Abstract
Background:
The endothelin system is involved in tumour growth. Atrasentan, a selective endothelin-A-receptor antagonist, blocks endothelin signalling. This phase I trial studied combining treatment of interferon-alpha (IFN-α) with atrasentan in renal cell carcinoma (RCC).
Patients and methods:
This study evaluated the safety and tolerance of IFN-α (9MU subcutaneously (s.c.) three times a week) in combination with atrasentan (2.5, 5 and 10 mg orally once daily) in untreated metastatic RCC. Cohort 10 mg was extended to obtain insights in efficacy and pharmacodynamics.
Results:
Observed toxicities mainly consisted of known IFN-like toxicities (anorexia, chills, fever, fatigue and nausea), and of nasal congestion (associated to atrasentan). None of these toxicities were considered dose limiting. Cohort 10 mg was extended up to 32 patients; in a subset of patients treated according to the protocol (n=27), median overall survival (OS) was 17.3 months. One patient (3.1%) showed a partial response lasting 14.3 months. In an exploratory analysis, we observed that in the subset of patients with declining vascular endothelial growth factor (VEGF) levels (in combination with rising Endothelin-1 levels), median OS was 22.2 months compared with 2.2 months in patients with increasing VEGF levels.
Conclusion:
Combination treatment of IFN-α 9MU-α s.c. three times a week and atrasentan 10 mg once daily is tolerated. Clinical activity, especially OS, and biomarkers in our view warrant further studies targeting the endothelin axis.
Similar content being viewed by others
Main
Metastatic renal cell carcinoma (mRCC) has been subject to many trials with different approaches, including immunotherapy, chemotherapy and targeted therapy. Until recently and at the moment of designing this study, interferon-alpha (IFN-α) was standard care. This cytokine provided survival benefit over supportive therapy (Coppin, 2008) or hormone therapy with medroxyprogesterone acetate (Medical Research Council Renal Cancer Collaborators, 1999). IFN-α-induced toxicity largely consists of flu-like symptoms (Coppin, 2008). Although its anti-cancer effects are still not comprehensively understood, anti-proliferative, anti-angiogenic and immunogenic characteristics have been described (Kirkwood, 2002). The present treatment options, consisting of sunitinib, sorafenib and bevacizumab, address the vascular endothelial growth factor (VEGF) pathway (Motzer et al, 2007; Escudier et al, 2007a, 2007b).
The target of the current study is the endothelin axis. Endothelin-1 (ET-1) is primarily expressed by endothelial cells but also by cells of certain types of cancer (Nelson et al, 2003). ET-1 promotes the production of VEGF (Ferrara, 2004), through enhanced HIF-1α stability and accumulation (Spinella et al, 2002). Furthermore, ET-1 is mitogenic to cancer cells, and has anti-apoptotic and tumour-enhancing effects (Spinella et al, 2002; Nelson et al, 2003; Ferrara, 2004; Bagnato and Rosano, 2008), mediated by the endothelin-A-receptor (ETAR) (Pflug et al, 2007). Receptor blockade by specific antagonists inhibits the proliferative effects of ET-1 in cancer cells (Nelson et al, 2003) and reverses ET-1-mediated cell survival during chemotherapy-induced apoptosis (Pflug et al, 2007).
Atrasentan (ABT-627) was developed as a potent, selective ETAR inhibitor (Opgenorth et al, 1996). Phase I studies reported maximum tolerated doses of 60 mg (Carducci et al, 2002), 75 mg (Ryan et al, 2004) or 95 mg (Zonnenberg et al, 2003) once daily. Most side effects were attributable to the vasoactive nature, including rhinitis, headache, peripheral oedema and anaemia (caused by hemodilution). On the basis of pharmacodynamic characteristics, the dose of 10 mg once daily was chosen for further studies, mostly performed in prostate cancer (Carducci et al, 2003, 2007).
Because ET-1 and ETAR are overexpressed in RCC (Douglas et al, 2004; Pflug et al, 2007), suggesting pathological endothelin signalling, and because of complementary mechanisms of action exercised by atrasentan and IFN-α, we hypothesised that mRCC patients might benefit from combining these agents. This phase I study evaluates the safety of combination treatment with atrasentan 10 mg once daily and IFN-α 9MU subcutaneously (s.c.) three times a week. An extension cohort was included to obtain an insight into toxicities in a larger set of patients, and to obtain an insight in anti-tumour effects and pharmacodynamics in an exploratory analysis of VEGF and ET-1 kinetics.
Patients and methods
Study design
This open-label phase I study protocol was reviewed and approved by Institutional Review Boards of the participating centres and conducted according to institutional, national and European guidelines. Patients were required to provide written informed consent before study participation. This study was not registered in a trial database, as this was not common practise at the time of initiation. Patient enrolment was between January 2003 and May 2007.
Dose escalation
The primary objective of the dose escalation part, performed by the University Medical Center Utrecht only, was to demonstrate the safety and tolerability of combination treatment of IFN-α (IFN-α-2a, Roferon, Roche; Roche Nederland, Woerden, The Netherlands) 9MU s.c. three times a week and atrasentan (Abbott Laboratories, Chicago, IL, USA) 10 mg orally once daily. A fixed dose of IFN-α was combined with escalating doses of atrasentan (2.5, 5 or 10 mg once daily) in three predefined consecutive cohorts, according to a standard design of 3–6 patients per cohort. Atrasentan was started 2 weeks after the first administration of IFN-α. Dose escalation was based on at least three assessable patients per dose level completing 4 weeks of the combination treatment. Dose limiting toxicity (DLT) was defined as grade 3/4 adverse events occurring in the first 4 weeks of combination treatment, except for nausea, vomiting and fever. Standard supportive care consisted of anti-pyretics (acetaminophen) and anti-emetics (metoclopramide).
Extension of cohort 10 mg
The objective of the extension of cohort 10 mg, performed at two centres, was to obtain better insight into the toxicity and to obtain information on progression-free survival (PFS), overall survival (OS) and biomarkers dynamics. All patients received 10 mg atrasentan once daily and the fixed dose of IFN-α as in the phase 1 dose escalation part.
Toxicity evaluation was performed according to Common Terminology Criteria for Adverse Events version 3.0 (CTCAE). Toxicities were clustered into treatment periods. Period 1 included the 2 weeks of IFN-α monotherapy, period 2 the first 4 weeks of combination treatment and period 3 the episode of continued treatment thereafter.
Treatment was continued for 1 year or until unacceptable toxicity or progressive disease (PD) was reported. PD was assessed according to Response Evaluation Criteria in Solid Tumours (RECIST). PFS and OS were recorded from start of IFN-α treatment until documented PD or death. Clinical outcome was assessed in the patients treated per protocol (exposed to combination treatment), as depicted in Figure 1. Toxicity was evaluated in the intent-to-treat group (receiving at least one dose of IFN-α).
Patients
Patients with histologically confirmed mRCC (including non-clear cell) without prior systemic treatment were included. Tumour progression had to be demonstrated within 6 weeks before the start of study treatment. Other key eligibility criteria included age >18 years, life expectancy of more than 3 months, WHO performance status score of 0–2 and measurable disease. Adequate renal, hepatic, bone marrow and cardiac functions were required, and any hypertension needed to be controlled. Exclusion criteria were primary tumours other than RCC, clinical evidence of cerebral metastases, immune disease, active infection, use of immunosuppressive and/or non-steroidal anti-inflammatory drugs, HIV positivity, pregnancy or lactation. Radiotherapy had to be completed at least 4 weeks before the administration of study medication.
Assessments
Patient visits were planned pre-treatment, once a week during the first 6 treatment weeks, bi-weekly for the next 6 weeks, then every 4 weeks until 36 weeks, followed by every 2 months until treatment termination. Study procedures consisted of physical examination and laboratory assessments. Tumour measurements were performed every 8 weeks on-treatment, with appropriate imaging techniques. After treatment discontinuation, survival evaluation and PD assessment occurred every 3 months for 1 year, thereafter every 6 months.
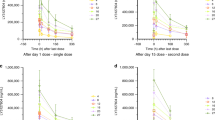
Pharmacodynamic analyses
For an exploratory analysis, plasma samples and platelet counts were obtained pre-treatment, and 2, 4 and 8 weeks after the first administration of IFN-α. Plasma ET-1 and VEGF concentrations were quantified in 27 of 44 patients, using commercially available ELISA kits (R&D Systems, Minneapolis, MN, USA) following manufacturer's protocols.
Statistical analysis
Time-to-event analyses were performed using the Kaplan–Meier methodology.
Paired t-tests were performed to evaluate the changes in biomarker levels over time. The log rank test was used to correlate biomarkers with PFS/OS. Platelet counts were correlated to VEGF levels with the Pearson correlation coefficient.
For these analyses SPSS (version 15.0; SPSS INC., Chigaco, IL, USA) was used with defined significance level of P<0.05. Reported P-values are two-sided.
Results
Conduct of the study
A total of 16 patients were included in three dose escalation cohorts of the phase I study (Figure 1). The total number of patients of cohort 2.5 mg was eight. Because of a DLT (pulmonary embolism) in one patient this cohort was extended. One patient did not complete 4 weeks of combination treatment because of hepatic toxicity ascribed to IFN-α; this patient was replaced. Unintentionally, the first patient of cohort 5 mg received 2.5 mg atrasentan instead of 5 mg once daily; this patient was included in cohort 2.5 mg.
One patient of cohort 5 mg was ineligible for analysis, as the pathologist's review diagnosed metastatic colorectal cancer. Another patient of this cohort discontinued treatment because of cerebral metastases, which became clinically manifested at an early stage of treatment; this patient was replaced and still included in the safety analysis. DLT's were not observed in this cohort.
The three initial patients in cohort 10 mg did not show any DLT. A total of 31 patients were enroled in the extension of cohort 10 mg (Figure 1). Two patients were deemed ineligible because of inadequate performance status and of unconfirmed histological diagnosis; these patients were excluded from the analysis. Combining these numbers, the total number of patients evaluated for toxicity was 32.
Of these 32 patients, 5 did not start atrasentan treatment because of IFN-α toxicity (including 1 allergic reaction), leaving 27 patients in the per protocol group. Patient enrolment in the study was discontinued once sunitinib became available in the Netherlands for first line treatment of mRCC.
Patient characteristics
Gender, age and MSKCC risk scores of the patient groups, as depicted in Table 1, were consistent with recent published studies for RCC (Motzer et al, 2007; Escudier et al, 2007b).
Treatment duration
Results per patient concerning treatment duration and discontinuation, PFS and OS are presented in Table 2.
Phase I
Median time on study treatment for the eligible patients in the escalation part of the study was 163 days (range: 23–364), evaluated from the start of IFN-α administration. Two patients in cohort 2.5 mg discontinued treatment because of toxicity, three because of PD and three because of completion of 1 year of treatment. The discontinuation in cohort 5 mg was caused by toxicity in one patient and PD in two patients. One patient completed 1 year of treatment. One patient in this cohort required a 33% dose reduction of IFN-α, following treatment interruption for 1 week, 2 months after start. In cohort 10 mg two patients discontinued as a consequence of PD, while one patient completed 1 year of treatment.
Extended cohort 10 mg
Median time on study treatment in the entire group (n=32) and the treated per protocol group (n=27) was 68 days (range: 1–364) and 102 days (range: 20–364), respectively. One patient withdrew the informed consent after 1 month of treatment and one patient discontinued treatment because of irradiation of remaining lesions, which had regressed on study treatment. For this patient PFS was censored from the start of radiation treatment. One patient discontinued treatment because of PD, however, retrospectively this patient had PD earlier during treatment. Other treatment discontinuations were due to completion of 1 year of treatment (n=2), PD (n=16) and toxicity (n=12). From the latter 12 patients, 5 received <2 weeks of treatment (only IFN-α), 3 patients 3–4 weeks, 3 patients approximately 2.5 months (1 patient received only 2 weeks atrasentan, but continued with IFN-α) and 1 patient 6 months.
Three patients discontinued IFN-α prematurely after 2, 4 and 5.5 months, but continued atrasentan for an additional 4, 2 and 1 month, respectively. Five patients halted atrasentan treatment after 3 weeks, 1.5 months, 1.5 months, 2 months and 8 months of study start, but continued IFN-α for an additional 1.5 months, 1 week, 3 weeks, 3 weeks and 2 months, respectively.
Toxicity: phase I plus extension of cohort 10 mg
Table 3 shows grade 1/2 treatment-related toxicity when observed in more than one patient and all grade 3/4 adverse events of both phase I study, and the extension of cohort 10 mg. The three atrasentan dose levels were combined, as the occurrence of adverse events was similar both quantitatively and qualitatively (data not shown). All reported non-laboratory adverse events were grade 2 or less, except for fever (excluded as DLT), allergic reaction and pulmonary embolism. Notably, the most adverse events began in period 1 (IFN-α monotherapy). Flu-like symptoms generally diminished over time. Three patients were hospitalised with fever, most likely attributed to IFN-α, accompanied by anorexia/vomiting in two patients. One patient was hospitalised because of an allergic reaction to IFN-α. Three patients had complaints of dyspnoea, weight loss, malaise, nasal congestion or fatigue, resulting in the discontinuation of atrasentan while IFN-α treatment was sustained. Although vasovagal complaints/dizziness were reported by several patients, no relation to hypotension could be established as changes in blood pressure were not observed (data not shown). One hypertensive patient discontinued anti-hypertensive treatment after the start of study treatment and remained normotensive throughout the study. Headaches were handled adequately with acetaminophen.
The observed laboratory abnormalities were as expected from IFN-α or atrasentan treatment. Approximately 85% of patients developed grade 1/2 anaemia during period 2 (first 4 weeks of combination treatment), recovering thereafter. Neutropenia and lymphocytopenia, observed during long-term treatment, did not result in infection.
Clinical outcome measures: per protocol group treated with 10 mg once daily atrasentan
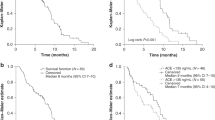
Data cut-off was set at the first of August 2010. In Table 4, median OS and PFS are presented, including data for the separate risk groups (the MSKCC index was also used for patients with non-clear histology RCC) (Motzer et al, 2002). Median and PFS in the per protocol group were 17.3 and 5.1 months, respectively. Best OS of 30 months was observed in the best risk subset.
Eight patients treated with 10 mg atrasentan received treatment with sunitinib or sorafenib upon disease progression. If censored for this treatment, median OS extended to 19.8 months. One patient (3.1%) showed a partial response lasting 14.3 months.
Biomarkers
An exploratory analysis was performed for biomarkers. VEGF expression is an established biomarker associated with worse prognosis in RCC and other tumour types (Djordjevic et al, 2007; Dirim et al, 2008). We reasoned that VEGF and ET-1 levels might serve as potential biomarkers in this study. In an exploratory analysis, 27 of 44 patients were categorised into three groups, according to baseline VEGF levels and dynamics during treatment (Table 4). Group 1 (n=16) showed low plasma baseline VEGF levels, which remained low throughout treatment. Group 2 (n=7) showed elevated baseline levels, which significantly declined during treatment. Finally, in group 3 (n=4), initially elevated levels further increased during treatment.
ET-1 levels significantly increased in group 1 and group 2 (Table 5). However, ET-levels did not change in group 3. Survival analysis was explored for these three groups (Figure 2 and Table 4). Best OS and PFS were observed in groups 1 and 2.
Kaplan–Meier estimates of OS of groups categorised to VEGF level dynamics (definition of groups is outlined in the text and in Table 4).
As platelets are the main transporters of VEGF in the blood (Verheul et al, 1997) and thrombocytosis is related to tumour progression (Symbas et al, 2000; Bensalah et al, 2006), platelet counts were analysed during treatment. Platelet counts appeared to be related to plasma VEGF concentrations (Pearson's correlation coefficient, r=0.64, P=0.01). It is therefore tempting to speculate that platelets might influence tumour biology. Further exploration of this observation is ongoing.
Discussion
This is to our knowledge the first reported study to target the endothelin axis in RCC. In our view, it shows that combination treatment with 9MU IFN-α s.c. three times a week and 10 mg atrasentan orally once daily in previously untreated mRCC patients is well tolerated and seems to show biological and clinical activity.
Observed toxicities (anorexia, chills, fever, fatigue, nausea and nasal congestion) were manageable with supportive care and in accordance with previous studies on IFN-α or atrasentan. None of the toxicities were considered dose limiting. The majority of adverse events originated in the first 2 weeks of IFN-α treatment, before the administration of atrasentan. The number of toxicity-related discontinuations (34% of patients) could be largely attributed to IFN-α, and is comparable to a recent trial combining bevacizumab with IFN-α (Escudier et al, 2007b). Toxicity profiles of IFN-α and atrasentan did not seem to influence each other.
The cohort 10 mg was extended in order to study toxicity more extensively and to obtain a first impression of the clinical activity of this combination. Observed efficacy results showed a median OS of 17.3 months in the per protocol group and 30 months in the best risk group, which is higher than Motzer's defined clinical outcome expectations for IFN-α monotherapy in mRCC (Motzer et al, 2002). We are fully aware that inter-study comparison of clinical outcome is full of limitations. These results suggest an effect of atrasentan on top of IFN-α. Further clinical studies are needed to clarify this effect. Collectively, combination treatment with 9MU IFN-α s.c. three times a week and 10 mg atrasentan orally once daily is tolerated and our data tentatively indicate the notion that this combination might induce a more indolent course of disease, possibly contributed by additive and/or synergistic anti-tumour effects of both the agents.
VEGF is an important target in RCC treatment. IFN-α treatment recently showed to inhibit VEGF expression or secretion in several tumour types in vitro and in vivo (Rosewicz et al, 2004; Wu et al, 2005; Raig et al, 2008; Tochizawa et al, 2008). Moreover, ETAR blockade reduced the promotion of VEGF production (Rosano et al, 2003; Gorenflo et al, 2007). We observed that, although the pre-treatment VEGF levels of patients in group 2 were elevated, the subsequent drop resulted in a clinical outcome that was similar to group 1 with low VEGF concentrations and the best OS. Although exploratory in nature and based on only a small number of patients, these results are of interest because, to our knowledge, no association between reduction of increased pre-treatment VEGF levels and improved clinical outcome has been previously described. We also observed increased ET-1 levels in group 1 and 2 during treatment. If receptor blocking results in increased levels of the ligand, as observed in other studies as well (Carducci et al, 2002; Zonnenberg et al, 2003), this supports a role of atrasentan in these observed pharmacodynamic effects. Further studies will need to clarify these putative effects of atrasentan.
As to how to proceed, the results of this study in our view warrant further exploration of the endothelin axis as a target in mRCC treatment. For a phase II study, a randomised discontinuation trial design for atrasentan with continuous IFN-α or a randomised study with IFN-α with and without atrasentan would be the appropriate study designs. However, as the standard of care has changed from IFN-α to sunitinib, these options are not realistic. Also, a randomised study comparing combination treatment IFN-α and atrasentan with the current standard of care sunitinib is unlikely to be sufficiently supported in the field. Alternatively, atrasentan could be combined with other targeted drugs, particularly VEGF and mTOR inhibitors. This seems especially feasible, as the mild toxicity profiles for atrasentan as a single agent and in combination with interferon suggest a tolerable combination with other targeted drugs. Particularly, the VEGF-reducing activity and vasoactive nature make it an attractive candidate for combination treatment with TKIs.
In conclusion, we present a study combining atrasentan with IFN-α in patients with previously untreated progressive mRCC showing tolerability and clinical anti-tumour effects. Clinical activity seems to be related to low VEGF levels (either low levels throughout treatment or elevated baseline levels that declined during treatment) and to increasing ET-1 levels. These findings warrant further exploration of targeting the endothelin axis in mRCC.
Change history
29 March 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Medical Research Council Renal Cancer Collaborators (1999) Interferon-alpha and survival in metastatic renal carcinoma: early results of a randomised controlled trial. Lancet 353: 14–17
Bagnato A, Rosano L (2008) The endothelin axis in cancer. Int J Biochem Cell Biol 40: 1443–1451
Bensalah K, Leray E, Fergelot P, Rioux-Leclercq N, Tostain J, Guille F, Patard JJ (2006) Prognostic value of thrombocytosis in renal cell carcinoma. J Urol 175: 859–863
Carducci MA, Nelson JB, Bowling MK, Rogers T, Eisenberger MA, Sinibaldi V, Donehower R, Leahy TL, Carr RA, Isaacson JD, Janus TJ, Andre A, Hosmane BS, Padley RJ (2002) Atrasentan, an endothelin-receptor antagonist for refractory adenocarcinomas: safety and pharmacokinetics. J Clin Oncol 20: 2171–2180
Carducci MA, Padley RJ, Breul J, Vogelzang NJ, Zonnenberg BA, Daliani DD, Schulman CC, Nabulsi AA, Humerickhouse RA, Weinberg MA, Schmitt JL, Nelson JB (2003) Effect of endothelin-A receptor blockade with atrasentan on tumor progression in men with hormone-refractory prostate cancer: a randomized, phase II, placebo-controlled trial. J Clin Oncol 21: 679–689
Carducci MA, Saad F, Abrahamsson PA, Dearnaley DP, Schulman CC, North SA, Sleep DJ, Isaacson JD, Nelson JB (2007) A phase 3 randomized controlled trial of the efficacy and safety of atrasentan in men with metastatic hormone-refractory prostate cancer. Cancer 110: 1959–1966
Coppin C (2008) Immunotherapy for renal cell cancer in the era of targeted therapy. Expert Rev Anticancer Ther 8: 907–919
Dirim A, Haberal AN, Goren MR, Tekin MI, Peskircioglu L, Demirhan B, Ozkardes H (2008) VEGF, COX-2, and PCNA expression in renal cell carcinoma subtypes and their prognostic value. Int Urol Nephrol 40: 861–868
Djordjevic G, Mozetic V, Mozetic DV, Licul V, Ilijas KM, Mustac E, Oguic R, Fuckar Z, Jonjic N (2007) Prognostic significance of vascular endothelial growth factor expression in clear cell renal cell carcinoma. Pathol Res Pract 203: 99–106
Douglas ML, Richardson MM, Nicol DL (2004) Endothelin axis expression is markedly different in the two main subtypes of renal cell carcinoma. Cancer 100: 2118–2124
Escudier B, Eisen T, Stadler WM, Szczylik C, Oudard S, Siebels M, Negrier S, Chevreau C, Solska E, Desai AA, Rolland F, Demkow T, Hutson TE, Gore M, Freeman S, Schwartz B, Shan M, Simantov R, Bukowski RM (2007a) Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med 356: 125–134
Escudier B, Pluzanska A, Koralewski P, Ravaud A, Bracarda S, Szczylik C, Chevreau C, Filipek M, Melichar B, Bajetta E, Gorbunova V, Bay JO, Bodrogi I, Jagiello-Gruszfeld A, Moore N (2007b) Bevacizumab plus interferon alfa-2a for treatment of metastatic renal cell carcinoma: a randomised, double-blind phase III trial. Lancet 370: 2103–2111
Ferrara N (2004) Vascular endothelial growth factor: basic science and clinical progress. Endocr Rev 25: 581–611
Gorenflo M, Ullmann MV, Herpel E, Neumayer S, Dieckmann R, Demirakca S, Klimpel H, Hagl S, Gebhard MM (2007) Atrasentan treatment of pulmonary vascular disease in piglets with increased pulmonary blood flow. J Cardiovasc Pharmacol 50: 286–292
Kirkwood J (2002) Cancer immunotherapy: the interferon-alpha experience. Semin Oncol 29: 18–26
Motzer RJ, Bacik J, Murphy BA, Russo P, Mazumdar M (2002) Interferon-alfa as a comparative treatment for clinical trials of new therapies against advanced renal cell carcinoma. J Clin Oncol 20: 289–296
Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Rixe O, Oudard S, Negrier S, Szczylik C, Kim ST, Chen I, Bycott PW, Baum CM, Figlin RA (2007) Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med 356: 115–124
Nelson J, Bagnato A, Battistini B, Nisen P (2003) The endothelin axis: emerging role in cancer. Nat Rev Cancer 3: 110–116
Opgenorth TJ, Adler AL, Calzadilla SV, Chiou WJ, Dayton BD, Dixon DB, Gehrke LJ, Hernandez L, Magnuson SR, Marsh KC, Novosad EI, Von Geldern TW, Wessale JL, Winn M, Wu-Wong JR (1996) Pharmacological characterization of A-127722: an orally active and highly potent ETA-selective receptor antagonist. J Pharmacol Exp Ther 276: 473–481
Pflug BR, Zheng H, Udan MS, D’Antonio JM, Marshall FF, Brooks JD, Nelson JB (2007) Endothelin-1 promotes cell survival in renal cell carcinoma through the ET(A) receptor. Cancer Lett 246: 139–148
Raig ET, Jones NB, Varker KA, Benniger K, Go MR, Biber JL, Lesinski GB, Carson III WE (2008) VEGF secretion is inhibited by interferon-alpha in several melanoma cell lines. J Interferon Cytokine Res 28: 553–561
Rosano L, Spinella F, Salani D, Di CV, Venuti A, Nicotra MR, Natali PG, Bagnato A (2003) Therapeutic targeting of the endothelin a receptor in human ovarian carcinoma. Cancer Res 63: 2447–2453
Rosewicz S, Detjen K, Scholz A, von MZ (2004) Interferon-alpha: regulatory effects on cell cycle and angiogenesis. Neuroendocrinology 80 (Suppl 1): 85–93
Ryan CW, Vogelzang NJ, Vokes EE, Kindler HL, Undevia SD, Humerickhouse R, Andre AK, Wang Q, Carr RA, Ratain MJ (2004) Dose-ranging study of the safety and pharmacokinetics of atrasentan in patients with refractory malignancies. Clin Cancer Res 10: 4406–4411
Spinella F, Rosano L, Di C, V, Natali PG, Bagnato A (2002) Endothelin-1 induces vascular endothelial growth factor by increasing hypoxia-inducible factor-1alpha in ovarian carcinoma cells. J Biol Chem 277: 27850–27855
Symbas NP, Townsend MF, El-Galley R, Keane TE, Graham SD, Petros JA (2000) Poor prognosis associated with thrombocytosis in patients with renal cell carcinoma. BJU Int 86: 203–207
Tochizawa S, Masumori N, Yanai Y, Ohmoto Y, Yabuuchi Y, Tsukamoto T (2008) Antitumor effects of a combination of interferon-alpha and sorafenib on human renal carcinoma cell lines. Biomed Res 29: 271–278
Verheul HM, Hoekman K, Luykx-de BS, Eekman CA, Folman CC, Broxterman HJ, Pinedo HM (1997) Platelet: transporter of vascular endothelial growth factor. Clin Cancer Res 3: 2187–2190
Wu WZ, Sun HC, Shen YF, Chen J, Wang L, Tang ZY, Iliakis G, Liu KD (2005) Interferon alpha 2a down-regulates VEGF expression through PI3 kinase and MAP kinase signaling pathways. J Cancer Res Clin Oncol 131: 169–178
Zonnenberg BA, Groenewegen G, Janus TJ, Leahy TW, Humerickhouse RA, Isaacson JD, Carr RA, Voest E (2003) Phase I dose-escalation study of the safety and pharmacokinetics of atrasentan: an endothelin receptor antagonist for refractory prostate cancer. Clin Cancer Res 9: 2965–2972
Acknowledgements
We acknowledge the UMCU IKMN data managers (especially I van Beuningen), the UMCU study nurses (especially S.Verkleij), M de Waal (data manager NKI-AVL) and H Mallo (nurse practitioner NKI-AVL) for their support. We also thank H Verheul, Department of Oncology, VUMC Amsterdam, for his contribution. Finally, we acknowledge Abbott Laboratories, Chicago, IL, USA. This investigator-initiated trial was supported partially by Abbott Laboratories consisting of drug supply, and an educational grant for data management and laboratory studies. This work was supported by the Dutch Cancer Foundation and an AEGON scholarship (to MW) and by a Dutch Organization for Scientific Research VIDI grant (to RG).
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Groenewegen, G., Walraven, M., Vermaat, J. et al. Targeting the Endothelin Axis with Atrasentan, in combination with IFN-alpha, in metastatic renal cell carcinoma. Br J Cancer 106, 284–289 (2012). https://doi.org/10.1038/bjc.2011.515
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2011.515
Keywords
This article is cited by
-
Integrative meta-analysis identifies microRNA-regulated networks in infantile hemangioma
BMC Medical Genetics (2016)
-
Incidence and Risk of Hypertension with Ramucirumab in Cancer Patients: A Meta-Analysis of Published Studies
Clinical Drug Investigation (2015)
-
Chemotherapy-mediated p53-dependent DNA damage response in clear cell renal cell carcinoma: role of the mTORC1/2 and hypoxia-inducible factor pathways
Cell Death & Disease (2013)
-
Endothelin 1 in cancer: biological implications and therapeutic opportunities
Nature Reviews Cancer (2013)