Abstract
BRCA1/BRCA2 mutations account for a substantial proportion of familial breast cancer, but clearly mutations in additional genes exist, one candidate being the p53 gene. To evaluate its putative involvement in inherited predisposition to breast/ovarian cancer in Jewish high-risk women, mutational analysis of the p53 gene (exons 4–9) was carried out using exon-specific polymerase chain reaction followed by denaturing gradient gel electrophoresis (DGGE) analysis, complemented by DNA sequencing of abnormally migrating fragments. Overall, 132 Jewish breast cancer patient non-BRCA1/2 mutation carriers and 167 average risk controls (Ashkenazi (n=60), non-Ashkenazi (n=107)) were genotyped, and no inactivating p53 germline mutations were detected. Consistent migration abnormalities were noted in 167 fragments, 134 of which were shown to be the Arg72Pro polymorphism, whereas migration abnormalities in fragments containing exons 4 (n=2) and 6 (n=23) and introns 3 (n=4) and 9 (n=4) corresponded to five previously described polymorphisms. Allele distribution of the R72P missense mutation between ethnically diverse Jewish breast cancer cases and average risk controls showed significant differences: among non-Ashkenazi breast cancer cases, 62.5%, 33.3% and 4.2% were homozygous, heterozygous and homozygous for the Arg72, Arg72Pro and the Pro72 polymorphism, respectively, whereas for controls, the distribution was 22.4%, 65.4% and 12.2%, respectively (P=0.00052), and among Ashkenazi breast cancer cases, allele distribution was 68.5%, 29.6% and 1.9%, whereas for controls, the distribution was 50%, 40% and 10%, respectively (P=0.0125). We conclude that arginine homozygosity at codon 72 of the p53 gene is associated with a significant increased breast cancer risk in Jewish high-risk population.
Similar content being viewed by others
Main
Germline mutations in the BRCA1 (MIM#113705) and BRCA2 (MIM#600185) genes account for genetic predisposition and increased risk for breast and ovarian cancer in the majority of families with inherited predisposition to both these neoplasms and in 20–40% of families with site-specific breast cancer (Hall et al, 1990; Easton et al, 1993; Frank et al, 1998). In the majority of high-risk families of different ethnicities, germline mutations are scattered throughout both genes and are family specific (BIC database). In Jewish individuals, only a handful of recurring mutations have been described in high-risk families (Ganguly et al, 1997; Shiri-Sverdlov et al, 2000). Notably, among Ashkenazim (East European ancestry), three mutations in BRCA1 (185delAG, 5382InsC) and BRCA2 (6174delT) predominate, and can be detected in more than 80% of familial breast and ovarian cancer, in about 40–50% of site-specific familial breast cancer and in 2.5% of the general population of this ethnic group (Abeliovich et al, 1997). Among non-Ashkenazi (Sephardic) Jews, the 185delAG and the Tyr978X BRCA1 and the 8765delAT in BRCA2 mutations can be detected in high-risk families (Shiri-Sverdlov et al, 2001). Yet, a substantial proportion of familial breast cancer cases have no identifiable BRCA1/BRCA2 germline mutations (Tereschenko et al, 2002; Perkowska et al, 2003), and other, yet unidentified genetic factors underlie these cases (Slattery and Kerber, 1993). One of the most promising candidates as target for molecular analysis as an inherited breast cancer predisposition gene is the p53 tumour suppressor gene: it is frequently somatically mutated in a wide range of human cancers including breast cancer (Harris and Hollstein, 1993); germline mutations lead to an increased risk for developing diverse malignancies, including 25–30% of breast cancer cases (Bukholm et al, 1997), in the context of Li–Fraumeni syndrome (LFS) or LFL – Li–Fraumeni-like syndrome (Varley, 2003). In addition, based on its pivotal role in DNA damage repair and its physical and functional interactions with BRCA1 and BRCA2 proteins (Storey et al, 1998), p53 seems to be a strong candidate breast cancer predisposition gene. However, previous analyses of high-risk families of different ethnic background yielded a paucity of germline mutations in p53 gene in familial breast cancer (Zelada-Hedman et al, 1997; Balz et al, 2002).
In addition to bona fide inactivating mutations, which seem to cluster to the central region of the gene (exons 5–8) (Hartmann et al, 1995), there are several missense mutations within this gene that seem to have a deleterious effect on p53 function (p53 database). Notably, the Pro72 and Arg72 variants have been reported to differ in functional activity: the Arg72 variant was found to be more susceptible to degradation by the human papillomavirus (HPV) E6 type 18 protein (Storey et al, 1998), while Pro72 is a stronger inducer of transcription than Arg72. Additionally, the Arg72 variant suppressed effectively cellular transformation (Thomas et al, 1999), and was more efficient than the Pro72 variant at inducing apoptosis (Dumont et al, 2003).
In the present study, the putative contribution of p53 germline mutations to inherited predisposition to breast/ovarian cancer was assessed, initially by genotyping high-risk Jewish individual noncarriers of the predominant Jewish BRCA1/2 mutations for p53 germline mutations, and subsequently by comparing the distribution of the R72P alleles among cases and controls.
Materials and methods
DNA isolation
Genomic DNA was prepared from anticoagulated venous blood samples, using standard techniques, and using the PUREGene DNA extraction kit (Gentra Systems Inc., Minneapolis, MN, USA) and following the manufacturer's recommended protocol.
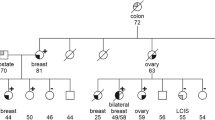
Breast cancer cases
Ashkenazi and non-Ashkenazi individuals who were counselled at the Oncogenetic services of the Sheba and Rambam Medical Centers were eligible for participation. Their ethnic origin was determined by an interview, and dating parental origin as far back as possible by at least three generations. All individuals had breast cancer and one of the following additional criteria: ovarian cancer; two first or second degree relatives with one of these neoplasms at any age; age at onset under 40 for breast cancer, bilateral breast cancer; cooccurrence of breast and ovarian cancer in one first-degree relative. The study was approved by the Institutional review board of both participating medical centers (Rambam and Sheba) and each participant signed a written, informed consent. All participants were tested, and found not to harbour any of the predominant Jewish mutations in BRCA1/BRCA2 (see below).
Controls
Jewish individuals of diverse ethnic origin who came for genetic counselling at the Genetics institutes in Sheba and Rambam Medical Centers served as ‘ethnic controls’. These individuals were either counselled for prenatal disorders or were counselled as to their risk for developing cancer, and none was deemed ‘high cancer risk’ by standard criteria. All tested individuals were unrelated to each other, had no personal or relevant family history of breast or ovarian cancer, and their precise ancestry was confirmed at least three generations back.
Mutation analyses of the predominant Jewish mutations in BRCA1 and BRCA2
Mutational analyses for the three predominant mutations (185delAG, 5382InsC in BRCA1 and 6174delT in BRCA2) were carried out by restriction enzyme digest of amplified polymerase chain reaction (PCR) product. The primers used generated novel restriction sites that distinguish the mutant from the wild-type allele. Thus, restriction enzyme digest followed PCR, and analysis of the digested PCR products on agarose gels was carried out as described previously (Abeliovich et al, 1997; Rohlfs et al, 1997). The Tyr978X mutation was detected by a modified PCR-restriction enzyme digest with EcoRV, as described previously (Theodor et al, 1998). With each gel, a positive control (i.e. a known mutation proven by DNA sequencing) was run in an adjacent lane.
Mutational analyses of the P53 gene
Polymerase chain reaction
Polymerase chain reactions were performed in a final volume of 50 μl containing 3 μl template DNA (about 50–100 ng), 10 pM of each primer, 200 mM of each dNTP, standard PCR buffer (1.5 mM MgCl2), 1 U of Taq DNA polymerase. Thermal cycling was accomplished by PTC-100-60 thermocycler (MJ Research Inc., Watertown, MA, USA). The cycling profile included an initial denaturation at 94°C for 5 min, followed by 35 cycles of thermal cycling including 94°C for 20 s, the designated annealing temperature (range 52–68°C) for 1 min, extension at 72°C for 20 s and a final extension cycle at 72°C for 5 min.
Denaturing gradient gel electrophoresis (DGGE) and sequence analysis of the p53 gene
Primer sequences, PCR conditions and DGGE analyses parameters were carried out under the conditions described previously (Guldberg et al, 1997). All consistently abnormally migrating fragments (i.e. repeated abnormalities on three independent PCRs) were subject to sequence analysis using the big Dye terminator chemistry and kit (PE Biosystems, Foster City, CA, USA), and using the ABI Prism 310 semiautomatic DNA sequencer (PE Biosystems).
Statistical analyses
χ2 was performed in order to evaluate Hardy–Weinberg equilibrium (HWE) in the control group, alleles's prevalence in ethnicities, association genotype/allele–phenotype, Hardy–Weinberg deviation (in the patient group), Fisher's exact test and Armitage's trend test (Crow, 2001). Type I error was set at 5%, as is the accepted practised level.
The websites for checking HWE in the control group, χ2 for genes and alleles association, HWE by the phenotypic categories in the patient group and Armitage's trend test: http://ihg.gsf.de/cgi-bin/hw/hwa1.pl, http://www.unc.edu/~preacher/chisq/chisq.htm.
Results
Characteristics of breast cancer cases
Overall, 132 Jewish breast cancer patients were analysed: 108 (82%) patients were of Ashkenazi origin and 24 (18%) were of non-Ashkenazi origin. Among individuals of Ashkenazi origin, 10 patients presented with bilateral breast cancer (9.25%); age range at diagnosis of first breast cancer was 23–70 years (46±10.1 years – mean±s.d.); mean age at counselling was 50.2±10.8 years; the interval between date of diagnosis and date of testing was 0.5–27 years (5.35±5.8 years).
Among non-Ashkenazi cases (n=24), three patients presented with bilateral breast cancer (12.5%), and the age range at diagnosis of first breast cancer was 26–61 years (42.6±9.8 years); mean age range at counselling was 49±10.6 years. The interval between date of diagnosis and date of testing ranged from 0.5 to 33 years (6.6±7.6 years).
Mutational analyses of the predominant BRCA1/BRCA2 Jewish mutations among cases
All cases were tested and found not to be carriers of one of the predominant mutations in BRCA1 (185delAG, 5382InsC) and BRCA2 (6174delT). The non-Ashkenazis were also analysed for the Tyr978X BRCA1 mutation, and none was a carrier.
Controls
The age range among Ashkenazi controls (n=60) was 27–65 years (39.3±8.8 years).
The age range among non-Ashkenazi controls (n=107) was 21–70 years (34.1±9.6 years).
Mutational analysis
DGGE analysis of exons 4–9 of the p53 gene revealed consistent migration abnormalities in 167 fragments; 134 of these fragments were shown to be the Arg72Pro polymorphism (see below). Migration abnormalities in other fragments containing exons 4 and 6 and introns 3 and 9 were detected in 2, 23, 4 and 4 patients, respectively. All abnormally migrating fragments were sequenced and results showed that all abnormal migration patterns could be attributed to previously described polymorphisms (Table 1). No inactivating mutations could be shown in any of the analysed individuals.
R72P analysis
The distribution of the Arg72Pro polymorphism in cases and controls is presented in Tables 2 and 3. Among cases, no deviation from the HWE was shown. Allele distribution of the R72P missense mutation among breast cancer cases (Ashkenazi and non-Ashkenazi) and average risk controls (Ashkenazi (n=60), non-Ashkenazi (n=107)) showed significant differences: among non-Ashkenazi cases, 62.5%, 33.3% and 4.2% were homozygous, heterozygous and homozygous for the Arg72, Arg72Pro and the Pro72 polymorphisms, respectively, whereas for controls the distribution was 22.4%, 65.4% and 12.2%, respectively (P=0.00052), and among Ashkenazi cases, allele distribution was 68.5%, 29.6% and 1.9%, whereas for controls, the distribution was 50%, 40% and 10%, respectively (P=0.0125) (Tables 2 and 3).
In Armitage's trend test, which examines genotype–phenotype correlation, Arg72 homozygosity was significantly associated with breast cancer cases for the Ashkenazi subgroup (P=0.00452) as well as in the non-Ashkenazi subgroup (P=0.0075).
Analysis by allele prevalence (A/P) also shows a significant association between the arginine-bearing allele and high-risk cases (P=0.00432 for Ashkenazi origin; P=0.02412 for non-Ashkenazi origin).
Discussion
In the present study, no inactivating germline mutations in exons 4–9 of the p53 gene were detected in high-risk Jewish individuals who are not carriers of any of the predominant Jewish mutations in BRCA1/BRCA2. Previous analyses of high-risk families of different ethnic background yielded a paucity of germline mutations in p53 gene in familial breast cancer: only two mutations were identified among 237 high-risk Norwegian individuals (Borresen et al, 1992), one mutation among 126 high-risk American individuals (Sidransky et al, 1992) and one mutation among 21 families from the UK (Evans et al, 2002). Similar to the results of the present study, no inactivating p53 germline mutations were found in any of Swedish familial breast cancer patients (Zelada-Hedman et al, 1997) or in German breast and/or ovarian cancer families (Balz et al, 2002). Thus, despite features suggesting that this might be a strong candidate underlying inherited breast cancer predisposition, p53 germline mutations probably contribute little to these families, unless it is in the context of LFS or LFS-like phenotype. It is still possible that germline sequence alterations in the p53 gene affect breast cancer risk. Intronic variants within the p53 gene have a functional effect on p53 protein activity and occur at high frequency in familial breast cancer cases. Lehman et al (2000) detected an intronic variant (13964G/C) at a significantly high frequency among familial breast cancer cases (n=42), with evidence that this sequence variant is associated with prolonged in vitro survival in response to cisplatinum treatment and showed decreased chemotherapy-induced apoptosis (Lehman et al, 2000). The data regarding the high rate of this specific polymorphism in high-risk women could not be reproduced in Australian women (Marsh et al, 2001). In addition, intronic polymorphisms with no known functional consequences (e.g. intron 3–16 bp insertion) were reported to be over-represented in Swedish (Sjalander et al, 1996) and German breast cancer-prone families (Wang-Gohrke et al, 1998).
An intriguing finding in the present study is that the distribution of the R72P missense mutation significantly differs in affected individuals compared with ethnically matched controls. Specifically, ethnically diverse Jewish breast cancer individuals are significantly more likely to be R72 homozygotes, compared with average risk, unaffected individuals.
The Pro72 and Arg72 p53 gene variants have been reported to display different functional activities: the Arg72 variant is more susceptible to degradation by the HPV E6 type 18 protein (Storey et al, 1998), while Pro72 is a stronger inducer of transcription than the Arg72 variant. Additionally, the Arg72 variant suppressed effectively cellular transformation (Thomas et al, 1999), and was more efficient than the Pro72 variant in inducing apoptosis (Dumont et al, 2003).
The rate of this sequence variant has also been evaluated in breast cancer cases in ethnically diverse populations, with inconsistent results. In line with the findings in the present study, a significantly higher prevalence of homozygosity for the p53 arginine-bearing allele was observed in Turkish breast cancer patients compared with controls (Buyru et al, 2003), whereas among Japanese breast cancer cases, Pro72 homozygosity was significantly more prevalent than in controls (32% Pro72 in cases and 40.4% in controls) (Huang et al, 2003). Notably, there was no evidence of association between p53 codon 72 polymorphism and breast cancer risk Tunisian (Mabrouk et al, 2003), and Russian individuals (Suspitsin et al, 2003). In addition, this polymorphic variant was reported to be associated with breast cancer survival among English breast cancer patients, but this association lacked statistical significance in multivariate analysis (Goode et al, 2002).
The limitations of this study should be pointed out. This is a limited study encompassing only women affected with breast cancer, counselled and tested in two medical centres in Israel. The implications to other breast cancer populations, even among Jewish individuals, are unclear and need to be validated. Furthermore, the applicability of this finding to average risk population is unclear and needs to be established.
In conclusion, the contribution of p53 germline mutations to inherited predisposition to breast cancer by inactivating mutations seems to be limited in Jewish women. It seems that a common missense mutation (R72P) confers an increased risk to breast cancer in familial cases of Jewish origin. The applicability and the generalisability of this preliminary finding need to be confirmed.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abeliovich D, Kaduri L, Lerer I, Weinberg N, Amir G, Sagi M, Zlotogora J, Heching N, Peretz T (1997) The founder mutations 185delAG and 5382insC in BRCA1 and 6174delT in BRCA2 appear in 60% of ovarian cancer and 30% of early-onset breast cancer patients among Ashkenazi women. Am J Hum Genet 60: 505–514
Balz V, Prisack HB, Bier H, Bojar H (2002) Analysis of BRCA1, TP53, and TSG101 germline mutations in German breast and/or ovarian cancer families. Cancer Genet Cytogenet 138: 120–127
Borresen A, Andersen T, Garber J, Barbier-Piraux N, Thorlacius S, Eyfjord J, Ottestad L, Smith-Sorensen B, Hovig E, Malkin D (1992) Screening for germ line TP53 mutations in breast cancer patients. Cancer Res 52: 3234–3236
Bukholm I, Nesland J, Karesen R, Jacobsen U, Borresen-Dale A (1997) Expression of E-cadherin and its relation to the p53 protein status in human breast carcinomas. Virchows Arch 431: 317–321
Buyru N, Tigli H, Dalay N (2003) P53 codon 72 polymorphism in breast cancer. Oncol Rep 10: 711–714
Crow JF (2001) The beanbag lives on. Nature 409: 771
Dumont P, Leu JI, Della Pietra III AC, George DL, Murphy M (2003) The codon 72 polymorphic variants of p53 have markedly different apoptotic potential. Nat Genet 33: 357–365
Easton DF, Bishop DT, Ford D, Crockford GP (1993) Genetic linkage analysis in familial breast and ovarian cancer: results from 214 families. The Breast Cancer Linkage Consortium. Am J Hum Genet 52: 678–701
Evans D, Birch J, Thorneycroft M, McGown G, Lalloo F, Varley J (2002) Low rate of TP53 germline mutations in breast cancer/sarcoma families not fulfilling classical criteria for Li–Fraumeni syndrome. J Med Genet 39: 941–944
Frank TS, Manley SA, Olopade OI, Cummings S, Garber JE, Bernhardt B, Antman K, Russo D, Wood ME, Mullineau L, Isaacs C, Peshkin B, Buys S, Venne V, Rowley PT, Loader S, Offit K, Robson M, Hampel H, Brener D, Winer EP, Clark S, Weber B, Strong LC, Thomas A (1998) Sequence analysis of BRCA1 and BRCA2: correlation of mutations with family history and ovarian cancer risk. J Clin Oncol 16: 2417–2425
Ganguly A, Leahy K, Marshall AM, Dhulipala R, Godmilow L, Ganguly T (1997) Genetic testing for breast cancer susceptibility: frequency of BRCA1 and BRCA2 mutations. Genet Test 1: 85–90
Goode EL, Dunning AM, Kuschel B, Healey CS, Day NE, Ponder BA, Easton DF, Pharoah PP (2002) Effect of germ-line genetic variation on breast cancer survival in a population-based study. Cancer Res 62: 3052–3057
Guldberg P, Nedergaard T, Nielsen HJ, Olsen AC, Ahrenkiel V, Zeuthen J (1997) Single-step DGGE-based mutation scanning of the p53 gene: application to genetic diagnosis of colorectal cancer. Hum Mutat 9: 348–355
Hall JM, Lee MK, Newman B, Morrow JE, Anderson LA, Huey B, King MC (1990) Linkage of early-onset familial breast cancer to chromosome 17q21. Science 250: 1684–1689
Harris CC, Hollstein M (1993) Clinical implications of the p53 tumor-suppressor gene. N Engl J Med 329: 1318–1327
Hartmann A, Blaszyk H, McGovern RM, Schroeder JJ, Cunningham J, De Vries EM, Kovach JS, Sommer SS (1995) p53 gene mutations inside and outside of exons 5–8: the patterns differ in breast and other cancers. Oncogene 10: 681–688
Huang XE, Hamajima N, Katsuda N, Matsuo K, Hirose K, Mizutani M, Iwata H, Miura S, Xiang J, Tokudome S, Tajima K (2003) Association of p53 codon Arg72Pro and p73 G4C14-to-A4T14 at exon 2 genetic polymorphisms with the risk of Japanese breast cancer. Breast Cancer 10: 307–311
Lehman TA, Haffty BG, Carbone CJ, Bishop LR, Gumbs AA, Krishnan S, Shields PG, Modali R, Turner BC (2000) Elevated frequency and functional activity of a specific germ-line p53 intron mutation in familial breast cancer. Cancer Res 60: 1062–1069
Mabrouk I, Baccouche S, El-Abed R, Mokdad-Gargouri R, Mosbah A, Said S, Daoud J, Frikha M, Jlidi R, Gargouri A (2003) No evidence of correlation between p53 codon 72 polymorphism and risk of bladder or breast carcinoma in Tunisian patients. Ann NY Acad Sci 1010: 764–770
Marsh A, Spurdle AB, Turner BC, Fereday S, Thorne H, Pupo GM, Mann GJ, Hopper JL, Sambrook JF, Chenevix-Trench G (2001) The intronic G13964C variant in p53 is not a high-risk mutation in familial breast cancer in Australia. Breast Cancer Res 3: 346–349
Perkowska M, BroZek I, Wysocka B, Haraldsson K, Sandberg T, Johansson U, Sellberg G, Borg A, Limon J (2003) BRCA1 and BRCA2 mutation analysis in breast-ovarian cancer families from northeastern Poland. Hum Mutat 21: 553–554
Rohlfs EM, Learning WG, Friedman KJ, Couch FJ, Weber BL, Silverman LM (1997) Direct detection of mutations in the breast and ovarian cancer susceptibility gene BRCA1 by PCR-mediated site-directed mutagenesis. Clin Chem 43: 24–29
Shiri-Sverdlov R, Gershoni-Baruch R, Ichezkel-Hirsch G, Gotlieb WH, Bruchim Bar-Sade R, Chetrit A, Rizel S, Modan B, Friedman E (2001) The Tyr978X BRCA1 mutation in non-Ashkenazi Jews: occurrence in high-risk families, general population and unselected ovarian cancer patients. Community Genet 4: 50–55
Shiri-Sverdlov R, Oefner P, Green L, Baruch RG, Wagner T, Kruglikova A, Haitchick S, Hofstra RM, Papa MZ, Mulder I, Rizel S, Bar Sade RB, Dagan E, Abdeen Z, Goldman B, Friedman E (2000) Mutational analyses of BRCA1 and BRCA2 in Ashkenazi and non-Ashkenazi Jewish women with familial breast and ovarian cancer. Hum Mutat 16: 491–501
Sidransky D, Tokino T, Helzlsouer K, Zehnbauer B, Rausch G, Shelton B, Prestigiacomo L, Vogelstein B, Davidson N (1992) Inherited p53 gene mutations in breast cancer. Cancer Res 52: 2984–2986
Sjalander A, Birgander R, Hallmans G, Cajander S, Lenner P, Athlin L, Beckman G, Beckman L (1996) p53 polymorphisms and haplotypes in breast cancer. Carcinogenesis 17: 1313–1316
Slattery ML, Kerber RA (1993) A comprehensive evaluation of family history and breast cancer risk. The Utah Population Database. JAMA 270: 1563–1568
Storey A, Thomas M, Kalita A, Harwood C, Gardiol D, Mantovani F, Breuer J, Leigh IM, Matlashewski G, Banks L (1998) Role of a p53 polymorphism in the development of human papillomavirus-associated cancer. Nature 393: 229–234
Suspitsin EN, Buslov KG, Grigoriev MY, Ishutkina JG, Ulibina JM, Gorodinskaya VM, Pozharisski KM, Berstein LM, Hanson KP, Togo AV, Imyanitov EN (2003) Evidence against involvement of p53 polymorphism in breast cancer predisposition. Int J Cancer 103: 431–433
Tereschenko IV, Basham VM, Ponder BA, Pharoah PD (2002) BRCA1 and BRCA2 mutations in Russian familial breast cancer. Hum Mutat 19: 184
Theodor L, Bar-Sade R, Kruglikova A, Ben-Baruch G, Risel S, Shiri-Sverdlov R, Hirsh Yechezkel G, Modan B, Papa MZ, Rechavi G, Friedman E (1998) An identical novel mutation in BRCA1 and a common haplotype in familial ovarian cancer in non-Ashkenazi Jews. Br J Cancer 77: 1880–1883
Thomas M, Kalita A, Labrecque S, Pim D, Banks L, Matlashewski G (1999) Two polymorphic variants of wild-type p53 differ biochemically and biologically. Mol Cell Biol 19: 1092–1100
Varley JM (2003) Germline TP53 mutations and Li–Fraumeni syndrome. Hum Mutat 21: 313–320
Wang-Gohrke S, Rebbeck TR, Besenfelder W, Kreienberg R, Runnebaum IB (1998) p53 germline polymorphisms are associated with an increased risk for breast cancer in German women. Anticancer Res 18: 2095–2099
Zelada-Hedman M, Borresen-Dale AL, Claro A, Chen J, Skoog L, Lindblom A (1997) Screening for TP53 mutations in patients and tumours from 109 Swedish breast cancer families. Br J Cancer 75: 1201–1204
Acknowledgements
This study was in part sponsored by a grant from the Middle East Cancer Consortium (MECC) to Eitan Friedman.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Ohayon, T., Gershoni-Baruch, R., Papa, M. et al. The R72P P53 mutation is associated with familial breast cancer in Jewish women. Br J Cancer 92, 1144–1148 (2005). https://doi.org/10.1038/sj.bjc.6602451
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6602451
Keywords
This article is cited by
-
p.Arg72Pro polymorphism of P53 and breast cancer risk: a meta-analysis of case-control studies
BMC Medical Genetics (2020)
-
The association of polymorphic markers Arg399Gln of XRCC1 gene, Arg72Pro of TP53 gene and T309G of MDM2 gene with breast cancer in Kyrgyz females
BMC Cancer (2017)
-
Breast cancer risk in relation to TP53 codon 72 and CDH1 gene polymorphisms in the Bangladeshi women
Tumor Biology (2016)
-
Association of the TP53 codon 72 polymorphism and breast cancer risk: a meta-analysis
SpringerPlus (2014)
-
RAD51 135G>C and TP53 Arg72Pro polymorphisms and susceptibility to breast cancer in Serbian women
Familial Cancer (2014)