Abstract
Background:
There are around 2 million cancer survivors in the UK. This study describes the inpatient and day case hospital activity among the population of cancer survivors in England. This is one measure of the burden of cancer on the individual and the health service.
Methods:
The national cancer registry data set for England (1990–2006) is linked to the NHS Hospital Episode Statistics (HES) database. Cohorts of survivors were defined as those people recorded in the cancer registry data with a diagnosis of breast, colorectal, lung or prostate cancer before 2007. The person-time of prevalence in 2006 for each cohort of survivors was calculated according to the cancer type, sex, age and time since diagnosis. The corresponding HES episodes of care in 2006 were used to calculate the person-time of admitted hospital care for each cohort of survivors. The average proportion of time spent in hospital by survivors in each cohort was calculated as the summed person-time of hospital activity divided by the summed person-time of prevalence. The analysis was conducted separately for cancer-related episodes and non-cancer-related episodes.
Results:
Lung cancer survivors had the highest intensity of cancer-related hospital activity. For all cancers, cancer-related hospital activity was highest in the first year following diagnosis. Breast and prostate cancer survivors had peaks of cancer-related hospital activity in the relatively young and relatively old age groups. The proportion of time spent in hospital for non-cancer-related care was much lower than that for cancer-related care and increased gradually with age but was generally constant regardless of time since diagnosis.
Conclusion:
The person-time approach used in this study is more revealing than a simple enumeration of cancer survivors and hospital admissions. Hospital activity among cancer survivors is highest soon after diagnosis. The effect of age on the amount of hospital activity is different for each type of cancer.
Similar content being viewed by others
Main
Cancer survivors are defined as people who are alive following a diagnosis of cancer from some point in their past. In UK, there are approximately 2 million cancer survivors (approximately 1.66 million of these in England), and this number is increasing by 3% per year (Maddams et al, 2009). The size and demographics of the population of cancer survivors has been described, but there is still a need for more detailed analyses of the burden of cancer on the individual and on health-service resources.
This work presents a person-time analysis of a linked cancer registry and health-service activity data set. ‘Person-time of survivorship’ refers to the total time at risk of hospitalisation experienced by a population of survivors, and ‘person-time of hospitalisation’ refers to the total time spent in hospital by this population. Acute health-service utilisation among cancer survivors in England is described according to age and time since diagnosis, for both cancer- and non-cancer-related care. The work presented here is complementary to that previously published by the same authors (Maddams et al, 2011).
Materials and methods
Data
The analysis was based on two linked data sets (Maddams et al, 2011). The first was a national merged cancer registry data set featuring patient and diagnostic information relating to all cancers recorded by the eight regional population-based cancer registries in England. The merging process was carried out by the staff at the Thames Cancer Registry (TCR), on behalf of the United Kingdom Association of Cancer Registries (UKACR). This provided 100% coverage of geographical regions of England and included all registered cancers diagnosed from 1990 to 2006 (inclusive).
This data set was linked to an extract from the NHS Hospital Episode Statistics (HES). Hospital Episode Statistics is a record-level data repository managed by the National Health Service Information Centre on behalf of the Secretary of State for Health. It contains patient, clinical and administrative details for admitted patients and outpatients treated in NHS hospitals in England, and is mainly populated by extracts from routine data flows exchanged between health-care providers and commissioners (NHS Health and Social Care Information Centre, 2010). Each HES record defines a finished consultant episode (FCE) of care under a given consultant in a given NHS provider. A patient's journey from admission to discharge may be made up of several FCEs. The English Cancer Registries’ National HES extract is a subset of the complete HES database and contains only episodes for admitted patients (i.e., inpatients and day patients) who have at least one recorded episode ‘for or with’ cancer. An episode is considered to be ‘for or with’ cancer if any of its 14 diagnostic fields contain an ICD-10 code between C00 and C97 (malignant neoplasms), between D01 and D48 (in situ, benign or uncertain neoplasms) or equal to O01 (hydatidiform mole).
The linkage between these two data sets was designed and developed jointly by the TCR and the Northern and Yorkshire Cancer Registry and Information Service on behalf of the UKACR. The methodology matches fields such as sex, date of birth, date of death, NHS number and postcode across the two data sets and provides a unique patient identifier for matched patients. Using the patient identifier as a link, it is possible to extract all HES episodes of care for a cohort of cancer patients, as defined in the national cancer registry data set.
The national cancer registry data set was used to identify a cohort of cancer survivors who had been both diagnosed with a malignant neoplasm (ICD-10 C00–C97 excluding C44) in the period 1990–2006, and alive for at least some portion of 2006 (Maddams et al, 2011). Subcohorts were defined according to the type of cancer diagnosis received: colon, rectum and anus cancers (ICD-10 C18–C21); lung, bronchus and trachea cancers (ICD-10 C33–C34); prostate cancer (ICD-10 C61); and female breast cancer (ICD-10 C50). Survivors with multiple diagnoses entered multiple subcohorts. The unique patient identifiers were then used to extract all the HES episodes of care that occurred in, or overlapped, the year 2006 for the cohorts of cancer survivors. As the English Cancer Registries’ HES extract contains all inpatient and day case episodes for those patients with at least one cancer-related episode in the entire HES data set, the extracted cancer survivor episodes may or may not mention cancer. Episodes not mentioning cancer may have pertained to an entirely unrelated condition, or (less likely) may have been incorrectly coded. Some cancer survivors had no matching HES episode of care in 2006, because of a failure to register episodes that did occur, a failure in the matching procedure between the two data sets or simply because they were not admitted to hospital in 2006. In this analysis, matched episodes of care were considered to be ‘cancer related’ if one of the 14 diagnostic codes was between C00 and C97 (excluding C44); otherwise, they were considered to be ‘non-cancer related’.
Hospital activity among cancer survivors
A person-time approach was used to describe the effect of age and time since diagnosis on the amount of hospital activity in the population of cancer survivors. When considering the interaction of survivors with the health service, a person-time approach has a distinct advantage, as it allows us to estimate the proportion of survivor time spent admitted to hospital, as well as to count the number of admissions. The calendar year 2006 was the period of analysis. The effect of age was analysed in 5-year age groups, and the effect of time since diagnosis was analysed in 1-year periods and broader periods (<1, 1–5 and 5–16 years since diagnosis).
Diagnoses were available for the period 1990–2006, and thus there were some survivors in the 2006 cohort who had been diagnosed more than 16 years (but less than 17 years) previously. However, the cohort did not contain all such survivors (as no diagnoses from 1989 were available), and therefore the maximum time since diagnosis considered was 16 years.
For each survivor in each cohort, the person-time for which they were prevalent in 2006 (i.e., that which was postdiagnosis and predeath and overlapped the calendar year 2006) was split into segments according to the time points at which the indexing variables ‘time since diagnosis’ and ‘age’ changed (Maddams et al, 2011). The amount of time spent in hospital by cancer survivors was counted in a similar way, according to age and time since diagnosis, for cancer-related and non-cancer-related episodes of care separately. This was achieved using the SAS software package (SAS Institute Inc., Cary, NC, USA) and code developed by JM specifically for this task, similar to the program Lexis.sas by Carstensen (2007).
The proportion of person-time each cohort of survivors spent admitted to hospital, according to age and time since diagnosis, was then calculated by dividing the total population person-time spent in HES activity by the total population person-time of prevalence. This quantity may be interpreted as the mean proportion of time spent in HES activity by a survivor of a given age and time since diagnosis sampled at random. An alternative interpretation is that the quantity provides an estimate of the probability of that survivor being an admitted hospital patient on any given day in the period. It may be presented either as the number of days spent admitted to hospital per 100 person-days or as a percentage of time. Confidence intervals (CIs) for this proportion were calculated by using a standard binomial model, modified to include a dependence parameter (Klotz, 1973; Budescu, 1985), to account for the fact that days spent in hospital for an individual survivor are likely to be clustered together in episodes or spells of care, rather than randomly distributed in time. The dependence was assumed to be of the first-order Markov type, and both the dependence parameters and CIs were estimated using the methods described in Budescu (1985).
Results
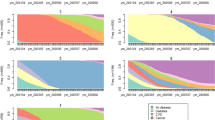
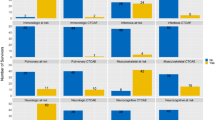
Tables 1 and 2, and the corresponding Figures 1 and 2, display the average number of days (per 100 person-days) that cancer survivors spent admitted to hospital in England during 2006, by 5-year age group or 1-year time since diagnosis period. Data are presented for cancer-related and non-cancer-related episodes of care separately, but are omitted if less than 20 person-years of survivorship contributed to the estimate.
In all age groups older than 35 years, the number of days admitted to hospital for cancer-related episodes of care (per 100 person-days) was highest among lung cancer survivors; it was lowest among prostate and breast cancer survivors. Among prostate cancer survivors, the relatively young and relatively old age groups spent a higher number of days admitted to hospital for cancer-related episodes (per 100 person-days) than the middle-age groups (55–75 years). A similar trend was observed among breast cancer survivors, although the observed increase in the number of days spent admitted to hospital above the age of 75 years was not as significant as among prostate cancer survivors. Among male lung and colorectal cancer survivors, the number of days spent admitted to hospital for cancer-related episodes of care (per 100 person-days) generally decreased as age increased – this association was reversed in male lung cancer survivors under the age of 50 years, but CIs were wide because of a relatively small number of lung cancer survivors in these age groups. Similar age effects were observed among female lung and colorectal cancer survivors.
The number of days spent admitted to hospital for non-cancer-related episodes of care (per 100 person-days) generally increased as age increased above 60 years. Colorectal and lung cancer survivors spent a similar number of days admitted for non-cancer-related episodes of care (per 100 person-days); however, prostate and breast cancer survivors spent significantly fewer.
The number of days survivors spent admitted to hospital (per 100 person-days) for cancer-related episodes of care was much higher in the first year following diagnosis than at any other time. In the first 5 years after diagnosis, it was highest among survivors of lung cancer.
Three periods of time after diagnosis were considered in detail: <1 year, between 1 and 5 years and 5–16 years (as only diagnoses from 1990–2006 were available). The first period contained the majority of the cancer-related hospital activity for all cancer survivors, but the period between 1 and 5 years after diagnosis also had a significant amount of hospital activity.
Figure 3 displays the average number of days spent admitted to hospital (per 100 person-days) by cancer survivors in England in 2006, by 5-year age group and broad post-diagnosis period. Only cancer-related episodes of care are presented in this figure. As with all tables and figures, data are omitted if less than 20 person-years of survivorship contributed. Figure 3 shows that, for each age group, the number of days spent admitted to hospital for cancer-related episodes of care (per 100 person-days) was highest in the first year after diagnosis. For colorectal cancer survivors, it was approximately 30 times higher than in the period >5 years after diagnosis. Similarly, for lung cancer survivors, it was approximately 35 times higher than in the period >5 years after diagnosis. The period 1–5 years after diagnosis also contained significantly more cancer-related hospital activity than the period >5 years after diagnosis: it was approximately four times higher among colorectal cancer survivors, and 7 times higher among lung cancer survivors, although Figure 2 shows that much of this increase is due to the high activity in years 2 and 3 after diagnosis. There was a smaller difference in the cancer-related activity in the periods 1–5 and >5 years after diagnosis among prostate and female breast cancer survivors, compared with colorectal and lung cancer survivors.
Mean cancer-related admitted patient hospital activity among cancer survivors, England, 2006. Number of days admitted to hospital per 100 person-days¶, by 5-year age group and broad time since diagnosis period. ¶With 95% CIs. Only data points with at least 20 survivor person-years are plotted. †Centre of 5-year age group.
The number of days spent admitted to hospital for cancer-related episodes of care (per 100 person-days) in the first year after diagnosis was significantly higher among survivors over the age of 75 years, compared with younger survivors. This is most noticeable for survivors of prostate cancer – those aged ⩾85 years spent around three times as many days admitted in the first year after diagnosis, compared with those aged 70–74 years.
Discussion
This paper presents a person-time analysis of a linked cancer registry and hospital activity data set for England. Age and time since diagnosis were anticipated to be important factors in the level of health-care utilisation among cancer survivors, and were studied in detail. The linked data sets allowed an analysis of all recorded episodes of hospital inpatient or day case health care in England during 2006 among registered cancer survivors, with at least one cancer-related episode recorded in the HES in the period 1990–2006. A person-time approach was used throughout, which made it possible to quantify the intensity of hospitalisation, as well as the associated burden on cancer survivors and the health service, by considering the amount of time spent in hospital, rather than just the number of admissions. Person-time of survivorship and person-time of hospitalisation were classified according to the variables of interest (age and time since diagnosis) – this made it possible to describe in detail the ways in which acute health-service utilisation among survivors was related to these factors.
It is not possible to distinguish between the cancer survivors who had no recorded hospital activity and those for whom the linkage process between the cancer registry and HES data failed. It was therefore not possible to exclude patients with ‘no match’ to HES. This results in an underestimation of the amount of hospital activity among the cancer survivors, but this is believed to be only a small effect.
Each record in the HES data had up to 14 diagnostic codes (using the ICD-10 classification), and 12 operation procedure codes (using the OPCS4 classification), with the first of each of these codes intended to indicate the primary diagnosis/intent of the episode (Maddams et al, 2011). For simplicity, episodes of care were broadly categorised as ‘related to cancer’ or ‘not related to cancer’ according to the diagnostic codes only – an episode was considered to be cancer related if any of the diagnostic codes was between C00 and C97 (excluding C44). This was an intentionally broad definition, designed to negate any possible regional variation in coding of primary diagnosis in the HES data, and to take account of the wide range of health problems associated with cancer and the side effects of its treatment. Defined thus, ‘cancer-related’ hospitalisation for a given survivor may be considered as that directly or indirectly caused by, or associated with, a cancer diagnosis. A future area of study may be to define ‘cancer-related’ HES admissions according to the clinical procedure codes, as well as the admission codes.
Perhaps a more precise way of defining the health-care burden directly attributable to cancer would be to compare hospitalisation of any kind among cancer survivors with that observed in a randomly selected age- and sex-matched subset of the cancer-free population (or, more practically, the general population). This would allow some measure of the ‘background’ hospitalisation experienced by the cancer-free or general population to be removed from the levels observed in cancer survivors. However, no such data set was available to the authors at the time of analysis – the Cancer Registries’ National HES extract only contains episodes of care for patients with at least one episode ‘for or with cancer’ – and thus it was only possible to make the broad cancer/non-cancer-related distinction at a population level. It is acknowledged, however, that at an individual level it may not be possible to make such a clear distinction between cancer-related and non-cancer-related health-service utilisation. Non-cancer-related acute health-care utilisation was shown to generally increase with age, but remained roughly constant regardless of time since diagnosis, indicating that it may be a good minimum measure of ‘background’ acute health-care utilisation. That said, there is higher non-cancer-related acute health-care utilisation in the first year following diagnosis, particularly among those with lung and colorectal cancer. This may be explained by the fact that some survivors may have had an emergency admission to hospital during which they were diagnosed with cancer. In addition, some genuine cancer-related hospital activity may not be coded as such in the HES.
The primary motivation for using a person-time approach in this analysis was the need to properly account for the length of time cancer survivors spent ‘at risk’ of hospitalisation during the period of analysis, and how this depended on both age and time since diagnosis. The person-time methods allowed a precise assessment of the influence of these variables on the amount of hospitalisation among cancer survivors. The number of days survivors spent admitted to hospital (per 100 person-days) provides a more revealing assessment of the burden of cancer on the health service than a count of the number of admissions. However, the limitation of this approach is that, as person-time is pooled for all survivors in the population, it provides only a measure of the mean health-service utilisation in the population of survivors and obscures the underlying distribution. For example, on average male survivors of colorectal cancer who were no more than 1 year from diagnosis in 2006 spent 9 days per 100 person-days admitted to hospital (equivalent to approximately one month per year); however, in reality, many such survivors spent no time admitted to hospital at all, whereas others spent more than 9 days per 100 as an admitted hospital patient. This variation in the intensity of hospitalisation across survivors of a similar age and post-diagnosis period is considered in Maddams et al (2011), which used a population person-time analysis to estimate the proportion of survivors with a low or high level of health-service utilisation, as well as those with none. It was shown that the underlying distribution of hospital activity is skewed towards those with no hospital activity, particularly in the period more than 1 year after diagnosis, and it should therefore be kept in mind that the mean number of days spent in hospital per 100 person days, as described in this paper, is largely influenced by the small number of survivors who have a very high level of hospital activity.
Another limitation of this approach when used to assess the burden of cancer on the health service is that each day of hospitalisation is treated equally and the variation in the burden presented by different types of admission and procedures is not taken into account. For example, some survivors will be admitted to hospital for routine observation and monitoring, whereas others will be admitted for complicated operations that consume large amounts of hospital resources and require intense periods of rehabilitation.
The majority of cancer-related health-service utilisation occurred during the first year following diagnosis, for all types of cancer studied. Most cancer patients receive some form of care or treatment as soon as possible after diagnosis, and thus it is perhaps unsurprising that this period contains a large amount of hospital activity. However, this study also shows that there is a significant amount of cancer-related health-service utilisation in the period 1–5 years after diagnosis, particularly among survivors of lung and colorectal cancers. This is no longer the initial treatment phase, but is indicative of the ongoing needs of cancer survivors.
The highest levels of cancer-related acute health-service utilisation were observed in survivors of the relatively poor prognosis cancers, but these differences largely disappeared more than 5 years after diagnosis. This indicates that the worse prognosis cancers required more intensive treatment regimes (including end-of-life care) in the short to medium term after diagnosis, but not in the long term.
Prostate cancer survivors, despite having lower levels of cancer-related acute health-service utilisation in the first year after diagnosis than those with colorectal, lung or breast cancer, actually had the highest levels five or more years after diagnosis (Figure 2). This effect is the result of the relatively high levels of hospitalisation among prostate cancer survivors aged over 70 years and five or more years from diagnosis (Figure 3). A more detailed investigation (not included here) showed that these survivors experienced a large amount of hospital activity recorded in the HES data with a non-cancer primary diagnosis code, but with prostate cancer recorded as one of the supplementary diagnoses, and it was largely these episodes that resulted in the relatively high number of days spent admitted to hospital (per 100 person-days) among this group, compared with equivalent survivors of other cancers. In the analysis, these episodes were considered to be ‘cancer related’ because cancer was recorded as one of the supplementary diagnosis codes in the HES data. However, the recorded primary diagnosis codes, together with the operation procedure codes, indicate that these episodes were not generally related directly to prostate cancer. For example, the most common procedure codes were endoscopic examinations of the bladder and urethral catheterisations of the bladder, and the most common primary diagnosis codes were for disorders of the urinary system. There are several physiological changes that occur in men as they get older and lead to alterations in lower urinary tract function, making urinary disorders in elderly men common (Dubeau, 2006; Griebling, 2008). Many prostate cancer survivors are likely to be closely monitored in urology clinics for many years after initial diagnosis – often an extended period of either ‘active surveillance’ or ‘watchful waiting’ is pursued, especially if the cancer is less aggressive and treatment is not immediately necessary (Cancer Research UK, 2010a). This may explain the greater hospital activity recorded among prostate cancer survivors over the age of 70 years many years after diagnosis, compared with male lung or colorectal cancer survivors – it is possible that the increased observation and monitoring of these survivors leads to a high level of urological intervention, which is only indirectly related to their prostate cancer diagnosis.
The patterns of cancer-related health-service utilisation by age, as described in Figure 1, must be viewed in the context of the findings presented in Figure 3. For example, older cancer survivors are more likely to be more than 1 year from diagnosis, compared with younger survivors, and this alone explains the apparent decreasing levels of utilisation as age increases among lung and colorectal cancer survivors. Acute health-service utilisation in the first year after diagnosis was generally highest in survivors aged over 70 years. Initial cancer treatment can be physically very arduous, particularly for older patients who may be more frail and suffering from comorbidities, resulting in more frequent and extended admissions to hospital. Particularly striking was the threefold increase in cancer-related acute health-service utilisation in the first year after diagnosis among prostate cancer survivors aged ⩾85 years compared with those aged 65–69 years (Figure 3). Similar, but not as significant, increases were observed among survivors of colorectal, lung and breast cancers. Since the early 1990s, the PSA test has increasingly been available (usually to men aged over 50 years of age) as a screening tool for prostate cancer, although in the UK no organised PSA screening programme is in place. This test is still controversial and considered to potentially result in overdiagnosis and overtreatment of prostate cancers that would otherwise never have become symptomatic (Barry, 2009; van Leeuwen et al, 2010). Recorded incidence and survival have, accordingly, greatly increased since the test's introduction (Evans and Møller, 2003; Cancer Research UK, 2010b, 2010c), as have the number of prostate cancer survivors (Maddams et al, 2009). Men diagnosed with prostate cancer over the age of 70 years are more likely to have symptomatic disease requiring intensive initial treatment compared with those aged 50–70 years who are more likely to have been diagnosed via the PSA test. Similarly, the observed lower acute health-service utilisation in recently diagnosed breast cancer survivors aged 50–70 years (the age range in which women are routinely invited to attend breast screening units in England (NHS Breast Cancer Screening Programme, 2011), compared with other age groups, reflects some of the benefits of early detection offered by the screening programmes.
This paper highlights the significant effect that time since diagnosis has on the average amount of hospitalisation experienced by cancer survivors. The majority of cancer-related admitted hospital episodes of care occurred in the first year following diagnosis (when initial cancer treatment takes place); however, there was also a significant amount of hospital activity in the period 1–5 years after diagnosis, particularly among survivors of colorectal and lung cancers, which is indicative of the ongoing consequences of cancer and its treatment. Other work has shown that the final year before death also contains significant amounts of hospitalisation of cancer survivors (Maddams et al, 2011). These findings help to understand the burden of cancer on the health service, but further work is still required to identify potential areas of unmet needs among cancer survivors.
References
Barry MJ (2009) Screening for prostate cancer – the controversy that refuses to die. N Engl J Med 360 (13): 1351–1354
Budescu DV (1985) Analysis of dichotomous variables in the presence of serial dependence. Psychol Bull 97 (3): 547–561
Cancer Research UK (2010a) Monitoring prostate cancer. http://www.cancerhelp.org.uk/type/prostate-cancer/treatment/monitoring-prostate-cancer (accessed 23 June 2011)
Cancer Research UK (2010b) Prostate cancer – survival statistics. http://info.cancerresearchuk.org/cancerstats/types/prostate/survival/ (accessed 23 June 2011)
Cancer Research UK (2010c) Prostate cancer – UK incidence statistics. http://info.cancerresearchuk.org/cancerstats/types/prostate/incidence/ (accessed 23 June 2011)
Carstensen B (2007) Examples and programs for splitting follow-up time in cohort studies. http://staff.pubhealth.ku.dk/~bxc/Lexis/ (accessed 23 June 2011)
Dubeau CE (2006) The aging lower urinary tract. J Urol 175 (3 Pt 2): S11–S15
Evans HS, Møller H (2003) Recent trends in prostate cancer incidence and mortality in southeast England. Eur Urol 43 (4): 337–341
Griebling T (2008) Urinary incontinence and voiding dysfunction in elderly men. Curr Bladder Dysfunct Rep 3 (4): 241–246
Klotz J (1973) Statistical inference in Bernoulli trials with dependence. Ann Statist 1 (2): 373–379
Maddams J, Brewster D, Gavin A, Steward J, Elliott J, Utley M, Moller H (2009) Cancer prevalence in the United Kingdom: estimates for 2008. Br J Cancer 101 (3): 541–547
Maddams J, Utley M, Moller H (2011) Levels of acute health service use among cancer survivors in the United Kingdom. Eur J Cancer 47 (14): 2211–2220
NHS Breast Cancer Screening Programme (2011) About breast screening. http://www.cancerscreening.nhs.uk/breastscreen/about-breast-screening.html (accessed 23 June 2011)
NHS Health and Social Care Information Centre (2010) HES User Guide. http://www.hesonline.nhs.uk/Ease/servlet/ContentServer?siteID=1937&categoryID=87 (accessed 23 June 2011)
van Leeuwen PJ, Connolly D, Tammela TLJ, Auvinen A, Kranse R, Roobol MJ, Schroder FH, Gavin A (2010) Balancing the harms and benefits of early detection of prostate cancer. Cancer 116 (20): 4857–4865
Acknowledgements
This paper is a contribution from the National Cancer Intelligence Network and is based on the information collected and quality assured by the regional cancer registries in UK (www.ukacr.org; www.ncin.org.uk). The Thames Cancer Registry in King's College London receives funding from the Department of Health (DoH) for England. The views expressed in the article are those of the authors and not necessarily those of the DoH. The Clinical Operational Research Unit receives funding from the DoH for England Policy Research Programme. This article is sponsored by Macmillan Cancer Support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Maddams, J., Utley, M. & Møller, H. A person-time analysis of hospital activity among cancer survivors in England. Br J Cancer 105 (Suppl 1), S38–S45 (2011). https://doi.org/10.1038/bjc.2011.421
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2011.421
Keywords
This article is cited by
-
Risk stratification of young adult survivors of cancer to estimate hospital morbidity burden: applicability of a pediatric therapy-based approach
Journal of Cancer Survivorship (2021)
-
Health care services use among long-term breast cancer survivors: a systematic review
Journal of Cancer Survivorship (2019)
-
Using routinely collected data to stratify prostate cancer patients into phases of care in the United Kingdom: implications for resource allocation and the cancer survivorship programme
British Journal of Cancer (2015)
-
Projections of cancer prevalence in the United Kingdom, 2010–2040
British Journal of Cancer (2012)
-
The National Cancer Survivorship Initiative: new and emerging evidence on the ongoing needs of cancer survivors
British Journal of Cancer (2011)