Abstract
Although only a relatively small proportion of cancer is attributable to occupational exposure to carcinogenic agents, the estimated number of deaths due to occupational cancer is high when compared to other deaths due to work-related ill health and injury. However, risk from occupational exposure to carcinogens can be minimised through proportionate but effective risk management. The Health and Safety Executive (HSE) is the regulator of workplace health and safety in Great Britain. As part of its aim to reduce ill health arising from failures to control properly exposure to hazards at work, HSE commissioned the research presented elsewhere in this supplement to enable it to identify priorities for preventing occupational cancer. The research has shown that occupational cancer remains a key health issue and that low-level exposure of a large number of workers to carcinogens is important. The finding that a small number of carcinogens have been responsible for the majority of the burden of occupational cancer provides key evidence in the development of priorities for significant reduction of occupational cancer. Although the research presented in this supplement reflects the consequences of past exposures to carcinogens, occupational cancer remains a problem. The potential for exposure to the agents considered in this research is still present in the workplace and the findings are relevant to prevention of future disease. In this article, the principle approaches for risk reduction are described. It provides supporting information on some of the initiatives already being undertaken, or those being put in place, to reduce occupational cancer in Great Britain. The need also for systematic collection of exposure information and the importance of raising awareness and changing behaviours are discussed.
Similar content being viewed by others
Main
Society expects people to support themselves and their families by seeking gainful employment, and being employed is now generally recognised as beneficial to the health and well-being of individuals and those dependent on them. However, work can involve exposure to health and safety risks that may have the potential to cause harm; individuals should be able to expect that any potential harm in their work environment would be properly addressed. Unlike lifestyle factors, such as smoking and obesity, occupational exposure to carcinogens is mostly involuntary where it occurs. The risks from such exposure can, however, be minimised through proportionate but effective risk management.
The Great Britain (GB) Health and Safety Executive (HSE) is responsible for enforcing the legislation that requires employers to ensure, so far as is reasonably practicable, the health and safety of their workers and others arising from their work activities. It also provides guidance, advice and support to duty holders. The concept of ‘reasonable practicability’ is a key element of GB health and safety legislation and has the purpose of ensuring a proper balance between risks and the cost in terms of time trouble and money to reduce them. The papers presented earlier in this supplement demonstrate the potential for workplace hazards to present significant risks of cancer for people at work in Britain (Rushton et al, 2012). The measures required for control of carcinogens present in the workplace are consequently more demanding than for many other workplace hazards.
This paper describes the principles applied to the prevention of work-related cancer in Britain, HSE's overarching strategy for bringing about continuing improvements in health and safety (HSE, 2009b), including preventing work-related cancer, and provides examples of how HSE is addressing some of the important hazards identified elsewhere in the supplement.
Broad principles for the prevention of exposure to carcinogens at work
The legal framework for controlling exposure to occupational carcinogens is set out in the Health and Safety at Work Act 1974 (HMSO, 1974) and secondary legislation in the form of regulations stemming from it. This legislation makes the creator of any potential risk responsible for its control. The Health and Safety Executive, along with local authorities, regulates the performance of such duty holders and does so by providing information and advice, as well as enforcing compliance with the law. HSE also advises the British Government on health and safety policy matters such as the need to introduce or revise legislation and the negotiation of European Directives.
The main regulations addressing risks from carcinogens are the Control of Substances Hazardous to Health (COSHH) Regulations 2002 (HMSO, 2002), the Control of Asbestos Regulations (CAR) (HMSO, 2006), the Ionising Radiation Regulations (IR) (HMSO, 1999), the Registration, Evaluation, Authorisation and Restriction of Chemicals Regulation (REACH) 2008 (ECHA, 2006; HMSO, 2008) and the Classification, Labelling and Packaging of Hazardous Chemical Regulation (CLP) 2008 (ECHA, 2008). COSHH, IR and CAR address control in the workplace itself; REACH and CLP address the marketing and movement of chemicals, and are not dealt with further here.
COSHH prohibits the use of some substances and requires duty holders to protect employees from exposure to other hazardous substances. It is based on the principle of risk assessment and application of a ‘hierarchy’ of controls to prevent risk as far as is reasonably practicable.
Elimination from use and substitution of a carcinogen by a lesser hazard are the first considerations in the hierarchy of control. Where this is not practical, the next level of controls should limit the number of workers exposed and reduce the intensity and duration of the exposure to as low as reasonably practicable. Control measures include a hierarchy flowing from isolation, through engineering controls, to using personal protective equipment. An example of engineering controls is putting in place local exhaust ventilation systems to remove hazardous dusts, gases or vapours. Administrative controls are essential and include training, safe operating procedures, preventative maintenance schedules on machines and equipment, and effective plans for system failure.
The choice of the control measures depends on the actual exposure circumstance, the workplace and practicality, but the objective is to eliminate the harmful exposure or control the level of exposure as low as reasonably practicable. In addition to these key prevention strategies, periodical health surveillance to identify and reduce the number of individuals at higher risk may also be useful. A similar approach to risk assessment and a hierarchy of controls is required by CAR and IR.
HSE's strategic approach to workplace control of carcinogen exposure
The impact of legislation on reducing carcinogen exposure could be limited without suitable implementation strategies. The incidence of work-related disease in Britain remains significant (as shown by the data presented in this supplement (Rushton et al, 2012)), and although cases of work-related cancer seen now will be a consequence of exposures in the past the current prevalence and levels of exposure to workplace carcinogens leave no room for complacency (Cherrie, 2009).
HSE has an overarching strategy (HSE, 2009b) for engaging with others in the health and safety system to ensure proportionate control of risks at work. This is built around all those with a role (employers, manufacturers and suppliers, workers, third-party organisations, HSE and local authorities) working in partnership to deliver the desired outcomes. Elements of success might include strong leadership from company board level through to supervisory levels, so that health and safety management is integrated with other key management priorities; competence in identifying and prioritising risks and implementing the right controls; and the provision of advice, guidance and, where appropriate, inspection, investigation and enforcement actions by HSE and local authorities. HSE will undertake and commission research where it is best placed to do so, but will look first to industry to address important gaps in knowledge specific to discrete business sectors.
The following examples, which relate to a number of the key findings from the occupational cancer burden project, are used to illustrate some of the practical challenges associated with controlling exposure to carcinogens and HSE's approach to addressing them.
Asbestos
Asbestos continues to be responsible for the largest proportion of the overall burden of occupational cancer. The study reported in this supplement estimates that one in two occupational cancer deaths and one in three occupational cancer registrations were caused by past occupational exposure to asbestos (Rushton et al, 2010; Hutchings and Rushton, 2012). Mesothelioma is responsible for the largest burden of occupational cancer due to occupational exposure to asbestos. Data from the Mesothelioma Register have shown that the annual mesothelioma deaths have increased from 153 deaths in 1968 to 2084 in 2005 and 2249 in 2008 in GB (HSE, 2010c).
This large increase in annual mesothelioma deaths was driven by high exposure to asbestos many years ago. According to the figures for asbestos imports, the use of asbestos peaked in 1960s and reduced sharply in 1970s in GB. Since 1985, the importation, supply and new use of asbestos were banned completely in the country. However, there is still a considerable amount of asbestos in old buildings where hazardous exposure can still occur during removing and stripping the asbestos materials (Hodgson et al, 2005; Rake et al, 2009). Because of the long latency in disease development (15–60 years), this increased trend of mesothelioma deaths is predicted to continue and peak within the next 10 years and then fall away (Tan et al, 2010). Such is the nature of the epidemic curve that a total of around 91,000 cases in men will have occurred eventually as a consequence of the widespread importation and the use of asbestos before the introduction of bans on importation, supply and new use of various types of asbestos over a number of years, leading up to a complete ban in 1985.
The case–control study conducted by Rake et al (2009), using structured interviews and job titles, provides evidence on the shift of asbestos exposure by industry. Prior to it being banned, control of asbestos exposure was initially focussed on traditional manufacturing industry (insulation board, textiles, friction materials and asbestos cement). Exposure of manufacturing workers more generally, for example, in ship building, and construction workers, particularly carpenters working with amosite containing insulation board, was less well controlled in the 1970s (meaning that carpenters with >10 years of exposure before the age of 30 years currently have a 1 in 17 lifetime risk for mesothelioma). The heaviest exposure had ceased by 1982. Workers engaged in renovating and maintaining asbestos-contaminated old buildings (as well as those working in asbestos removal and stripping) are now potentially at highest risk of exposure, a finding that confirms those from earlier analyses of mesothelioma mortality by occupation as recorded on the death certificate.
The new challenge in controlling exposure to asbestos has therefore been to change the focus of preventive efforts and increase awareness of the potential presence of asbestos, in old buildings for example, and to communicate the need to manage the risk effectively to those responsible, and those most affected by it. Regulation 4 of the CAR 2006 now requires owners of non-domestic premises to know where asbestos is present in their buildings and make that information known to those who may disturb it (HMSO, 2006). To complement this, ‘The Asbestos: Hidden Killer’ campaign (HSE, 2009a) was designed to capture the attention of tradesman and maintenance workers and has successfully helped them understand when they might be in contact of asbestos at work and how to protect themselves.
Respiratory crystalline silica
Findings from the cancer burden study have given a new emphasis to the need for effective control of occupational exposure to respiratory crystalline silica (RCS) (IARC, 1997). They demonstrate the impact that widespread exposure to carcinogens can have even if the exposure creates a relatively low level of risk. The relative risk of lung cancer for workers with prolonged (>15 years) exposure ranges between 1.17 and 1.47 (Pelucchi et al, 2006), but it is estimated that about 2.8 million workers have ever been exposed to RCS during the 40 years of the risk exposure period (Hutchings, 2007), and overall this leads to an estimated attributed number of about 800 lung cancer deaths in GB in 2005 (Rushton et al, 2010).
In April 2006, the European Network for Silica (NEPSI), which includes European employee and employer sector associations, signed the Social Dialogue agreement. This represented the commitment of five industry sectors with >2 million employees to reduce exposure to RCS in brick and tile manufacture, as well as quarrying. Although this initiative has gained the support from key sectors of industry, the construction sector was not directly involved.
Between 2005 and 2008, HSE carried out a survey of RCS exposure in four industry sectors namely brickworks and tile manufacture, quarrying, stonemasonry and construction and found that a large proportion of workers continued to be exposed to RCS at a level above the current workplace exposure limit (Easterbrook, 2009).
In 2008, HSE worked with stakeholders who used construction methods with the potential for silica exposure (such as power tool cutting of silica-containing kerbs, blocks and paving slabs) to promote awareness and knowledge of RCS risks within the industry and to increase the use of effective engineering control measures such as wet cutting to reduce dust emissions and on-tool ventilation extraction (HSE, 2008, 2010e). The key to the success of this initiative was collaboration with industry to identify what would work best to bring about the necessary change in understanding and commitment to improve control. For example, in the application of a supply chain model in construction to control silica exposure, a new cut-off saw for cutting stone and concrete with a novel electronic control system to optimise water supply for dust suppression was launched. The impact of this collaboration with industry has been evaluated in a HSE-funded study ‘Achieving change using the supply chain model in construction’ conducted by the Institute for Employment Studies (Wilson, 2011). Research has also been undertaken to establish a standard for the health surveillance of silica-exposed workers, in order to assist duty holders in complying with the appropriate legislation (Bradshaw et al, 2010).
Diesel engine exhaust
Diesel engine exhaust (DEE) was classified as a Group 2A probable human carcinogen by the IARC in 1989 (IARC, 1989). This was based on sufficient evidence in experimental animals but limited evidence in humans. Twenty years after the IARC evaluation, the specific causal link between DEE and lung cancer has not yet been confirmed. This uncertainty has posed challenges for developing regulatory policies for the control of DEE. The risk of cancer due to long-term (>20 years) exposure to DEE is probably moderately increased, with smoking-adjusted relative risk of 1.47 (95% CI=1.29–1.67), according to a synthesis of pooled epidemiologic studies (Lipsett and Campleman, 1999). The major source of workplace exposure to DEE is from heavy vehicles that use diesel fuel such as buses, trains, lorries, tractors and forklift trucks in the transportation, distribution, mining, farming and heavy construction industries. DEE is also generated from stationary power engines, which may be present in tunnels, alongside railway lines during maintenance work and on construction sites.
There is no clear consensus on the best measure of exposure to DEE, which is a complex mixture of gases and particulates. A survey of 40 work sites that are thought to represent a cross-sectional occupational exposure to DEE in the United Kingdom was conducted (Groves and Cain, 2000) using elemental carbon (EC), one of the particulates in DEE, as a surrogate measure of exposure. The survey showed that the mean exposure to EC from the 217 personal samples was 0.025 mg m−3. Those working with forklift trucks had the highest exposure of 0.066 mg m−3. Wheatley and Sadhra (2004) subsequently carried out a survey in nine distribution depots where, in particular, forklift trucks were used. The mean exposure to EC ranged between 0.011 and 0.055 mg m−3. Although these EC levels were not considered high when compared to the recommended exposure limit of 0.1 mg m−3 in Germany and Austria, they have been associated with increases in lung cancer in exposed workers as indicated in a recent study (Silverman et al, 2012).
The ubiquity of DEE exposure makes control of exposure challenging, and although exposure to DEE is often relatively low large numbers of workers are continuously exposed to it, leading to substantial attributed numbers of occupational cancers. Furthermore, DEE is one of few known carcinogens that have little evidence of effective reduction in exposure levels in recent years, whereas the number of exposed workers is increasing (Cherrie et al, 2007).
HSE's investment in the Occupational Cancer Burden project has provided the evidence that DEE is the third largest contributor to lung cancers attributable to occupation, with an estimated 605 lung cancer deaths. There were also an estimated 47 bladder cancer deaths per year in GB in 2005 that were also attributable to exposure to DEE (Brown et al, 2012a; Brown et al, 2012b). However, there are uncertainties in the actual estimated number of cancers due to DEE because of the lack of reliable exposure data, for example, in the classification of the prevalence of high or low exposure in the GB working population.
HSE produced specific guidance in 1999 to provide practical advice to employers and self-employed people on how to control exposure to DEE emissions in workplace. This guidance was recently updated in 2008 (HSE, 2010e).
Shift work and breast cancer
In 2007, IARC classified shift work, especially night work, as a group 2A probable human carcinogen, causing female breast cancer (Straif et al, 2007). This classification was based on sufficient evidence in experimental animals but limited evidence in humans (i.e., few studies, with potential for unadjusted confounding, and inconsistent definitions of shift work). If the putative causal link is confirmed, the elevated risk of breast cancer would likely be modest with a relative risk of 1.51 (95% CI=1.36–1.68), based on an analysis of a pool of epidemiologic studies in Europe and the United States (Megdal et al, 2005). The risk appears to be concentrated in female workers who have been engaged in shift work at night for >20 years (Wang et al, 2011). However, given that breast cancer is the most common cancer in women and about 16% of the female workers in the United Kingdom are engaged in shift work, with a large proportion of them involved in night work (Steel, 2010), the public health impact in terms of attributable numbers of cases would be substantial as is confirmed by the analysis presented in this supplement.
Shift work including night work is an essential part of some industries such as health and social care and the emergency services, and is of increasing importance in the context of globalisation of trade and changing expectations of the availability of services. Elimination is therefore not a control option, nor is a reduction in numbers exposed likely to be practicable. Restricting the number of years employed in night work might be an option if the risk is heavily concentrated in those with long histories of such work (Wang et al, 2011). Any solution to this problem will require engagement with all parties that have a stake in the outcome if changes to shift-work patterns were proposed. To ensure that such decisions are based upon sound evidence, HSE has commissioned research (Swerdlow, 2003) and more recently a large study to investigate the link between shift work and risk of breast cancer by analysing data collected by the ‘million women’ study (The Million Women Study Collaborative Group, 1999).
Construction industry
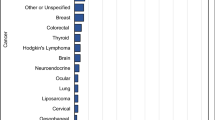
A major outcome of the present HSE study was the recognition that just under half of the estimated cases of occupational cancer (48% of cancer deaths and 41% of cancer registration) in GB were from construction workers, particularly men (Rushton et al, 2010; Hutchings and Rushton, 2012). The top carcinogens and exposure circumstances causing cancer deaths in this industry are asbestos, silica, DEE and working as painters. In addition, solar radiation and polycyclic aromatic hydrocarbons have also caused a large number of cancers, mostly non-melanoma skin cancer, in the industry. Construction is also one of the major hazardous industries and has the highest number of fatal injuries and major injuries (HSE, 2010a). The cancer burden study once again highlighted the construction industry as the hazardous industry that should be the priority for risk reduction.
According to the Labour Market Statistics, published by the Office for National Statistics 2010, the construction industry has over 2 million workers, which comprised ∼7% of the total working population, with the self-employed individuals comprising ∼40% of the workforce, the largest proportion of self-employed workers in the UK industrial makeup (ONS, 2010a). Furthermore, roughly one in ten construction workers are foreign born. This was based on Labour Force Survey data and was likely to be underestimated (ONS, 2010b). Compared with other industrial sectors, a relatively large number of construction workers are working in small and medium-sized enterprises (SMEs). One worker can be working with multiple employers because of the extensive use of sub-contractors. The temporary nature of the working environment also means that the hazard the workers are exposed to will change day to day. The labour market characteristics of the construction industry require a special risk-control strategy for reaching out to the large and diverse group of workers in order to enable them to manage their health and safety risks. This has been part of HSE's strategy goal (HSE, 2010b). Ways to engage workers to achieve positive behaviour change have been investigated in the construction industry (Cameron et al, 2006; Lunt et al, 2008). These have focused more on safety rather than on occupational health. However, the studies recommended ways to raise the profile of occupational health by developing persuasive risk communication techniques, communicating the short-, medium- and long-term consequence of failure to manage risk and emphasising the harm that exposure to occupational health hazards can cause the individual, their family and their colleagues. Further research commissioned by HSE that aimed to inform the development of a strategy to reach and influence small construction site operators also found that the message of ‘Remember, it is dangerous’ has a much stronger impact than ‘Make it safer’. Furthermore, the recent ‘Working Well Together’ campaign (HSE, 2010d) and the ‘Small Sites’ campaign within the construction sector work in partnership with industry stakeholders also have a strong focus on communicating and implementing good health and safety practice in SMEs to reduce work-related injury and ill health.
The future
The estimates of cancer burden presented in this supplement necessarily reflect exposures from the past given the long latent interval between exposure and onset of disease. Cherrie et al (2007) have shown that there has been a steady decline in many occupational exposures over the years, but many have not been eliminated. HSE has commissioned further work to assess the likely future burden of work-related cancer from some key hazards still present in today's work places. The figures derived from these estimates will be valuable in making the case for further efforts to control exposures to carcinogens and minimise any future legacy of avoidable work-related cancer. In addition, early findings suggest that they will also be valuable in assessing the relative effectiveness of different intervention options as has been demonstrated with some hypothetical options in the case of silica (Hutchings and Rushton, 2011).
References
Bradshaw LB, Fishwick J, Powell DS (2010) Health surveillance in silica exposed workers. Prepared by Health and Safety Laboratory for Health and Safety Executive (HSE), http://www.hse.gov.uk/research/rrpdf/rr827.pdf
Brown T, Darnton A, Fortunato L, Rushton L with the Britsh Occupational Cancer Burden Study Group (2012a) Occupational cancer in Britain: Respiratory cancer sites: larynx, lung and mesothelioma. Br J Cancer 107 (Suppl 1): S56–S70
Brown T, Slack R, Rushton L with the Britsh Occupational Cancer Burden Study Group (2012b) Occupational cancer in Britain: Urinary tract cancers: bladder and kidney. Br J Cancer 107 (Suppl 1): S76–S84
Cameron IH, Duff B, Maloney RB (2006) An investigation of approaches to worker engagement. Prepared by Glasgow Caledonian University for the Health and Safety Executive (HSE), http://www.hse.gov.uk/research/rrpdf/rr516.pdf
Cherrie JW (2009) Reducing occupational exposure to chemical carcinogens. Occup Med 59: 96–100
Cherrie JW, Van Tongeren M, Semple S (2007) Exposure to occupational carcinogens in Great Britain. Ann Occup Hyg 51: 653–664
Easterbrook ABP (2009) Silica baseline survey. Prepared by Health and Safety Laboratory for Health and Safety Executive (HSE), http://www.hse.gov.uk/research/rrpdf/rr689.pdf
ECHA (2006) The Registration, Evaluation, Authorisation and Restriction of Chemicals (REACH) EC 1907/2006. European Chemicals Agency (ECHA), Official Journal of the European Union, http://eur-lex.europa.eu/
ECHA (2008) Regulation EC 1272/2008 on Classification, Labelling and Packaging of Substances and Mixtures, and amending Directive 67/548/EEC and Regulation EC 1907/2006. European Chemicals Agency (ECHA), Official Journal of the European Union, http://eur-lex.europa.eu/
Groves J, Cain JR (2000) A survey of exposure to diesel engine exhaust emissions in the workplace. Ann Occup Hyg 44: 435–447
HMSO (1974) The Health and Safety at Work etc. Act 1974. Her Majesty's Stationery Office (HMSO), The National Archives, http://www.legislation.gov.uk
HMSO (1999) The Ionising Radiations Regulations 1999. Her Majesty's Stationery Office (HMSO), The National Archives, http://www.legislation.gov.uk
HMSO (2002) The Control of Substances Hazardous to Health Regulation 2002. Her Majesty's Stationery Office (HMSO), The National Archives, http://www.legislation.gov.uk
HMSO (2006) The Control of Asbestos Regulation 2006. Her Majesty's Stationery Office (HMSO), The National Archives, http://www.legislation.gov.uk
HMSO (2008) The REACH Enforcement Regulation 2008. Her Majesty's Stationery Office (HMSO), The National Archives, http://www.legislation.gov.uk
Hodgson JT, McElvenny DM, Darnton AJ, Price MJ, Peto J (2005) The expected burden of mesothelioma mortality in Great Britain from 2002 to 2050. Br J Cancer 92: 587–593
HSE (2008) Time to Clear the Air! Protect Your Lungs When Using Cut-off Saws. Health and Safety Executive (HSE): Bootle, Merseyside. http://www.hse.gov.uk/pubns/misc830.pdf
HSE (2009a) Asbestos: Hidden Killer Campaign. The Health and Safety Executive: Bootle, Merseyside. http://www.hse.gov.uk/asbestos/hiddenkiller/index.htm
HSE (2009b) The Health and Safety of Great Britain, Be Part of the Solution. Health and Safety Executive: Bootle, Merseyside, http://www.hse.gov.uk/strategy/strategy09.pdf
HSE (2010a) The Health and Safety Executive Statistics 2009/10. In The Annual Statistics Report, Sweeney K (ed). Health and Safety Executive: Bootle, Merseyside. http://www.hse.gov.uk/statistics/overall/hssh0910.pdf
HSE (2010b) The Health and Safety Executive, Business Plan 2010/11. Health and Safety Executive: Bootle, Merseyside. http://www.hse.gov.uk/aboutus/strategiesandplans/businessplans/plan1011.pdf
HSE (2010c) Mesothelioma, Overall Scale of Disease Including Trends. Health and Safety Executive (HSE): Bootle, Merseyside. http://www.hse.gov.uk/statistics/causdis/mesothelioma/mesothelioma.pdf
HSE (2010d) Working Well Together: Construction Industry Awareness. The Health and Safety Executive: Bootle, Merseyside. http://www.wwt.uk.com/content/AbouttheCampaign.aspx
HSE (2010e) Mesothelioma Mortality in Great Britain 1968–2009. Health and Safety Executive (HSE): Bootle, Merseyside. http://www.hse.gov.uk/statistics/causdis/mesothelioma/mesothelioma.pdf
Hutchings S (2007) The Burden of Occupational Cancer in Great Britain, Methodology, Vol. RR595. Health and Safety Executive, HSE Books, http://www.hse.gov.uk/research/rrpdf/rr595meth.pdf
Hutchings S, Rushton L (2011) Toward risk reduction: predicting the future burden of occupational cancer. Am J Epidemiol 173: 1069–1077
Hutchings SJ, Rushton L with the British Occupational Cancer Burden Study Group (2012) Occupational cancer in Britain: Industry sector results. Br J Cancer 107 (Suppl 1): S92–S103
IARC (1989) IARC Monographs on the Evaluation of the Carcinogenic Risks of Chemicals to Humans: Diesel and Gasoline Engine Exhausts and Some Nitroarenes, Vol. 46. International Agency for Research on Cancer: Lyon, France
IARC (1997) IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Crystalline Silica - Inhaled in the Form of Quartz or Cristobalite from Occupational Sources (Group 1) Amorphous Silica (Group3), Vol. 68. International Agency for Research on Cancer: Lyon, France
Lipsett M, Campleman S (1999) Occupational exposure to diesel exhaust and lung cancer: a meta-analysis. Am J Public Health 89: 1009–1017
Lunt JB, Bennett V, Hopkinson J (2008) Behaviour change and worker engagement practices within the construction sector. Prepared by the Health and Safety Laboratory for the Health and Safety Executive (HSE), http://www.hse.gov.uk/research/rrpdf/rr660.pdf
Megdal SP, Kroenke CH, Laden F, Pukkala E, Schernhammer ES (2005) Night work and breast cancer risk: a systematic review and meta-analysis. Cancer chemoprevention – an update on a novel and exciting field of oncology. Eur J Cancer 41 (13): 2023–2032
ONS (2010a) Table 12.6 Employment in the Construction Industry by Gender, Chapter 12 Trends in Employment and the Professions, Construction Statistics Annual 2010. Office for National Statistics (ONS), http://www.statistics.gov.uk/download/theme_commerce/CSA-2010
ONS (2010b) Understanding the divergence between output and employment in the UK construction industry. In Economic & Labour Market Review, Vol. 4, No. 3, March 2010 edition. Office for National Statistics (ONS) http://www.statistics.gov.uk/elmr/03_10/downloads/ELMR_Mar10_Brink.pdf
Pelucchi C, Pira E, Piolatto G, Coggiola M, Carta P, La Vecchia C (2006) Occupational silica exposure and lung cancer risk: a review of epidemiological studies 1996–2005. Ann Oncol 17: 1039–1050
Rake C, Gilham C, Hatch J, Darnton A, Hodgson J, Peto J (2009) Occupational, domestic and environmental mesothelioma risks in the British population: a case-control study. Br J Cancer 100: 1175–1183
Rushton L, Hutchings SJ, Fortunato L, Young C, Evans GS, Brown T, Bevan R, Slack R, Holmes P, Bagga S, Cherrie JW, Van Tongeren M (2012) Occupational cancer in Great Britain. Br J Cancer 107 (Suppl 1): S3–S7
Rushton L, Bagga S, Bevan R, Brown TP, Cherrie JW, Holmes P, Fortunato L, Slack R, Van Tongeren M, Young C, Hutchings SJ (2010) Occupation and cancer in Britain. Br J Cancer 102: 1428–1437
Silverman DT, Samanic CM, Lubin JH, Blair AE, Stewart PA, Vermeulen R, Coble JB, Rothman N, Schleiff PL, Travis WD, Ziegler RG, Wacholder S, Attfield MD (2012) The diesel exhaust in miners study: a nested case-control study of lung cancer and diesel exhaust. J Natl Cancer Inst 104: 1–14
Steel M (2010) Changes in Shift Work Patterns Over the Last Ten Years, 1999–2009. Office for National Statistics (ONS): Newport
Straif K, Baan R, Grosse Y, Secretan B, Ghissassi FE, Bouvard V, Altieri A, Benbrahim-Tallaa L, Cogliano V (2007) Carcinogenicity of shift-work, painting, and fire-fighting. Lancet Oncol 8: 1065–1066
Swerdlow A (2003) Shift work and breast cancer: a critical review of the epidemiological evidence. In HSE Books. Prepared by The Institute of Cancer Research for the Health and Safety Executive 2003, http://www.hse.gov.uk/research/rrpdf/rr132.pdf
Tan E, Warren N, Darnton AJ, Hodgson JT (2010) Projection of mesothelioma mortality in Britain using Bayesian methods. Br J Cancer 103: 430–436
The Million Women Study Collaborative Group (1999) The Million Women Study: design and characteristics of the study population. Breast Cancer Res 1: 73–80
Wang X.-S, Armstrong MEG, Cairns BJ, Key TJ, Travis RC (2011) Shift work and chronic disease: the epidemiological evidence. Occup Med 61: 78–89
Wheatley AD, Sadhra S (2004) Occupational exposure to diesel exhaust fumes. Ann Occup Hyg 48: 369–376
Wilson STC (2011) Achieving change using the supply chain model in construction. Prepared by the Institute for Employment Studies for the Health and Safety Executive (HSE), http://www.hse.gov.uk/research/rrpdf/rr843.pdf
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Chen, Y., Osman, J. Occupational cancer in Britain. Br J Cancer 107 (Suppl 1), S104–S108 (2012). https://doi.org/10.1038/bjc.2012.125
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.125