Abstract
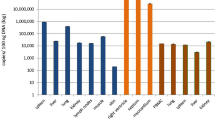
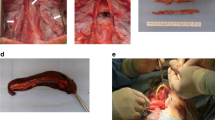
Thrombotic microangiopathy (TM) is a serious complication of bone marrow transplantation (BMT) that resembles thrombotic thrombocytopenic purpura (TTP). In attempting to achieve hematopoietic cell chimerism in the pig-to-baboon model, we have observed TM following infusion of high doses (>1010 cells/kg) of porcine peripheral blood mobilized progenitor cells (PBPC) into baboons. We performed investigations to analyze the pathobiology of this TM and to test therapeutic interventions to ameliorate it. PBPC were obtained by leukapheresis of cytokine-stimulated swine. The initial observations were made in two baboons that underwent a non-myeloablative regimen (NMR) prior to PBPC transplantation (TX) (group 1). We then studied three experimental groups. Group 2 (n = 2) received NMR without PBPC TX. Group 3 (n = 2) received PBPC TX alone. Group 4 (n = 6) received NMR + PBPC TX combined with prostacyclin, low-dose heparin, methylprednisolone, and cyclosporine was replaced by anti-CD40L mAb in five cases. Baboons in groups 1 and 3 developed severe thrombocytopenia (<10 000/mm3), intravascular hemolysis with schistocytosis (>10/high powered field (hpf)), increase in plasma lactate dehydrogenase (LDH) (2500–9000 U/l), transient neurologic changes, renal insufficiency, and purpura. Autopsy on two baboons confirmed extensive platelet thrombi in the microcirculation, and, similar to clinical BMT-associated TM/TTP, no unusually large vWF multimers or changes in vWF protease activity were observed in the plasma of baboons with TM. In group 2, self-limited thrombocytopenia occurred for 10–15 days following NMR. Group 4 baboons developed thrombocytopenia (<20 000/mm3) rarely requiring platelet transfusion, minimal schistocytosis (<3/hpf), minor increase in LDH (<1000 U/l), with no clinical sequelae. We conclude that high-dose porcine PBPC infusion into baboons induces a microangiopathic state with vWF biochemical parameters resembling clinical BMT-associated TM/TTP and that administration of antithrombotic and anti-inflammatory agents can ameliorate this complication. Bone Marrow Transplantation (2001) 27, 1227–1236.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Pettitt AR, Clark RE . Thrombotic microangiopathy following bone marrow transplantation Bone Marrow Transplant 1994 14: 495–504
Rock GA, Shumak KH, Buskard NA et al. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura New Engl J Med 1991 325: 393–397
Tsai HM, Lian EC . Antibodies to von Willebrand factor-cleaving protease in acute thrombotic thrombocytopenic purpura New Engl J Med 1998 339: 1585–1594
Furlan M, Robles R, Galbusera M et al. Von Willebrand factor-cleaving protease in thrombotic thrombocytopenic purpura and the hemolytic-uremic syndrome New Engl J Med 1998 339: 1578–1584
Moake JL, Rudy CK, Troll JH et al. Unusually large plasma factor VIII: von Willebrand factor multimers in chronic relapsing thrombotic thrombocytopenic purpura New Engl J Med 1982 307: 1432–1435
Van der Plas RM, Schiphrost ME, Huizinga EG et al. Von Willebrand factor proteolysis is deficient in classic, but not in bone marrow transplantation-associated thrombotic thrombocytopenic purpura Blood 1999 93: 3798–3802
Sharabi Y, Abraham VS, Sykes M, Sachs DH . Mixed allogeneic chimeras prepared by a non-myeloablative regimen: requirement for chimerism to maintain tolerance Bone Marrow Transplant 1992 9: 191–197
Sharabi Y, Aksentijevich I, Sundt TM et al. Specific tolerance induction across a xenogeneic barrier: production of mixed rat/mouse lymphohematopoietic chimeras using a nonlethal preparative regimen J Exp Med 1990 172: 195–202
Kawai T, Cosimi AB, Colvin RB et al. Mixed allogeneic chimerism and renal allograft tolerance in cynomolgus monkeys Transplantation 1995 59: 256–262
Bartholomew AM, Cosimi AB, Sachs DH et al. A study of tolerance in a concordant xenograft model Transplant Proc 1997 29: 923–924
Kozlowski T, Monroy R, Xu Y et al. Anti-αGal antibody response to porcine bone marrow in unmodified baboons and baboons conditioned for tolerance induction Transplantation 1998 66: 176–182
Kozlowski T, Shimizu A, Lambrigts D et al. Porcine kidney and heart transplantation in baboons undergoing a tolerance induction regimen and antibody adsorption Transplantation 1999 67: 18–30
Cooper DKC, Ye Y, Niekrasz M . Heart transplantation in primates. In Cramer DV, Podesta L, Makowka L (eds) Handbook of Animal Models in Transplantation Research CRC Press: Boca Raton 1994 pp 173–200
Hawley RJ, Abraham S, Akiyoshi DE et al. Xenogeneic bone marrow transplantation: I. Cloning, expression, and species specificity of porcine IL-3 and granulocyte–macrophage colony-stimulating factor Xenotransplantation 1997 4: 103–111
Giovino MA, Hawley RJ, Dickerson MW et al. Xenogeneic bone marrow transplantation: II. Porcine-specific growth factors enhance bone marrow engraftment in an in vitro primate microenvironment Xenotransplantation 1997 4: 112–119
Nash K, Chang Q, Watts A et al. Peripheral blood progenitor cell mobilization and leukapheresis in pigs Lab Anim Sci 1999 49: 645–649
Xu Y, Lorf T, Sablinski T et al. Removal of anti-porcine natural antibodies from human and nonhuman primate plasma in vitro and in vivo by a Galα1–3Galβ1–4βGlc-X immunoaffinity column Transplantation 1998 65: 172–179
Kozlowski T, Ierino FL, Lambrigts D et al. Depletion of anti-Galα1–3Gal antibody in baboons by perfusion of specific immunoaffinity columns combined with apheresis Xenotransplantation 1998 5: 122–131
Lambrigts D, Van Calster P, Xu Y et al. Pharmacologic immunosuppressive therapy and extracorporeal immunoadsorption in the suppression of anti-αGal antibody in the baboon Xenotransplantation 1998 5: 274–283
Kobayashi T, Taniguchi S, Neethling FA et al. Delayed xenograft rejection of pig-to-baboon cardiac transplants after cobra venom factor therapy Transplantation 1997 64: 1255–1261
Cooper DKC, Lanza RP . Xeno – The Promise of Transplanting Animal Organs into Humans Oxford University Press: New York 2000
Cooper DKC, Ye Y, Rolf LL, Zuhdi N . The pig as potential organ donor for man. In: Cooper DKC, Kemp E, Reemtsma K, White DJG (eds) Xenotransplantation, first edn Springer: Heidelberg 1991 pp 481–500
Sykes M, Sachs DH . Xenogeneic tolerance through hematopoietic cell and thymic transplantation. In: Cooper DKC, Kemp E, Platt JL, White DJG (eds) Xenotransplantation, second edn Springer: Heidelberg 1997 pp 496–518
Holler E, Kolb HJ, Hiller E et al. Microangiopathy in patients on cyclosporine prophylaxis who developed acute graft-versus-host disease after HLA-identical bone marrow transplantation Blood 1989 73: 2018–2024
Smith RE, Berg DD . Coagulation defects in cyclosporine A treated allogeneic bone marrow transplant patients Am J Hematol 1988 28: 137–140
Moschcowitz E . Hyaline thrombosis of the terminal arterioles and capillaries: a hitherto undescribed disease Proc NY Pathol Soc 1924 24: 21–24
Cohen JA, Brecher ME, Bandarenko N . Cellular source of serum lactate dehydrogenase elevation in patients with thrombotic thrombocytopenic purpura J Clin Apher 1998 13: 16–19
Asada Y, Sumiyoshi A, Hayashi T et al. Immunohistochemistry of vascular lesion in thrombotic thrombocytopenic purpura, with special reference to factor VIII antigen Thromb Res 1985 38: 469–479
Furlan M, Robles R, Solenthaler M et al. Deficient activity of von Willebrand factor-cleaving protease in chronic relapsing thrombotic thrombocytopenic purpura Blood 1997 89: 3097–3103
Furlan M, Robles R, Solenthaler M, Lämmle B . Acquired deficiency of von Willebrand factor-cleaving protease in a patient with thrombotic thrombocytopenic purpura Blood 1998 91: 2839–2846
Moake JL, Chow TW . Thrombotic thrombocytopenic purpura: understanding a disease no longer rare Am J Med Sci 1998 316: 105–119
Byrnes JJ, Hussein AM . Thrombotic microangiopathic syndromes after bone marrow transplantation Cancer Invest 1996 14: 151–157
Sarode R, McFarland JG, Flomenberg N et al. Therapeutic plasma exchange does not appear to be effective in the management of thrombotic thrombocytopenic purpura/hemolytic uremic syndrome following bone marrow transplantation Bone Marrow Transplant 1995 16: 271–275
Llamas P, Romero R, Cabrera R et al. Management of thrombotic microangiopathy following allogeneic transplantation: what is the role of plasma exchange? Bone Marrow Transplant 1997 20: 305–306
Lian EC . Pathogenesis of thrombotic thrombocytopenic purpura Semin Hematol 1987 24: 82–100
Sanders WE, Read MS, Reddick RL et al. Thrombotic thrombocytopenia with von Willebrand factor deficience induced by botrocetin Lab Invest 1988 59: 443–452
Sanders WE, Reddick RL, Nichols TC et al. Thrombotic thrombocytopenia induced in dogs and pigs Arterioscler Thromb Vasc Biol 1995 15: 793–800
Mant MJ, Turner AR, Bruce D et al. Splenectomy during partial remission in thrombotic thrombocytopenic purpura with prolonged plasma exchange dependency Am J Hematol 1999 62: 56–57
Kelton JG, Moore JC, Murphy WG . Studies investigating platelet aggregation and release initiated by sera from patients with thrombotic thrombocytopenic purpura Blood 1987 69: 924–928
Samuelsson B, Dahler SE, Lindgren JA et al. Leukotrienes and lipoxins: structures, biosynthesis, and biological effects Science 1987 237: 1171–1176
Marcus AJ . Multicellular eicosanoid and other metabolic interactions of platelets and other cells. In: Colman RW, Hirsch J, Marder VJ, Salzman EW (eds) Hemostasis and Thrombosis: Basic Principles and Clinical Practice, third edn JB Lippincott: Philadelphia 1993 pp 590–602
Tardy B, Page Y, Comtet C et al. Intravenous prostacyclin in thrombotic thrombocytopenic purpura: case report and review of the literature J Intern Med 1991 230: 279–282
Henn V, Slupsky JR, Grafe M et al. CD40 ligand on activated platelets triggers an inflammatory reaction of endothelial cells Nature 1998 391: 591–594
Robson SC, Schulte am Esch J II, Bach FH . Factors in xenograft rejection Ann NY Acad Sci 1999 875: 261–276
Acknowledgements
We thank Drs J Fishman and T Spitzer for their considerable advice throughout this study, Drs C Ferran and T Spitzer for their review of the manuscript, A Watts, S Treter and K Nash for excellent technical assistance and Mrs Lisa Bernardo for help in manuscript preparation. We also wish to record our gratitude to Ms Stephanie Spaide of Abbott Laboratories for making available additional Omniflow 4000 infusion pumps on several occasions, and to the following companies for generous gifts of their products: Abbot Laboratories (Hetastarch 6%), Baxter Healthcare (Albumin 5%), Novartis Pharmaceuticals (Sandimmune iv), Glaxo-Wellcome (Zantac iv), and Roche Laboratories, Inc. (CellCept iv). This work was supported in part by National Institutes of Health grant No. 5P01 AI39755 and by a Sponsored Research Agreement between the Massachusetts General Hospital and BioTransplant, Inc.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Bühler, L., Goepfert, C., Kitamura, H. et al. Porcine hematopoietic cell xenotransplantation in nonhuman primates is complicated by thrombotic microangiopathy. Bone Marrow Transplant 27, 1227–1236 (2001). https://doi.org/10.1038/sj.bmt.1703067
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1703067
Keywords
This article is cited by
-
Transplantation-associated thrombotic microangiopathy: twenty-two years later
Bone Marrow Transplantation (2002)