Abstract
Background:
This study was designed to evaluate the role of epidural methadone-lidocaine in cancer pain combined or not to epidural dexamethasone.
Methods:
In all, 72 cancer patients, 32- to 67-year-old were randomized to six groups (n=12) and prospectively studied to examine analgesia and adverse effects for 3 weeks. Patients received single-dose protocol epidural test drugs: Control group (CG) received epidural 40-mg lidocaine diluted to 10-ml volume with saline. Dexamethasone group (DG) 40-mg lidocaine plus 10-mg dexamethasone. The 2.5MetG 2.5-mg epidural methadone with 40-mg lidocaine; the 5MetG, 5-mg epidural methadone plus 40-mg lidocaine, the 7.5MetG, 7.5-mg epidural methadone plus 40-mg lidocaine and finally the 7.5Met-DexG, 7.5-mg methadone with 40-mg lidocaine and 10-mg dexamethasone.
Results:
Groups CG, DG and 2.5MetG were similar regarding analgesia and side effects. Patients from 5MetG and 7.5MetG took 3±1 and 5±1 days, respectively, to restart oral morphine. Patients from 7.5MetDG took 14±2 to restart oral morphine (P<0.001). Daily somnolence and appetite improved in the 7.5MetDG during 2-week evaluation (P<0.005). Fatigue improved for both DG and 7.5MetDG during 2-week evaluation (P<0.005). By the third week of evaluation, all patients were similar.
Conclusions:
Epidural methadone plus lidocaine resulted in dose-dependent analgesia, further improved by epidural dexamethasone, which also improved fatigue.
Similar content being viewed by others
Main
Spinal analgesics have been suggested as the fourth step in the World Health Organisation guidelines in the management of cancer pain for those patients who suffer from severe and refractory pain, or are incapable to bear the adverse effects from oral opioids (Christo and Mazloomdoost, 2008; Hattori et al, 2009). Although there are not sufficient clinical trials to evaluate spinal opioids in adult cancer patients (Kurita et al, 2011), morphine has been one of the cornerstones for the management of chronic intractable cancer pain. Due to the proximity to the receptor sites, the therapeutic efficacy of spinal opioid application lasts longer and also reduces systemic side effects. However, some patients unable to tolerate spinal morphine may suffer with side-effects from high doses. The opioid methadone has a broad-spectrum of suggested spinal actions: μ receptor agonist, N-methyl-D-aspartate receptor (NMDA) receptor antagonist (Sotgiu et al, 2009), glial activator (Hutchinson et al, 2010), and has been increasingly used as a second-line opioid in recent years in the management of cancer-related pain (Leppert, 2009; Anghelescu et al, 2011; Mercadante, 2012). In addition, corticosteroids were described to be commonly used in cancer pain, in spite of its limited scientific evidence (Leppert and Buss, 2012). The purpose of the present study was to examine the potential role of epidural methadone in cancer pain therapy. Its efficacy was further evaluated by the association of epidural dexamethasone.
Materials and methods
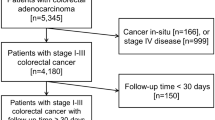
The Ethics Committee at the University of São Paulo’s Teaching Hospital, Ribeirão Preto, approved the study protocol. After written informed consent, 72 from the total of 112 patients suffering from cancer pain were selected at the Pain Clinic (∼64% inclusion). The 72 patients were randomized to one of six groups (n=12) and prospectively studied using a placebo-controlled design to examine analgesia and adverse effects and assigned to treatments using a randomized number generator in a computer programme.
The study was designed to have a power of 80% to detect a treatment difference of 1-day analgesia on a two-sided level of significance of α=0.05 assuming a standard deviation of 2 days, and a minimum number of eight patients per group. Eligible patients were aged 32–67 year-old, with a diagnosis of cancer, documented history of moderate/severe, chronic cancer pain, classified as Tumour-Node-Metastasis stage III or IV, requiring round-the-clock opioid, and capacity to understand the study protocol. Patients were excluded from the study for the following reasons: evidence of clinically unstable disease, clinically significant gastro-intestinal disease, cyclic chemotherapy within 3 weeks before screening visit or planned during the core study (shown in the past to influence bowel function); radiotherapy that would influence bowel function or pain, refusal, allergy to any of the drugs used or inability to ingest the oral rescue analgesic morphine. The concept of a visual analogue scale (VAS), which consisted of a 10-cm line with 0 equalling ‘no pain at all’ and 10 equalling ‘the worst possible pain’ was introduced. The patient brought the VAS scores and daily morphine consumption recorded each day at the weekly appointments (21-day study). However, patients were free to contact one of the authors anytime by a personal phone number, through a collect call, whenever necessary.
All patients were regularly taking oral amitriptyline 25 mg at bedtime as part of our institutional protocol, and oral morphine regimen individually adjusted to a maximal oral dose of 80–90 mg per day, in order to keep the VAS score <4/10. When patients complained of pain (VAS ≥4/10), despite the 80–90 mg daily oral morphine, they were submitted to the epidural test drugs and all patients were blind to the treatments. The day before the epidural test block was considered day-zero, and the day of the epidural block was performed was considered day-1 of the study. The groups were computer divided into six as follow: The Control group (CG) received epidural 40 mg lidocaine (1%, 20 ml ampoule with no adrenaline, Cristalia) diluted to 10-ml volume with saline. The Dexamethasone group (DG) received 40 mg lidocaine plus 10 mg dexamethasone (8 mg dexamethasone acetate +2 mg dexamethasone phosphate, Ache). The 2.5MetG received 2.5 mg epidural methadone (Methadone, 1 ml ampoule, dl-racemic mixture, 10 mg|ml, conservative-free, Cristalia) combined with 40 mg lidocaine; the 5MetG received 5 mg epidural methadone plus 40 mg lidocaine, the 7.5MetG received 7.5 mg epidural methadone plus 40 mg lidocaine and finally the 7.5Met-DG received 7.5 mg epidural methadone combined with 40 mg lidocaine and 10 mg dexamethasone. All patients received sacral block only, which was done under aseptic conditions always by the same anaesthetist that was unaware of the study drug prepared by a second anaesthetist. The drugs were diluted in a 10-ml covered syringe in order to keep the blindness of the study. The correct position of the needle as assessed by fluoroscopy and by injection of 1 ml contrast (Omnipaque, 300 mg|ml iohexol, Sanofi). All sacral blocks were performed in the morning. Patients were free to manipulate their daily oral morphine consumption, in order to keep daily pain VAS<4/10 and were followed on a weekly basis during 3 consecutive weeks. The 10 mg morphine tablets were given by the government. All patients registered once a day before bed-time (at 23-h) the VAS resembling the pain average of the day, the final daily consumption of oral morphine and the listed adverse effects. Patients assigned as ‘yes’ or ‘no’ the final impression of the side effects listed at the final of each week evaluation: (1) daily somnolence, (2) nocturnal insomnia, (3) nausea, (4) occurrence of vomiting, (5) constipation, (6) diminished appetite, (7) fatigue, (8) sadness. Complain of nausea >3 cm in a 10 cm VAS and occurrence of vomiting was treated with 8 mg sublingual ondansetron two-three times daily, if necessary. Constipation was treated with improved ingest of fibres and/or oral laxative if necessary. Patients had free access to the personal cell phone of one of the authors that was unaware of the study groups.
Statistical analysis
The normality of the distributions was assessed using the Shapiro–Wilk’s test. Groups were compared for demographic data (age, weight, and height) by one-way ANOVA. Incidence of adverse events, gender and site of primary disease were compared among groups by χ2 analysis corrected for multiple comparisons. P was considered significant if <0.008. VAS scores; and the daily morphine consumption from day-zero to day-21 were compared among groups by two-way ANOVA for repeated measures (Dexter and Chestnut, 1995). The statistical analysis compared among the six different groups on each day of the study. Tukey Honest analysis was applied to correct P values for multiple group comparisons. P<0.05 was considered significant. Data are expressed as mean±s.d., otherwise stated.
Results
Four patients from the CG, 3 from the DG, 2 from the 2.5MetG, 5Met and 7.5Met G; and finally one from the 7.5MetDG were excluded from the final analysis due to incomplete data collection. However, the minimum of eight patients per group was maintained for statistical purposes. The exclusion reasons are detailed: three patients from the CG took their own decision to take oral codeine or diclofenac during the study period combined with oral morphine, while the remaining patient did not come to the last appointment. Related to the DG group, two patients forgotten to make notes related to VAS pain scores or oral morphine consumption, and other patient included by its own oral diclofenac during the study period. Two patients from 2.5MetG and 7.5MetG and 1 from the 5MetG were also excluded due to incomplete data collection regarding oral morphine consumption and pain VAS. One patient from 5MetG did not come to the last week appointment. Finally, 1 patient from the 7.5MetDG was excluded due to ingestion of oral metamizol for pain control during the study period.
The groups showed no differences regarding gender, weight, age and height (Table 1), distribution of the primary site of the cancer pathology (Table 2) and incidence of metastasis, which varied from 60% to 73% (P>0.05; Table 2). In addition, all overall daily VAS scores were <4 cm to all groups during the study period (P>0.05, data not shown). On day-zero (day before the epidural test drugs) all patients were taking 80–90 mg oral morphine, as part of the study protocol (P>0.05). On the following days, patients were free to take oral 10 mg morphine as much as necessary in order to keep pain VAS <4|10 cm. Final VAS scores.
On day-1 (the day patients were submitted to epidural test drugs), only the CG, DG and 2.5MetG kept the daily oral consumption of 80–90 mg morphine. These three groups gradually increased daily oral morphine consumption until day-21 (150–170 mg morphine) (P>0.05). CG=DG=2.5MetG during all the 21-day evaluation regarding oral daily morphine consumption (P>0.05; Figure 1).
Daily consumption of oral morphine in the groups. CG=control group; 2.5MetG=2.5 mg methadone group; 5MetG=5 mg methadone group; 7.5MetG=7.5 mg methadone group; 7.5MetDG=7.5 mg methadone-dexamethasone group. Day-1=the CG, DG and 2.5MetG kept the daily oral consumption of 80–90 mg morphine (P>0.05). CG=DG=2.5MetG during all the 21-day evaluation regarding oral daily morphine consumption (P>0.05). Patients started the evaluation on day-1 taking 80–90 mg oral morphine, which was gradually increasing for CG, DG and 2.5MetG until day-21 (150–170 mg morphine) (daily evaluation-P>0.05) 5MetG=from day-1 to day-3, the daily intake of oral morphine was: 5MetG=7.5MetG=7.5MetDG (P>0.05) < CG=DG=2.5MetG (P<0.001). From day-4, patients started getting daily increasing oral morphine intake, which was similar to the CG, DG and to the 2.5MetG from day-7 forwards (daily evaluation-P>0.05). 7.5MetG=from day-1 to day-5, the daily intake of oral morphine was: 7.5MetG=7.5MetDG (P>0.05) <CG=DG=2.5MetG (P<0.001). From day-6, patients started getting daily increasing oral morphine intake, which was similar to the CG, DG and to the 2.5MetG from day-10 forwards (daily evaluation-P>0.05). 7.5MetDG=from day-1 to day-15, the daily intake of oral morphine was lesser when compared with the CG=DG=2.5MetG (P<0.001). On day-4, 7.5MetDG <5MetG (P<0.05). On day-6, 7.5MetDG <7.5MetG (P<0.05). From day-15, the oral intake of daily morphine was similar to all groups (P>0.05).
Related to the 5MetG, from day-1 to day-3, the daily intake of oral morphine was: 5MetG=7.5MetG=7.5MetDG (P>0.05)<CG=DG=2.5MetG (P<0.001). From day-4, patients started getting daily increasing oral morphine intake, which was similar to the CG, DG and to the 2.5MetG from day-7 forwards (daily evaluation-P>0.05; Figure 1). The evaluation of the 7.5MetG revealed that from day-1 to day-5, the daily intake of oral morphine was: 7.5MetG=7.5MetDG (P>0.05)<CG=DG=2.5MetG (P<0.001). From day-6, patients started getting daily increasing oral morphine intake, which was similar to the CG, DG and to the 2.5MetG from day-10 forwards (daily evaluation-P>0.05; Figure 1). Related to the 7.5MetDG, from day-1 to day-15, the daily intake of oral morphine was lesser when compared with the CG=DG=2.5MetG (P<0.001). On day-4, 7.5MetDG<5MetG (P<0.05). On day-6, 7.5MetDG<7.5MetG (P<0.05). From day-15, the oral intake of daily morphine was similar to all groups (P>0.05).
The incidence of adverse effects is described in Table 3. The complaints of gastric upsetting, constipation, sadness and nocturnal insomnia were similar among groups at day-7, -14 and -21 evaluations (P>0.05). Related to all adverse effects questioned, daily somnolence and appetite improved in the 7.5MetDG during at day-7 and -14 evaluations (P<0.005). Fatigue improved for both DG and 7.5MetDG during at day-7 and -14 (P<0.005). However, all side effects were similar at the third week evaluation (P>0.05). No other adverse effects rather than the questioned were spontaneously described by the patients.
Discussion
In the present study, patients suffering from cancer pain treated chronically with oral morphine at round clock and amitriptyline before bedtime showed a dose-dependent analgesia after a single dose of 2.5, 5 and 7.5 mg epidural methadone, which was further increased by the addition of epidural dexamethasone. Previously, doses varying from daily epidural 12–32 mg methadone were formerly described to result in pain control in 80% of cancer patients suffering from visceral or somatic pain, with an average of 27-daily infusion and no serious side-effects (Shir et al, 1991). We used a single bolus of epidural racemic methadone for treating cancer pain, as the purpose of the study. Methadone was demonstrated to act primarily as agonist of μ-opioid receptor, and its d isomer has also NMDA receptor antagonist activity (Inturrisi, 2005). It has high lipid solubility that could facilitate its entrance from the epidural space into the spine, although a peripheral action has also been described (He et al, 2010). Nevertheless, epidural methadone has an intrinsic spinal effect regardless of whether or not there is extra-spinal action arising from systemic absorption (Parramon et al, 2003).
Epidural methadone combined (Prieto-Alvarez et al, 2002; Pérez et al, 2010) or not (Parramon et al, 2003) to local anaesthetic has been described before as analgesic for acute pain in patients and horses (Olbrich and Mosing, 2003). Different combinations have been used in the actual multimodal cancer pain study. Clinically used Na+ channel blockers such as lidocaine, at doses which do not block conduction can relieve spinal sensitization and facilitator processes in dorsal horn neurons via blockade of Na+ and K+ channels (Olschewski et al, 2009), can directly modulate NMDA-receptor in the superficial dorsal horn, can inhibit persistent Na+ current in injured dorsal root ganglion neurons (Dong et al, 2008), and additionally may have a general glycine-like action of lidocaine or some of its metabolites on inhibitory strychnine-sensitive receptors and on strychnine-insensitive glycine receptors (Muth-Selbach et al, 2009; Furutani et al, 2010). Other inherent action of lidocaine would be the phosphorylation attenuation of p38 mitogen-activated protein kinase in the activated microglia of spinal cord, reversing established tactile allodynia in chronic constriction injury model of rats (Gu et al, 2008). In our study, the association of low-dose lidocaine and escalating doses of epidural methadone was evaluated. The results demonstrated that neither the epidural dose of 40 mg lidocaine alone nor combined with 2.5 mg methadone were effective for improving cancer pain. Lidocaine has been previously demonstrated to produce analgesia for somatic and visceral pain at the spinal level, which was synergistic with a non-NMDA glutamate receptor antagonist in rats (Imamashi et al, 1999). Isobolographic analysis also revealed that the epidural opioid morphine and lidocaine interacted synergistically in both somatic and visceral nociception tests, and naloxone antagonised the antinociceptive effects produced by the combination (Kaneko et al, 1994). Whether local anaesthetics would act as anti-inflammatory and in micro-molar concentrations would inhibit extracellular oxygen release in spinal microglia; as described elsewhere for neutrophil priming and activation (Ploppa et al, 2010), is unknown.
A different combination of drugs was the DG, which patients received both epidural dexamethasone and lidocaine. Dexamethasone profits may be secondary to glucocorticoid receptor activation, in turn rapidly suppressing basal and stress-induced hypothalamus–pituitary–adrenal activity partly through a central mechanism of action (Andrews et al, 2012). At the level of the paraventricular nucleous, dexamethasone rapidly reduced hypothalamus–pituitary–adrenal axis activation in a non-genomic, membrane-associated manner, involving cannabinoid receptor type 1 signalling (Evanson et al, 2010). Apart, corticosteroid was demonstrated to effectively reduce myelin changes accompanying brain oedema (Kozler et al, 2011) that would benefit patients suffering from oedema secondary to spinal metastasis or to hidroeletrolytic disturbances. In addition, high levels of glucocorticoid receptor and mineralocorticoid receptor are colocalized in the substantia gelatinosa where pain pathways appear to be under a strong regulation of these receptors, and nociception was attenuated by spinal dexamethasone (Gu et al, 2011). Other possible speculated mechanism of action for the epidural dexamethasone could be the attenuation of the ciclooxigenase-2-dependent production of prostanoids, mainly vasoactive prostaglandin-E(2) (Font-Nieves et al, 2012) from the astrocytes that surround the synapse between the first- and second-order neuron in the spinal cord. Apart from spinal mechanism of action, dexamethasone could also decrease astrocyte-to-neuron communication in the hypothalamus through inhibition of production of the gliotransmitter prostaglandin-E(2) (Clasadonte et al, 2011). Dexamethasone also prevented lidocaine-induced neurotoxicity in tumour cells through prevention of mitochondrial potential decline and also increased levels of threonine-serine protein kinase B phosphorylation (Ma et al, 2010). Finally, the final combination evaluated in this clinical setting was epidural lidocaine plus methadone plus the glucocorticoid dexamethasone. Co-administration of dexamethasone and glutamate receptor antagonists (such as spinal methadone and lidocaine) for treating nociception have been previously described in rats in the periphery (Lam and Ng, 2012) and centrally (Bertorelli et al, 1998). In accordance, our results revealed around 14 days of pain relief from a single bolus dose of the combination of the three drugs.
Additional benefits in patients who received epidural dexamethasone included decreased incidence of daily somnolence, decrease fatigue and appetite improvement after both dexamethasone and 7.5 mg methadone during the first 14 days evaluation, while only fatigue improved for DG at day-7 and -14. Probably somnolence and appetite improvement were not enriched in this group due to the higher oral daily dose of morphine consumption they displayed. The gradual increase in morphine consumption to all groups after day-15 was probably reflection of the particularity of the study population (high incidence of metastasis) and of the study drug protocol, where only morphine was allowed as rescue analgesic. Another point to be considered is that cancer patients suffer from stress of the disease knowledge, anxiety and pain that may result in dysfunction of glutamatergic neurotransmission, including effects on glutamate release, glutamate receptors and glutamate clearance and metabolism (Popoli et al, 2011). A positive effect of the combination of lidocaine, methadone and dexamethasone in this population could be at least partly due to their neuroprotective effect on the dorsal root ganglion and Schawnn cells (Zhu and Glaser, 2008; Ma et al, 2010), as antagonists of NMDA receptor combined with dexamethasone have been described to reduce the production of tumour necrosis factor level in the brain.
In summary, dexamethasone would enhance methadone analgesia partly through: (1) overwhelming the hypothalamus–pituitary–adrenal activity (Andrews et al, 2012), that would be further enhanced by ciclooxigenase-2 attenuation at astrocytes in the hypothalamus (Clasadonte et al, 2011); (2) inhibition of glutamate release at the dorsal raphe serotonergic 5-HT neurons (Evanson et al, 2010; Wang et al, 2012); and (3) ciclooxigenase-2 attenuation (Font-Nievis et al, 2012) from the astrocytes at the spine (Clasadonte et al, 2011). In addition, because mental fatigue is related to activation of NMDA receptors (Morimoto et al, 2012), it would be improved by NMDA antagonist such as methadone. Another detail that deserves attention is that cannabinoids have been described to improve fatigue in cancer patients (Johnson et al, 2012) and dexamethasone is known to bind at glucocorticoid receptors, activate G-protein coupled receptors and be signalled by endocannabinoid messengers (Morimoto et al, 2012) and could therefore diminish fatigue by acting indirectly as adjuvant cannabinoid.
Other adverse effects described in the literature, however, not mentioned by our population was pruritus and urinary retention. The incidence of pruritus after epidural methadone was significantly slighter compared with morphine. Epidural morphine was also associated with a significantly greater incidence of urinary retention than methadone (Gedney and Liu, 1998).
In conclusion, epidural 2.5–7.5 mg methadone combined to low-dose lidocaine (40 mg) resulted in dose-dependent analgesia in cancer pain patients. This analgesic effect was further enhanced by 10 mg epidural dexamethasone, associated with improvement of fatigue, daily somnolence and appetite.
Change history
05 February 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Andrews MH, Wood SA, Windle RJ, Lightman SL, Ingram CD (2012) Acute glucocorticoid administration rapidly suppresses basal and stress-induced hypothalamus-pituitary-adrenal axis activity. Endocrinology 153: 200–211
Anghelescu DL, Faughnan LG, Hankins GM, Ward DA, Oakes LL (2011) Methadone use in children and young adults at a cancer center: a retrospective study. J Opioid Manag 7: 353–361
Bertorelli R, Adami M, Di Santo E, Ghezzi P (1998) MK 801 and dexamethasone reduce both tumor necrosis factor levels and infarct volume after focal cerebral ischemia in the rat brain. Neurosci Lett 246: 41–44
Christo PJ, Mazloomdoost D (2008) Interventional pain treatments for cancer pain. Ann NY Acad Sci 1138: 299–328
Clasadonte J, Poulain P, Hanchate NK, Corfas G, Ojeda SR, Prevot V (2011) Prostaglandin E2 release from astrocytes triggers gonadotropin-releasing hormone (GnRH) neuron firing via EP2 receptor activation. Proc Natl Acad Sci USA 108: 16104–16109
Dexter F, Chestnut DH (1995) Analysis of statistical tests to compare visual analog scale measurements among groups. Anesthesiology 82: 896–902
Dong H, Fan YH, Wang YY, Wang WT, Hu SJ (2008) Lidocaine suppresses subthreshold oscillations by inhibiting persistent Na(+) current in injured dorsal root ganglion neurons. Physiol Res 57: 639–645
Evanson NK, Tasker JG, Hill MN, Hillard CJ, Herman JP (2010) Fast feedback inhibition of the HPA axis by glucocorticoids Is mediated by endocannabinoid signaling. Endocrinology 151: 4811–4819
Font-Nieves M, Sans-Fons MG, Gorina R, Bonfill-Teixidor E, Salas-Pérdomo A, Márquez-Kisinousky L, Santalucia T, Planas AM (2012) Induction of COX-2 enzyme and down-regulation of COX-1 expression by lipopolysaccharide (LPS) control prostaglandin E2 production in astrocytes. J Biol Chem 287: 6454–6468
Furutani K, Ikoma M, Ishii H, Baba H, Kohno T (2010) Bupivacaine inhibits glutamatergic transmission in spinal dorsal horn neurons. Anesthesiology 112: 138–143
Gedney JA, Liu EH (1998) Side-effects of epidural infusions of opioid bupivacaine mixtures. Anaesthesia 53: 1148–1155
Gu X, Peng L, Yang D, Ma Q, Zheng Y, Liu C, Zhu B, Song L, Sun X, Ma Z (2011) The respective and interaction effects of spinal GRs and MRs on radicular pain induced by chronic compression of the dorsal root ganglion in the rat. Brain Res 1396: 88–95
Gu YW, Su DS, Tian J, Wang XR (2008) Attenuating phosphorylation of p38 MAPK in the activated microglia: a new mechanism for intrathecal lidocaine reversing tactile allodynia following chronic constriction injury in rats. Neurosci Lett 431: 129–134
Hattori S, Sano H, Tanaka K, Yokota M (2009) Intrathecal morphine treatment in advanced cancer pain patients. Masui 58: 1384–1392
He L, Kim J, Ou C, McFadden W, van Rijn RM, Whistler JL (2010) Methadone antinociception is dependent on peripheral opioid receptors. J Pain 10: 369–379
Hutchinson MR, Lewis SS, Coats BD, Rezvani N, Zhang Y, Wieseler JL, Somogyi AA, Yin H, Maier SF, Rice KC, Watkins LR (2010) Possible involvement of toll-like receptor 4/myeloid differentiation factor-2 activity of opioid inactive isomers causes spinal proinflammation and related behavioral consequences. Neuroscience 167: 880–893
Imamachi N, Saito Y, Hara K, Sakura S, Kosaka Y (1999) The non-NMDA glutamate receptor antagonist CNQX augments lidocaine antinociception through a spinal action in rats. Anesth Analg 89: 416–421
Inturrisi CE (2005) Pharmacology of methadone and its isomers. Minerva Anestesiol 71: 435–437
Johnson JR, Lossignol D, Burnell-Nugent M, Fallon MT (2012) An open-label extension study to investigate the long-term safety and tolerability of THC/CBD oromucosal spray and oromucosal THC spray in patients with terminal cancer-related pain refractory to strong opioid analgesics. J Pain Symptom Manage S0885-3924 (12): 00439–3
Kaneko M, Saito Y, Kirihara Y, Collins JG, Kosaka Y (1994) Synergistic antinociceptive interaction after epidural coadministration of morphine and lidocaine in rats. Anesthesiology 80: 137–150
Kozler P, Riljak V, Pokorný J (2011) Methylprednisolone reduces axonal impairment in the experimental model of brain oedema. Neuro Endocrinol Lett 32: 831–835
Kurita GP, Kaasa S, Sjøgren P European Palliative Care Research Collaborative (EPCRC) (2011) Spinal opioids in adult patients with cancer pain: a systematic review: a European Palliative Care Research Collaborative (EPCRC) opioid guidelines project. Palliat Med 25: 560–577
Lam FF, Ng ES (2012) Substance P and glutamate receptor antagonists improve the anti-arthritic actions of dexamethasone in rats. Br J Pharmacol 159: 958–969
Leppert W (2009) The role of methadone in cancer pain treatment–a review. Int J Clin Pract 63: 1095–1109
Leppert W, Buss T (2012) The role of corticosteroids in the treatment of pain in cancer patients. Curr Pain Headache Rep 16: 307–313
Ma R, Wang X, Lu C, Li C, Cheng Y, Ding G, Liu L, Ding Z (2010) Dexamethasone attenuated bupivacaine-induced neuron injury in vitro through a threonine-serine protein kinase B-dependent mechanism. Neuroscience 167: 329–342
Mercadante S (2012) Switching methadone: a 10-year experience of 345 patients in an acute palliative care unit. Pain Med 13: 399–404
Morimoto Y, Zhang Q, Adachi K (2012) Effects of memantine, an N-methyl-D-aspartate receptor antagonist, on fatigue and neuronal brain damage in a rat model of combined (physical and mental) fatigue. Biol Pharm Bull 35: 481–486
Muth-Selbach U, Hermanns H, Stegmann JU, Kollosche K, Freynhagen R, Bauer I, Lipfert P (2009) Antinociceptive effects of systemic lidocaine: involvement of the spinal glycinergic system. Eur J Pharmacol 613: 68–73
Olbrich VH, Mosing M (2003) A comparison of the analgesic effects of caudal epidural methadone and lidocaine in the horse. Vet Anaesth Analg 30: 156–164
Olschewski A, Schnoebel-Ehehalt R, Li Y, Tang B, Bräu ME, Wolff M (2009) Mexiletine and lidocaine suppress the excitability of dorsal horn neurons. Anesth Analg 109: 258–264
Parramon F, García Ch, Gambús P, Vilaplana J, Aragonés N, Villalonga A (2003) Postoperative patient-controlled analgesia is more effective with epidural methadone than with intravenous methadone in thoracic surgery. Rev Esp Anestesiol Reanim 50: 326–331
Ploppa A, Kiefer RT, Haverstick DM, Groves DS, Unertl KE, Durieux ME (2010) Local anesthetic effects on human neutrophil priming and activation. Reg Anesth Pain Med 35: 45–50
Popoli M, Yan Z, McEwen BS, Sanacora G (2011) The stressed synapse: the impact of stress and glucocorticoids on glutamate transmission. Nat Rev Neurosci 13: 22–37
Prieto-Alvarez P, Tello-Galindo I, Cuenca-Peña J, Rull-Bartomeu M, Gomar-Sancho C (2002) Continuous epidural infusion of racemic methadone results in effective postoperative analgesia and low plasma concentrations. Can J Anaesth 49: 25–31
Pérez J, de Santos P, Plaza A, Mercadal J (2010) Adjuvant methadone or fentanyl in spinal anesthesia with bupivacaine: a randomized, double-blind, placebo-controlled trial. Rev Esp Anestesiol Reanim 57: 546–552
Shir Y, Shapira SS, Shenkman Z, Kaufman B, Magora F (1991) Continuous epidural methadone treatment for cancer pain. Clin J Pain 7: 339–341
Sotgiu ML, Valente M, Storchi R, Caramenti G, Biella GE Cooperative (2009) N-methyl-D-aspartate (NMDA) receptor antagonism and mu-opioid receptor agonism mediate the methadone inhibition of the spinal neuron pain-related hyperactivity in a rat model of neuropathic pain. Pharmacol Res 60: 284–290
Wang J, Shen RY, Haj-Dahmane S (2012) Endocannabinoids mediate the glucocorticoid-induced inhibition of excitatory synaptic transmission to dorsal raphe serotonin neurons. J Physiol 590 (Pt 22): 5795–808
Zhu TS, Glaser M (2008) Neuroprotection and enhancement of remyelination by estradiol and dexamethasone in cocultures of rat DRG neurons and Schwann cells. Brain Res 1206: 20–32
Acknowledgements
We thank Cristalia for the donation of conservative-free racemic Methadone ampoules. The cost of the study was supported by the Center for Pain management-HC-FMRP-USP.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Lauretti, G., Rizzo, C., Mattos, A. et al. Epidural methadone results in dose-dependent analgesia in cancer pain, further enhanced by epidural dexamethasone. Br J Cancer 108, 259–264 (2013). https://doi.org/10.1038/bjc.2012.593
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.593
Keywords
This article is cited by
-
Pharmacological options for the management of refractory cancer pain—what is the evidence?
Supportive Care in Cancer (2015)



