Abstract
Background:
Mutations affecting RAS genes are now established predictive markers of nonresponse to anti-EGFR antibodies in advanced CRC. This analysis assessed the prognostic and predictive impact of extended RAS and PIK3CA gene mutation status in patients receiving capecitabine plus or minus bevacizumab (±mitomycin C) in the randomised phase III MAX study.
Methods:
DNA was extracted from archival macrodissected formalin-fixed paraffin-embedded tumour tissue. Mutation status was determined using pyrosequencing, confirmed with Sanger sequencing (for equivocal RAS) and correlated with efficacy outcomes. Predictive analyses were undertaken using a test for interaction involving both C vs CB+CBM.
Results:
Of the available 280 of the 471 (59.4%) patients, mutations in KRAS exons 2, 3 and 4 and NRAS 2, 3 and 4 were as follows: 32%, 2.9%, 2.2%, 1.4%, 0.7% and 0% (total RAS MT 39%). The PIK3CA MT rate was 7.5% exon 9 and 3.6% exon 20. Extended RAS gene mutation status (WT vs MT) had no prognostic impact for PFS (HR 0.91 (0.71–1.17)) or OS (HR 0.95 (0.71–1.25)). The RAS gene mutation status was not predictive of the effectiveness of bevacizumab for PFS (HR 0.56 (0.37–0.85) for RAS MT and HR 0.69 (0.5–0.97) for RAS WT; P for interaction 0.50). The PIK3CA mutation was neither predictive for bevacizumab effect nor prognostic.
Conclusion:
Of KRAS exon 2 WT patients, 10% had additional RAS mutations. Neither all RAS gene mutation status nor PIK3CA mutation status was prognostic for PFS or OS, or predictive of bevacizumab outcome in patients with advanced CRC.
Similar content being viewed by others
Main
The management of advanced colorectal cancer has improved significantly over recent years. Targeted or biological agents provide additional benefit to standard chemotherapy. The most important targets for biological agents in metastatic colorectal cancer (mCRC) are the epithelial growth factor receptor (EGFR) and the vascular endothelial growth factor-A (VEGF-A). With targeted agents there was hope that better patient selection would follow and this has been the case for anti-EGFR therapy, but it remains elusive for therapy targeting VEGF.
The KRAS gene exon 2 mutation is predictive of nonresponse to EGFR-targeted monoclonal antibody (MAb) therapy across all treatment lines, either as a single agent or in combination with irinotecan- or oxaliplatin-based chemotherapy (Amado et al, 2008; Karapetis et al, 2008; Bokemeyer et al, 2011; Van Cutsem et al, 2011). More recent evidence assessing the impact of additional RAS mutations (KRAS exons 3 and 4 and NRAS exons 1–4) has further defined the group of patients who do not respond to anti-EGFR agent. Douillard et al (2013) and Peeters et al (2014) have reported that additional RAS mutations occur in 17–18% of patients previously classified as KRAS WT and that this group also do not respond to anti-EGFR therapy. Importantly, the recently published results from the PEAK trial reported extra RAS mutations in 23% of KRAS exon 2 WT patients, highlighting the potential for significant clinical impact (Schwartzberg et al, 2014). Determination of extended RAS status is therefore now recommended in advanced CRC patients being considered for anti-EGFR-targeted therapy and current evidence suggests that patients with a mutated RAS should not receive such therapy.
Phosphatidylinositol 3-kinases (PI3K) are a family of three lipid kinases. Class 1A molecules are heterodimers of regulatory (p85) and catalytic (p110) subunits and in CRC the p110α isoform is encoded by PIK3CA and is mutated in 15–18% of patients (De Roock et al, 2011; Karapetis et al, 2014). More than 80% of these mutations occur in exon 9 or 20, with exon 9 and exon 20 making up 60–65% and 20–25%, respectively. PIK3CA mutations can co-occur with RAS mutations. Mutations of PIK3CA are thought to be potentially predictive of anti-EGFR effect, although prediction of cetuximab activity is thought to be primarily associated with exon 20 mutations (Sartore-Bianchi et al, 2009; De Roock et al, 2010). The low frequency of exon 20 mutations (3–5% in total) however makes assessment of these results difficult to interpret and the impact of PIK3CA mutations on prognosis is still uncertain (Day et al, 2013; Karapetis et al, 2014). More importantly, the question of whether PIK3CA may have some role in tumour angiogenesis and therefore anti-VEGF therapy has been postulated. In this setting, a difference based on type of mutation is also unclear (Jiang and Liu, 2009).
Bevacizumab (anti-VEGF MAb) in combination with chemotherapy (single agent or combination) is an accepted standard of care for advanced colorectal cancer (Hurwitz et al, 2005; Saltz et al, 2008; Tebbutt et al, 2010). Unlike EGFR MAbs, there remains no reliable and reproducible predictive marker to assist in patient selection. In solid tumours, VEGF and EGFR pathways have been shown to interact effecting an increase in angiogenesis (Ellis, 2004; Ciardiello et al, 2006), although we have previously reported results from the MAX trial that failed to indicate any relationship between outcomes of anti-VEGF therapy and KRAS exon 2 and BRAF mutation status (Price et al, 2011). These results confirmed a previous but smaller retrospective analysis (Ince et al, 2005). Both of these analyses were based on KRAS exon 2 mutation status alone. With additional RAS mutation rates as high as 23%, there has been renewed interest in the potential interaction between the EGFR and VEGF pathway.
This analysis was performed to explore the rate of additional RAS mutations in a first-line population randomised within a trial focussing on anti-VEGF therapy and to further assess whether a change to an extended RAS mutation population has any impact on the predictive and prognostic outcomes of extended RAS MT vs WT. In addition, we undertook an analysis of PIK3CA mutation status (exons 9 and 20 combined), exploring any interaction with progression-free survival (PFS), overall survival (OS) and response rate (RR) in patients receiving anti-VEGF therapy with bevacizumab when combined with capecitabine in the randomised phase III MAX study.
Materials and methods
Patients and study design
The MAX study design and eligibility criteria have been reported previously (Tebbutt et al, 2010). The primary objective of this phase III study was to evaluate the effect of adding bevacizumab with or without mitomycin to capecitabine on PFS among patients receiving first-line chemotherapy for their mCRC. Enrollment of patients in the original trial occurred between July 2005 and June 2007. Patients were randomly assigned to receive capecitabine (C); capecitabine and bevacizumab (CB); and capecitabine, bevacizumab and mitomycin C (CBM). All patients who participated in the MAX translational studies provided written informed consent at the time of study enrolment. Ethics approval for translational studies was obtained centrally.
Tumour collection and processing
Tissue consent and collection was performed at the time of trial commencement before this planned biomarker analysis. Formalin-fixed, paraffin-embedded samples of tumour tissue from archival specimens collected at the time of cancer diagnosis were retrieved from storage at hospital pathology departments. A histopathologist reviewed cases and if deemed to have <50% malignant crypts in the section, the tissue was macrodissected to ensure a high proportion (90%) of tumour cells. Assays of tissue samples for KRAS (exons 2, 3 and 4), NRAS (exons 2, 3 and 4) and PIK3CA (exons 9 and 20) mutations were performed by investigators who were blinded to patient outcomes. Patients were classified as mutated (MT) if a mutation was detected in any of the exons examined, or wild-type (WT) in the absence of any mutation, for RAS and PIK3CA, respectively.
Mutation analyses
Mutation analysis of RAS and PIK3CA genes was performed using genomic DNA extracted from formalin-fixed, paraffin-embedded tissue sections (QIAamp DNA FFPE Tissue Kit, Qiagen, Carlsbad, CA, USA) and pyrosequencing performed by the Perth node of the Australian Genome Research Facility (AGRF) using the PyroMark Q24 Pyrosequencing system (Qiagen). The sensitivity for this platform is 2% mutant to WT alleles; a cutoff of 10% was used to call mutations based on prior recommendations for pyrosequencing. Full details are described in Supplementary File online. Variant sequences were confirmed by Sanger sequencing using both forward and reverse primers (AGRF).
Statistical analysis
All randomly assigned patients for whom data on KRAS, NRAS and PI3K mutation status were available were included in this analysis. PFS, the primary end point, was defined as the time from randomisation until documented evidence of disease progression according to the Response Evaluation Criteria in Solid Tumours (RECIST) version 1.0, the occurrence of new disease or death from any cause. The secondary end points were OS, defined as the time from randomisation until death from any cause, and RR, defined according to RECIST version 1.0.
The PFS and OS of patients in each RAS group (MT vs WT) and treatment groups (C vs CB and CBM) were summarised using Kaplan–Meier curves, and the difference between these groups was compared using log-rank test, with the hazard ratio (HR) and its 95% confidence interval (CI) calculated from a Cox regression model with a single covariate. A Cox regression model with treatment covariate (C vs CB and CBM), RAS status and their interaction was used to assess whether RAS was predictive of bevacizumab treatment efficacy. If no significant treatment interaction was detected, multivariate proportional hazards regression model was fitted to data for all patients, with RAS status and other protocol prespecified baseline covariates in the model to assess whether RAS was an independent prognostic factor.
We calculated the odds ratio (OR) and its 95% CI using univariate and multivariate logistic regression models to compute the difference in RR for the RAS group. A logistic regression model with treatment covariate, RAS status and their interaction was used to assess whether RAS was predictive of an effect of bevacizumab on RR.
The same methodologies were adopted in assessing the predictive and prognostic values of PIK3CA.
We also compared baseline characteristics of patients with and without tumour samples available for mutational analysis. Multivariate logistic regression model was also performed to identify predictors (if any) of tumour samples available for mutational analysis.
All reported P-values were two sided and were not adjusted for multiple testing.
Results
Characteristics of the patients
Of the 471 patients who underwent randomisation, a total of 280 tumour specimens (n=95 from the C group, n=99 from the CB group and n=86 from the CBM group) were available and examined for RAS, accounting for 59.4% of the total study population (Figure 1). The median follow-up time of these patients was 30.2 months (range 0.4 to 42.4). Tumour specimens from the remaining patients could not be retrieved, were not suitable for mutational analysis or had insufficient DNA for mutational analysis to be performed for both KRAS and NRAS. The characteristics of patients with and without tissue sample available for mutational analysis were similar aside from a higher rate of primary resection and lower rate of residual local disease in the tissue available group (Supplementary Table 1 online), reflecting the amount of tissue available that will be greater in a resected primary specimen when compared with a colonoscopic or metastasis biopsy. In multivariate logistic regression of baseline characteristics, prior resection of primary tumour (OR 6.98, P<0.001) and no prior radiotherapy (OR 0.47, P<0.01) were associated with having tumour specimens available for mutational analysis.
A total of 276 tumour specimens (n=89 from the C group, n=97 from the CB group and n=90 from the CBM group) were examined for PIK3CA mutation status, accounting for 58.6% of the total study population. The baseline characteristics were balanced between treatment groups in the tissue subpopulation (Supplementary Table 1).
The RAS mutation was detected in 108 (38.9%) patients. Mutation was detected in KRAS exon 2 (n=89), KRAS exon 3 (n=8), KRAS exon 4 (n=5), NRAS exon 2 (n=4), NRAS exon 3 (n=2) but none for NRAS exon 4. One patient had mutation in both KRAS exons 2 and 4. A total of 19 patients who were KRAS exon 2 WT had other RAS mutations (10%). PIK3CA mutation was rare and detected in only 30 patients (10.8%; exon 9, n=20; exon 20, n=9; exons 9 and 20, n=1).
Among the 262 patients with tumour specimens tested and results available for KRAS, NRAS and PIK3CA mutation status, 13 (5.0%) patients had both RAS and PIK3CA mutations, 16 (6.1%) RAS WT patients had PIK3CA mutation and 80 (30.5%) PIK3CA WT patients had RAS mutation.
Baseline characteristics by mutation status are summarised in Table 1. Clinical outcomes were comparable with no significant difference in primary or secondary clinical outcomes between the total study population and the patients who were evaluated for RAS mutations (Tables 2 and 3).
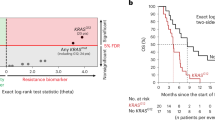
Progression-free survival
Among patients with RAS MT tumour, the median PFS was 6.2 months in the group receiving C and 8.8 months in the groups receiving CB or CBM. The HR for disease progression was 0.56 (95% CI, 0.37–0.86; P=0.007; Figure 2). Among patients with RAS WT tumour, the median PFS was 6.0 months in the group receiving C and 8.6 months in the groups receiving CB or CBM (HR 0.69; 95% CI, 0.49–0.97; P=0.03; Figure 2). The additional benefit of bevacizumab on PFS was not significantly greater among the patients with RAS WT tumours than among those with RAS MT tumours (P=0.54 for the interaction between RAS status and the assigned treatment).
For patients with PIK3CA MT tumours, the median PFS was 9.9 months in the group receiving C and 8.5 months in the groups receiving CB or CBM (HR, 1.48; 95% CI, 0.61–3.58; P=0.38; Figure 2). Among patients with PIK3CA WT tumours, the median PFS was 5.9 months in the group receiving C and 8.4 months in the groups receiving CB or CBM (HR, 0.58; 95% CI, 0.44–0.77; P<0.001; Figure 2). The additional benefit of bevacizumab on PFS appears greater among the patients with PIK3CA WT tumours than among those with PIK3CA MT tumours but does not reach statistical significance (P=0.06 for the interaction between PIK3CA status and the assigned treatment).
Overall survival
Among patients with RAS MT tumours, there was no statistical difference in OS, and the median OS was 22.8 months in the group receiving C and 20.4 months in the groups receiving CB or CBM (HR, 0.91; 95% CI, 0.58–1.44; P=0.70). Among patients with RAS WT tumours, the median OS was 20.6 months in the group receiving C and 18.9 months in the groups receiving CB or CBM (HR, 0.99; 95% CI, 0.67–1.45; P=0.95). The effect of the addition of bevacizumab on OS was not significantly greater among the patients with RAS WT tumours than among those with RAS MT tumours (P=0.73 for the interaction between RAS status and the assigned treatment).
Among patients with PIK3CA MT tumours, the median OS was 18.9 months in the group receiving C and 19.2 months in the groups receiving CB or CBM (HR, 1.18; 95% CI, 0.46–3.06; P=0.73). Among patients with PIK3CA WT tumours, the median OS was 20.6 months in the group receiving C and 19.8 months in the groups receiving CB or CBM (HR, 0.89; 95% CI, 0.65–1.22; P=0.47). The effect of the addition of bevacizumab on OS was not significantly greater among the patients with PIK3CA WT tumours than among those with PIK3CA MT tumours (P=0.49 for the interaction between PIK3CA status and the assigned treatment).
Response to treatment
The response rate based on RAS and PIK3CA mutation status is summarised in Table 4 and Supplementary Table 2 online. Patients with RAS WT tumour appeared to have a borderline greater likelihood of response with the addition of bevacizumab (P=0.04 for the interaction between RAS status and the assigned treatment). The effect of the addition of bevacizumab on response was similar among the patients with PIK3CA WT tumours compared with those with PIK3CA MT tumours (P=0.26 for the interaction between PIK3CA status and the assigned treatment).
Prognostic value of RAS and PIK3CA mutation
There was no significant difference in PFS between patients with RAS MT tumours and those with RAS WT tumours. The median PFS was 7.7 months among the patients with RAS MT tumours as compared with 7.6 months among those with RAS WT tumours (HR (RAS WT vs MT), 0.92; 95% CI, 0.71–1.17; P=0.49). Similarly, RAS has no prognostic impact on OS (Figure 3A), with median OS of 20.4 months for RAS MT tumours compared with 19.7 months for RAS WT tumours (HR (RAS WT vs MT), 0.94; 95% CI, 0.71–1.24; P=0.65). Multivariate analysis did not change these results significantly (results not shown).
There was also no significant difference in PFS and OS between patients with PIK3CA MT tumours and those with PIK3CA WT tumours. The median PFS was 8.8 months among the patients with PIK3CA MT tumours as compared with 7.5 months among those with PIK3CA WT tumours (HR (PIK3CA WT vs MT), 0.90; 95% CI, 0.60–1.35; P=0.61). The median OS was 19.2 months among patients with PIK3CA MT tumours as compared with 20.4 months among those with PIK3CA WT tumours (HR (PIK3CA WT vs MT), 1.06; 95% CI, 0.68–1.66; P=0.77; Figure 3B). Multivariate analysis did not change these results significantly (results not shown).
Sensitivity analysis
As there was higher rate of primary resection and lower rate of residual local disease in the patients who were evaluated for RAS and PIK3CA mutations as compared with those without tissue, we perform sensitivity analysis by adjusting for these baseline factors. With adjustment, RAS remained nonpredictive of benefit for bevacizumab (PFS: P=0.62, OS: P=0.95 for the interaction between RAS status and the assigned treatment). PIK3CA also remained nonpredictive of benefit for bevacizumab (PFS: P=0.06, OS: P=0.47 for the interaction between PIK3CA status and the assigned treatment).
Discussion
We have previously shown that KRAS exon 2 mutation status is not predictive of bevacizumab effect despite the proposed cross-talk between the EGFR and VEGF signalling pathways (Ellis, 2004). Given the recently reported data on the frequency and relevance of additional RAS mutations on prediction for anti-EGFR therapy, we aimed to assess the mutation rate in the MAX trial as an extension of our prior analysis (Price et al, 2011). In our population we now show that 1 in 10 patients (10%) considered KRAS WT have an additional RAS mutation. Despite these additional mutations, there was still no predictive effect on the outcome of bevacizumab, and RAS mutation status remained nonprognostic.
The MAX trial reported improved PFS with the addition of bevacizumab to capecitabine when compared with capecitabine alone. The potential impact of KRAS mutation status on outcomes with bevacizumab had been questioned and this led to a number of investigators to undertake retrospective analysis of bevacizumab trials, our group being one of them. The finding that up to 23% of KRAS exon 2 WT patients may have additional RAS mutation led us to re-analyse our data set with extended RAS results. Of the patients, 59% had available tissue for RAS assessment. Outcomes for PFS and OS were consistent between the intention-to-treat (ITT) and tissue population (Tables 2 and 3). Consistent with the primary analysis, PFS was improved by a similar magnitude and there was no apparent impact of the extended RAS status (HR, 0.56 RAS MT and 0.69 RAS WT, P for interaction between RAS status and assigned treatment=0.54). These data for extended RAS are consistent with the retrospective analyses of the MAX and the pivotal Hurwitz study (IFL±bevacizumab) for exon 2 KRAS MT (Ince et al, 2005; Hurwitz et al, 2009). In contrast to the study of Hurwitz et al (2009) where only 31.3% of patient’s tissue was assessable, our data set has 60% of the ITT population available for analysis and thus we are able to confirm that changes in RAS MT rates has not altered our prior conclusions.
We detected extended RAS mutations in 39% of the patient group with available tissue. Importantly, 10% of patients previously labelled KRAS (exon 2) WT harboured an additional RAS mutation. The proportion of exon 2 WT patients with an additional RAS mutation is less than reported in the published series with panitumumab and cetuximab (PRIME 17%, FIRE-3 16% and PEAK 23%) (Douillard et al, 2013; Heinemann et al, 2014; Schwartzberg et al, 2014). Subsequently, investigators from the CRYSTAL and OPUS studies have reported in abstract form additional RAS MT rates of 15% and 26%, respectively (Bokemeyer et al, 2014; Ciardiello et al, 2014). The difference may be explained partly as the MAX trial represented an older population considered suitable for bevacizumab and single-agent fluorouracil. Although there is no definite evidence that KRAS exon 2 MT rate may differ with age, additional mutations may vary and Russo et al (2014) recently reported different rates of NRAS MT based on age. Thus, subtle differences in these patient populations and patient characteristics may explain the lower rate of additional RAS mutations seen here. It is also likely that the method chosen to detect mutations will have differing sensitivity and recommended cutoff percentages, resulting in variation in reported rates of mutation (Whitehall et al, 2009; Pinto et al, 2011). Here, for example, we used pyrosequencing that differs with the method used by the PRIME and PEAK investigators who chose bidirectional sanger sequencing and WAVE-based surveyor kits. The investigators from the CRYSTAL and OPUS studies used the BEAMing technique. Although this is one of the most sensitive techniques reported, a 5% sensitivity cutoff was chosen for these analyses to be consistent with other literature. Variation between the technique chosen is further highlighted by the NRAS exon 4 results that appear only detectable when using BEAMing. Only the FIRE-3 investigators used pyrosequencing and their extended RAS MT rate was one of the lowest reported. Ultimately, differences in patient populations within trials and the sensitivity of the methods used will lead to a range of RAS mutations rates. The exact frequency will become clearer as additional studies are analysed and this will help define the optimal technique and sensitivity cutoff for clinical practice.
The PI3K signalling is considered to regulate tumour growth and angiogenesis by activating AKT and other targets, as well as inducing VEGF and HIF-1 expression (Jiang and Liu, 2009; Zhang et al, 2012). Furthermore, Soler et al (2013) have reported in a mouse model that inactivation of PIK3CA leads to increased vascular density, reduced vessel size and altered pericyte coverage, and thus PIK3CA has a role in regulation of vessel formation. As there is evidence for a potential interaction of PIK3CA and angiogenesis, and importantly as a biomarker for guiding antiangiogenic therapy remains elusive, we decided to explore whether there was any signal for an association between PIK3CA mutation status and outcome. In the MAX patients PIK3CA mutation was seen in 11.1% of patients (7.5% exon 9 and 3.6% exon 20). We chose to combine PIK3CA MT (exons 9 and 20) for this analysis. In contrast to prior studies assessing MT status and activity of anti-EGFR therapy (De Roock et al, 2010, 2011) where only exon 20 is relevant for predicting outcome, there is no suggestion of a similar relationship with a specific mutation when considering a potential interaction with the VEGF pathway (Zhang et al, 2012). Furthermore, the small numbers of each PIK3CA exon MT would make results difficult to interpret. Despite theoretical relationships between PIK3CA and angiogenesis and VEGF activation, we found no predictive effect. The borderline trend to a reduced effect of bevacizumab in the PIK3CA MT patients is likely because of small numbers, although ultimately larger data sets or prospective analysis will be required to asses whether this outcome is real. Furthermore, differences in response rate are also likely to be a random phenomenon based on the small sample size. That said, and although not directly comparable, patients with PIK3CA MT treated with the combination of bevacizumab, temsirolimus and liposomal doxorubicin had the opposite outcome with improved response rates when compared with those with WT PIK3CA, potentially supporting some interaction of VEGF pathway (Moroney et al, 2012), and further analysis of larger data sets may therefore be appropriate. Finally, in keeping with a number of publications, we found no indication that PIK3CA MT was prognostic. When considering whether investigators should assess PIK3CA based on individual exon or combined, evidence from Liao et al (2012) recently found that neither exon 9 nor 20 was prognostic when assessed independently, supporting a combined analysis particularly given the small numbers.
It is important to comment on the potential limitations of a subset analysis. This study is restricted to 59.4% of the tissue that was available for mutation analysis and hence not necessarily generalisable to the broader population. However, the results of our study still demonstrate good internal validity. There is no strong evidence to support that either RAS or PIK3CA is a predictive factor for bevacizumab benefit. The available tissue was obtained at the time of study enrolment and not post hoc after the primary trial result became available. Although there is an in balance between the tissue population and ITT population in terms of primary in situ, this is balanced in each analysis. Thus, although this may be prognostic, the outcomes for bevacizumab benefit are unaltered. Although there might be differences in patients’ baseline characteristics between those with and without tissue (Supplementary Table 1), such differences might exist for patients not enrolled in the MAX trial. Furthermore, sensitivity analysis performed to adjust for these different baseline characteristics does not change the overall conclusion of this study.
In conclusion, our analysis of extended RAS and PIK3CA mutation status from the MAX trial tissue population did not find any therapeutic relevance of mutation status of either RAS or PIK3CA when bevacizumab is given in combination with capecitabine chemotherapy. The RAS and PIK3CA status was not prognostic for metastatic CRC for PFS or OS. Finally, we confirm that a clinically relevant proportion of patients (10%) considered KRAS exon 2 WT have an additional mutation in the RAS pathway.
Change history
17 March 2015
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Amado RG, Wolf M, Peeters M, Van Cutsem E, Siena S, Freeman DJ, Juan T, Sikorski R, Suggs S, Radinsky R, Patterson SD, Chang DD (2008) Wild-type KRAS is required for panitumumab efficacy in patients with metastatic colorectal cancer. J Clin Oncol 26 (10): 1626–1634.
Bokemeyer C, Bondarenko I, Hartmann JT, de Braud F, Schuch G, Zubel A, Celik I, Schlichting M, Koralewski P (2011) Efficacy according to biomarker status of cetuximab plus FOLFOX-4 as first-line treatment for metastatic colorectal cancer: the OPUS study. Ann Oncol 22 (7): 1535–1546.
Bokemeyer C, Kohne C-H, Ciardiello F, Lenz H-J, Heinemann V, Klinkhardt U, Beier F, Duecker K, Tejpar S (2014) Treatment outcome according to tumor RAS mutation status in OPUS study patients with metastatic colorectal cancer (mCRC) randomized to FOLFOX4 with/without cetuximab. J Clin Oncol 32 (Suppl 5): abstr 3505.
Ciardiello F, Lenz H-J, Kohne C-H, Heinemann V, Tejpar S, Melezinek I, Beier F, Stroh C, Van Cutsem E (2014) Treatment outcome according to tumor RAS mutation status in CRYSTAL study patients with metastatic colorectal cancer (mCRC) randomized to FOLFIRI with/without cetuximab. J Clin Oncol 32 (Suppl 5): abstr 3506.
Ciardiello F, Troiani T, Bianco R, Orditura M, Morgillo F, Martinelli E, Morelli MP, Cascone T, Tortora G (2006) Interaction between the epidermal growth factor receptor (EGFR) and the vascular endothelial growth factor (VEGF) pathways: a rational approach for multi-target anticancer therapy. Ann Oncol 17 (Suppl 7): vii109–vii114.
Day FL, Jorissen RN, Lipton L, Mouradov D, Sakthianandeswaren A, Christie M, Li S, Tsui C, Tie J, Desai J, Xu ZZ, Molloy P, Whitehall V, Leggett BA, Jones IT, McLaughlin S, Ward RL, Hawkins NJ, Ruszkiewicz AR, Moore J, Busam D, Zhao Q, Strausberg RL, Gibbs P, Sieber OM (2013) PIK3CA and PTEN gene and exon mutation-specific clinicopathologic and molecular associations in colorectal cancer. Clin Cancer Res 19 (12): 3285–3296.
De Roock W, Claes B, Bernasconi D, De Schutter J, Biesmans B, Fountzilas G, Kalogeras KT, Kotoula V, Papamichael D, Laurent-Puig P, Penault-Llorca F, Rougier P, Vincenzi B, Santini D, Tonini G, Cappuzzo F, Frattini M, Molinari F, Saletti P, De Dosso S, Martini M, Bardelli A, Siena S, Sartore-Bianchi A, Tabernero J, Macarulla T, Di Fiore F, Gangloff AO, Ciardiello F, Pfeiffer P, Qvortrup C, Hansen TP, Van Cutsem E, Piessevaux H, Lambrechts D, Delorenzi M, Tejpar S (2010) Effects of KRAS, BRAF, NRAS, and PIK3CA mutations on the efficacy of cetuximab plus chemotherapy in chemotherapy-refractory metastatic colorectal cancer: a retrospective consortium analysis. Lancet Oncol 11 (8): 753–762.
De Roock W, De Vriendt V, Normanno N, Ciardiello F, Tejpar S (2011) KRAS, BRAF, PIK3CA, and PTEN mutations: implications for targeted therapies in metastatic colorectal cancer. Lancet Oncol 12 (6): 594–603.
Douillard JY, Oliner KS, Siena S, Tabernero J, Burkes R, Barugel M, Humblet Y, Bodoky G, Cunningham D, Jassem J, Rivera F, Kocakova I, Ruff P, Blasinska-Morawiec M, Smakal M, Canon JL, Rother M, Williams R, Rong A, Wiezorek J, Sidhu R, Patterson SD (2013) Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med 369 (11): 1023–1034.
Ellis LM (2004) Epidermal growth factor receptor in tumor angiogenesis. Hemat Oncol Clin North Am 18 (5): 1007–1021, viii.
Heinemann V, von Weikersthal LF, Decker T, Kiani A, Vehling-Kaiser U, Al-Batran SE, Heintges T, Lerchenmüller C, Kahl C, Seipelt G, Kullmann F, Stauch M, Scheithauer W, Hielscher J, Scholz M, Müller S, Link H, Niederle N, Rost A, Höffkes HG, Moehler M, Lindig RU, Modest DP, Rossius L, Kirchner T, Jung A, Stintzing S (2014) FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer (FIRE-3): a randomised, open-label, phase 3 trial. Lancet Oncol 15 (10): 1065–1075.
Hurwitz HI, Fehrenbacher L, Hainsworth JD, Heim W, Berlin J, Holmgren E, Hambleton J, Novotny WF, Kabbinavar F (2005) Bevacizumab in combination with fluorouracil and leucovorin: an active regimen for first-line metastatic colorectal cancer. J Clin Oncol 23 (15): 3502–3508.
Hurwitz HI, Yi J, Ince W, Novotny WF, Rosen O (2009) The clinical benefit of bevacizumab in metastatic colorectal cancer is independent of K-ras mutation status: analysis of a phase III study of bevacizumab with chemotherapy in previously untreated metastatic colorectal cancer. Oncologist 14 (1): 22–28.
Ince WL, Jubb AM, Holden SN, Holmgren EB, Tobin P, Sridhar M, Hurwitz HI, Kabbinavar F, Novotny WF, Hillan KJ, Koeppen H (2005) Association of k-ras, b-raf, and p53 status with the treatment effect of bevacizumab. J Natl Cancer Inst 97 (13): 981–989.
Jiang BH, Liu LZ (2009) PI3K/PTEN signaling in angiogenesis and tumorigenesis. Adv Cancer Res 102: 19–65.
Karapetis CS, Jonker D, Daneshmand M, Hanson JE, O’Callaghan CJ, Marginean C, Zalcberg JR, Simes J, Moore MJ, Tebbutt NC, Price TJ, Shapiro JD, Pavlakis N, Gibbs P, Van Hazel GA, Lee U, Haq R, Virk S, Tu D, Lorimer IA (2014) PIK3CA, BRAF, and PTEN status and benefit from cetuximab in the treatment of advanced colorectal cancer—results from NCIC CTG/AGITG CO.17. Clin Cancer Res 20 (3): 744–753.
Karapetis CS, Khambata-Ford S, Jonker DJ, O'Callaghan CJ, Tu D, Tebbutt NC, Simes RJ, Chalchal H, Shapiro JD, Robitaille S, Price TJ, Shepherd L, Au HJ, Langer C, Moore MJ, Zalcberg JR (2008) K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med 359 (17): 1757–1765.
Liao X, Morikawa T, Lochhead P, Imamura Y, Kuchiba A, Yamauchi M, Nosho K, Qian ZR, Nishihara R, Meyerhardt JA, Fuchs CS, Ogino S (2012) Prognostic role of PIK3CA mutation in colorectal cancer: cohort study and literature review. Clin Cancer Res 18 (8): 2257–2268.
Moroney J, Fu S, Moulder S, Falchook G, Helgason T, Levenback C, Hong D, Naing A, Wheler J, Kurzrock R (2012) Phase I study of the antiangiogenic antibody bevacizumab and the mTOR/hypoxia-inducible factor inhibitor temsirolimus combined with liposomal doxorubicin: tolerance and biological activity. Clin Cancer Res 18 (20): 5796–5805.
Peeters M, Oliner KS, Price TJ, Cervantes A, Sobrero A, Ducreux M, Hotko Y, Andre T, Chan E, Lordick F, Punt CJ, Strickland A, Wilson G, Ciuleanu T, Roman L, Van Cutsem E, Yu H, Jung A, Sidhu R, Patterson SD (2014) Updated analysis of KRAS/NRAS and BRAF mutations in study 20050181 of panitumumab (pmab) plus FOLFIRI for second-line treatment (tx) of metastatic colorectal cancer (mCRC). J Clin Oncol 32 (Suppl 5): abstr 3568.
Pinto P, Rocha P, Veiga I, Guedes J, Pinheiro M, Peixoto A, Pinto C, Fragoso M, Sanches E, Araujo A, Alves F, Coutinho C, Lopes P, Henrique R, Teixeira MR (2011) Comparison of methodologies for KRAS mutation detection in metastatic colorectal cancer. Cancer Genet 204 (8): 439–446.
Price TJ, Hardingham JE, Lee CK, Weickhardt A, Townsend AR, Wrin JW, Chua A, Shivasami A, Cummins MM, Murone C, Tebbutt NC (2011) Impact of KRAS and BRAF gene mutation status on outcomes from the phase III AGITG MAX trial of capecitabine alone or in combination with bevacizumab and mitomycin in advanced colorectal cancer. J Clin Oncol 29 (19): 2675–2682.
Russo AL, Borger DR, Szymonifka J, Ryan DP, Wo JY, Blaszkowsky LS, Kwak EL, Allen JN, Wadlow RC, Zhu AX, Murphy JE, Faris JE, Dias-Santagata D, Haigis KM, Ellisen LW, Iafrate AJ, Hong TS (2014) Mutational analysis and clinical correlation of metastatic colorectal cancer. Cancer 120 (10): 1482–1490.
Saltz LB, Clarke S, Diaz-Rubio E, Scheithauer W, Figer A, Wong R, Koski S, Lichinitser M, Yang TS, Rivera F, Couture F, Sirzen F, Cassidy J (2008) Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol 26 (12): 2013–2019.
Sartore-Bianchi A, Martini M, Molinari F, Veronese S, Nichelatti M, Artale S, Di Nicolantonio F, Saletti P, De Dosso S, Mazzucchelli L, Frattini M, Siena S, Bardelli A (2009) PIK3CA mutations in colorectal cancer are associated with clinical resistance to EGFR-targeted monoclonal antibodies. Cancer Res 69 (5): 1851–1857.
Schwartzberg LS, Rivera F, Karthaus M, Fasola G, Canon JL, Hecht JR, Yu H, Oliner KS, Go WY (2014) PEAK: a randomized, multicenter phase II study of panitumumab plus modified fluorouracil, leucovorin, and oxaliplatin (mFOLFOX6) or bevacizumab plus mFOLFOX6 in patients with previously untreated, unresectable, wild-type KRAS exon 2 metastatic colorectal cancer. J Clin Oncol 32 (21): 2240–2247.
Soler A, Serra H, Pearce W, Angulo A, Guillermet-Guibert J, Friedman LS, Vinals F, Gerhardt H, Casanovas O, Graupera M, Vanhaesebroeck B (2013) Inhibition of the p110alpha isoform of PI 3-kinase stimulates nonfunctional tumor angiogenesis. J Exp Med 210 (10): 1937–1945.
Tebbutt NC, Wilson K, Gebski VJ, Cummins MM, Zannino D, van Hazel GA, Robinson B, Broad A, Ganju V, Ackland SP, Forgeson G, Cunningham D, Saunders MP, Stockler MR, Chua Y, Zalcberg JR, Simes RJ, Price TJ (2010) Capecitabine, bevacizumab, and mitomycin in first-line treatment of metastatic colorectal cancer: results of the Australasian Gastrointestinal Trials Group Randomized Phase III MAX Study. J Clin Oncol 28 (19): 3191–3198.
Van Cutsem E, Kohne CH, Lang I, Folprecht G, Nowacki MP, Cascinu S, Shchepotin I, Maurel J, Cunningham D, Tejpar S, Schlichting M, Zubel A, Celik I, Rougier P, Ciardiello F (2011) Cetuximab plus irinotecan, fluorouracil, and leucovorin as first-line treatment for metastatic colorectal cancer: updated analysis of overall survival according to tumor KRAS and BRAF mutation status. J Clin Oncol 29 (15): 2011–2019.
Whitehall V, Tran K, Umapathy A, Grieu F, Hewitt C, Evans TJ, Ismail T, Li WQ, Collins P, Ravetto P, Leggett B, Salto-Tellez M, Soong R, Fox S, Scott RJ, Dobrovic A, Iacopetta B (2009) A multicenter blinded study to evaluate KRAS mutation testing methodologies in the clinical setting. J Mol Diagn 11 (6): 543–552.
Zhang Y, Liu X, Zhang J, Li L, Liu C (2012) The expression and clinical significance of PI3K, pAkt and VEGF in colon cancer. Oncol Lett 4 (4): 763–766.
Acknowledgements
Primary MAX trial was supported by an untied educational grant from Roche Products Pty Ltd (Australia), an additional untied educational grant from Roche Products Ltd (United Kingdom) and grants for infrastructure to the NHMRC Clinical Trials Centre from Cancer Australia and the Cancer Institute New South Wales. RAS and PIK3CA analysis was supported by a research grant from The Queen Elizabeth Hospital Haematology/Oncology Unit and an additional untied educational grant from Roche Products Pty Ltd (Australia).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
TJ Price: advisory board Roche, Merck, AMGEN; G Van Hazel: advisory board Roche; D Cunningham: research funding Roche; NC Tebbutt, advisory board Roche. The other authors declare no conflict of interest.
Additional information
Presented in part at the American Society of Clinical Oncology annual meeting, Chicago 31 May to 3 June 2014.
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
Supplementary Information accompanies this paper on British Journal of Cancer website
Supplementary information
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Price, T., Bruhn, M., Lee, C. et al. Correlation of extended RAS and PIK3CA gene mutation status with outcomes from the phase III AGITG MAX STUDY involving capecitabine alone or in combination with bevacizumab plus or minus mitomycin C in advanced colorectal cancer. Br J Cancer 112, 963–970 (2015). https://doi.org/10.1038/bjc.2015.37
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2015.37
Keywords
This article is cited by
-
Current treatment options in RAS mutant metastatic colorectal cancer patients: a meta-analysis of 14 randomized phase III trials
Journal of Cancer Research and Clinical Oncology (2020)
-
Capecitabine plus bevacizumab versus capecitabine in maintenance treatment for untreated characterised KRAS exon 2 wild-type metastatic colorectal cancer: a retrospective analysis in Chinese postmenopausal women
BMC Gastroenterology (2019)
-
Evolving Tissue and Circulating Biomarkers as Prognostic and Predictive Tools in Colorectal Cancer
Current Colorectal Cancer Reports (2018)
-
Final analysis of the randomised PEAK trial: overall survival and tumour responses during first-line treatment with mFOLFOX6 plus either panitumumab or bevacizumab in patients with metastatic colorectal carcinoma
International Journal of Colorectal Disease (2017)
-
eNOS polymorphisms as predictors of efficacy of bevacizumab-based chemotherapy in metastatic colorectal cancer: data from a randomized clinical trial
Journal of Translational Medicine (2015)