Abstract
Etoposide (VP-16) is a topoisomerase II (topo II) inhibitor chemotherapeutic agent. Studies indicate that VP-16 enhances proinflammatory cytokines secretion from tumour cells, including IL-8, a chemokine associated with proangiogenic effects. Fluoroquinolones inhibit topo II activity in eukaryotic cells by a mechanism different from that of VP-16. The fluoroquinolone moxifloxacin (MXF) has pronounced anti-inflammatory effects in vitro and in vivo. We studied the effects of MXF and VP-16 on purified human topo II activity and further analysed their combined activity on proliferation, apoptosis and caspase-3 activity in THP-1 and Jurkat cells. Moxifloxacin alone slightly inhibited the activity of human topo II; however, in combination with VP-16 it led to a 73% reduction in enzyme activity. VP-16 inhibited cell proliferation in a time and dose-dependent manner. The addition of moxifloxacin for 72 h to low-dose VP-16 doubled its cytotoxic effect in THP-1 and Jurkat cells (1.8- and 2.6-fold decrease in cell proliferation, respectively) (P<0.004). Moxifloxacin given alone did not induce apoptosis but enhanced VP-16-induced apoptosis in THP-1 and Jurkat cells (1.8- and two-fold increase in annexin V positive cells and caspase-3 activity, respectively) (P<0.04). VP-16 induced the release of IL-8 in a time and dose-dependent manner from THP-1 cells. Moxifloxacin completely blocked the enhanced release of IL-8 induced by 0.5 and 1 μg ml−1 VP-16, and decreased IL-8 release from cells incubated for 72 h with 3 μg ml−1 VP-16 (P<0.001). VP-16 enhanced the release of IL-1β and TNF-α from THP-1 cells, whereas the addition of MXF prevented the enhanced cytokine secretion (P<0.001). We conclude that MXF significantly enhances VP-16 cytotoxicity in tumour-derived cells while preventing VP-16-induced proinflammatory cytokine release. This unique combination may have clinical benefits and cytotoxic drug ‘sparing effect’ and should be further studied in vivo.
Similar content being viewed by others
Main
Topoisomerase II (topo II) is an important target of chemotherapeutic agents (Berger and Wang, 1996). One of the first drugs to demonstrate an antineoplastic effect through inhibition of topo II was etoposide (VP-16), which prevents resealing of the enzyme-linked DNA breaks (Handle, 1998). Etoposide is used today as frontline therapy for a variety of human malignancies, including leukaemias, lymphomas and several solid tumours (Fry et al, 1991; Handle, 1998).
Several studies have indicated that in addition to their known cytotoxic effects, many chemotherapeutic agents, including VP-16, are also prooxidative stressors (Kagan et al, 2001) and trigger cytokine production in a variety of cell types in vitro (Kawagishi et al, 2001; Darst et al, 2004). These findings were supported by reports of significant levels of proinflammatory cytokines in patients undergoing chemotherapy for a variety of tumours (Villani et al, 2002). The role of proinflammatory cytokines in tumour progression, angiogenesis and metastases has been elucidated in recent years. Specifically, IL-8 was shown to be a potent proangiogenic factor associated with increased microvessel count, increased VEGF expression and poor prognosis in oesophageal squamous cell carcinoma, colonic cancer cells and pancreatic adenocarcinoma cells (Mizukami et al, 2005; Ren et al, 2005; Trevino et al, 2005). Various studies have shown that blocking IL-8 expression reversed many of these proangiogenic and metastatic cell activities, further supporting the important role of this proinflammatory cytokine in tumour progression ((Mizukami et al, 2005; Ren et al, 2005; Trevino et al, 2005).
Combination chemotherapy is commonly employed for treatment of many neoplastic diseases and is considered to provide several advantages over single-agent regimens.
Fluoroquinolones are highly effective antibiotics with a broad antibacterial spectrum (Bakshi et al, 2001). At high concentrations, some fluoroquinolones exhibit genotoxic effects in eukaryotic systems as a result of topo II inhibition (Robinson et al, 1991). Quinolone-induced inactivation of topo IIα at high concentrations was proposed to involve the direct binding of quinolones to DNA and their mode of inhibition was shown to be distinct from the inhibitory mechanism of agents like VP-16 (Bromberg et al, 2003a). Additional studies suggest that quinolones such as CP-115 953 enhance the formation of double-stranded DNA breaks by human topo IIα and exert cytotoxic activity in Chinese hamster ovary cells (Elsea et al, 1997). Our group and others assessed the in vitro activity of certain quinolones against various tumour cell lines. Ciprofloxacin was found to inhibit tumour cell growth of bladder transitional cell carcinoma, colon cancer and prostate cancer cell lines at concentrations achievable with its oral administration (Zehavi-Willner and Shalit, 1992; Shalit et al, 1995; Herold et al, 2002; Aranha et al, 2003).
We have previously shown that the fluoroquinolone moxifloxacin (MXF) inhibits nuclear factor kappa B (NF-κB) activation, mitogen-activated protein kinase activation and synthesis of the proinflammatory cytokines IL-8, TNF-α and IL-lβ in activated human monocytic cells (Weiss et al, 2004). It also had a protective anti-inflammatory effect in vivo in a model of Candida albicans pneumonia in immune suppressed animals, resulting in enhanced survival and reduction in IL-8 and TNF-α in lung homogenates (Shalit et al, 2002). In the present study, we investigated the effect of MXF alone and in combination with VP-16 on isolated human topo IIα activity and further studied the effect of the combination on cell proliferation, cytotoxicity and apoptosis in two tumour-derived cell lines, THP-1 and Jurkat. In parallel, we investigated the effect of MXF on VP-16-induced release of proinflammatory cytokines, including IL-8, in these cells.
Materials and methods
Human topo II assay
A previously described method was used with slight modifications (Bendetz-Nezer et al, 2004). Purified human DNA topo II (p170) (0.5–2 units) (TopoGen Inc., Port Orange, FL, USA) was added to a topo II reaction mixture containing, at a final volume of 20 μl, 50 mM Tris-HCl, (pH 8), 0.5 mM dithiothreitol (DTT), 120 mM KCl, 10 mM MgCl2, 0.5 mM EDTA, 25 μg ml−1 bovine serum albumin, 1 mM ATP and 250–750 ng of pUC 19 supercoiled DNA plasmid (MBI Fermentas, Hanover, MD, USA). Different concentrations of MXF (20–100 μg ml−1) and VP-16 (5–10 μg ml−1) were added. After incubation at 37°C for 10 min, the reaction was terminated by adding 5 μl of stopping buffer (final concentration, 1% SDS, 15% glycerol, 0.5% bromphenol blue and 50 mM EDTA, pH 8). The reaction products were analysed by electrophoresis on 1% agarose gel using a Tris-borate/EDTA buffer (89 mM boric acid and 62 mM EDTA) at 1 V cm−1, stained with ethidium bromide (1 μg ml−1), and photographed using a short-wavelength UV lamp (ChemiImager 5500; Alpha Innotech, San Leandro, CA, USA).
Cell lines
Human acute monocytic leukaemia cell line THP-1 (ATCC TIB 202) and human acute T-cell leukaemia Jurkat cells were maintained in RPMI 1640 medium supplemented with 10% heat-inactivated fetal bovine serum, 2 mM L-glutamine, 100 units ml−1 penicillin and 100 μg ml−1 streptomycin at 37°C in a humidified incubator with 5% CO2.
Cytotoxicity assay
THP-1 and Jurkat cells, cultured as described above, were seeded on 96-well plates (at a concentration of 5 × 104 THP-1 cells per 0.1 ml well−1 and 2.5 × 104 Jurkat cells per 0.1 ml well−1) in triplicate, and various concentrations of MXF, VP-16 and their combination were added. The cells were incubated for 24–72 h at 37°C in 5% CO2 atmosphere. For the last 3 h of incubation, MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium) (5 mg ml−1) in phosphate-buffered saline (PBS) was added to each well. The cells were incubated at 37°C for 3 h and 0.04 M HCl was added to dissolve the formazan crystals. The absorbance was then measured at 560 nm with a spectrophotometer (ELISA Reader Molecular Devices Corporation, Sunnyvale, CA, USA).
Apoptosis assay
Apoptosis was measured by flow cytometry after concurrent staining with fluorescein-conjugated annexin V and propidium iodide (PI), as previously described (Gross-Fischer and Fabian, 2002). In brief, following incubation of THP-1 and Jurkat cells with 1 μg ml−1 VP-16 and various concentrations of MXF and their combination for 24 h, cells were collected and washed with cold PBS and resuspended in annexin V-PI binding buffer (10 mM HEPES, pH 7.4, 140 mM NaCl, 2.5 mM CaCl2). An aliquot of 100 μl was removed and mixed with 4 μl of annexin V-PI. The mixture was incubated for 15 min at room temperature (RT) in the dark. The cells were then washed once with binding buffer, resuspended in binding buffer and subjected to flow cytometric analysis on FACScan (Becton Dickinson, Franklin Lakes, NJ, USA).
Fluorogenic assay for caspase-3 activity
Caspse-3 was measured as previously described by us (Gross-Fischer and Fabian, 2002). THP-1 and Jurkat cells were incubated for 24 h with 1 and 3 μg ml−1 VP-16 or various concentrations of MXF, or combination of both drugs. Following incubation, the cells were collected, washed, resuspended in 50 mM HEPES (pH 7.4), 0.1% CHAPS, 5 mM DTT and 0.1 mM EDTA, incubated for 15 min on ice and lysed by three successive freeze–thaw cycles at dry ice/37°C. Cell lysates were centrifuged at 14 000 r.p.m. for 15 min, and the supernatants were stored at −70°C. The protein concentration of each sample was estimated using the Bradford Bio-Rad protein assay. For caspase-3 activity, a total of 25 μg protein was incubated with 30 mM ac-DEVD-AMC (BIOMOL Research Laboratories, Plymouth Meeting, PA, USA) at 37°C, for 60 min in the dark. The release of 7-amino-4-methylcoumarine was monitored by a spectrofluorometer using an excitation wavelength of 360 nm and an emission wavelength of 460 nm. In some experiments, a caspase-3 inhibitor (Z-DEVD-FMK, Calbiochem, Nottingham, UK) was added directly to the medium 30 min before the addition of 1 μg ml−1 VP-16.
Western blot analysis of caspase-3
For caspase-3 immunoblotting, total cell lysates were prepared as described before with slight modifications. Cells were collected and washed twice in ice-cold PBS, and then lysed with a solubilising solution on ice for 30 min (Gross-Fischer and Fabian, 2002). The extracts were cleared by centrifugation. Equal amounts of protein (50 μg) were subjected to electrophoresis on 12% SDS–polyacrylamide gel and then electrophoretically transferred to a nitrocellulose membrane. The membranes were incubated with anti-caspase-3 polyclonal antibody (diluted 1:1000, PharMingen, Franklin Lakes, NJ, USA). Actin levels were also assessed as a loading control using an antibody (Santa Cruz Biotechnology, Santa Cruz, CA, USA) that reacts with a broad range of actin isoforms. The blots were then incubated with a secondary antibody, horseradish peroxidase-linked anti-mouse IgG (Santa Cruz Biotechnology). After 1 h at RT and three washes in TBST, the blots were incubated in enhanced chemiluminescence reagent (ECL, Amersham Pharmacia Biotech, Uppsala, Sweden). Bound antibodies were visualised following chemiluminescence detection on autoradiographic film.
IL-8, IL-1β and TNF-α production analysis by ELISA
THP-1 cells suspended in RPMI medium, as described above, were placed in 24-well culture plates at a concentration of l × 106 cells ml−1 (for the determination of IL-8) and incubated for 24–72 h with various concentrations of VP-16 in the presence or absence of 5–20 μg ml−1 MXF. For the determination of IL-1β and TNF-α, cells were plated at concentrations of l × 106 cells ml−1 and 1.5 × 106 cells ml−1, respectively, for 24 h in the presence of VP-16 and MXF as described above. Cell-free supernatants were recovered, and the concentrations of IL-8, IL-1β and TNF-α were determined using ELISA (R&D Systems Inc., Minneapolis MN, USA). The sensitivity of the assay for IL-8 is >10 pg ml−1, for IL-1β >4 pg ml−1 and for TNF-α >15 pg ml−1. Jurkat cells were pretreated for 1 h with 1–10 ng ml−1 phorbol myristate acetate (PMA) and 5–500 ng ml−1 ionomycin (Sigma Chemical Co., St Louis, MO, USA) to promote cytokine production (Pestka et al, 2005). Various concentrations of VP-16 and MXF were added and the concentrations of IL-8, IL-1β and TNF-α were determined as described above.
Statistical analysis
Statistical significance was determined by paired t-test (for MTT, fluorogenic assay for caspase-3 activity and for cytokine secretion) and ANOVA: two-factor without replication test (for the annexin-PI studies). A P-value of ⩽0.05 was considered significant.
Results
Purified human topo II DNA relaxation activity assay
The inhibition of the DNA relaxation activity of human topo II by various concentrations of MXF and VP-16 was investigated using purified human topo II added to a specific reaction mixture containing ATP and supercoiled pUC 19 DNA as the substrate, as described in Materials and Methods. As shown in Figure 1A, MXF at a concentration of 20 and 40 μg ml−1 caused a 5–6% inhibition of topo II activity (lanes 3 and 4, respectively). Etoposide reduced topo II activity only slightly at a concentration of 10 μg ml−1 (10%) (lane 6), and not at all at a lower concentrations (5 μg ml−1) (lane 5). By contrast, the combination of 20 μg ml−1 MXF with 5 or 10 μg ml−1 VP-16 markedly reduced topo II activity, by 20% (lane 7) and 67% (lane 8), respectively. The combination of a higher concentration of MXF (40 μg ml−1) with VP-16 revealed only a slight further inhibition of topo II activity (up to 73%) (lane 10).
(A) Representative agarose gel electrophoresis analysis of the topo II reaction products, obtained with increasing amounts of MXF, VP-16 or their combination. The pUC supercoiled DNA plasmid and the relaxed forms are shown. (B) Increasing amounts of topo II (0.5–2 units) were added to reaction mixtures containing a constant amount of pUC19 DNA (250 ng) and 10 μg ml−1 VP-16+40 or 100 μg ml−1 MXF. (C) Increasing amounts of pUC-19 DNA (500–750 ng) were added to topo II reaction mixture containing constant amounts of topo II (1 unit) and 10 μg ml−1 VP-16+40 μg ml−1 MXF. R=relaxed DNA, S=supercoiled DNA, u=units.
The observed increased inhibitory effect of VP-16 by MXF might be due to (1) a direct effect of MXF on the topo II protein, rendering it more susceptible to the action of VP-16; (2) MXF affects the DNA (e.g. intercalation) in a way that increases the VP-16-induced stabilisation of the DNA–enzyme cleavable complexes. To determine which of the possibilities do occur, we performed two classical biochemical competition-based assays (Aflalo et al, 1994). Topoisomerase II activity was measured in the presence of constant amounts of DNA and MXF/VP-16 and increasing amounts of topo II enzyme (Figure 1B) or vice versa; topo II activity was measured in the presence of constant amounts of enzyme and MXF/VP-16 and increasing amounts of DNA (Figure 1C). The results show that only by increasing the amount of topo II enzyme, it is possible to overcome the inhibitory effect of MXF/VP-16 (Figure 1B compared to 1C), suggesting a possible, yet unclear, interaction of MXF with the topo II protein.
On the basis of our observations that MXF enhances the inhibition of purified topo II activity conferred by VP-16, we investigated the possible association between the effect on isolated topo II activity and the cytotoxic activity of the drug combination.
Effect of MXF on the antiproliferative action of VP-16
We performed time-dependent studies on the effect of VP-16 (0.5 μg ml−1) on the proliferation of THP-1 cells. Figure 2A indicates that a decrease of 17.7±0.2 and 29±0.3% was observed upon incubation of the cells with the drug for 48 and 72 h, respectively (P<0.001). Moxifloxacin given alone, at concentrations of 5 or 10 μg ml−1 did not affect cell proliferation (data not shown) whereas incubation of the cells with 20 μg ml−1 MXF for 24–72 h resulted in a 16±0.1–20±0.4% inhibition in cell proliferation (P<0.05).
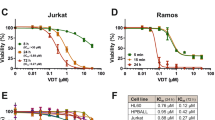
Moxifloxacin enhances the antiproliferative effect of VP-16. Time-dependent studies: THP-1 cells (A) and Jurkat cells (C) were incubated for 24–72 h with 0.5 μg ml−1 VP-16 in the presence or absence of various concentrations of MXF. Cell proliferation was determined by colorimetric MTT assay. Dose-dependent studies: THP-1 cells (B) and Jurkat cells (D) were incubated for 48 h in the presence of the indicated concentrations of VP-16 and MXF. Cell proliferation was determined as described above. Results are expressed as mean±s.e. of four experiments performed in triplicate. *P<0.05 cells treated with drugs vs control. **P<0.007 for cells treated by VP-16+MXF vs VP-16 alone.
A significant decrease in cell proliferation was seen with the combination of 0.5 μg ml−1 VP-16 and MXF compared to VP-16 alone. Upon exposure of the cells to a combination of VP-16 and 10 μg ml−1 MXF for 48 and 72 h, a marked decrease in cell proliferation (up to 36±0.6 and 45±0.8%, respectively) was observed (P=<0.001). Maximum inhibition in cell proliferation was observed upon incubation of the cells with 0.5 μg ml−1 VP-16 and 20 μg ml−1 MXF for 72 h (up to 52±0.5%), compared to VP-16 alone (P<0.001) (Figure 2A).
Dose-dependent studies of VP-16 and MXF were performed, following incubation of the cells for 48 h with the drugs. Exposure of THP-1 cells to VP-16 for 48 h resulted in a concentration-dependent decrease in cell proliferation (Figure 2B). It should be noted that exposure of THP-1 cells to a low dose of the cytotoxic drug VP-16 (0.5 μg ml−1) and 20 μg ml−1 MXF resulted in a 46% inhibition of cell proliferation, similar to the inhibitory effect of 1 μg ml−1 VP-16 alone (41%). Maximal inhibition of cell proliferation was observed upon incubation of the cells with 3 μg ml−1 VP-16 and 20 μg ml−1 MXF compared to VP-16 alone (85.4±1.6 vs 76±1.5%, respectively, P=0.006).
In Jurkat cells (Figure 2C), incubation of the cells for 72 h with a low dose of VP-16 (0.5 μg ml−1), resulted in a 21±0.6% inhibition of cell proliferation (P<0.001). As with THP-1 cells, incubation of Jurkat cells with 5 or 10 μg ml−1 MXF for 24–72 h, did not affect cell proliferation (data not shown), whereas incubation for 72 h with 20 μg ml−1 MXF, resulted in a 24±0.6% inhibition of cell proliferation (P=0.008). Exposure of the cells for 72 h to a combination of VP-16 (0.5 μg ml−1) and 10 or 20 μg ml−1 MXF, led to 31±0.1 and 54±0.5% inhibition, respectively, compared to 21±0.6% with VP-16 alone (P<0.004).
The addition of various concentrations of VP-16 alone reduced cell proliferation in a dose-dependent manner (Figure 2D). Like in THP-1 cells, the addition of increasing concentrations of MXF to Jurkat cells incubated for 48 h with various concentrations of VP-16 further decreased cell proliferation. Incubation of the cells with 1 μg ml−1 VP-16 and 20 μg ml−1 MXF resulted in 56±5% decrease, compared to 22±2% for VP-16 alone (P=<0.001). The maximal inhibition of cell proliferation was observed upon incubation of the cells with 3 μg ml−1 VP-16 and 20 μg ml−1 MXF (up to 89±8%) (Figure 2D).
Effect of MXF on VP-16-induced apoptosis
Phosphatidylserine, which is normally confined to the inner leaflet of the plasma membrane, is exported to the outer plasma membrane leaflet during apoptosis. We assessed phosphatidylserine externalisation following the exposure of THP-1 and Jurkat cells for 24 h to MXF alone or to 1 μg ml−1 VP-16 in the presence or absence of 5–20 μg ml−1 MXF. As shown in Figure 3A and C, in the THP-1 cells, MXF (20 μg ml−1) given alone, did not affect apoptosis whereas a marked increase in apoptotic (annexin V-positive) cells was observed after exposure to VP-16, and a further 1.7-fold to 1.8-fold increase with the addition of 5–20 μg ml−1 MXF (P=0.038). As with THP-1 cells, exposure of Jurkat cells to 20 μg ml−1 MXF did not affect apoptosis whereas exposure to 1 μg ml−1 VP-16 alone (Figure 3B) resulted in a mild increase in apoptotic cells, with a further increase after the addition of MXF, by 1.7-fold for 10 μg ml−1 MXF (P=0.024), and by 2.2-fold for 20 μg ml−1 MXF (P=0.015) (Figure 3C).
Moxifloxacin enhances apoptosis induced by VP-16. THP-1 (A and C) and Jurkat cells (B and C) were incubated for 24 h with VP-16 and MXF as indicated and flow cytometric analysis was performed by binding of annexin V and uptake of PI. A representative experiment is shown in (A and B). Results (mean±s.e.) of two independent experiments are shown in (C). The percentage of annexin V-positive, PI-negative cells is indicated in the lower right quadrangle and of annexin V-positive, PI-positive cells in the upper right quadrangle. The X-axis shows log annexin V fluorescence intensity and the Y-axis shows PI fluorescence intensity. *P<0.04 for cells treated with VP-16+MXF vs VP-16 alone.
Caspase-3 activation
DEVD-AMC is a specific substrate for caspase-3 that mimics the PARP cleavage site. To test caspase-3 activation, cell lysates from THP-1 and Jurkat cells that were treated with VP-16 in the presence or absence of 5–20 μg ml−1 MXF for 24 h were incubated with the substrate, and the increase in fluorescence due to enzymatic cleavage of the peptides was measured with a fluorometer. As shown in Figure 4A, in THP-1 cells, treatment with 1 or 3 μg ml−1 VP-16 significantly increased caspase-3 activation (P=0.011 and P=0.044, respectively). The addition of 20 μg ml−1 MXF further enhanced this increase by two-fold in the presence of 1 μg ml−1 VP-16 (P=0.045) and by 1.7-fold in the presence of 3 μg ml−1 VP-16 (P=0.05). To confirm that the caspase activity observed was specific to caspase-3, we used a caspase-3-specific inhibitor, Z-DEVD-FMK. Treatment of cells with the inhibitor before the addition of 1 μg ml−1 VP-16 reduced the degree of caspase-3 activation (insert in Figure 4A).
Moxifloxacin enhances caspase-3 activation induced by VP-16. THP-1 (A) and Jurkat cells (C) were incubated with the indicated concentrations of VP-16 and MXF for 24 h and lysates were prepared. Caspase-3 activity was measured using DEVD-AMC as the substrate. The data represent the mean±s.e. of three experiments. Effect of caspase-3 inhibitor (insert in A and C): grey column indicates control cells; white column indicates cells treated with 1 μg ml−1 VP-16. The black column cells were preincubated for 30 min with Z-DEVD-FMK (caspase-3 inhibitor) before exposure to 1 μg ml−1 VP-16. *P<0.05; **P<0.012 VP-16+MXF vs VP-16-treated cells. Western blot analysis of procaspase-3. THP-1 (B) and Jurkat cells (D) were incubated in medium (lane 1) or with 1 μg ml−1 VP-16 (lanes 2–5) and MXF (5–20 μg ml−1) (lanes 3–5, respectively). Lysates were prepared and samples containing 50 μg protein were resolved in 12% SDS gels and electroblotted onto nitrocellulose membranes. The membranes were probed with anticaspase-3 rabbit polyclonal antibody and with antiactin antibody.
Immunoblots performed on lysates of these cells demonstrated that MXF enhanced the cleavage of procaspase 3 induced by 1ìg ml−1 VP-16 in a dose-dependent manner (Figure 4B).
In Jurkat cells, as shown in Figure 4C, incubation with 1 or 3 μg ml−1 VP-16 significantly enhances caspase-3 activity by 4.4-fold (P<0.001) and by 21.3-fold (P=0.014), respectively. The addition of MXF to VP-16 further enhanced the activity of caspase-3. The addition of 5, 10 or 20 μg ml−1 MXF to l μg ml−1 VP-16 resulted in a 2.3-, 3.5- and 4.4-fold increase in caspase-3 activity, respectively (P=0.028, P=0.05 and P=0.05, respectively), indicating that MXF increases the inhibition of Jurkat cell growth, induced by VP-16, by induction of apoptosis via activation of caspase-3 activity. Similarly, the combination of 20 μg ml−1 MXF and 3 μg ml−1 VP-16 led to an additional 1.45-fold increase in caspase-3 activity (P=0.035) (Figure 4C). Treatment of the cells with Z-DEVD-FMK before the addition of 1 μg ml−1 VP-16 reduced the degree of caspase-3 activation (inset in Figure 4C), confirming that the caspase activity observed was specific to caspase-3. Immunoblots performed on lysates of these cells demonstrated that MXF enhanced the cleavage of procaspase-3 induced by 1 μg ml−1 VP-16 in a dose-dependent manner (Figure 4D).
Secretion of proinflammatory cytokines
We investigated the effect of VP-16 on the secretion of proinflammatory cytokines by THP-1 and Jurkat cells. The spontaneous release of IL-8 by THP-1 cells cultured for 72 h was 61±4 pg ml−1. The addition of 5 μg ml−1 MXF resulted in a three-fold decrease in the spontaneous release of the cytokine (to 19.3±1.2 pg ml−1) (P<0.001). Time-dependent studies performed with THP-1 cells indicate that exposure of the cells to 1 μg ml−1 VP-16 for 24–72 h resulted in a 3.1–8.9-fold increase in IL-8 secretion (P<0.001) (Figure 5A). The addition 5 μg ml−1 MXF to cells cultured for 72 h with 1 μg ml−1 VP-16 completely abolished the increase in IL-8 secretion induced by VP-16 (P<0.001) (data not shown). Exposure of the cells for 24–72 h to 3 μg ml−1 VP-16 resulted in additional increase in IL-8 secretion up to 2318±70 pg ml−1 (at 72 h) (P<0.001) (Figure 5A). The addition of 5 μg ml−1 MXF to cells cultured with 3 μg ml−1 VP-16 induced a time-dependent decrease in IL-8 secretion induced by VP-16 (up to 10-fold decrease at 72 h) (P<0.001). No additional decrease in IL-8 secretion was observed in the presence of 10 or 20 μg ml−1 MXF (Figure 5A). Dose-dependent studies of VP-16 on the secretion of IL-lβ and TNF-α were performed. Exposure of THP-1 cells for 24 h to 1 or 3 μg ml−1 VP-16 induced an increase in the secretion of IL-lβ and TNF-α (Figure 5B and C, respectively). The addition of MXF, even at low concentration (5 μg ml−1), completely inhibited the enhanced IL-lβ and TNF-α secretion induced by 0.5 and 1 μg ml−1 VP-16. The addition of 5, 10 or 20 μg ml−1 MXF to cells incubated with 3 μg ml−1 VP-16 decreased TNF-α secretion by 52%, 44% and 66%, respectively (P=<0.001 for each concentration) (Figure 5C). In Jurkat cells, no secretion of IL-8 could be detected without stimulation with PMA and ionomycin (data not shown). Pretreatment of the cells with 500 ng ml−1 ionomycin and 1–10 ng ml−1 PMA for 24 h resulted in a dose-dependent increase in IL-8 secretion (Figure 5D). Lower concentrations of IL-8 were detected upon pretreatment with 10 ng ml−1 PMA and 5 or 50 ng ml−1 ionomycin (Figure 5D). The addition of 1–3 μg ml−1 VP-16 to Jurkat cells pretreated with PMA at a dose of 10 ng ml−1 or lower and 500 ng ml−1 ionomycin or lower had no effect on IL-8 release from the cells (data not shown).
Moxifloxacin decreases proinflammatory cytokine secretion induced by VP-16 in THP-1 cells. Time-dependent studies: THP-1 cells were incubated for 24–72 h with increasing concentrations of VP-16 and 5 μg ml−1 MXF as indicated. The concentrations of IL-8 (A) were measured by ELISA. Dose-dependent studies: THP-1 cells were incubated for 24 h with increasing concentrations of VP-16 and MXF. The concentrations of IL-1β (B) and TNF-α (C) in culture supernatant were measured by ELISA. The values are the mean±s.e. of four experiments performed in duplicates. *P<0.018; **P<0.008 VP-16+MXF vs VP-16-treated cells. (D) Jurkat cells were incubated for 24 h with the indicated concentrations of PMA and ionomycin and the concentration of IL-8 was measured by ELISA. The values are the mean±s.e. of four experiments performed in duplicate.
Discussion
Several studies on the antiproliferative activity of fluoroquinolone antibiotics have shown that quinolones such as ciprofloxacin and fleroxacin inhibit the growth of various human tumour cells, including transitional cell carcinoma of the bladder and human colorectal carcinoma cells (Miclau et al, 1998; Aranha et al, 2000). El-Rayes et al (2002) reported that ciprofloxacin acts synergistically with VP-16 in hormone-resistant prostate cancer cells and Kamat et al (1999) demonstrated that ciprofloxacin and ofloxacin exert synergistic activity with doxorubicin in bladder cancer cell lines.
The present study investigated, for the first time, the effect of MXF in combination with VP-16 on the activity of human topo II by measuring the relaxation of supercoiled pUC 19 DNA plasmid. We have also defined the functional interaction of the drugs by investigating their effect on the cytotoxic activity towards THP-1 and Jurkat cells.
We found that MXF alone (at a concentration of 20 or 40 μg ml−1) only slightly inhibited human topo II activity, but in combination with VP-16 it led to a significant increase in the inhibitory effect of the anticancer drug on topo II activity. In addition, we found that the inhibitory effect of the combined drugs on topo II could be inhibited only by increasing the amount of the enzyme protein in the reaction and not by adding higher concentrations of the DNA substrate. This suggests that MXF enhances the inhibitory effects of VP-16 on topo II by affecting the enzyme protein in such a way that it renders it to become more susceptible to VP-16.
Other investigators (Perrone et al, 2002) studied the inhibition of topo II by four quinolones and ultraviolet A irradiation, and found that MXF at various concentration up to 10 μ M (equivalent to 4 μg ml−1) did not show enzyme inhibitory activity in the absence or presence of UVA irradiation. We believe that the discrepancy between the studies may be explained by the use of different concentrations of the drug.
To the best of our knowledge, the experiments reported here are also the first to examine the interaction of MXF and VP-16 on the cytotoxic activity of VP-16 and the effect of the combination on cytokine release induced by VP-16. Our study revealed that MXF by itself (at 20 μg ml−1) induced a slight antiproliferative effect (up to 20% decrease in cell proliferation) on THP-1 or Jurkat cells. An additive effect was observed upon incubation of the cells with VP-16 to significantly decrease cell proliferation. A possible explanation for this additive effect is the different mechanisms of action against topo II conferred by the two drugs. Bromberg et al (2003b) have shown that VP-16 acts by inhibiting the ability of topo II to ligate cleaved DNA molecules, whereas quinolones have little effect on ligation but stimulate the forward rate of topo II-mediated DNA cleavage. These two distinct mechanisms may work in concert and lead to the observed additivity in the antiproliferative effects of VP-16 and MXF. Using flow cytometric analysis to determine the mechanism of action of the drugs, we observed that VP-16 induced apoptosis in the two cell lines and that MXF potentiated this apoptotic effect. This finding was supported by measuring levels of caspase-3, which is activated during the process of apoptosis and is one of the key enzymes required for the execution of the apoptotic programme. The results showed that MXF significantly enhanced VP-16-induced activation of caspase-3 in THP-1 and Jurkat cells and that its effect was dose dependent. Western blot analysis confirmed the enhanced proteolytic cleavage of procaspase-3 induced by the combination of MXF and VP-16. Together, these observations indicate that MXF acts as a potentiating drug with VP-16 to enhance VP-16's cytotoxic effect and tumour lysis via activation of caspase-3 activity.
An important observation is the fact that 0.5 μg mg−1 VP-16 combined with 20 μg mg−1 of MXF led to the same inhibition of cell proliferation as a double dose of VP-16 (1 μg ml−1) alone. This may imply a cytotoxic-drug ‘sparing effect’ by MXF. The translation of this phenomenon in the clinical setting is that instead of increasing the dose of the cytotoxic agent, along with its associated toxic side effect, one may use a lower dose of the cytotoxic agent and add the antimicrobial agent MXF with its excellent safety profile, and obtain the same antitumour effects with much less toxicity and adverse effects. It should also be noted, that the concentration of MXF cited above is readily attainable in various tissues such as colon, bladder, prostate and lung cells following the commonly used 400 mg daily oral dose of MXF.
We show in the present study that treatment of THP-1 cells with VP-16 induced the release of the proinflammatory cytokines IL-8, IL-1β and TNF-α. Recent studies have shown that IL-8 is a proangiogenic cytokine regulating tumorigenesis in DLD-1 colon cancer cells (Mizukami et al, 2005), and that it also serves as an autocrine growth factor in human colon carcinoma cells in vitro (Brew et al, 2000). These effects should be looked at as undesired side effects of the drug. Chemotherapy and radiotherapy are prescribed to cancer patients in the hope that dying cells will be safely scavenged by phagocytic cells, such as macrophages. However, in vitro and in vivo studies showed that phagocytosis of VP-16-treated P388 cells by macrophages was associated with the release of IL-8 and other cytokines, such as MIF and MIP-2 (Kawagishi et al, 2001). In addition, VP-16 and the chemotherapeutic agent mitomycin were also found to induce IL-8 and TNF-α production by a human epithelial carcinoma cell line (KB cells) that expressed platelet-activating factor receptor (Darst et al, 2004). The enhanced expression of cytokines induced by VP-16 may in part be associated with certain side effects and should be looked upon with caution owing to the associated proangiogenic activity of IL-8. Our results showed that MXF significantly inhibited the VP-16-enhanced production of IL-8, TNF-α and IL-1β in THP-1 cells, but not in Jurkat cells. Accordingly, Aceves et al (2004) reported a different pattern of gene expression in THP-1 and Jurkat cells on their exposure to chemotherapeutic drugs. This may suggest that the inhibitory effect of MXF on the release of proinflammatory cytokines by cells is tumour cell specific.
The inhibitory effect of MXF on cytokine secretion from THP-1 cells also confirms our previous observations of MXF inhibition of the synthesis of proinflammatory cytokines in THP-1 cells and human peripheral blood monocytes stimulated with LPS-phorbol myristate acetate (Weiss et al, 2004) or Aspergillus fumigatus (Shalit et al, 2006). Additionally, MXF inhibited NF-κB and mitogen-activated protein kinase activation in THP-1 cells and in a human respiratory epithelial cell line (Weiss et al, 2004; Werber et al, 2005). Using a murine model of Candida pneumonia in immune-suppressed animals, we found that MXF exerted a protective anti-inflammatory effect, resulting in a marked decrease in bronchopneumonia and enhanced survival. This protective efficacy was associated with a significant reduction in IL-8 and TNF-α in lung homogenates and an inhibition of NF-κB nuclear mobilisation in alveolar macrophages and lung epithelial cells (Shalit et al, 2002).
Nuclear factor-κB is a well-known mediator of inflammatory cytokines (Won et al, 2005), and it was shown to be activated during apoptosis following cell incubation with a variety of agents including VP-16 (Usami et al, 1998). Based on our previous and current observations, it seems plausible that MXF decreases VP-16-induced proinflammatory cytokine secretion in THP-1 cells via inhibition of NF-κB activation.
In summary, this study demonstrates an important role for MXF in enhancing the cytotoxic effects of VP-16 whereas, at the same time, decreasing VP-16-induced proinflammatory cytokine secretion from cells, which may be harmful during chemotherapeutic treatment. Our results suggest that MXF may be a valuable new addition to chemotherapeutic armamentarium, simultaneously improving the cytotoxic activity while reducing the side effects of VP-16 and similar agents.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Aceves M, Duenas A, Gomez C, San Vicente E, Crespo MS, Garcia-Rodriguez C (2004) A new pharmacological effect of salicylates: inhibition of NFAT-dependent transcription. Immunology 173: 5721–5729
Aflalo E, Seri I, Segal S, Gazit A, Priel E (1994) Inhibition of topoisomerase I activity tyrphostin derivatives, protein tyrosine kinase blockers: mechanism of action. Cancer 54: 5138–5142
Aranha O, Wood DP, Sarkar FH (2000) Ciprofloxacin mediated cell growth inhibition, S/G2-cell cycle, and apoptosis in a human transitional cell carcinoma of the bladder cell line. Cancer Res 6: 891–900
Aranha O, Grignon R, Fernandes N, McDonnell TJ, Wood Jr DP, Sarkar FH (2003) Suppression of human prostate cancer cell growth by ciprofloxacin is associated with cell cycle arrest and apoptosis. Int J Oncol 22: 787–794
Bakshi RP, Galande S, Muniyappa K (2001) Functional and regulatory characteristics of eukaryotic type II DNA topoisomerase. Crit Rev Biochem Mol Biol 36: 1–37
Bendetz-Nezer S, Gazit A, Priel E (2004) DNA topoisomerase I as one of the cellular targets of certain tyrphostin derivatives. Mol Pharmacol 66: 627–634
Berger JM, Wang JC (1996) Recent developments in DNA topoisomerase II structure and mechanism. Curr Opin Struct Biol 6: 84–90
Brew R, Erikson JS, West DC, Kinsella AR, Slavin J, Christmas SE (2000) Interleukin-8 as an autocrine growth factor for human colon carcinoma cells in vitro. Cytokines 12: 78–85
Bromberg KD, Burgin AB, Osheroff N (2003a) Quinolone action against human topoisomerase II alpha: stimulation of enzyme-mediated double-stranded DNA cleavage. Biochemistry 42: 3393–3398
Bromberg KD, Burgin AB, Osheroff N (2003b) A two-drug model for etoposide action against human topoisomerase II alpha. J Biol Chem 278: 7406–7412
Darst M, Al-Hassani M, Li T, Yi Q, Travers JM, Lewis DA, Travers JB (2004) Augmentation of chemotherapy-induced cytokine production by expression of the platelet-activating factor receptor in a human epithelial carcinoma cell line. J Immunol 172: 6330–6335
Elsea SH, Westergaard M, Burden DA, Lomenick JP, Osheroff N (1997) Quinolones share a common interaction domain on topoisomerase II with other DNA cleavage-enhancing antineoplastic drugs. Biochemistry 36: 2919–2924
El-Rayes BF, Grignon R, Aslam N, Aranha O, Sarkar FH (2002) Ciprofloxacin inhibits cell growth and synergises the effect of etoposide in hormone resistant prostate cancer cells. Int J Oncol 21: 207–211
Fry AM, Chresta CM, Davies SM, Walker MC, Harris AL, Hartley JA, Masters JR, Hickson ID (1991) Relationship between topoisomerase-II level and chemosensitivity in human tumour cell lines. Cancer Res 51: 6592–6595
Gross-Fischer T, Fabian I (2002) Protection by ascorbic acid from denaturation and release of cytochrome c, alteration of mitochondrial membrane potential and activation of multiple caspases induced by H2O2, in human leukemia cells. Biochem Pharmacol 63: 1325–1335
Handle KR (1998) Clinical applications of anticancer drugs targeted to topoisomerase II. Biochim Biophys Acta 1400: 173–184
Herold C, Ocker M, Ganslmayer M, Gerauer H, Hahn EG, Schuppan D (2002) Ciprofloxacin induces apoptosis and inhibits proliferation of human colorectal carcinoma cells. Br J Cancer 86: 443–448
Kagan VE, Kuzmenko AI, Tyurina YY, Shvedova AA, Matsura T, Yalowich JC (2001) Pro-oxidant and antioxidant mechanisms of etoposide in HL-60 cells: role ofmyeloperoxidase. Cancer Res 6: 7777–7784
Kamat AM, DeHaven JI, Lamm DL (1999) Quinolone antibiotics: a potential adjunct to intravesical chemotherapy for bladder cancer. Urology 54: 56–61
Kawagishi C, Kurosaka K, Watanabe N, Kobayashi Y (2001) Cytokine production by macrophages in association with phagocytosis of etoposide-treated P388 cells in vitro and in vivo. Biophys Acta 1541: 221–230
Miclau T, Edin ML, Lester GE, Lindsey RW, Dahners LE (1998) Effect of ciprofloxacin on the proliferation of osteoblast-like MG-63 human osteosarcoma cells in vitro. J Orthoped Res 16: 509–512
Mizukami YJo WS, Duerr EM, Gala M, Li J, Zhang X, Zimmer MA, Iliopoulos O, Zukerberg LR, Kohgo Y, Lynch MP, Rueda BR, Chung DC (2005) Induction of interleukin-8 preserves the angiogenic response in HIF-1 alpha-deficient colon cancer cells. Nat Med 11: 92–97
Perrone CE, Takahashi KC, Williams GM (2002) Inhibition of human topoisomerase II alpha by fluoroquinolones and ultraviolet A irradiation. Toxicol Sci 69: 6–22
Pestka J, Uzarski RL, Islam Z (2005) Induction of apoptosis and cytokine production in the Jurkat human T cells by deoxynivalenol: role of mitogen-activated protein kinases and comparison to other 8- ketotrichothecenes. Toxicology 206: 207–219
Ren Y, Cao B, Law S, Xie Y, Lee Py, Cheung L, Chen Y, Huang X, Chan HM, Zhao P, Luk J, Woude GV, Wong J (2005) Hepatocyte growth factor promotes cancer cell migration and angiogenic factors expression: a prognostic marker of human esophageal squamous cell carcinoma. Clin Cancer Res 11: 6190–6197
Robinson MJ, Martin BA, Gootz TD, McGuirk PR, Moynihan M, Sutcliffe JA, Osheroff N (1991) Effects of quinolone derivatives on eukaryotic topoisomerase-II. A novel mechanism for enhancement of enzyme-mediated DNA cleavage. J Biol Chem 266: 14585–14592
Shalit I, Halperin D, Haite D, Levitov A, Romano J, Osherov N, Fabian I (2006) Anti-inflammatory effects of moxifloxacin on IL-8, IL-1β and TNF-α secretion and NFκB and MAP-kinase activation in human monocytes stimulated with Aspergillus fumigatus. J Antimicrob Chemother 57: 230–235
Shalit I, Horev-Azaria L, Fabian I, Blau H, Kariv N, Shechtman I, Alteraz H, Kletter Y (2002) Immunomodulatory and protective effects of moxifloxacin against Candida albicans induced bronchopneumonia in cyclophosphamide injected mice. Antimicrob Agents Chemother 46: 2442–2449
Shalit I, Nasrallah N, Bar-On S, Rabau M (1995) In vitro effect of ciprofloxacin and ofloxacin on murine and human colon carcinoma cell lines. Drugs 2 (49 Suppl): 296–297
Trevino JG, Summy JM, Gray MJ, Nilsson MB, Lesslie DP, Baker CH, Gallick GE (2005) Expression and activity of SRC regulate interleukin-8 expression in pancreatic adenocarcinoma cells: implications for angiogenesis. Cancer Res 65: 7214–7222
Usami I, Kubota M, Bessho R, Kataoka A, Koishi S, Watanabe K, Sawada M, Lin YW, Akiyama Y, Furusho K (1998) Role of protein tyrosine phosphorylation in etoposide-induced apoptosis and NF-κB activation. Biochem Pharmacol 55: 185–191
Villani F, Viola G, Vismara C, Laffranchi A, Di Russo A, Viviani S, Bonfante V (2002) Lung function and serum concentrations of different cytokines in patients submitted to radiotherapy and intermediate/high dose chemotherapy for Hodgkin's disease. Anticancer Res 22: 2403–2408
Weiss T, Shalit I, Blau H, Werber S, Halperin D, Levitov A, Fabian I (2004) Anti- inflammatory effects of MXF on activated human monocytic cells: inhibition of NFkB and MAPK activation and synthesis of proinflammatory cytokines. Antimicrob Agents Chemother 48: 1974–1982
Werber S, Shalit I, Fabian I, Steuer G, Weiss T, Blau H (2005) MXF inhibits cytokine- induced nitric oxide production and down-regulates expression of iNOS, NFkB and MAP kinases in human respiratory epithelial cells. J Antimicrob Chemother 55: 293–300
Won JH, Park SY, Nam SG, Park HJ, Choi JW, Lee KT (2005) Inhibition of lipopolysaccharide- induced expression of inducible nitric oxide and cyclooxygenase-2 by chiisanoside via suppression of nuclear factor-kappa B activation in RAW 264.7 macrophage cells. Biol Pharm Bull 28: 1919–1924
Zehavi-Willner T, Shalit I (1992) The inhibitory effects of ciprofloxacin on proliferation of a murine bladder carcinoma cell line. J Antimicrob Chemother 29: 323–328
Acknowledgements
This work constitutes a section of Debby Reuveni's PhD thesis at the Tel Aviv University, Tel Aviv Israel.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Fabian, I., Reuveni, D., Levitov, A. et al. Moxifloxacin enhances antiproliferative and apoptotic effects of etoposide but inhibits its proinflammatory effects in THP-1 and Jurkat cells. Br J Cancer 95, 1038–1046 (2006). https://doi.org/10.1038/sj.bjc.6603355
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6603355
Keywords
This article is cited by
-
Interaction between moxifloxacin and Mcl-1 and MITF proteins: the effect on growth inhibition and apoptosis in MDA-MB-231 human triple-negative breast cancer cells
Pharmacological Reports (2022)
-
Molecular docking studies on thirteen fluoroquinolines with human topoisomerase II a and b
In Silico Pharmacology (2017)
-
Moxifloxacin and ciprofloxacin induces S-phase arrest and augments apoptotic effects of cisplatin in human pancreatic cancer cells via ERK activation
BMC Cancer (2015)
-
Using antimicrobial adjuvant therapy in cancer treatment: a review
Infectious Agents and Cancer (2012)