Abstract
Background:
Patients with prostate cancer tend to die from bone metastases. Until now, no evidence has shown that Paget’s disease of bone (PDB) affects the progression of bone metastasis or overall survival of patients with prostate cancer.
Methods:
We searched our patient database for men who had presented with prostate cancer and PDB between June 1993 and March 2009, and identified best-matched control patients according to stage, grade, age, date of diagnosis, treatment, and race.
Results:
Among 1346 consecutive patients with prostate cancer diagnosed before 2008, 15 were confirmed to have comorbid PDB. Twenty-six more were identified from the institutional billing search. Including the 41 best-matched controls, our total study population was 82 patients. In the Kaplan–Meier analysis, we estimated median times from diagnosis of prostate cancer to bone metastasis to be 21.5 years for those with PDB and 9.4 years for those without PDB (P=0.044). Median overall survival times were 11.8 and 9.2 years for the two groups, respectively (P=0.008).
Conclusion:
For the first time, we have obtained evidence that patients with prostate cancer and PDB have delayed time to bone metastases and improved overall survival than do patients with prostate cancer alone.
Similar content being viewed by others
Main
Prostate cancer displays an uncanny ability to metastasise to the bone. More than 80% of patients who are not cured of their prostate cancer will develop clinical osseous metastases. In a majority of these patients, metastasis is confined to or predominantly involves the skeleton (Tu and Lin, 2008; Tu et al, 2010).
Bone metastasis may be the single most important prognostic factor for patients with prostate cancer, because the metastases tend to cause debilitating symptoms such as pain, fractures, and nerve impingement, which compromise patients’ performance and quality of life. In general, the amount of bone metastasis and the time to its development determine a patient’s clinical outcome. Thus, in patients with widespread prostate cancer that rapidly progresses to bone metastasis, it tends to have a fulminant clinical course, whereas prostate cancers with delayed, minimal, or stable bone metastasis tend to have a more indolent course.
A hallmark of prostate cancer bone metastasis is that it is overwhelmingly osteoblastic. Not only is there a special affinity of prostate cancer for the bone, there is also a unique interaction between prostate cancer cells and osteoblasts. An improved understanding of the bone microenvironment and how it affects this interaction may help us elucidate the complex biology of prostate cancer and devise improved strategies for its treatment.
Paget’s disease of bone (PDB), also known as osteitis deformans or osteodystrophia deformans, is the second most frequent metabolic bone disorder after osteoporosis, affecting individuals older than 55 years. The prevalence of PDB in men of European ancestry and older than 55 years is 2.5% (Cooper et al, 1999). The aetiology of PDB may be related to genetic or viral causes, among others. Paget’s disease of bone is a chronic disorder in which excessive breakdown and formation of affected bones result in enlarged and misshapen bones. The increased bone turnover seen in PDB is initiated by activated osteoclasts, which cause enhanced osteolysis, followed by recruitment of osteoblasts, which provide compensatory but irregular bone formation.
Until now, to our knowledge, a relationship between PDB and prostate cancer has not been investigated. It is interesting that although both prostate cancer and PDB are relatively common in elderly men, it is uncommon to find men with both diseases. Our clinical observation of those rare cases, however, suggests that prostate cancer patients with comorbid PDB have a decreased incidence of osteoblastic metastases. They tend to experience a more indolent clinical course, with a delay in the development of progressive, symptomatic bone metastases. If this observation is proven to be true, it would suggest that modification of the bone microenvironment caused by PDB results in the delayed progression of prostate cancer to bone metastasis.
In this retrospective matched-control study, we examined the possible influence of PDB on the progression of prostate cancer in bone by comparing the survival time of men with prostate cancer with and without PDB.
Patients and methods
Patient population
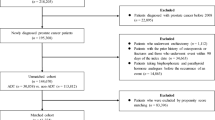
This study (DR11-0194) was approved by the institutional review board of The University of Texas MD Anderson Cancer Center. We identified 1346 consecutive patients who had been evaluated by one medical oncologist (S-MT) either as a new patient or one seen for a consultation in the Genitourinary Medical Oncology clinic at the MD Anderson Cancer Center during the period from 1 June 1993, through 31 March 2009. Among those patients diagnosed before January 2008, 15 were confirmed to have comorbid PDB. By searching our institutional billing data for ‘osteitis deformans’ using ICD code 731.0, we identified an additional 26 patients with prostate cancer and PDB, who had been evaluated during the same period but by different oncologists. Thus, our total population in the Paget’s group was 41.
Study design
From the same patient database, 41 patients were identified as controls (i.e., non-Paget’s group). They were matched to the study patients according to the following criteria at the time of diagnosis, in descending order of priority: (1) stages: staging was more accurate in surgical cases; therefore, the patients were matched according to prostatectomy or radiation therapy. For stage D0, we took into account the prostate-specific antigen (PSA) concentration and local therapy. For stage D1, we distinguished between radiographic and microscopic (after lymph node dissection) disease. For stage D2, we determined the burden of bone metastases, that is, <6 vs ⩾6 lesions on bone scanning; (2) grades: Gleason score; (3) age; (4) date of diagnosis.
Both patients and controls were excluded from the study if they were also known to have any of the following:
-
1)
A life-threatening secondary malignancy (e.g., haematological malignancy, such as leukaemia or lymphoma; gastrointestinal malignancy, such as colorectal, gastric, or pancreatic cancer; lung cancer; melanoma; metastatic renal cell carcinoma; invasive urothelial carcinoma) that could affect their life expectancy. Exceptions to this exclusion criterion were diagnoses of superficial transitional cell carcinoma of the bladder, non-melanomatous skin cancers, stable or indolent cancers like thyroid carcinoma, localised renal cell carcinoma, or cancers of any kind that had not recurred for >5 years after treatment.
-
2)
Small cell carcinoma or sarcoma of the prostate.
-
3)
Congestive heart failure with a left ventricular ejection fraction <40%.
-
4)
Inadequate medical records. This criterion pertained to international patients, for whom follow-ups were often limited for various reasons.
To be included, patients with PDB had to have radiographically confirmed disease. We documented the date of diagnosis of prostate cancer as the date of the pathology report, and the date of diagnosis of prostate cancer bone metastasis as the date of the radiology report. If only the year was available, we used 1 January, and if only the year and month were available, we used 1 for the day of the month. We then calculated both the age-adjusted and age-unadjusted Charlson comorbidity scores (Charlson et al, 1987) for the patients around the time of their initial diagnosis or treatment, or during their first evaluation at the MD Anderson Cancer Center. To determine the exact date of death, we used the scanned documents in our ClinicStation database or the Social Security Death Index (http://ssdi.rootsweb.ancestry.com/).
The time to bone metastasis and overall survival time were defined as the times from the date of diagnosis of prostate cancer to the dates of bone metastasis and death. If the patient had no bone metastasis or was still alive, we used the current date.
Statistical analyses
We calculated the differences between the Paget’s and non-Paget’s groups by using χ2-test, paired t-test, and the Wilcoxon rank-sum test. We also performed the log-rank test, Kaplan–Meier analysis, and Fine–Gray competing risk analysis to determine the differences in time to development of bone metastasis and time to death between the two groups. Risk factors (e.g., age, race, Gleason grade, stage at the time of diagnosis, PDB, Charlson score, and bisphosphonate use) were analysed using multivariate Cox regression analysis. Fine–Gray competing risk analysis was performed using the R statistical package (Version 2.13.0, The R Foundation for Statistical Computing), and all other statistical analyses were performed using SPSS version 17.0 (SPSS, Cary, NC, USA) and SigmaPlot version 11.0 (Systat, Chicago, IL, USA) software with two-sided tests, with a P-value of ⩽0.05 considered statistically significant.
Results
The patients’ baseline characteristics are shown in Table 1. The Paget’s and non-Paget’s groups were well matched for age, disease stage, and Gleason score. The baseline Charlson comorbidity scores (adjusted and unadjusted for age) were not statistically significantly different between the two groups. There were more Black patients in the Paget’s group (P=0.096, χ2-test). The baseline PSA concentration was slightly higher in the non-Paget’s group, although that difference was not statistically significant (P=0.25, Wilcoxon rank-sum test). Similar numbers from both groups had undergone definitive local therapies, that is, surgery, radiation, or brachytherapy. More patients in the non-Paget’s control group had received chemotherapy (data not shown), reflecting the fact that their prostate cancer had tended to progress and they required more aggressive therapy to control it and/or to palliate their symptoms.
Six patients were excluded from the pool of PDB for analysis, because they had developed osteosarcoma (n=1), lung cancer (n=1), lymphoma (n=2), renal cell carcinoma (n=1), or pancreatic cancer (n=1). The following patients were excluded from the pool of matched controls for the following comorbidities that were active at the time of evaluation and could have influenced patients’ overall survival: small cell carcinoma (n=10), sarcoma (n=2), leukaemia or lymphoma (n=15), lung or head and neck cancers (n=18), gastrointestinal malignancies (n=18), melanoma or Merkel cell cancer (n=4), renal cell or adrenocortical carcinoma (n=4), urothelial carcinoma (n=3), breast carcinoma (n=1), and thyroid carcinoma (n=1). Also excluded were those with a history of severe congestive heart failure (n=7) or inadequate medical or pathology records (n=15).
The distribution of PDB (5 involving the skull, clavicle, or humerus; 27 involving the spine and/or pelvis; and 9 involving the femur, tibia, or calcaneous) did not match with that of bone metastases that occurred upfront or developed subsequently, except for one patient who had a documented ‘burnt-out’ PDB involving L3, which was later on shown to harbour a biopsy-proven prostate cancer metastasis. At various times during their course of disease, six patients with PDB received bisphosphonate therapy (four with zoledronic acid, one with pamidronic acid, and one with risedronic acid) and three patients in the control arm received treatment for bone health (two with zoledronic acid and one with teriparatide).
Univariate analyses of time to bone metastasis and overall survival were performed using the Kaplan–Meier method and life tables for the factor PDB (the Paget’s vs non-Paget’s groups). Figure 1 shows the Kaplan–Meier curves of the time from diagnosis of prostate cancer to the time of detection of bone metastasis in the Paget’s and non-Paget’s groups. There were 15 bone metastasis events in the Paget’s group and 22 events in the non-Paget’s group. The estimated median times from diagnosis to bone metastasis were 21.5 and 9.4 years for the Paget’s and non-Paget’s groups, respectively. That difference was statistically significant (P=0.044, log-rank test). In a similar format, Figure 2 demonstrates the difference in overall survival of patients with comorbid PDB and of those without it. There were 14 deaths in the Paget’s group and 25 deaths in the non-Paget’s group. The estimated median overall survival times were 11.8 and 9.2 years for the Paget’s and non-Paget’s groups, respectively; this difference was also statistically significant (P=0.008, log-rank test). As death in prostate cancer patients without bone metastasis will prevent the occurrence of bone metastasis in those patients, the events of death without bone metastasis will compete against the events of occurrence of bone metastasis. Therefore, we performed Fine–Gray competing risk analysis to exclude the influence of death without bone metastasis on the cumulative incidence of bone metastasis (Figure 3). We found that PDB significantly delays the occurrence of bone metastasis compared with the control non-Paget’s group (P=0.030), whereas there was no significant difference in the cumulative incidence of death without bone metastasis between the two groups (P=0.994).
We used the multivariate Cox regression modelling to examine the impact of PDB while controlling for factors that are known to influence the outcome events. The factors in the models were determined a priori. Age at diagnosis of prostate cancer, Black race, advanced disease (stage 3 or higher), high Gleason score (8 or higher), and comorbidity (as measured by age-unadjusted Charlson comorbidity score) are known factors influencing overall survival. As active PDB is often treated with bisphosphonate therapy and bisphosphonate may influence bone metastasis, bisphosphonate therapy is also entered into the equations. For the time between prostate cancer diagnosis and development of bone metastasis, Cox modelling results indicate that disease stage 3 or higher and PDB were statistically significant predictors of the time to develop bone metastasis (Table 2a). A similar evaluation for association between those same factors and overall survival time revealed that age at diagnosis, disease stage 3 or higher and PDB were significant predictors of overall survival (Table 3a). However, the sample size in our data set is small; to mitigate the potential danger of overfitting the Cox models and ending up with spurious results, we also examined alternative Cox models with four factors. For the time between prostate cancer diagnosis and development of bone metastasis, disease stage 3 or higher and PDB were statistically significant predictors, but tumour grade and bisphosphonate usage were not (Table 2b). For overall survival, disease stage 3 or higher and PDB were significant predictors, but tumour grade and age adjusted Charlson comorbidity were not (Table 3b). Therefore, PDB is a robust predictor of delayed bone metastasis and improved overall survival.
Of note, 4 out of 14 patients with PDB who passed away never developed bone metastasis. Eight of these 14 patients developed visceral metastases (in the lungs or liver) or locally advanced disease (involving the bladder, rectum, or penis, causing haematuria or perineal pains, or requiring urinary diversion). Similarly, 4 out of 25 patients without PDB who passed away did not develop bone metastasis. Six of these 25 patients developed visceral metastases or locally advanced disease.
Discussion
The results from this matched case–control study provide evidence for the first time, to our knowledge, that comorbid PDB has a favourable effect on the overall survival time of patients with prostate cancer (11.8 years, Paget’s group, vs 9.2 years, non-Paget’s group; P=0.008). That observed improvement in overall survival time is consistent with our finding that the time from the diagnosis of prostate cancer to the development of bone metastasis was longer in the patients who had both diseases.
We recognise that cancer-specific survival time, not overall survival time, would have been a preferable end point in this study, but it was not possible to obtain that information because complete details of the cause of death were not available in the medical records. Considering that many patients with PDB likely died from causes unrelated to their cancer, we expect that their cancer-specific survival time would have been longer than their overall survival time. Thus, we believe that the results reported here could actually underestimate the cancer-specific survival time of prostate cancer patients with PDB. This would account for a merge of the survival curves after 10 years in Figure 2.
The distinction between prostate cancer bone metastasis and PDB was subtle in some cases and required confirmation by experienced radiologists. It is true that the timing of radiographic studies could have affected the time between prostate cancer diagnosis and bone metastasis, but the likelihood of finding new bone lesions on a bone scan when the PSA concentration was increasing would be the same for both groups. Therefore, the chance that any lead-time bias favoured either group in this study was low. In fact, one would expect that the attention and scrutiny resulting from the identification of bony abnormalities in PDB would lead to a bias against patients with PDB for the early detection of prostate cancer bone metastasis.
It is important that the patients in the two groups were well matched for age at time of diagnosis, disease stage, Gleason grade, initial therapy, and Charlson comorbidity score. Although the baseline PSA concentration was slightly higher in the non-Paget’s group, the difference was not statistically significant. Black patients tend to harbour a more aggressive form of prostate cancer than whites do, (Danley et al, 1995; Clegg et al, 2002), and there were more Black patients in our Paget’s group than in the non-Paget’s group (P=0.096), but the better survival results in the Paget’s group cannot be accounted for by this imbalance.
It remains unknown what effect the stage, location, or extent of PDB has on prostate cancer. Additional questions include whether treatment of PDB negates any benefits that PDB may have on prostate cancer and whether that treatment itself delays prostate cancer bone metastasis. However, our data do not suggest that the use of bisphosphonates either counteracts or causes any such effects, because this treatment is a relatively recent practice and most of the patients we studied never received it.
Our results suggest that PDB alters the bone microenvironment and interferes with the progression of prostate cancer in bone. Although a plethora of factors are involved in the progression of prostate cancer, it is unlikely that all of them actually have an effect on bone metastasis. We propose that PDB provides a unique experiment of nature through which we can identify factors that may be used to prevent the progression of prostate cancer to bone.
It is plausible that patients with PDB have a distinct bone condition or a unique bone microenvironment that protects them from prostate cancer bone metastasis. For instance, 67% of the genetic risk for PDB is derived from genetic variants close to four genes that are in some manner involved in osteoclastogenesis: CSF1 (macrophage colony-stimulating factor); OPTN (optineurin, a nuclear factor-kappa B (NF-κB) essential-modulator-related polyubiquitin-binding protein); TM7SF4 (DC-STAMP, a dendritic cell-specific transmembrane protein, master regulator of osteoclast fusion); and TNFRSF11A (a receptor activator of NF-κB or RANK) (Chung et al, 2010).
Another factor for the apparent effect of PDB on progression of prostate cancer may be overproduction of Dickkopf-1 (DKK-1, a Wnt antagonist). Dickkopf-1 is implicated in osteolytic diseases, including PDB (Marshall et al, 2009), multiple myeloma (Tian et al, 2003), and rheumatoid arthritis (Diarra et al, 2007), in which it enhances osteoclastic activity by inhibiting bone formation and stimulating its breakdown. In particular, osteoblasts from patients with PDB overexpress DKK-1, leading to elevated serum DKK-1 concentrations in such patients (Marshall et al, 2009). We speculate that certain bone factors such as DKK-1, which are produced by pagetoid osteoblasts, myeloma plasma cells, and rheumatoid synovial fibroblasts, inhibit the progression of prostate cancer bone metastasis. Of note, elevated DKK-1 expression occurs early in prostate carcinogenesis; as the disease progresses, DKK-1 expression declines, particularly in advanced bone metastases (Hall et al, 2008). This decline of DKK-1 in bone metastases coincides with a surge in Wnts and increased prostate-cancer-induced osteoblastic activity (Hall et al, 2005). Likely, the overproduction of DKK-1 in PDB antagonises the osteogenic activity of the Wnts. Further, elevated levels of DKK1 may negatively influence several important steps of bone metastasis, such as mobilisation, engraftment, and proliferation of prostate cancer stem cells to and within the bone marrow (Tian et al, 2003; Adams and Scadden, 2006; Lee et al, 2011).
It is of interest whether a delay in bone metastasis ensures an improvement in overall survival time of patients with prostate cancer. Recently, a randomised phase III trial demonstrated that denosumab delayed bone metastasis by 3.7 months, but did not affect the overall survival of men with castrate-resistant prostate cancer (Smith et al, 2012). Currently, a randomised Zoledronic acid EUropean Study trial is being conducted to determine whether zoledronic acid can delay bone metastasis in high-risk patients with androgen-dependent prostate cancer. The fully human monoclonal antibody denosumab specifically inhibits osteoclastic activity by binding and inactivating the ligand of RANK. The bisphosphonate zoledronic acid also inhibits osteoclastic activity by reducing osteoclast development from precursor, disrupting bone resorption after internalisation by osteoclasts and inducing apoptosis of osteoclasts. Therefore, we anticipate that the effects of PDB on prostate cancer bone metastasis are more complex than merely increased osteoclastogenesis or osteoclastic activity in bone.
Further studies need to be performed to confirm the preliminary results of our exploratory retrospective study. Ideally, we would conduct a prospective clinical trial to validate our results. However, given the scarcity of patients who have prostate cancer with comorbid PDB, the relative longevity of these patients, and the logistics and cost that such studies will incur, we realise that it may not be feasible to conduct such a definitive prospective study. An alternative way to validate our findings is to discover disease correlations and stratify patient cohorts by using electronic patient records (Roque et al, 2011).
In summary, for the first time, to our knowledge, we have obtained data showing that in patients with both prostate cancer and PDB, the time to develop bone metastasis is delayed and the overall survival time is longer than they are in men with prostate cancer alone. Our results suggest that certain bone factors related to the presence of PDB affect the progression of prostate cancer bone metastasis. Future study of these factors may enhance our understanding of the biology of prostate cancer bone metastasis and facilitate the discovery of relevant targets for use in developing effective prostate cancer treatments.
References
Adams GB, Scadden DT (2006) The hematopoietic stem cell in its place [review]. Nat Immunol 7: 333–337
Charlson ME, Ales KA, Pompei P, MacKenzie CR (1987) A new method of classification of prognostic comorbidity for longitudinal studies: development and validation. J Chron Disease 40: 373–383
Chung PYJ, Beyens G, Boonen S, Papapoulos S, Geusens P, Karperien M, Vanhoenacker F, Verbruggen L, Fransen E, Van Offel J, Goemaere S, Zmierczak HG, Westhovens R, Devogelaer JP, Van Hul W (2010) The majority of the genetic risk for Paget’s disease of bone is explained by genetic variants close to the CSF1, OPTN, TM7SF4, and TNFRSF11A genes. Hum Genet 128: 615–626
Clegg LX, Li FP, Hankey BF, Chu K, Edwards BK (2002) Cancer survival among US whites and minorities: a SEER (Surveillance, Epidemiology, and End Results) Program population-based study. Arch Intern Med 162: 1985–1993
Cooper C, Schafheutle K, Dennison E, Kellingray S, Guyer P, Barker D (1999) The epidemiology of Paget’s disease in Britain: is the prevalence decreasing? J Bone Miner Res 14: 192–197
Danley KL, Richardson JL, Bernstein L, Langholz B, Ross RK (1995) Prostate cancer: trends in mortality and stage-specific incidence rates by racial/ethnic group in Los Angeles County, California (United States). Cancer Causes Control 6: 492–498
Diarra D, Stolina M, Polzer K, Zwerina J, Ominsky MS, Dwyer D, Korb A, Smolen J, Hoffmann M, Scheinecker C, van der Heide D, Landewe R, Lacey D, Richards WG, Schett G (2007) Dickkopf-1 is a master regulator of joint remodeling. Nat Med 13: 156–163
Hall CL, Bafico A, Dai J, Aaronson SA, Keller ET (2005) Prostate cancer cells promote osteoblastic bone metastases through Wnts. Cancer Res 65: 7554–7560
Hall CL, Daignault SD, Shah RB, Pienta KJ, Keller ET (2008) Dickkopf-1 expression increases early in prostate cancer development and decreases during progression from primary tumor to metastasis. Prostate 68: 1396–1404
Lee Y-C, Cheng C-J, Bilen MA, Lu JF, Satcher RL, Yu-Lee LY, Gallick GE, Maity SN, Lin SH (2011) BMP4 promotes prostate tumor growth in bone through osteogenesis. Cancer Res 71: 5194–5203
Marshall MJ, Evans SF, Sharp CA, Powell DE, McCarthy HS, Davie MWJ (2009) Increased circulating Dickkopf-1 in Paget’s disease of bone. Clin Biochem 42: 965–969
Roque FS, Jensen PB, Schmock H, Roque FS, Jensen PB, Schmock H, Dalgaard M, Andreatta M, Hansen T, Søeby K, Bredkjær S, Juul A, Werge T, Jensen LJ, Brunak S (2011) Using electronic patient records to discover disease correlations and stratify patient cohorts. PLoS Comput Biol 7: e1002141
Smith MR, Saad F, Coleman R, Shore N, Fizazi K, Tombal B, Miller K, Sieber P, Karsh L, Damião R, Tammela TL, Egerdie B, Van Poppel H, Chin J, Morote J, Gómez-Veiga F, Borkowski T, Ye Z, Kupic A, Dansey R, Goessl C (2012) Denosumab and bone-metastasis-free survival in men with castration-resistant prostate cancer: results of a phase 3, randomised, placebo-controlled trial. Lancet 379: 39–46
Tian E, Zhan F, Walker R, Rasmussen E, Ma Y, Barlogie B, Shaughnessy JD (2003) The role of the Wnt-signaling antagonist DKK1 in the development of osteolytic lesions in multiple myeloma. N Engl J Med 349: 2483–2494
Tu S-M, Lin S-H, Podoloff DA, Logothetis CJ (2010) Multimodality therapy: bone-targeted radioisotope therapy of prostate cancer (review). Clin Adv Hematol Oncol 8: 341–351
Tu S-M, Lin S-H (2008) Current trials using bone-targeting agents in prostate cancer (review). Cancer J 14: 35–39, ; erratum in Cancer J 2008 May-June; 14: 199
Acknowledgements
This study was supported in part by the National Institutes of Health through the MD Anderson’s Cancer Center Support Grant CA016672. We thank Sue-Hwa Lin, PhD, and Karen Phillips, ELS, for editorial assistance. We also thank Avik Som and Cherie Perez for help with collecting cases and regulatory issues.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Tu, SM., Som, A., Tu, B. et al. Effect of Paget’s disease of bone (osteitis deformans) on the progression of prostate cancer bone metastasis. Br J Cancer 107, 646–651 (2012). https://doi.org/10.1038/bjc.2012.315
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.315
Keywords
This article is cited by
-
Pearls and pitfalls in clinical interpretation of prostate-specific membrane antigen (PSMA)-targeted PET imaging
European Journal of Nuclear Medicine and Molecular Imaging (2017)
-
The Implications of the Sequestosome 1 Mutation P392L in Patients with Paget’s Disease in a United States Cohort
Calcified Tissue International (2016)