts (P<0.05), while no reproducible difference was detected for KIR expression. This observation is of interest because CD159a is associated with CD94 as an heterodimer at the cell surface to form an inhibitory receptor, which antibodies can discriminate from the activating counterpart (contrary to most antibodies directed against KIR molecules).
NK cells in allogeneic products from different origins. (a) Frequency of CD3−CD16+CD56+ NK cells within the lymphocyte compartment of cord blood (CB), bone marrow (BM) and apheresis products (AP). (b) Relative proportion of CD56dim NK cell subset within the total CD3−CD56+ NK cell population. (c) CD162R expression on CD56dim cells.
Sequential follow-up of normal donors treated with rhG-CSF reveals no significant change in NK cell phenotype
Apheresis products obtained after rhG-CSF-induced mobilisation represent an abundant source of NK cells and are now widely used in the allogeneic setting. In order to evaluate the consequences of rhG-CSF administration, we sequentially analysed donor NK cells: at steady state, in PB samples obtained before rhG-CSF treatment or at a distance from this treatment in DLI samples, and after 4 and 5 rhG-CSF injections (aphereses #1 and #2, respectively). In seven out of eight donors studied, we observed a nonsignificant decrease in NK cell (CD3−/CD56+) frequencies among lymphocytes, before and after rhG-CSF administration (15.0±6.8, 9.4±4.7 and 8.9±5.7% for PB, aphereses #1 and #2, respectively; P=0.07).
As expected,15 most CD56dim NK cells expressed high levels of the CD162R, a highly NK cell-specific post translational modification of PSGL-1; this was unchanged after rhG-CSF administration. A minority of CD56bright NK cells expressed low levels of CD162R, with a nonsignificant increase for aphereses 1 and 2 (19.1±10.4; 26.9 +12.7 and 31.2±14.4% for PB, apheresis #1 and apheresis #2, respectively; n=7, P>0.05).
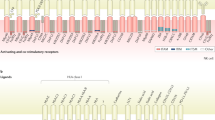
The percentage of NKR+ – CD94/NKG2A+ and KIR+ – cells within the CD3−//CD56+/CD16+ subset was not reproducibly modified by G-CSF mobilisation (Figure 2a and b). We also analysed the density of CD158i (KIR2DS4) – a KIR molecule known for its activating function – expression at the cell surface. Consistent with the known polymorphism for KIR molecules, NK cells expressed CD158i only in certain individuals (11/23). For three CD158i+ normal donors that we studied before and after rhG-CSF infusion (# 5, 9 and 12), the CD158i expression profile was unchanged before and during G-CSF mobilisation.
rhG-CSF administration does not modify NKR expression. (a) Individual follow-up of NKR expression at the surface of CD3−//CD16+/CD56+ NK cells in 10 normal donors comparing steady state (PB sample before rhG-CSF administration or donor lymphocyte infusion sample obtained before rhG-CSF infusion or between 2 and 28 months after the first rhG-CSF infusion, SS) vs apheresis #1 and #2 (Aph #1 and #2). (b) Mean values for expression of NKR following rhG-CSF infusion in the same 10 normal donors. (c) Sequential analysis of NKR expression on CD3+//CD16+/CD56+ T cells for eight of the 10 previous normal donors.
Sequential analyses showed that rhG-CSF administration does not modify the percentage of NKp30+, NKp46+ or NKG2D+ cells in total NK cells (Figure 3a) from normal donors, nor within the CD56bright or CD56dim subsets (Figure 3b). Since the cytolytic activity of NK cells has been reported to depend upon the level of NCR expression,27 we studied whether these cell surface receptor densities were modified by rhG-CSF infusion: no significant modulation of expression level was observed for any of the three receptors.
As expected, NK cells from normal donors constitutively express perforin and granzyme B in their intracytoplasmic granules. Consistent with their known and distinct functions, all CD56dim NK cells expressed cytolytic enzymes, while CD56bright NK cells were more heterogeneous for both markers. rhG-CSF infusion did neither reproducibly modify the proportion (Figure 4a), nor the expression level (Figure 4b) of perforin and granzyme B. As for previously analysed markers (Figures 2 and 3), we observed individual variations following rhG-CSF administration, but these variations were not reproducible. Finally, it was not possible to correlate the mobilisation procedure with a significant modulation of perforin and granzyme B expression.
Sequential analysis of granzyme B and perforin expression before (PB) and after (apheresis #1 and apheresis #2) rhG-CSF infusion. (a) Percentage of CD56bright (CD3−/CD56++), CD56dim (CD3−/CD56+) NK cell subsets and CD56+ T cells (CD3+ CD56+) that express designated molecules. (b) To analyse the expression level for those two markers, we calculated a ‘specific median fluorescence intensity (sMFI)’ index for total NK (not shown), CD56bright, CD56dim NK cells and CD56+ T cells sequentially obtained from four normal donors. sMFI is the ratio of the mean fluorescence intensity of the considered population (NCD56bright, CD56dim NK cells and CD56+ T cells) stained with a given anticytotoxic enzyme mAb, over the median fluorescence intensity of the same population stained with the appropriate isotypic control mAb (see Materials and methods).
CD3+//CD56+/CD16+ and CD3+/CD56+ T cells subsets in allogeneic grafts of different origin
A proportion of CD3+ T cells express NK cell markers, including CD16, CD56 and also NKR and NKG2D. True NK T cells that express Vα24 represent only a subset of those populations. As for CD3− cells, we carried out a detailed phenotypic analysis of CD3+ cells. Mobilised PB grafts contain a significantly higher frequency of CD3+//CD56+/CD16+ lymphocytes than BM and CB (1.5-fold, P=0.0389, and 1.9-fold-P=0.0033, respectively).
Contrary to what we observed for NK cells, CD94 and CD159a (NKG2A) were significantly less expressed on CD3+//CD56+/CD16+ cells from CB compared to aphereses and BM (not shown). No other difference was detected in the expression of NKR molecules, when comparing the three types of allogeneic graft.
Similar to what we observed for NK cell analysis, rhG-CSF administration was associated with a nonsignificant decrease (20–25%) in the frequency of CD3+//CD56+/CD16+ lymphocytes. Sequential analyses of CD3+ cells that coexpress CD56 did not reveal any significant change in NKR (Figure 2c) or in NKG2D (Figure 3c) expression following rhG-CSF administration. Expression of NKp30 and NKp46 was basically undetectable in this cell population (n=21 – not shown).
Finally, 70.9±15.9% and 59.5±18.9% of unmobilised PB CD56+ T cells displayed detectable expression of perforin and granzyme B, respectively. The proportion of the perforin+ subset decreased in apheresis products for the four analysed donors (Figure 4a), while granzyme B expression profile was not reproducibly modified (Figure 4a and b). Interestingly, only a small subset of CD3+/CD56− T cells expressed perforin and granzyme B (7.5±6.2 and 9.8±3.5%, respectively).
Discussion
We performed a detailed analysis of NK cells that were obtained from normal donors in various conditions. The study focused on recently identified receptors that were shown to be involved in NK cell activation. As already demonstrated, NK cell numbers vary between adult PB, adult BM and CB allogeneic grafts, mostly as a result of different numbers of total cells in these different cell therapy products. However, the phenotype of NK cells essentially remains the same in these three different categories of samples, with the exception of a higher expression of CD94 and CD159a on CB cells.
Most importantly, the sequential follow-up of normal donors, who received pharmacological doses of rhG-CSF for progenitor cell mobilisation, revealed no significant change in membrane receptor expression, or in the presence of intracytoplasmic perforin or granzyme B. While interindividual variations in NKR and NCR expression may mask small changes in the expression level of these receptors, no reproducible pattern emerged to support a major effect of rhG-CSF. Another limitation associated with phenotypic studies is the inability of many currently available antibodies to discriminate between inhibiting and activating forms of NKR. Despite these limitations, our data suggest that rhG-CSF does not significantly affect NK cell phenotype, and thus that NK cells obtained from allogeneic aphereses are fully equipped for in vitro selection or activation. Although we did not perform functional assays, and several mechanisms account for the antitumour effect of NK cells,28 the flow cytometric evaluation of perforin and granzyme expression provides an insight on the cytolytic ability of NK cells.
Immunomodulatory effects associated with rhG-CSF used for progenitor cell mobilisation have been described in a number of studies.19,20,21,22,23,25 While results vary between studies, the influence of rhG-CSF has been reported on monocytes,21 T cells21,22,23 and NK cells.20,22,23 There are contradictory reports on changes in the absolute numbers of NK cells and their proportion within total lymphocytes, following rhG-CSF administration.20,22,23,29,30,31,32,33 Functional assays produced equally contradictory results,31,33,34,35,36,37,38 although in most instances impaired natural cytotoxic activity against NK-sensitive cell lines was evidenced after rhG-CSF treatment. Two studies reported a decreased expression of proinflammatory cytokines such as IFN-γ, IL-2 and TNF-α31,39 after rhG-CSF mobilization; interestingly, they observed no change in perforin, Fas and Fas-ligand expression on allogeneic NK cells, a result consistent with our observations.
There is no evidence that NK cells express the G-CSF receptor. In addition, no effect of G-CSF has been documented in a variety of in vitro assays, using either selected or unselected NK cells35,40; the latter observation suggests that other accessory mononuclear cells do not mediate an indirect effect that would change NK cell functions. There is one report41 however in patients with aplastic anaemia, particularly those treated with rhG-CSF, that suggests that neutrophils may interact directly with NK cells to reduce their cytolytic activity.
Several groups17,33,35,39 already demonstrated that rhG-CSF administration in vivo had no effect on the expression of CD2, CD7, CD8, CD16, CD25, CD94, CD161 and NKB1 receptors on PB NK cells. There is only one report that suggest a downmodulation of CD56 cell surface density, on both CD56bright/CD3− cells and CD56dim/CD3− cells.41 No report has provided an extensive evaluation of functionally important NK cell receptors. Our study extends previous observations, and confirms that administration of rhG-CSF to healthy donors does not alter the phenotype of PB NK cells.
While rhG-CSF has no or little effect on the phenotype of mature NK cells, another hypothesis is that it may compromise the ability of haematopoietic progenitors to differentiate towards the NK lineage. The addition of rhG-CSF to cultures impairs the NK cell differentiation of both PB and BM CD34+ Lin− DR− cells.20 However, in appropriate culture conditions, immunoselected mobilized PB CD34+ cells can differentiate in vitro into NK cells.42 This is further confirmed by clinical results in recipients of haploidentical transplantation: NK cells that rapidly arise from the donor T-cell-depleted graft after transplantation are able to mediate antitumour activity in case of KIR ligand incompatibility.
Together with published data, our results suggest the absence of a major impact of rhG-CSF administration on the phenotype of NK cells. Thus, ex vivo manipulation of the mature NK cell compartment from these cell therapy products appears feasible.
References
Gratwohl A, Baldomero H, Passweg J et al. Hematopoietic stem cell transplantation for hematological malignancies in Europe. Leukemia 2003; 17: 941–959.
Maraninchi D, Gluckman E, Blaise D et al. Impact of T-cell depletion on outcome of allogeneic bone-marrow transplantation for standard-risk leukaemias. Lancet 1987; 2: 175–178.
Asai O, Longo DL, Tian ZG et al. Suppression of graft-versus-host disease and amplification of graft-versus-tumor effects by activated natural killer cells after allogeneic bone marrow transplantation. J Clin Invest 1998; 101: 1835–1842.
Ruggeri L, Capanni M, Casucci M et al. Role of natural killer cell alloreactivity in HLA-mismatched hematopoietic stem cell transplantation. Blood 1999; 94: 333–339.
Ruggeri L, Capanni M, Urbani E et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science 2002; 295: 2097–2100.
Davies SM, Ruggieri L, DeFor T et al. Evaluation of KIR ligand incompatibility in mismatched unrelated donor hematopoietic transplants. Killer immunoglobulin-like receptor. Blood 2002; 100: 3825–3827.
Giebel S, Locatelli F, Lamparelli T et al. Survival advantage with KIR ligand incompatibility in hematopoietic stem cell transplantation from unrelated donors. Blood 2003; 102: 814–819.
Lowe EJ, Turner V, Handgretinger R et al. T-cell alloreactivity dominates natural killer cell alloreactivity in minimally T-cell-depleted HLA-non-identical paediatric bone marrow transplantation. Br J Haematol 2003; 123: 323–326.
Moretta A, Vitale M, Bottino C et al. P58 molecules as putative receptors for major histocompatibility complex (MHC) class I molecules in human natural killer (NK) cells. Anti-p58 antibodies reconstitute lysis of MHC class I-protected cells in NK clones displaying different specificities. J Exp Med 1993; 178: 597–604.
Ciccone E, Pende D, Viale O et al. Involvement of HLA class I alleles in natural killer (NK) cell-specific functions: expression of HLA-Cw3 confers selective protection from lysis by alloreactive NK clones displaying a defined specificity (specificity 2). J Exp Med 1992; 176: 963–971.
Mandelboim O, Lieberman N, Lev M et al. Recognition of haemagglutinins on virus-infected cells by NKp46 activates lysis by human NK cells. Nature 2001; 409: 1055–1060.
Bauer S, Groh V, Wu J et al. Activation of NK cells and T cells by NKG2D, a receptor for stress-inducible MICA. Science 1999; 285: 727–729.
Salih HR, Antropius H, Gieseke F et al. Functional expression and release of ligands for the activating immunoreceptor NKG2D in leukemia. Blood 2003; 102: 1389–1396.
Cooper MA, Fehniger TA, Turner SC et al. Human natural killer cells: a unique innate immunoregulatory role for the CD56 (bright) subset. Blood 2001; 97: 3146–3151.
Andre P, Spertini O, Guia S et al. Modification of P-selectin glycoprotein ligand-1 with a natural killer cell-restricted sulfated lactosamine creates an alternate ligand for L-selectin. Proc Natl Acad Sci USA 2000; 97: 3400–3405.
Mohty M, Kuentz M, Michallet M et al. Chronic graft-versus-host disease after allogeneic blood stem cell transplantation: long-term results of a randomized study. Blood 2002; 100: 3128–3134.
Ringden O, Labopin M, Bacigalupo A et al. Transplantation of peripheral blood stem cells as compared with bone marrow from HLA-identical siblings in adult patients with acute myeloid leukemia and acute lymphoblastic leukemia. J Clin Oncol 2002; 20: 4655–4664.
Cutler C, Giri S, Jeyapalan S et al. Acute and chronic graft-versus-host disease after allogeneic peripheral-blood stem-cell and bone marrow transplantation: a meta-analysis. J Clin Oncol 2001; 19: 3685–3691.
Gyger M, Stuart RK, Perreault C . Immunobiology of allogeneic peripheral blood mononuclear cells mobilized with granulocyte-colony stimulating factor. Bone Marrow Transplant 2000; 26: 1–16.
Miller JS, Prosper F, McCullar V . Natural killer (NK) cells are functionally abnormal and NK cell progenitors are diminished in granulocyte colony-stimulating factor-mobilized peripheral blood progenitor cell collections. Blood 1997; 90: 3098–3105.
Mielcarek M, Graf L, Johnson G, Torok-Storb B . Production of interleukin-10 by granulocyte colony-stimulating factor-mobilized blood products: a mechanism for monocyte-mediated suppression of T-cell proliferation. Blood 1998; 92: 215–222.
Rondelli D, Raspadori D, Anasetti C et al. Alloantigen presenting capacity, T cell alloreactivity and NK function of G-CSF-mobilized peripheral blood cells. Bone Marrow Transplant 1998; 22: 631–637.
Tayebi H, Kuttler F, Saas P et al. Effect of granulocyte colony-stimulating factor mobilization on phenotypical and functional properties of immune cells. Exp Hematol 2001; 29: 458–470.
Joshi SS, Lynch JC, Pavletic SZ et al. Decreased immune functions of blood cells following mobilization with granulocyte colony-stimulating factor: association with donor characteristics. Blood 2001; 98: 1963–1970.
Pascal V, Brunet C, Pradel V et al. Analysis of donor NK and T cells infused in patients undergoing MHC-matched allogeneic hematopoietic transplantation. Leukemia 2002; 16: 2259–2266.
Olivero S, Novakovitch G, Ladaique P et al. T-cell depletion of allogeneic bone marrow grafts: enrichment of mononuclear cells using the COBE Spectra cell processor, followed by immunoselection of CD34+ cells. Cytotherapy 1999; 1: 469–477.
Spaggiari GM, Carosio R, Pende D et al. NK cell-mediated lysis of autologous antigen-presenting cells is triggered by the engagement of the phosphatidylinositol 3-kinase upon ligation of the natural cytotoxicity receptors NKp30 and NKp46. Eur J Immunol 2001; 31: 1656–1665.
Hayakawa Y, Takeda K, Yagita H et al. Critical contribution of IFN-gamma and NK cells, but not perforin-mediated cytotoxicity, to anti-metastatic effect of alpha-galactosylceramide. Eur J Immunol 2001; 31: 1720–1727.
Sica S, Rutella S, Di Mario A et al. rhG-CSF in healthy donors: mobilization of peripheral hemopoietic progenitors and effect on peripheral blood leukocytes. J Hematother 1996; 5: 391–397.
Martinez C, Urbano-Ispizua A, Rozman C et al. Effects of G-CSF administration and peripheral blood progenitor cell collection in 20 healthy donors. Ann Hematol 1996; 72: 269–272.
Joshi SS, Lynch JC, Pavletic SZ et al. Decreased immune functions of blood cells following mobilization with granulocyte colony-stimulating factor: association with donor characteristics. Blood 2001; 98: 1963–1970.
Gurman G, Dilek I, Arslan O et al. The effect of G-CSF on lymphocyte subsets and CD34+ cells in allogeneic stem cell transplantation. Transfus Apheresis Sci 2001; 24: 23–28.
Trzonkowski P, Zaucha JM, Mysliwska J et al. Differences in kinetics of donor lymphoid cells in response to G-CSF administration may affect the incidence and severity of acute GvHD in respective HLA-identical sibling recipients. Med Oncol 2004; 21: 81–94.
Silva MR, Parreira A, Ascensao JL . Natural killer cell numbers and activity in mobilized peripheral blood stem cell grafts: conditions for in vitro expansion. Exp Hematol 1995; 23: 1676–1681.
Miller JS, Prosper F, McCullar V . Natural killer (NK) cells are functionally abnormal and NK cell progenitors are diminished in granulocyte colony-stimulating factor-mobilized peripheral blood progenitor cell collections. Blood 1997; 90: 3098–3105.
Rondelli D, Raspadori D, Anasetti C et al. Alloantigen presenting capacity, T cell alloreactivity and NK function of G-CSF-mobilized peripheral blood cells. Bone Marrow Transplant 1998; 22: 631–637.
Gazitt Y . Immunologic profiles of effector cells and peripheral blood stem cells mobilized with different hematopoietic growth factors. Stem Cells 2000; 18: 390–398.
Gazitt Y, Shaughnessy P, Devore P . Mobilization of dendritic cells and NK cells in non-Hodgkin's lymphoma patients mobilized with different growth factors. J Hematother Stem Cell Res 2001; 10: 177–186.
Tayebi H, Kuttler F, Saas P et al. Effect of granulocyte colony-stimulating factor mobilization on phenotypical and functional properties of immune cells. Exp Hematol 2001; 29: 458–470.
Durek C, Schafer I, Braasch H et al. Effects of colony-stimulating factors on cellular cytotoxicity. Cancer Immunol Immunother 1997; 44: 35–40.
Taga T, Kariya Y, Shimada M, Uchida A . Suppression of natural killer cell activity by granulocytes in patients with aplastic anemia: role of granulocyte colony-stimulating factor. Immunol Lett 1993; 39: 65–70.
Takenaka K, Mizuno SI, Harada M et al. Generation of human natural killer cells from peripheral blood CD34+ cells mobilized by granulocyte colony-stimulating factor. Br J Haematol 1996; 92: 788–794.
Acknowledgements
We thank Eric Vivier, Pascale Paul and Pascale André for stimulating discussions, all personnel at the Centre de Thérapie Cellulaire et Génique and Cord Blood Bank (RFSP), especially Thierry Alario, for their dedication to conduct flow cytometry analyses. This work was supported in part by Institut Paoli-Calmettes, and by a grant from Inserm and Ministèro de la Recherche (Action BioIngénierie # 91) to Institut Paoli-Calmettes.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lassailly, F., Sielleur, I., Blaise, D. et al. rhG-CSF does not affect the phenotype of adult donor peripheral blood NK cells. Bone Marrow Transplant 35, 25–32 (2005). https://doi.org/10.1038/sj.bmt.1704711
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1704711