Abstract
Despite the increasing clinical importance of germline BRCA mutation status in managing women with ovarian cancer, few patients are currently being tested. The traditional means of selecting patients for BRCA mutation testing using restrictive criteria will miss many women with a mutation. To expand access to testing and streamline the testing process, several centres in the UK have been developing new models for BRCA testing. Trials with these integrated models involving closer collaborations between genetics and oncology services are now under way. In addition to testing for BRCA mutations, there is also increasing interest in testing for other genes associated with a predisposition to ovarian cancer. Advances in next-generation sequencing technology have resulted in the development of comprehensive genetic testing panels for use in the research and diagnostic settings. Interest is also increasing in expanding testing for somatic mutations in ovarian cancer, particularly for genes such as BRCA1 and BRCA2, whereby mutations may allow more patients to benefit from targeted agents, including poly(ADP-ribose) polymerase inhibitors. In this review, the issues of who should be offered testing, how testing could be delivered, when testing should occur and the technology and costs associated with genetic testing are addressed.
Similar content being viewed by others
Main
The decisions about who should undertake testing for germline BRCA1 and BRCA2 mutations, as well as when and how it should be carried out, are becoming increasingly important for ovarian cancer patients in the UK. Over the last few years, greater public awareness of the genetic component of breast and ovarian cancer has resulted in increasing patient demand for testing. This, combined with an expanding range of clinical implications for ovarian cancer patients found to carry a BRCA1 or BRCA2 mutation, has presented a central role for genetic testing. Recent studies have suggested that approximately 15% of all ovarian cancer patients harbour a germline mutation in BRCA1 and BRCA2, few of whom are currently being offered testing (Pal et al, 2005; Walsh et al, 2011; Zhang et al, 2011; Alsop et al, 2012).
Access to genetic testing for ovarian cancer patients has traditionally been limited to those who meet specific criteria, largely for the purpose of familial cancer risk assessment. This dates back to the resource-intensive nature of older genetic testing methods, which were very time consuming and expensive to undertake. Advances in sequencing technology have led to next-generation sequencing (NGS), which offers fast, efficient, high-throughput testing at a considerably lower cost than with older methods (Bentley et al, 2008; Harismendy et al, 2009). It also means that results can consistently be provided within a clinically useful timeframe, allowing their incorporation into treatment decisions, such as choice of chemotherapy or eligibility for trials. The availability of this technology also opens up opportunities to re-evaluate traditional means of selecting patients for testing, particularly how well these criteria perform in differentiating between patients who should and should not be offered testing.
In the UK, there are no standard guidelines for testing patients with ovarian cancer for germline mutations of BRCA1/2, with practice varying by region. Guidelines do exist for patients with breast cancer, whereby the National Institute for Health and Care Excellence (NICE) recommends that all women with a 10% chance of harbouring a BRCA mutation should be offered testing, and testing should be considered down to a threshold of 5% (NICE, 2013). Following the publication of these guidelines, many regions have considered offering testing to ovarian cancer patients meeting the 10% threshold. However, the difficulty lies in deciding how to determine that threshold. A number of risk prediction models have been developed to estimate the risk of an individual, all of which require family history details on which to base risk assessments. These models, such as BOADICEA or BRCAPRO, can be cumbersome to use, particularly in a busy clinic (Fischer et al, 2013). An alternative is a validated scoring system such as the Manchester Score. These can be rapidly assessed during clinic consultations to determine if an individual meets testing thresholds (Evans et al, 2004); however, they also require multiple BRCA-related cancers to be present within the family for the threshold to be met. Use of such models or scoring systems was recommended by NICE as an acceptable way of assessing an individual’s risk of harbouring a BRCA mutation (NICE, 2013).
The selection of patients for testing has long relied on the presence of a strong family history of breast and ovarian cancer. It is now clear from a number of studies of ovarian cancer patients, unselected for family history that this criterion will result in substantial numbers of those with a BRCA mutation being missed. Møller et al (2007) tested all women presenting to their unit with ovarian cancer and reported a BRCA mutation rate of 23%. Of these, only one-third qualified for testing based on their family history. Alsop et al (2012) found that 13% of women with non-mucinous ovarian cancer in their Australian study carried a BRCA mutation, with 44% of carriers reporting no family history of BRCA-associated cancers. Similar mutation rates have been reported in women without a family history in multiple European, Canadian and American studies. These findings have led to several centres in the USA, Canada and the UK offering BRCA testing to all women with non-mucinous ovarian cancers (Metcalfe et al, 2009). This approach will detect many more women with BRCA mutations who would not have been offered testing using a selective approach.
The optimal time to test for a BRCA mutation has never been agreed. Testing of women during first-line treatment allows incorporation of mutation status into future treatment decisions without having to wait for results, which could potentially delay treatment. This is particularly relevant for areas where the time from referral to availability of results remains in excess of 6 months. However, this approach would leave a large subset of patients untested: those on long-term follow-up and those with relapsing disease who have not previously been offered testing. Such patients would need to be identified and offered testing during their routine follow-up. An alternative would be to test women only when there is an immediate difference in treatment choices. However, this approach would mean that many patients would miss out on testing, either because their disease has not relapsed or because the length of time for testing in some areas would delay treatment well beyond a clinically desirable timeframe. Long-term survivors of ovarian cancer would still benefit from testing, especially with regard to being informed of their second cancer risk and ensuring that they receive appropriate screening and advice (Domchek et al, 2013).
As the need for identifying BRCA mutations in patients with ovarian cancer is increasing, several hospitals in England have been implementing genetic testing models to allow BRCA testing to become a part of the routine clinical care of patients with ovarian cancer (Table 1).
Cambridge University Hospitals initiated the Genetic Testing in Epithelial Ovarian Cancer (GTEOC) study in July 2013, to explore the feasibility and acceptability of offering direct testing for BRCA mutations to all women who are diagnosed with ovarian cancer. The study asked all patients who were diagnosed with serous or endometrial epithelial ovarian cancer within 12 months of the initiation of the study, irrespective of their age and family history of cancer, whether they would consent to BRCA testing. Initial findings from this study showed that the population-based genetic testing approach used appeared to be acceptable to patients, and was less resource intensive than standard practice, whereby all patients have a full assessment by the genetics department prior to testing (Tischkowitz et al, 2014).
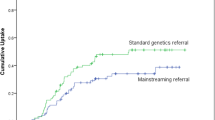
The Royal Marsden Hospital has developed an ‘oncogenetic’ testing model, implemented in July 2013, to identify BRCA mutations in patients with ovarian cancer. Oncology clinicians have been trained and certified to allow them to obtain consent from patients for testing. Patients with non-mucinous ovarian cancer or who have both ovarian cancer and another primary tumour (any age) are offered BRCA testing at their appointment with the oncologist. The patient and the oncology clinician receive the results from the genetics department, and those patients who carry a BRCA mutation then attend a genetics appointment with their results to allow detailed discussion and to have BRCA testing offered for their relatives. In addition, patients can contact or be referred to the genetics department at any time at their own request or at the discretion of their oncologist. This oncogenetic model of identifying patients with a BRCA mutation has provided a flexible, patient-centred, impartial, high-throughput approach, which has resulted in considerable time and cost savings compared with a standard genetics referral (George et al, 2014).
In November 2013, Scotland updated the Scottish Intercollegiate Guidelines Network (SIGN) guidelines on the management of epithelial ovarian cancer (SIGN 135) to include BRCA testing as standard for all patients with ovarian cancer (Scottish Intercollegiate Guidelines Network (SIGN), 2013). The guideline states that: (1) all women with non-mucinous ovarian or fallopian tube cancer should be offered BRCA1 and BRCA2 mutation testing; (2) women with ovarian cancer who have a family history of breast, ovarian or colon cancer should have a genetic risk assessment; and (3) BRCA1 and BRCA2 mutation analysis should be considered in a family where there is a 10% or greater risk of a mutation being present. The SIGN guidelines state that close collaboration between primary care and specialist cancer genetics services should be encouraged, to enable efficient genetic cancer risk assessments in individuals who are at medium or high risk.
The information provided from the small number of English hospitals and the Scottish guidelines described here demonstrates that there is currently no consensus for genetic testing of patients with ovarian cancer to identify a BRCA mutation. Even in those with clear, open criteria, it is likely that patients who do meet the criteria are not referred for genetic testing. Such under-referral of patients has been frequently reported in studies at specialist centres such as the MD Anderson Cancer Center in Texas, USA. It has also been reported in areas where genetic testing is more widely available, such as British Columbia and Ontario in Canada, where women can be referred for testing based on histology alone. Despite this, reports indicate that only 20% of eligible women are referred for testing. The uptake rate among those who are referred for testing is high, indicating that it is not patient reluctance that limits testing. This suggests that it is not only the eligibility criteria, but the entire attitude towards testing for germline mutations that needs to be considered.
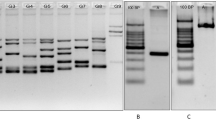
For a number of years, the ‘gold standard’ for BRCA mutation testing has involved a combination of Sanger sequencing and multiplex ligation-dependent probe amplification (MLPA). Direct Sanger sequencing allows identification of small variants (such as the deletion or insertion of single bases); whereas MLPA identifies large variants, such as the deletion or duplication of one or more exons. However, these methods are time consuming and costly, as they require the gene to be divided into small fragments, each of which is individually amplified and sequenced (Ruiz et al, 2014). More recently, high-throughput methods of NGS have been developed. These allow massive parallel sequencing of multiple genes; from multi-gene panels to whole genomes in a single run (Bentley, 2006). This technology has been rapidly adopted in research settings and is now used to perform diagnostic testing in several UK laboratories.
In addition to faster turnaround times for testing, another major potential advantage in the use of NGS is a reduction in the cost of performing BRCA testing. The standard cost of a BRCA test in the UK is currently £530 (NHS, 2014). There are several different NGS platforms available at present, all of which have slight variations in requirements and output. Each platform has variable costs per sample and costs for the sequencing equipment, but overall, the BRCA testing costs are lower using high-throughput NGS. This change results from higher levels of automation and far less laboratory technician time required to prepare and run samples. However, all platforms also require significant bioinformatic input for analysis and interpretation of the sequencing data. This has been a major limiting factor for laboratories considering moving to NGS, as few have such support available. Wider availability of cheaper testing may also increase demand for testing, increasing the need for integration between oncology and clinical genetics services.
Ovarian cancer is a genetically heterogeneous disease, with germline mutations in BRCA1, BRCA2, MLH1, MSH2, MSH6, PMS2, RAD51D, RAD51C, BRIP1 and PALB2 all associated with an inherited predisposition (Senter et al, 2008; Bonadona et al, 2011; Loveday et al, 2011; Pelttari et al, 2011; Rafnar et al, 2011; Loveday et al, 2012; Turnbull et al, 2014; Xiao et al, 2014). Mosaic mutations in the PPM1D gene have also been linked to ovarian cancer (Ruark et al, 2013). Of these, BRCA1 and BRCA2 appear to account for approximately two-thirds of germline mutations in ovarian cancer, with smaller contributions from the remaining genes (Walsh et al, 2011). This relative heterogeneity of ovarian cancer beyond BRCA1 and BRCA2 makes it ideally suited to either panel testing or exome testing, whereby comprehensive testing of multiple genes in parallel is performed. The sequential testing of multiple ovarian cancer genes is cumbersome and expensive and cannot be performed in a clinically relevant timeframe, leaving parallel sequencing the only viable alternative if all genes are to be evaluated in patients. This may soon become desirable, with genes such as RAD51D and PALB2 shown to cause similar in vivo sensitivity to poly(ADP-ribose) polymerase (PARP) inhibitors as that demonstrated in BRCA-deficient cells (Loveday et al, 2011; Turnbull et al, 2014). Interest in these genes is likely to intensify if they are found to influence response to targeted treatments and chemotherapy.
A range of multi-gene panels has been developed for use in the diagnostic or research setting, although use of these panels is not currently available within the UK National Health Service. One of the major difficulties with cancer panels to date is the reporting of mutations in cancer patients for genes in which there is no evidence of a causal link, such as MRE11A in ovarian cancer (Pennington et al, 2014). As more people with malignancies are tested for a wide variety of genes, it is increasingly likely that pathogenic mutations will be reported in genes that have previously been assessed or reported for that tumour type. It is possible that in some cases this will be found to be causally linked to the cancer, but in many cases it is likely to reflect the population frequency of such mutations. Determining which of those found are causative and how such variants should be reported will be a major challenge of the cancer panel era.
Somatic mutations in a range of different genes have been associated with each subtype of epithelial ovarian cancer. There is already interest in therapeutic exploitation of such somatic mutations, with trials investigating the role of drugs targeting BRAF, MTOR, MEK and AKT in ovarian cancer. There is also interest in identifying patients with somatic mutations in DNA repair genes such as BRCA1 and BRCA2, as they may demonstrate similar synthetic lethality to PARP inhibitors as that shown with germline mutations. Somatic mutations have been reported in DNA repair genes in approximately 9% of ovarian cancer, while BRCA1 promoter hypermethylation is reported in approximately 10% of high-grade serous and high-grade endometrioid ovarian cancer (Esteller et al, 2000; Cancer Genome Atlas Research Network, 2011; Pennington et al, 2014).
For years, the primary advantage in ovarian cancer patients undergoing genetic testing was the identification of at-risk family members, who would then choose risk-reducing interventions to modify their future risk of cancer. There are now clear differences in the behaviour, response to treatment options and prognosis of ovarian cancer between those with and without a BRCA1 or BRCA2 mutation. The emphasis should therefore be placed back on the individual with ovarian cancer to undergo testing to inform their management. Here, the integrated oncogenetic pathways have an advantage, with the oncology teams able to discuss the extent of the impact that knowledge of mutation status will have on an individual’s care when obtaining informed consent. In order to move forward to patient-centred, personalised cancer treatment in the era of targeted agents, genetic testing must now be considered an important part of the diagnostic process. In summary, it would be appropriate for all non-mucinous ovarian cancer patients to be offered BRCA mutation testing at the time of their diagnosis, to inform and enable the most appropriate treatment decisions to be made for each individual patient.
References
Alsop K, Fereday S, Meldrum C, deFazio A, Emmanuel C, George J, Dobrovic A, Birrer MJ, Webb PM, Stewart C, Friedlander M, Fox S, Bowtell D, Mitchell G ( 2012 ) BRCA mutation frequency and patterns of treatment response in BRCA mutation-positive women with ovarian cancer: a report from the Australian Ovarian Cancer Study Group . J Clin Oncol 30 : 2654 – 2663 .
Bentley DR ( 2006 ) Whole-genome re-sequencing . Curr Opin Genet Dev 16 : 545 – 552 .
Bentley DR, Balasubramanian S, Swerdlow HP, Smith GP, Milton J, Brown CG, Hall KP, Evers DJ, Barnes CL, Bignell HR, Boutell JM, Bryant J, Carter RJ, Keira Cheetham R, Cox AJ, Ellis DJ, Flatbush MR, Gormley NA, Humphray SJ, Irving LJ, Karbelashvili MS, Kirk SM, Li H, Liu X, Maisinger KS, Murray LJ, Obradovic B, Ost T, Parkinson ML, Pratt MR, Rasolonjatovo IM, Reed MT, Rigatti R, Rodighiero C, Ross MT, Sabot A, Sankar SV, Scally A, Schroth GP, Smith ME, Smith VP, Spiridou A, Torrance PE, Tzonev SS, Vermaas EH, Walter K, Wu X, Zhang L, Alam MD, Anastasi C, Aniebo IC, Bailey DM, Bancarz IR, Banerjee S, Barbour SG, Baybayan PA, Benoit VA, Benson KF, Bevis C, Black PJ, Boodhun A, Brennan JS, Bridgham JA, Brown RC, Brown AA, Buermann DH, Bundu AA, Burrows JC, Carter NP, Castillo N, Chiara E, Catenazzi M, Chang S, Neil Cooley R, Crake NR, Dada OO, Diakoumakos KD, Dominguez-Fernandez B, Earnshaw DJ, Egbujor UC, Elmore DW, Etchin SS, Ewan MR, Fedurco M, Fraser LJ, Fuentes Fajardo KV, Scott Furey W, George D, Gietzen KJ, Goddard CP, Golda GS, Granieri PA, Green DE, Gustafson DL, Hansen NF, Harnish K, Haudenschild CD, Heyer NI, Hims MM, Ho JT, Horgan AM, Hoschler K, Hurwitz S, Ivanov DV, Johnson MQ, James T, Huw Jones TA, Kang GD, Kerelska TH, Kersey AD, Khrebtukova I, Kindwall AP, Kingsbury Z, Kokko-Gonzales PI, Kumar A, Laurent MA, Lawley CT, Lee SE, Lee X, Liao AK, Loch JA, Lok M, Luo S, Mammen RM, Martin JW, McCauley PG, McNitt P, Mehta P, Moon KW, Mullens JW, Newington T, Ning Z, Ling NgB, Novo SM, O'Neill MJ, Osborne MA, Osnowski A, Ostadan O, Paraschos LL, Pickering L, Pike AC, Pike AC, Chris Pinkard D, Pliskin DP, Podhasky J, Quijano VJ, Raczy C, Rae VH, Rawlings SR, Chiva Rodriguez A, Roe PM, Rogers J, Rogert Bacigalupo MC, Romanov N, Romieu A, Roth RK, Rourke NJ, Ruediger ST, Rusman E, Sanches-Kuiper RM, Schenker MR, Seoane JM, Shaw RJ, Shiver MK, Short SW, Sizto NL, Sluis JP, Smith MA, Ernest Sohna Sohna J, Spence EJ, Stevens K, Sutton N, Szajkowski L, Tregidgo CL, Turcatti G, Vandevondele S, Verhovsky Y, Virk SM, Wakelin S, Walcott GC, Wang J, Worsley GJ, Yan J, Yau L, Zuerlein M, Rogers J, Mullikin JC, Hurles ME, McCooke NJ, West JS, Oaks FL, Lundberg PL, Klenerman D, Durbin R, Smith AJ ( 2008 ) Accurate whole human genome sequencing using reversible terminator chemistry . Nature 456 : 53 – 59 .
Bonadona V, Bonaiti B, Olschwang S, Grandjouan S, Huiart L, Longy M, Guimbaud R, Buecher B, Bignon YJ, Caron O, Colas C, Noguès C, Lejeune-Dumoulin S, Olivier-Faivre L, Polycarpe-Osaer F, Nguyen TD, Desseigne F, Saurin JC, Berthet P, Leroux D, Duffour J, Manouvrier S, Frébourg T, Sobol H, Lasset C, Bonaïti-Pellié C French Cancer Genetics Network. ( 2011 ) Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome . JAMA 305 : 2304 – 2310 .
Cancer Genome Atlas Research Network ( 2011 ) Integrated genomic analyses of ovarian carcinoma . Nature 474 : 609 – 615 .
Domchek SM, Jhaveri K, Patil S, Stopfer JE, Hudis C, Powers J, Stadler Z, Goldstein L, Kauff N, Khasraw M, Offit K, Nathanson KL, Robson M ( 2013 ) Risk of metachronous breast cancer after BRCA mutation-associated ovarian cancer . Cancer 119 : 1344 – 1348 .
Esteller M, Silva JM, Dominguez G, Bonilla F, Matias-Guiu X, Lerma E, Bussaglia E, Prat J, Harkes IC, Repasky EA, Gabrielson E, Schutte M, Baylin SB, Herman JG ( 2000 ) Promoter hypermethylation and BRCA1 inactivation in sporadic breast and ovarian tumors . J Natl Cancer Inst 92 : 564 – 569 .
Evans DG, Eccles DM, Rahman N, Young K, Bulman M, Amir E, Shenton A, Howell A, Lalloo F ( 2004 ) A new scoring system for the chances of identifying a BRCA1/2 mutation outperforms existing models including BRCAPRO . J Med Genet 41 : 474 – 480 .
Fischer C, Kuchenbacker K, Engel C, Zachariae S, Rhiem K, Meindl A, Rahner N, Dikow N, Plendl H, Debatin I, Grimm T, Gadzicki D, Flöttmann R, Horvath J, Schröck E, Stock F, Schäfer D, Schwaab I, Kartsonaki C, Mavaddat N, Schlegelberger B, Antoniou AC, Schmutzler R German Consortium for H ( 2013 ) Evaluating the performance of the breast cancer genetic risk models BOADICEA, IBIS, BRCAPRO and Claus for predicting BRCA1/2 mutation carrier probabilities: a study based on 7352 families from the German Hereditary Breast and Ovarian Cancer Consortium . J Med Genet 50 : 360 – 367 .
George A, Smith F, Cloke V, Gore ME, Hanson H, Banerjee S, Rahman N ( 2014 ) Implementation of routine BRCA gene testing of ovarian cancer (OC) patients at Royal Marsden Hospital (881PD) . Ann Oncol 25 (Suppl 4) : iv305 – iv326 .
Harismendy O, Ng PC, Strausberg RL, Wang X, Stockwell TB, Beeson KY, Schork NJ, Murray SS, Topol EJ, Levy S, Frazer KA ( 2009 ) Evaluation of next generation sequencing platforms for population targeted sequencing studies . Genome Biol 10 : R32 .
Loveday C, Turnbull C, Ramsay E, Hughes D, Ruark E, Frankum JR, Bowden G, Kalmyrzaev B, Warren-Perry M, Snape K, Adlard JW, Barwell J, Berg J, Brady AF, Brewer C, Brice G, Chapman C, Cook J, Davidson R, Donaldson A, Douglas F, Greenhalgh L, Henderson A, Izatt L, Kumar A, Lalloo F, Miedzybrodzka Z, Morrison PJ, Paterson J, Porteous M, Rogers MT, Shanley S, Walker L, Breast Cancer Susceptibility Collaboration (UK) Eccles D, Evans DG, Renwick A, Seal S, Lord CJ, Ashworth A, Reis-Filho JS, Antoniou AC, Rahman N ( 2011 ) Germline mutations in RAD51D confer susceptibility to ovarian cancer . Nat Genet 43 : 879 – 882 .
Loveday C, Turnbull C, Ruark E, Xicola RM, Ramsay E, Hughes D, Warren-Perry M, Snape K Breast Cancer Susceptibility Collaboration (UK) Eccles D, Evans DG, Gore M, Renwick A, Seal S, Antoniou AC, Rahman N ( 2012 ) Germline RAD51C mutations confer susceptibility to ovarian cancer . Nat Genet 44 : 475 – 476 .
Metcalfe KA, Fan I, McLaughlin J, Risch HA, Rosen B, Murphy J, Bradley L, Armel S, Sun P, Narod SA ( 2009 ) Uptake of clinical genetic testing for ovarian cancer in Ontario: a population-based study . Gynecol Oncol 112 : 68 – 72 .
Møller P, Hagen AI, Apold J, Maehle L, Clark N, Fiane B, Løvslett K, Hovig E, Vabø A ( 2007 ) Genetic epidemiology of BRCA mutations - family history detects less than 50% of the mutation carriers . Eur J Cancer 43 : 1713 – 1717 .
NHS ( 2014 ) Developing Testing Criteria for Familial Breast and Ovarian Cancer: Incorporating NICE Guidelines . UK Genetic Testing Network Meeting report from Chandos House, London Available from http://ukgtn.nhs.uk/fileadmin/uploads/ukgtn/Documents/Resources/Library/Reports_Guidelines/UKGTN%20breast%20cancer%20Final%20161014.pdf .
NICE ( 2013 ) Clinical Guideline CG164. Familial breast cancer: classification, care and managing breast cancer and related risks in people with a family history of breast cancer . 1 – 60, Available from http://www.nice.org.uk/guidance/cg164 .
Pal T, Permuth-Wey J, Betts JA, Krischer JP, Fiorica J, Arango H, LaPolla J, Hoffman M, Martino MA, Wakeley K, Wilbanks G, Nicosia S, Cantor A, Sutphen R ( 2005 ) BRCA1 and BRCA2 mutations account for a large proportion of ovarian carcinoma cases . Cancer 104 : 2807 – 2816 .
Pelttari LM, Heikkinen T, Thompson D, Kallioniemi A, Schleutker J, Holli K, Blomqvist C, Aittomäki K, Bützow R, Nevanlinna H ( 2011 ) RAD51C is a susceptibility gene for ovarian cancer . Hum Mol Genet 20 : 3278 – 3288 .
Pennington KP, Walsh T, Harrell MI, Lee MK, Pennil CC, Rendi MH, Thornton A, Norquist BM, Casadei S, Nord AS, Agnew KJ, Pritchard CC, Scroggins S, Garcia RL, King MC, Swisher EM ( 2014 ) Germline and somatic mutations in homologous recombination genes predict platinum response and survival in ovarian, fallopian tube, and peritoneal carcinomas . Clin Cancer Res 20 : 764 – 775 .
Rafnar T, Gudbjartsson DF, Sulem P, Jonasdottir A, Sigurdsson A, Jonasdottir A, Besenbacher S, Lundin P, Stacey SN, Gudmundsson J, Magnusson OT, le Roux L, Orlygsdottir G, Helgadottir HT, Johannsdottir H, Gylfason A, Tryggvadottir L, Jonasson JG, de Juan A, Ortega E, Ramon-Cajal JM, García-Prats MD, Mayordomo C, Panadero A, Rivera F, Aben KK, van Altena AM, Massuger LF, Aavikko M, Kujala PM, Staff S, Aaltonen LA, Olafsdottir K, Bjornsson J, Kong A, Salvarsdottir A, Saemundsson H, Olafsson K, Benediktsdottir KR, Gulcher J, Masson G, Kiemeney LA, Mayordomo JI, Thorsteinsdottir U, Stefansson K ( 2011 ) Mutations in BRIP1 confer high risk of ovarian cancer . Nat Genet 43 : 1104 – 1107 .
Ruark E, Snape K, Humburg P, Loveday C, Bajrami I, Brough R, Rodrigues DN, Renwick A, Seal S, Ramsay E, Duarte Sdel V, Rivas MA, Warren-Perry M, Zachariou A, Campion-Flora A, Hanks S, Murray A, Ansari Pour N, Douglas J, Gregory L, Rimmer A, Walker NM, Yang TP, Adlard JW, Barwell J, Berg J, Brady AF, Brewer C, Brice G, Chapman C, Cook J, Davidson R, Donaldson A, Douglas F, Eccles D, Evans DG, Greenhalgh L, Henderson A, Izatt L, Kumar A, Lalloo F, Miedzybrodzka Z, Morrison PJ, Paterson J, Porteous M, Rogers MT, Shanley S, Walker L, Gore M, Houlston R, Brown MA, Caufield MJ, Deloukas P, McCarthy MI, Todd JA Breast and Ovarian Cancer Susceptibility Collaboration; Wellcome Trust Case Control Consortium Turnbull C, Reis-Filho JS, Ashworth A, Antoniou AC, Lord CJ, Donnelly P, Rahman N ( 2013 ) Mosaic PPM1D mutations are associated with predisposition to breast and ovarian cancer . Nature 493 : 406 – 410 .
Ruiz A, Llort G, Yague C, Baena N, Viñas M, Torra M, Brunet A, Seguí MA, Saigí E, Guitart M ( 2014 ) Genetic testing in hereditary breast and ovarian cancer using massive parallel sequencing . Biomed Res Int 2014 : 542541 .
Scottish Intercollegiate Guidelines Network (SIGN) ( 2013 ) SIGN 135: Management of Epithelial Ovarian Cancer . Healthcare Improvement Scotland . Edinburgh, Available at http://www.sign.ac.uk/guidelines/fulltext/135/index.html .
Senter L, Clendenning M, Sotamaa K, Hampel H, Green J, Potter JD, Lindblom A, Lagerstedt K, Thibodeau SN, Lindor NM, Young J, Winship I, Dowty JG, White DM, Hopper JL, Baglietto L, Jenkins MA, de la Chapelle A ( 2008 ) The clinical phenotype of Lynch syndrome due to germ-line PMS2 mutations . Gastroenterology 135 : 419 – 428 .
Tischkowitz M, Drummond J, Thompson E, Sagoo G, Newcombe B, Barter E, Ridley P, Miller S, Thompson F, Webb H, Hodgkin C, Tan LT, Daly M, Ayers S, Rufford B, Parkinson C, Earl H, Duncan T, Pharoah P, Abbs S, Hulbert-Williams N, Crawford R, Brenton J, Shipman H ( 2014 ) The Genetic Testing in Epithelial Ovarian Cancer (GTEOC) study: direct access to BRCA1/2 genetic testing in oncology. 64th Annual Meeting of The American Society of Human Genetics (ASHG); 18–22 October; San Diego, CA, USA: abst 3503S .
Turnbull C, Ruark E, Seal S, Renwick A, Ramsay E, Powell S, Warren-Perry M, Hanson H, Lord C, Rahman N ( 2014 ) Implementing PALB2 gene testing in breast and ovarian cancer patients in the UK. Annual Conference of the British Society for Genetic Medicine; 22–24 September; Liverpool, UK: abst P09 .
Walsh T, Casadei S, Lee MK, Pennil CC, Nord AS, Thornton AM, Roeb W, Agnew KJ, Stray SM, Wickramanayake A, Norquist B, Pennington KP, Garcia RL, King MC, Swisher EM ( 2011 ) Mutations in 12 genes for inherited ovarian, fallopian tube, and peritoneal carcinoma identified by massively parallel sequencing . Proc Natl Acad Sci USA 108 : 18032 – 18037 .
Xiao X, Melton DW, Gourley C ( 2014 ) Mismatch repair deficiency in ovarian cancer - molecular characteristics and clinical implications . Gynecol Oncol 132 : 506 – 512 .
Zhang S, Royer R, Li S, McLaughlin JR, Rosen B, Risch HA, Fan I, Bradley L, Shaw PA, Narod SA ( 2011 ) Frequencies of BRCA1 and BRCA2 mutations among 1,342 unselected patients with invasive ovarian cancer . Gynecol Oncol 121 : 353 – 357 .
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
George, A. UK BRCA mutation testing in patients with ovarian cancer. Br J Cancer 113 (Suppl 1), S17–S21 (2015). https://doi.org/10.1038/bjc.2015.396
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2015.396
Keywords
This article is cited by
-
Delivering widespread BRCA testing and PARP inhibition to patients with ovarian cancer
Nature Reviews Clinical Oncology (2017)