Abstract
To investigate the occurrence of somatic mitochondrial DNA (mtDNA) mutations in human primary endometrial carcinomas, we sequenced the D-loop region, the 12S and 16S rRNA genes of mtDNA of cancer tissues and their matched normal controls. About 56% (28 out of 50) of cases carry one or more somatic changes in mtDNA including deletion, point mutation and mitochondrial microsatellite instability (mtMSI), namely the change in length of short base-repetitive sequences of mtDNA. In particular, mtMSI was frequently detected in 89% (25 out of 28) of all the cases carrying somatic changes followed by point mutations (25%; seven out of 28) and deletion (3.5%; one out of 28). The CCCCCTCCCC sequences located in the Hypervariable Regions I and II of the D-loop and 12S rRNA gene are instability hot spot regions in endometrial carcinomas. It is suggested that errors in replication may account for the high frequency of mtMSI in human endometrial carcinomas. The relatively high prevalence of mtMSI may be a potential new tool for detection of endometrial cancer.
Similar content being viewed by others
Main
The occurrence of somatic mitochondrial DNA (mtDNA) mutations in various human cancers has recently been reported (Polyak et al, 1998; Fliss et al, 2000; Jeronimo et al, 2001; Jones et al, 2001; Kirches et al, 2001; Liu et al, 2001; Maximo et al, 2001; Parrella et al, 2001). The genetic changes include deletions, point mutations and mitochondrial microsatellite instability (mtMSI), defined as the change in length in short base-repetitive sequences of mtDNA. Most of the mtDNA mutations were point mutations involving T → C or G → A transitions, probably induced by oxidative stress. In contrast, DNA deletions and mtMSI, which might be generated during erroneous replication, occurred sporadically.
This D-loop region is often selected for study in view of its tendency to accumulate mutations more rapidly than other regions of mtDNA. In our previous study, we sequenced the D-loop region (nucleotide position (np) 16024–576) of 15 pairs of ovarian tumour and matched normal samples and found a total of nine somatic mutations in three samples (20%; three out of 15) (Liu et al, 2001). In addition, in the same study, we completely sequenced the mitochondrial genomes of 10 ovarian tumour samples and found six somatic mutations, respectively, in six samples (60%; six out of 10) (Liu et al, 2001). Four point mutations and one mtMSI out of the six mutations were detected in the region containing the D-loop, 12S and 16S rRNA genes. Indeed, consistent with other studies, the majority of the mtDNA mutations have been found in the D-loop and the adjacent genes in several tumours (Fliss et al, 2000).
So far, the role of mtDNA in endometrial carcinomas has not been reported. To further our investigation on the occurrence of mtDNA mutations in human cancers, we selectively (based on our previous results) sequenced the D-loop, the 12S and 16S rRNA genes (spanning from np 16024–3229) of mtDNA of endometrial carcinomas.
Materials and methods
Fifty frozen samples of primary endometrial carcinomas and those of their matched normal tissues (including cervix and/or lymphocytes) obtained after surgery were retrieved without specific selection from our tissue bank and used for DNA analysis in this study (approved (No.: EC 1517-00) by the Ethics Committee of the University of Hong Kong). In addition, pathologic paraffin-embedded tumour tissues and sera (if available) from the same set of individuals were also used to cross-check the DNA changes found. DNA was extracted from frozen tissues, paraffin-embedded tumour tissues and sera by the methods described previously (Liu et al, 2001). The segment of mtDNA encompassing the D-loop, 12S and 16S rRNA genes was amplified from tissue extracts by long-range and high-fidelity PCR amplification system under conditions as recommended by the manufacturer (Roche Diagnostics GmbH, Mannheim, Germany). Sequencing of the PCR products was carried out using the same procedure as we used in our previous study of mtDNA mutations in ovarian carcinomas (Liu et al, 2001). DNA sequences were analysed using Dnasis software. In addition, electropherograms were read manually to identify mutant sequence present at a low level. From our experience, an mtDNA sequence constituting as low as 15% in a heteroplasmic sample (containing a mixture of mtDNA sequences) can be detectable by DNA sequencing. To confirm the DNA changes found in frozen tissues, the corresponding mtDNA fragments within DNA extracted from paraffin-embedded tissues and serum from the corresponding individuals were also analysed. Although paraffin-embedded DNA may undergo some degradation after chemical treatment for fixation, the high copy number of mitochondrial genomes per cell makes PCR amplification of short mtDNA fragments readily achievable, yielding reproducible data. Details of PCR primers and sequencing primers are available upon request from the authors.
Results and discussion
Fifty samples of primary endometrial carcinomas and their matched normal controls were studied to determine whether mtDNA mutations could be identified. Indeed, 56% (28 out of 50) of the endometrial tumours were found to carry one or more somatic mtDNA mutations including deletions, point mutations and mtMSI (Figure 1; Table 1). Somatic mtDNA mutations are defined as those present in the tumour but not in the normal tissue from the patient concerned. The revised Cambridge sequence (wild type) of the relevant position, in each case, is shown for reference in Table 1. The mtDNA in normal tissue of individual patients constitutes the mitochondrial haplotype but may differ from this reference sequence, thereby representing a germline polymorphism.
Location of somatic mtDNA mutations detected in a particular region (np from 16024–3229) of mitochondrial genome in endometrial carcinomas. The locations of the mtDNA mutations are indicated by arrows (positions not drawn exactly to scale). The arrows on top indicate the positions of the seven point mutations and the 50-bp deletion (arrow with a black circle at the tail). The arrows at the bottom indicate the positions of the mtMSI. Numbers in parentheses indicate the number of mtMSI detected out of 50 endometrial tumours. Gaps between genes indicate the positions of tRNAs.
In just one (U9; Table 1) of the 50 tumour samples, a homoplasmic mtDNA deletion involving a pair of 9-bp direct repeats (CCAAACCCC) located at np 298–306 and np 348–356 was detected in the D-loop. The mtDNA mutation deleted 50-bp of DNA sequence including the Conserved Sequence Block (CSB) II starting at np 298 with one of the direct repeats retained.
In addition, a total of seven somatic point mutations (14%; seven out of 50) were detected in the current set of endometrial tumour samples (Table 1). Three different mutations were detected in the D-loop, one in each of the samples G12, U34 and U10. Another three mutations were detected in the 12S rRNA gene (in U27, U59 and G29) and a further one in the 16S rRNA gene (in U44). They were all novel mtDNA mutations except the one at np 152 of G12 (Liu et al, 2001). The mutations were all either T → C or G → A transitions.
Other than deletion and point mutations, a high frequency (50%; 25 out of 50) of mtMSI was detected, especially in the D-loop region in these 50 endometrial tumour samples. We observed mtMSI in four different regions (Table 1), including CA repeats at np 514–523 within a nonfunctional D-loop sequence and a common homopolymeric C stretch interrupted by a T (CCCCCTCCCC) at each of the following locations: np 956–965 within the 12S rRNA gene; np 303–315 within the CSB II; and np 16184–16193 at the 3′ end of the termination-associated sequence.
The sequencing details illustrating two different features of the occurrence of mtMSI are depicted in Figure 2. The normal DNA of sample U111 (Figure 2A) is homoplasmic containing a consecutive set of four CA dinucleotides starting from np 514. In the tumour, the sequence has expanded to five CA dinucleotides. This CA-repeat instability was only found in U111 (2%; one out of 50) (Table 1). A more complex example of mtMSI is shown in Figure 2B. The normal DNA of sample U109 is heteroplasmic. It contains stretches of cytosine residues of different lengths starting from np 303 (C8, C9 and C10 are in similar proportions but C11 is a minority species). In the tumour, the relative predominance of these length variants has shifted markedly, the mtDNA sequence now containing mainly C8 and a small proportion of C9. The use of DNA sequencing to detect mtMSI allows us to determine exactly the somatic changes and to estimate the relative proportion of each type of sequence within a heteroplasmic sample.
Detection of mtMSI in endometrial carcinomas by DNA sequencing. (A) The normal sequence (commencing at np 514, arrows) of U111 (Table 1) is a microsatellite DNA containing four CA repeats. In the tumour, it was expanded to carry five CA repeats. (B) The mtDNA sequence found in the normal tissue of U109 (Table 1) contained heteroplasmic stretch of C residues, comprising C8, C9, C10 and C11 (commencing at np 303, arrows). In the tumour, mtDNA sequence contained mainly C8 and a small proportion of C9.
Novel mtMSI located within the 12S rRNA gene (Table 1) was found in the present study. The changes were either the deletion/insertion of one cytosine residue at the homopolymorphic C tract in front of the thymine (detected in U24; U32; U120) or the germline T → C polymorphism producing an extra long homopolymorphic C tract leading to DNA instability (detected in U27). The frequency of occurrence was 8% (four out of 50).
We observed mtMSI in two other regions in the D-loop. Changes in length of the homopolymorphic cytosine at np 303–309 were detected in 32% (16 out of 50) of endometrial carcinoma samples. Another mtMSI involves the CCCCCTCCCC sequence at np 16184–16193 at the 3′ end of the termination-associated sequence and within the 7S DNA binding site. The germline T → C polymorphism at np 16 189 produced an uninterrupted C tract that was unstable in the tumour (Table 1). The frequency of occurrence was 14% (seven out of 50).
The mtMSI within the mononucleotide repeat at np 303–309 is frequently observed in endometrial tumour samples (32%; 16 out of 50). This mtMSI was also detected in ovarian carcinomas (Liu et al, 2001) and other human tumours (Sanchez-Cespedes et al, 2001) with an average frequency of 22% (55 out of 247). In concordance with the data of Sanchez-Cespedes et al (2001), patients carrying mtDNA instability at this particular region had higher levels of heteroplasmic length variants in the normal tissues than patients not showing instability. Heteroplasmic length variants of this region were found to be quite constant during life (Lagerstrom-Fermer et al, 2001). This region is part of the CSB II and the binding site of replication primer. It is not clear if the relatively unstable somatic changes would alter mtDNA replication in the tumour cell.
The germline T → C polymorphism at np 16189 producing an uninterrupted C tract was unstable in the endometrial tumour. The frequency of occurrence was 14% (seven out of 50). This particular mtMSI has been reported in glioblastoma (Kirches et al, 2001) at a frequency of 23% (four out of 17). These sequence variants when in the mitochondrial haplotype have been considered as a significant genetic predisposing factor for Type II diabetes (Poulton, 1998). Indeed, we have recently observed (Liu et al, 2003) an elevated frequency of this haplotypic variant in patients with endometrial carcinomas, suggesting that this may also be a possible genetic predisposing factor for such human cancers.
The data presented here indicate a remarkably high frequency of somatic mtDNA mutations in endometrial carcinomas. Although the entire mitochondrial genome was not sequenced, this particular stretch of mtDNA may be a hot spot region of somatic mutations. The most abundant type of mutation observed in the D-loop region of endometrial carcinomas is mtMSI. While the mtDNA sequence variants representing the somatic mutations occurring here, including point mutations and mtMSI variants, are often found as germline polymorphisms in the human population, it is worthwhile considering relevant issues including their possible differential occurrence in various cancers, their proposed mechanisms of formation and their potential clinical significance.
Variation in the CA repeats was detected in only one (2%; one out of 50) of the endometrial carcinoma samples. Instability of the CA repeats was also found at a low frequency in ovarian (8%; two out of 25) (Liu et al, 2001), gastric (19%; six out of 32) (Maximo et al, 2001) and glioblastoma (6%; one out of 17) (Kirches et al, 2001) cancers. However, there is a significantly higher frequency of the CA-repeat instability in breast cancer (42.5%; 17 out of 40) (Richard et al, 2000). On the basis of these findings, we suggest that somatic mtMSI occurs differentially in different tumours.
Malfunctions of mismatch repair genes have been associated with nuclear MSI. However, to date, no mismatch repair genes have been found responsible for the maintenance of mammalian mitochondrial genome. The occurrence of high frequency (50%; 25 out of 50) of mtMSI in endometrial tumours indicates that DNA repair in mitochondria is highly inefficient after malignant transformation. The different frequencies of occurrence of the mtMSI at the mononucleotide repeat at np 303–309 in different tumour cell types suggests that deficits in mismatch repair function in mitochondria may vary from one tumour to another.
We detected a higher frequency of mtMSI than point mutations in human endometrial carcinomas. This may be explained by the different mechanisms of mtDNA alteration and/or repair in different tissues during carcinogenesis. The occurrence of mtMSI may derive mainly from erroneous replication, whereas point mutations may be attributed to oxidative damage caused by reactive oxygen species. In addition, a recent study (Longley et al, 2001) suggests that the homopolymorphic nucleotide tracts in mtDNA are error-prone because of the low frameshift fidelity of the DNA polymerase gamma that carries out the mtDNA replication. Thus, mtMSI in endometrial carcinomas may be mainly attributed to errors of replication. Moreover, there is supportive evidence that there are cell-specific differences in the repair of mtDNA damage (LeDoux and Wilson, 2001). The differential occurrence of mtDNA mutations in various cancers may be partly due to the prominence of different repair mechanisms in different tumour cell types.
The active generation of new mtDNA variants by replication error and inefficient repair is not the only explanation for the appearance of mtMSI. Somatic mtDNA mutations accumulated in tumours have been proposed to be the result of random genetic drift (Coller et al, 2001; Jones et al, 2001). This means that the pre-existing sequence variants, which could be present at a low level among the heteroplasmic population of mtDNA in the progenitor cells, could have outgrown, without any selection, other mtDNA molecules after the hundreds or thousands of cell division cycles leading to the clinically manifested tumour. Since many somatic mutations were found in mtDNA sequences without functional significance, for example, within the D-loop region, the presence of somatic mtDNA mutations in tumours might not necessarily lead to mitochondrial dysfunction. In this view, random genetic drift could satisfactorily explain the occurrence of somatic mtDNA mutations during carcinogenesis. A more detailed treatment of these ideas has recently been presented by Chinnery et al (2002).
Nevertheless, it is still open to question whether there might be a functional significance of the various mtMSI, point mutations and deletions that are found in cancer tissues as homoplasmic somatic mutations. It is conceivable that some mutations may be functionally selected during neoplastic expansion. The possible functional impact of somatic mtDNA mutations in cancer should therefore be investigated, especially concerning those mutations lying outside noncoding or nonconserved regions.
Finally, in a clinical context, the high frequency of mitochondrial genome instability, in combination with PCR-based assays of high sensitivity, may be a potential new tool for endometrial cancer detection (Parrella et al, 2001). Somatic mtMSI involving the change in DNA length, even though the difference is only 1 or 2 bp, can be readily detected by polyacrylamide gel electrophoresis (Figure 3). In general, the bandshifts or band spreading observed by gel electrophoresis after PCR amplification of tumour mtDNA reflects the distribution of novel or multiple sequence variants in the tumour compared to normal tissue from the same patient (see legend to Figure 3 and relevant parts of Table 1). One particular mutation, the mtMSI variant at the mononucleotide repeat at np 303–309 (Table l; see also foregoing discussion), because of its frequent occurrence in various cancers, may be considered as a potential new tool for early cancer detection. In this case, the application of PCR coupled with gel electrophoresis lends itself to rapid analysis of multiple samples.
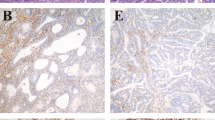
Detection of mtMSI in endometrial carcinomas by polyacrylamide gel electrophoresis. A homopolymeric C stretch interrupted by a T (CCCCCTCCCC) at 16184–16193 was analysed. As a control, U46 carried the wild-type sequence in this segment of mtDNA in both the normal (N) and tumour (T) tissues. The PCR product is a single band of 109 bp and band shifting was not observed. In contrast, both U44 and G29 carried a germline polymorphism T to C at np 16189 to produce an interrupted C stretch. Instability at this C stretch gave rise to heteroplasmic sequences and resulted in band shifting or smearing in PCR products derived from tumour samples. In sample U44, PCR product raised from normal tissue was a single band carrying C10, while the multiple PCR products (carrying C10, C11, and C12) were seen in the tumour sample, giving rise to a smeared band on the gel. Similarly, in sample G29, PCR product raised from normal was a single band carrying C7, while multiple PCR products (carrying C7, C8, C9 and C10) were seen in the tumour sample. The lane marked (M) contains 50 bp DNA markers (sizes of two bands shown in bp).
Accession codes
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Chinnery PF, Samuels DC, Elson J, Turnbull DM (2002) Accumulation of mitochondrial DNA mutations in ageing, cancer, and mitochondrial disease: is there a common mechanism? Lancet 360: 1323–1325
Coller HA, Khrapko K, Bodyak ND, Nekhaeva E, Herrero-Jimenez P, Thilly WG (2001) High frequency of homoplasmic mitochondrial DNA mutations in human tumors can be explained without selection. Nat Genet 28: 147–150
Fliss MS, Usadel H, Caballero OL, Wu L, Buta MR, Eleff SM, Jen J, Sidransky D (2000) Facile detection of mitochondrial DNA mutations in tumors and bodily fluids. Science 287: 2017–2019
Jeronimo C, Nomoto S, Caballero OL, Usadel H, Henrique R, Varzim G, Oliveira J, Lopes C, Fliss MS, Sidransky D (2001) Mitochondrial mutations in early stage prostate cancer and bodily fluids. Oncogene 20: 5195–5198
Jones JB, Song JJ, Hempen PM, Parmigiani G, Hruban RH, Kern SE (2001) Detection of mitochondrial DNA mutations in pancreatic cancer offers a ‘mass’ive advantage over detection of nuclear DNA mutations. Cancer Res 61: 1299–1304
Kirches E, Krause G, Warich-Kirches M, Weis S, Schneider T, Meyer-Puttlitz B, Mawrin C, Dietzmann K (2001) High frequency of mitochondrial DNA mutations in glioblastoma multiforme identified by direct sequence comparison to blood samples. Int J Cancer 93: 534–538
Lagerstrom-Fermer M, Olsson C, Forsgren L, Syvanen AC (2001) Heteroplasmy of the human mtDNA control region remains constant during life. Am J Hum Genet 68: 1299–1301
LeDoux SP, Wilson GL (2001) Base excision repair of mitochondrial DNA damage in mammalian cells. Prog Nucleic Acid Res Mol Biol 68: 273–284
Liu VWS, Shi HH, Cheung ANY, Chiu PM, Leung TW, Nagley P, Wong LC, Ngan HYS (2001) High incidence of somatic mitochondrial DNA mutations in human ovarian carcinomas. Cancer Res 61: 5998–6001
Liu VWS, Wang Y, Yang HJ, Tsang PCK, Ng TY, Wong LC, Nagley P, Ngan HYS (2003) Mitochondrial DNA variant (16189T>C) is associated with susceptibility to endometrial cancer. Hum Mutat, in press
Longley MJ, Nguyen D, Kunkel TA, Copeland WC (2001) The fidelity of human DNA polymerase gamma with and without exonucleolytic proofreading and the p55 accessory subunit. J Biol Chem 276: 38555–38562
Maximo V, Soares P, Seruca R, Rocha AS, Castro P, Sobrinho-Simoes M (2001) Microsatellite instability, mitochondrial DNA large deletions, and mitochondrial DNA mutations in gastric carcinoma. Genes Chromosomes Cancer 32: 136–143
Parrella P, Xiao Y, Fliss M, Sanchez-Cespedes M, Mazzarelli P, Rinaldi M, Nicol T, Gabrielson E, Cuomo C, Cohen D, Pandit S, Spencer M, Rabitti C, Fazio VM, Sidransky D (2001) Detection of mitochondrial DNA mutations in primary breast cancer and fine-needle aspirates. Cancer Res 61: 7623–7626
Polyak K, Li Y, Zhu H, Lengauer C, Willson JK, Markowitz SD, Trush MA, Kinzler KW, Vogelstein B (1998) Somatic mutations of the mitochondrial genome in human colorectal tumours. Nat Genet 20: 291–293
Poulton J (1998) Does a common mitochondrial DNA polymorphism underlie susceptibility to diabetes and the thrifty genotype? Trends Genet 14: 387–389
Richard SM, Bailliet G, Paez GL, Bianchi MS, Peltomaki P, Bianchi NO (2000) Nuclear and mitochondrial genome instability in human breast cancer. Cancer Res 60: 4231–4237
Sanchez-Cespedes M, Parrella P, Nomoto S, Cohen D, Xiao Y, Esteller M, Jeronimo C, Jordan RC, Nicol T, Koch WM, Schoenberg M, Mazzarelli P, Fazio VM, Sidransky D (2001) Identification of a mononucleotide repeat as a major target for mitochondrial DNA alterations in human tumors. Cancer Res 61: 7015–7019
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Liu, V., Yang, H., Wang, Y. et al. High frequency of mitochondrial genome instability in human endometrial carcinomas. Br J Cancer 89, 697–701 (2003). https://doi.org/10.1038/sj.bjc.6601110
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6601110
Keywords
This article is cited by
-
Detection of novel mitochondrial mutations in cytochrome C oxidase subunit 1 (COX1) in patients with familial adenomatous polyposis (FAP)
Clinical and Translational Oncology (2020)
-
Mitochondrial functions and melatonin: a tour of the reproductive cancers
Cellular and Molecular Life Sciences (2019)
-
Mitochondrial genotype in vulvar carcinoma - cuckoo in the nest
Journal of Biomedical Science (2010)
-
Implications of mitochondrial DNA mutations and mitochondrial dysfunction in tumorigenesis
Cell Research (2009)
-
Association of decreased mitochondrial DNA content with ovarian cancer progression
British Journal of Cancer (2006)