Abstract
Background:
Micrometastases in bone marrow of women with early breast cancer were first identified immunocytochemically in the 1980s. We report on the original cohort of women with a median follow-up of 30 years.
Patients and Methods:
In total, 350 women with primary breast cancer had eight bone marrow aspirates examined with antibody to epithelial membrane antigen. Data on long-term mortality were obtained via record linkage to death certification.
Results:
At a 30-year median follow-up, 79 out of 89 (89%) patients with micrometastases have died compared with 202 out of 261 (77%) without (hazard ratio=1.46 (95% CI 1.12–1.90), P=0.0043). Most marked effect of micrometastases on overall survival (OS) was seen in patients aged ⩽50 at surgery (N=97, P=0.012), and on all patients within 10 years of diagnosis. In multivariable analyses, the presence of micrometastases was no longer a statistically significant prognostic factor.
Conclusions:
Bone marrow micrometastases are predictive for OS, particularly in the first decade and in younger patients.
Similar content being viewed by others
Main
The identification by our laboratory of micrometastatic disease in the bone marrow of women with early breast cancer, using immunocytochemical techniques, first generated considerable interest in 1980 (Sloane et al, 1980). Initial reports indicated that the presence of these tumour cells, in the absence of disease elsewhere, predicted for a poor outcome (Mansi et al, 1987, 1991, 1999).
Over the years, many groups have evaluated different antibodies, different techniques and examined large cohorts of patients in an attempt to further define the importance of these cells. Two meta-analyses of bone marrow micrometastases (BMM) have been reported. The first in 1998 where BMM were identified in 35% of patients and appeared to be an independent predictor of poor survival in two of the studies, but not overall (Funke and Schraut, 1998). The second meta-analysis in 2005 identified BMM in 31% of patients, and was an independent predictor for inferior overall survival (OS) (Braun et al, 2005).
Our group initially reported outcomes for this cohort of 350 patients in 1991 and subsequently in 1999 with a 6- and 12.5-year median follow-up, respectively. We now report outcomes after a median of 30 years representing the longest follow-up using this technique to analyse BMM.
Materials and methods
Patients and methods
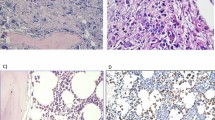
Study procedures and ethics approval have been described previously (Mansi et al, 1991). After written consent, each patient was screened for metastatic disease. At the time of surgery, ∼2 mls of bone marrow was aspirated from eight sites and was prepared and stained as described previously by using a polyclonal antibody to epithelial membrane antigen (Dearnaley et al, 1983).
Follow-up
Patients were reviewed as described previously (Mansi et al, 1991), with a 3 monthly clinical examination and blood test, a 6 monthly bone scan and annual chest X-ray for 5 years. At relapse all patients were fully staged to detect disease at other sites.
Most patients were discharged after 5-year follow-up. Details of outcome were obtained from hospital records and/or general practitioner. The mortality status of all patients within the study was flagged by the HSCIC. The causes of death were coded according to the International Classification of Diseases (versions 8–10) from the death certificates provided. No relapse data were sought after 1995.
Statistical analysis
Survival was calculated from date of surgery to death from any cause (OS) or from breast cancer-specific survival (BCSS) as written on the death certificate. Because of the lack of consistent relapse data after 1995, relapse-free survival results are not reported in this manuscript.
Kaplan–Meier curves were plotted and survival of patients with and without BMM was compared by the log-rank test. Cox PH modelling with reported hazard ratios (HRs; with 95% CIs) investigated the effect of BMM on OS and BCSS, both univariately and after adjusting for other prognostic factors (tumour size, ER status, lymph nodes, vascular invasion, adjuvant treatment and age at surgery). The effect of BMM on OS was also assessed in age-specific subgroups of ⩽50, 51–70 and >70 years. P-value <0.05 was considered statistically significant.
Proportional hazard assumptions determining whether any difference in OS or BCSS between patients with and without BMM are constant overtime was tested using Schoenfeld residuals.
Results
The cohort comprised 350 women, median age at surgery of 59 years (range 26–85). BMM were identified in 25% (89 out of 350) of patients at the time of primary surgery. The presence or absence of BMM in relation to a number of prognostic factors has been published previously (Supplementary Table 1).
Adjuvant treatment
Adjuvant therapy was given to 141 (40%) patients according to the various protocols available at that time and without knowledge of the patient’s BMM status.
Overall survival
After a median follow-up of 30 years (IQR 28·6–30·7), 281 (80%) patients are known to have died. OS was inferior in those women with BMM at the time of primary surgery: 79 out of 89 vs 202 out of 261 (HR=1.46 (95% CI 1.12–1.90), P=0.0043, Figure 1).
The most marked effect of BMM on OS was seen in patients aged ⩽50 at surgery (N=97, P=0.012) and those aged 51–70 (N=191, P=0.022), with less of a difference seen in those aged >70 (N=62, P=0.60) (Supplementary Figures 1 and 2).
In univariate analyses of OS, the following characteristics, large tumour size, ER-negative status, receipt of cytotoxic adjuvant treatment, presence of involved lymph nodes and vascular invasion at primary surgery, were all statistically significant poor prognostic factors (Table 1). After inclusion in an adjusted multivariable model, only tumour size and lymph node involvement remained statistically significant.
Breast cancer-specific survival
Breast cancer was one of the stated causes of death for 51out of 89 (57%) and 115 out of 261 (44%) of patients with and without BMM, respectively. The proportion of the total number of deaths classified as due to breast cancer decreased in later years of follow-up (Supplementary Table 2). Notably, of the 52 breast cancer deaths in patients with BMM, 44 (85%) occurred within the first 10 years after primary surgery compared with 81 out of 116 (70%) in patients who did not have BMM.
Breast cancer-specific survival was inferior in those with BMM univariately HR=1.67 (95% CI 1.20–2.32), P=0.002 (Table 2), but did not retain independent prognostic significance in multivariable analyses with this duration of follow-up.
The most marked effect of BMM on BCSS was seen in patients aged ⩽50 at surgery (P=0.029) and those aged 51–70 (P=0.029) and with less of a difference seen in those aged >70 (P=0.44).
Conclusion
Our results indicate that BMM predict for a poorer OS even after 30 years of follow-up. With longer follow-up, we have shown that this is most significant in the younger age groups and within 10 years of primary surgery. After this time, especially in older women, the test is no longer predictive for survival because women die from other conditions. That most of the impact of BMM is in the first 10 years in this study may be a consequence of the fact that the majority of women (209 out of 350) did not receive adjuvant cytotoxic chemotherapy, even in the younger age group.
Although from 1980 to 1987 our group was the sole group to describe BMM and their prognostic significance, many others have since studied this phenomenon as reflected in the meta-analysis published in 2005 (Braun et al, 2005). Results from other groups have not all consistently shown prognostic significance with BMM. We are unclear why this is the case (Salvadori et al, 1990; Courtemache et al, 1991).
In previous publications we have already discussed that our antibody to epithelial membrane antigen would not now be considered to be the best marker of tumour cells. The use of different antibodies or combinations of antibodies or different techniques such as PCR-based molecular assays has been the subject of continuing research over the past two decades (Salvadori et al, 1990; Courtemache et al, 1991; Braun et al, 2000; Becker et al, 2004; Body et al, 2006; Fehm et al, 2006).
A number of groups have looked at the comparison of BMM and circulating tumour cells in the peripheral blood using different methods for detection and, in particular, Slade et al (2009) studied the comparison as a means of providing information on early relapse by repeated sampling after primary surgery. These, and subsequent studies show that patients at high risk are more likely to show the continued presence of both BMM and circulating tumour cells during follow-up, even 12 years after diagnosis (Payne et al, 2012a). The same group of patients had circulating cell-free DNA with similar characteristics to the primary breast cancer even 12 years after diagnosis, despite there being no evidence of overt metastatic disease thus implying dormancy of such cells (Shaw et al, 2012). The concept of dormancy has been further explored by Payne et al (2012b) who showed that the presence of circulating tumour cells in the bone marrow was inversely related to circulating-free DNA in the plasma. Interestingly, Nadal et al (2012) suggested that if circulating tumour cells differ genetically from the primary tumour, this may explain the variability in response to the treatment and outcome.
With the focus now being on circulating tumour cells, recent studies in early breast cancer have shown that their presence does predict for a poorer outcome (Pierga et al, 2008; Lucci et al, 2012; Rack et al, 2014). Current guidelines for the American Society of Clinical Oncology do not recommend that the presence of circulating tumour cells be used to inform the decision-making on adjuvant therapy, although the most recent edition of the American Joint Commission on Cancer Staging Manual does include a new category of cM0(i+) to identify such women who have microscopic disease in the blood or bone marrow (American Joint Commission on Cancer Staging, 2010).
The initial detection of BMM in women with early breast cancer over three decades ago set in motion a large number of studies using a variety of techniques. Our understanding of molecular markers, methods of detection of minimal disease and the concept of dormancy has improved substantially over the years; furthermore, bone marrow aspiration has largely been superseded by detecting and characterising circulating tumour cells and circulating cell-free DNA.
Change history
02 February 2016
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
American Joint Commission on Cancer Staging (2010) AJCC Cancer Staging Manual. Springer: New York, NY.
Becker S, Becker-Pergola G, Fehm T, Wallwiener D, Solomayer EF (2004) Time is an important factor when processing samples for the detection of disseminated tumour cells in blood/bone marrow by reverse transcription-PCR. Clin Chem 50: 785–786.
Braun S, Pantel K, Müller P, Janni W, Hepp F, Kentenich CR, Gastroph S, Wischnik A, Dimpfl T, Kindermann G, Riethmüller G, Schlimok G (2000) Cytokeratin-positive cells in the bone marrow and survival of patients with stage 1,11 or 111 breast cancer. N Engl J Med 342: 525–533.
Braun S, Vogl FD, Naume B, Janni W, Osborne MP, Coombes RC, Schlimok G, Diel IJ, Gerber B, Gebauer G, Pierga JY, Marth C, Oruzio D, Wiedswang G, Solomayer EF, Kundt G, Strobl B, Fehm T, Wong GY, Bliss J, Vincent-Salomon A, Pantel K (2005) A pooled analysis of bone marrow micrometastases in breast cancer. N Engl J Med 353: 793–802.
Body JJ, Facon T, Coleman RE, Lipton A, Geurs F, Fan M, Holloway D, Peterson MC, Bekker PJ (2006) A study of the biological receptor activator of the nuclear factor-kappaB ligand inhibitor, denosumab, in patients with multiple myeloma or bone metastases from breast cancer. Clin Cancer Res 12: 1221–1228.
Coombes RC, Powles TJ, Easton D, Chilvers C, Ford HT, Smith IE, McKinna A, White H, Bradbeer J, Yarnold J, Nash A, Bettelheim R, Dowsett M, Gazet JC Investigators of the Collaborative Breast Cancer Project (1987) Adjuvant aminoglutethimide therapy for postmenopausal patients with primary breast cancer. Cancer Res 47: 2494–2497.
Courtemanche DJ, Worth AJ, Coupland RW, Rowell JL, MacFarlane JK (1991) Monoclonal antibody LICR-LON-M8 does not predict outcome in operable breast cancer. Can J Surg 47: 32–36.
Dearnaley DP, Ormerod MG, Sloane JP, Lumley H, Imrie S, Jones M, Coombes RC, Neville AM (1983) Detection of isolated mammary carcinoma cells in marrow of patients with primary breast cancer. J R Soc Med 76: 359–364.
Fehm T, Braun S, Muller V, Janni W, Gebauer G, Marth C, Schindlbeck C, Wallwiener D, Borgen E, Naume B, Pantel K, Solomayer E (2006) A concept for the standardized detection of disseminated tumour cells in bone marrow from patients with primary breast cancer and its clinical implementation. Cancer 107: 885–892.
Funke I, Schraut W (1998) Meta-analysis of studies on bone marrow micrometastases: an independent prognostic impact needs to be substantiated. J Clin Oncol 16: 557–566.
Lucci A, Hall CS, Lodhi AK, Bhattacharyya A, Anderson AE, Xiao L, Bedrosian I, Kuerer HM, Krishnamurthy S (2012) Circulating tumour cells in non-metastatic breast cancer: a prospective study. Lancet Oncol 13: 688–695.
Mansi JL, Berger U, Easton D, McDonnell T, Redding WH, Gazet JC, McKinna A, Powles TJ, Coombes RC (1987) Micrometastases in bone marrow in patients with primary breast cancer: evaluation as an early predictor of bone metastases. Br Med J (Clin Res Ed) 295: 1093–1096.
Mansi JL, Easton D, Berger U, Gazet JC, Ford HT, Dearnaley D, Coombes RC (1991) Bone marrow micrometastases in primary breast cancer: prognostic significance after 6 years follow up. Eur J Cancer 27: 1552–1555.
Mansi JL, Gogas H, Bliss JM, Gazet JC, Berger U, Coombes RC (1999) Outcome of primary breast cancer patients with micrometastases: a long-term follow up study. Lancet 354: 197–202.
Nadal R, Fernandez A, Sanchez-Rovira P, Salido M, Rodríguez M, García-Puche JL, Macià M, Corominas JM, Delgado-Rodriguez M, Gonzalez L, Albanell J, Fernández M, Solé F, Lorente JA, Serrano MJ (2012) Biomarker characterization of circulating tumour cells in breast cancer patients. Breast Cancer Res 14 (3): R71.
Payne RE, Wang F, Su N, Krell J, Zebrowski A, Yagüe E, Ma XJ, Luo Y, Coombes RC (2012a) Viable circulating tumour cell detection using multiplex RNA in situ hybridisation predicts progression-free survival in metastatic breast cancer patients. Br J Cancer 106: 1790–1797.
Payne RE, Hava NL, Page K, Blighe K, Ward B, Slade M, Brown J, Guttery DS, Zaidi SA, Stebbing J, Jacob J, Yagüe E, Shaw JA, Coombes RC (2012b) The presence of disseminated tumour cells in the bone marrow is inversely related to circulating free DNA in plasma in breast cancer dormancy. Br J Cancer 106: 375–382.
Pierga JY, Bidard FC, Mathiot C, Brain E, Delaloge S, Giachetti S, de Cremoux P, Salmon R, Vincent-Salomon A, Marty M (2008) Circulating tumor cell detection predicts early metastatic relapse after neoadjuvant chemotherapy in large operable and locally advanced breast cancer in a phase 11 randomized trial. Clin Cancer Res 14: 7004–7010.
Rack B, Schindlbeck C, Jückstock J, Andergassen U, Hepp P, Zwingers T, Friedl TW, Lorenz R, Tesch H, Fasching PA, Fehm T, Schneeweiss A, Lichtenegger W, Beckmann MW, Friese K, Pantel K, Janni W SUCCESS Study Group (2014) Circulating tumor cells predict survival in early average-to-high risk breast cancer patients. J Natl Cancer Inst 106: 1–11.
Salvadori B, Squicciarini P, Rovini D, Orefice S, Andreola S, Rilke F, Barletta L, Menard S, Colnaghi MI (1990) Use of monoclonal antibody MBri to detect micrometastases in bone marrow specimens of breast cancer patients. Eur J Cancer 26: 865–867.
Shaw JA, Page K, Blighe K, Hava N, Guttery D, Ward B, Brown J, Ruangpratheep C, Stebbing J, Payne R, Palmieri C, Cleator S, Walker RA, Coombes RC (2012) Genomic analysis of circulating cell-free DNA infers breast cancer dormancy. Genome Res 22: 220–231.
Slade MJ, Payne R, Riethdorf S, Ward B, Zaidi SA, Stebbing J, Palmieri C, Sinnett HD, Kulinskaya E, Pitfield T, McCormack RT, Pantel K, Coombes RC (2009) Comparison of bone marrow, disseminated tumour cells and blood circulating tumour cells in breast cancer patients after primary treatment. Br J Cancer 100: 160–166.
Sloane JP, Omerod MG, Neville AM (1980) Potential pathological application of immunocytochemical methods to the detection of micrometastases. Cancer Res 40: 3079–3082.
Acknowledgements
This work was supported by the Ludwig Institute of Cancer Research, who funded staff and reagents. The Institute of Cancer Research supported the statistical analysis and follow-up. ICR-CTSU receives core funding from Cancer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Mansi, J., Morden, J., Bliss, J. et al. Bone marrow micrometastases in early breast cancer–30-year outcome. Br J Cancer 114, 243–247 (2016). https://doi.org/10.1038/bjc.2015.447
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2015.447