Abstract
Background:
The Sloane Project, an audit of UK screen-detected non-invasive carcinomas and atypical hyperplasias of the breast, has accrued over 5000 cases in 5 years; with paired radiological and pathological data for 2564 ductal carcinoma in situ (DCIS) cases at the point of this analysis. We have compared the radiological estimate of DCIS size with the pathological estimate of DCIS size. We have correlated these sizes with histological grade, specimen-handling methods, particularly the use of specimen slice radiographs, and the success or failure of breast-conserving surgery (BCS).
Methods:
The Sloane Project database was interrogated to extract information on all patients diagnosed with DCIS with complete radiological and pathological data on the size of DCIS, nuclear grade, specimen handling (with particular reference to specimen radiographs) and whether primary BCS was successful or whether the patient required further conservation surgery or a mastectomy.
Results:
Of 2564 patients in the study, 2013 (79%) had attempted BCS and 1430 (71%) had a successful single operation. Of the 583 BCS patients who required further surgery, 65% had successful conservation and 97% of them after a single further operation. In successful one-operation BCS patients, there was a close agreement between radiological and pathological DCIS size with radiology tending to marginally overestimate the disease extent. In multiple-operation BCS, radiology underestimated DCIS size in 59% of cases. The agreement between pathological and radiological size of DCIS was poor in mastectomies but was improved by specimen slice radiography, suggesting specimen-handling techniques as a cause.
Conclusion:
In 30% of patients undergoing BCS for DCIS, preoperative imaging underestimates the extent of disease resulting in a requirement for further surgery. This has implications for the further improvement of preoperative imaging and non-operative diagnosis of DCIS so that second operations are reduced to a minimum.
Similar content being viewed by others
Main
The clinical management of ductal carcinoma in situ (DCIS) of the breast remains problematic. The disease is thought to spread radially along the duct systems in the breast (Faverly et al, 1994; Vicini et al, 2001), and treatment demands a close cooperation between surgeons, radiologists and pathologists if the true size of the disease can be accurately assessed preoperatively. The radiologist will identify the mammographic abnormality, but crucially must help the surgeon by accurate measurement. The surgeon must meticulously orientate the surgical specimen to help the pathologist define the margins. It has been previously shown that there is a correlation between size of disease and the requirement for further surgery, underlining the need for accurate preoperative assessment (Vicini et al, 2001).
The Sloane Project (The Sloane Project, 2009), named in memory of the late Professor John Sloane, is a prospective UK audit of patients with screen-detected non-invasive carcinomas and atypical hyperplasias of the breast detected by the National Health Service Breast Screening Programme (NHSBSP). The audit started in 2003 with the aim of assessing the effect of current clinical management on the long-term outcome of patients. All the UK NHSBSP breast-screening units are encouraged to participate in the project, and 77 out of 95 (81%) of the UK screening units voluntarily submit the data. Each clinical specialty in a screening unit contributes profession-specific data relating to diagnosis and treatment using specially designed data collection forms. The data recorded include details of specimen radiology and orientation, the radiological and pathological size, and surgical margins. There is published guidance for the UK Breast Screening Programme on the optimal standards for specimen handling of the resected DCIS (Ellis et al, 2005). Further guidance is also available from the Sloane Project website (The Sloane Project, 2009).
The key problem in treating patients with DCIS is tumour-positive surgical margins after breast-conserving surgery (BCS), which is likely to be associated with residual DCIS and a high risk of local recurrence (Dunne et al, 2009). Prevention of local recurrence is the main issue in treating patients with a curable in situ carcinoma as half of these recurrences are invasive carcinomas (Silverstein et al, 1998). This underlines the value of accurate preoperative measurement to guide BCS.
This paper examines specifically the relationship between radiological and pathological size measurements, their relationship to DCIS grade, specimen-handling techniques (particularly specimen slice radiography) and whether BCS was successful as a primary procedure.
Materials and methods
The period of study covered all entrants to the Sloane Project from its inception in April 2003–December 2008 – over 5000 patients. All patients were screen-detected with an age range of 50–70 years and a screening interval of 3 years. Approximately 70% of the entered patients had either a missing pathological or radiological data form at the time of analysis with some overlap giving an initial study population of 3883 patients who had both pathological and radiological data forms. In total, a further1319 cases were excluded from the study for the following reasons: unpaired pathological/radiological measurements (644), atypical ductal hyperplasia and/or lobular in situ neoplasia alone or in combination with DCIS (304), inappropriate first operation recorded (e.g., axillary surgery only, therapeutic re-excision) (39), DCIS grade not recorded (28) or if a diagnostic biopsy was performed (304) and thus true pathological size was not assessable. There was an overlap between these groups. The 304 diagnostic biopsies with paired size data and in which DCIS grade was recorded were excluded from the main study but will be analysed briefly in the Results section.
The remaining 2564 cases on the database were interrogated to identify three groups of patients with pure DCIS who had either a single successful breast-conserving operation (n=1430), a mastectomy as a primary procedure (n=551) or further surgery (re-excision and/or completion mastectomy) because of failed primary BCS the first time around (n=583). These three groups were compared for radiological and pathological size agreement, DCIS grade and whether specimen slice radiography had been carried out. These groups were chosen because they allowed a clear comparison of factors associated with the success or failure of BCS and also case selection for mastectomy.
We do not have precise records of imaging technique but we estimate that >90% of patients will have received film-screen mammography with only a small percentage receiving computerised radiography or digital mammography. The Sloane Project radiology form enables bi-dimensional recording of the disease extent. The radiological size is the largest diameter on either the craniocaudal or oblique view. This measurement is taken after viewing the magnification views to look for subtle additional calcifications, but not usually directly measured from the magnification views. A minority of cases will have had full-field digital mammography at assessment and in these cases the measurements will have been done from electronic magnification of the standard views on a digital workstation. Measurements were not taken from specimen radiographs. Intraoperative radiographs were read by the surgeon but had no influence on the final determination of radiological size, which is a preoperative measurement. For the purposes of this study, the maximum recorded radiological size of either the length or the diameter of the lesion was used.
The pathological measurement of DCIS size includes both the primary excision and any additional disease found at subsequent re-excision or mastectomy. Screen-detected DCIS in the United Kingdom is graded by nuclear morphology alone, as guided by the NHSBSP Reporting Guidelines (Ellis et al, 2005).
Data analysis
Data were analysed using ‘Analyse it’ version 2.20 software for Microsoft Excel. Measurements of agreement between radiological and pathological sizes were assessed using Altman–Bland plots to compare the difference between two measurement techniques of a continuous variable (pathology and radiology in this study) (Altman and Bland, 1983; Bland and Altman, 1986). The differences between the two paired measurements are plotted against the mean of values obtained using the two techniques. The mean of the differences is calculated to give a measure of ‘bias’ of one technique over the other. This may be a positive or negative value. The differences between radiological and pathological paired measurements for the various subgroups were compared using the Mann–Whitney U-test. Comparisons of frequencies were made using the χ2-test. We defined an α-error for tests of significance at P=0.05.
Results
All cases
The distribution of DCIS grade in patients having one successful BCS operation, primary mastectomy and failed primary BCS groups is shown in Table 1. Overall, 67% of cases had high-grade disease, 26% intermediate grade and 7% low grade. Those patients who were offered mastectomy as a primary procedure had a higher incidence of high-grade disease (80%) than those who had successful primary BCS (60%) or unsuccessful primary BCS (71%). These differences between groups for high-grade DCIS are all highly significant (P⩽0.0001).
Specimen radiography by the surgeon was carried out in 1811 of 2564 (71%) cases. Overall, specimen slice radiography was carried out by pathologists in only 757 of 2564 (29%) cases. There was no difference in the use of specimen slice radiography between women having successful one-operation BCS or unsuccessful BCS (31 vs 32%). Of the one-operation mastectomy specimens, 22% had slice radiography. For all cases, pathologists who elected to X-ray specimen slices took more blocks than those who did not (one-operation BCS: median=12 vs 10 per case; one-operation mastectomy: 17 vs 13 per case; and two operations or more: 14 vs 10 per case). These differences are all highly significant (all P⩽0.0001).
Although 445 cases out of the original 3883 had large blocks taken as part of the specimen handling in the study population of 2564 cases, only 10 were subjected to this technique.
Patients undergoing a single BCS procedure
The agreement between median maximum radiological and pathological DCIS sizes was very close in successful one-operation BCS patients (12 mm vs 14 mm) (Table 2). The level of agreement was not affected by specimen slice radiography but was affected by the DCIS grade (overall difference: 2 mm in low-grade vs 1 mm in high-grade disease).
Patients undergoing a mastectomy as a primary procedure
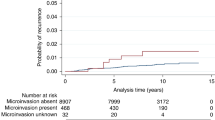
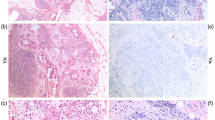
The agreement between radiological and pathological maximum DCIS size was less good in primary procedure mastectomy specimens with the overall median radiological size being 18 mm larger than the pathological size (50 mm vs 32 mm) (Table 2). The difference between radiological and pathological size increased with decreasing grade (15 mm for high-grade DCIS and 46 mm for low-grade disease). The level of agreement between radiological and pathological size was generally improved by specimen slice radiography (difference: 14 mm vs 17 mm for all cases) with the exception of low-grade DCIS in which the difference increased from 32 to 62 mm, but case numbers for this group were low. An example of an Altman–Bland plot for the primary mastectomy group is shown in Figure 1.
Altman–Bland agreement plot for primary mastectomies. The solid line shows the measure of bias (13.33 mm). The 95% confidence intervals refer to the differences between radiological and pathological measurements and are shown as broken lines. The colour reproduction of the figure is available on the html full text version of the paper.
Failed primary BCS – patients requiring re-excision or mastectomy
Of the 2013 patients who underwent BCS as a primary procedure, 583 (30%) required further surgery because of involved margins. Two-thirds of these 583 patients ultimately had successful breast conservation, the majority of these after a single further operation. One-third of these patients required mastectomy. These results are summarised in Table 3.
In this group of patients, who required subsequent re-excision in the form of additional breast conservation surgery or mastectomy, the radiological size of DCIS was significantly greater than the one-operation BCS group (P⩽0.0001). This is true for all histological grades (high grade: P=0.002; intermediate grade: P=0.03; low grade: P=0.02). The distribution of radiological sizes is shown in Figure 2. The radiological size of disease was also substantially less than that demonstrated pathologically (16 mm vs 23 mm) (Table 2). This mismatch was exaggerated in low-grade DCIS (15 mm vs 27 mm). Specimen slice radiography improved the agreement between radiological and pathological size (overall difference: 4 mm vs 7 mm). This effect was particularly marked for low-grade disease (7 mm vs 15 mm).
There was no difference in median specimen weight (55 vs 58 g). A record of whether radiological calcification was present or not was made in 2558 out of 2564 (>99%) cases. There was no significant difference between recorded calcification in the two conservation groups (92.0 vs 91.6%). We have not carried out a detailed review of the type of calcification recorded in this study. A representative Altman–Bland difference plot from this group is shown in Figure 3 demonstrating the negative measure of bias in this group.
Altman–Bland plot for agreement between radiological and pathological size measurements for all unsuccessful (2+operations) breast-conserving surgery (BCS) cases. Note that the measure of overall bias is now negative (mean: −6.46 mm). The 95% confidence intervals refer to the differences between radiological and pathological measurements and are shown as broken lines.
The trend of worsening agreement between radiological and pathological measurement of DCIS from conservation to mastectomy specimens, from high-grade to low-grade disease and from successful single BCS to failed primary BCS is underlined by the increasing Altman–Bland bias from one group to the next (Table 4).
Although the differences between radiological and pathological size at different grades within each group are not significant, the difference between the one-operation BCS (n=1430) and the failed primary BCS (n=583) groups as suggested by the polarised Altman–Bland plots is highly significant (P⩽0.0001). The differences between radiological and pathological sizes comparing the one-operation BCS group and the one-operation mastectomy group are also highly significant (P⩽0.0001) as is the difference between radiological and pathological sizes in the one-operation mastectomy and two-operation groups (P⩽0.0001).
Radiological–pathological size differences and the outcome of BCS
In the one-operation BCS group, 503 of 1430 patients (35%) showed a pathological DCIS size exceeding the radiological size compared with 343 of 583 (59%) in the failed BCS group. In all BCS cases in which pathological size exceeded radiological size, 59% were treated by a single operation, whereas those patients in whom radiological size exceeded pathological size, 79% were treated by a single operation. These differences are highly significant (P⩽0.0001). The percentage of all BCS cases treated by a single successful conservation operation grouped by size difference is summarised in Figure 4. When the pathological size exceeded radiological size by >30 mm, only 14% of patients received successful single-operation BCS, whereas when radiological size was the same or greater than pathological size, 80% of patients received successful single operation BCS. This overall pattern was not influenced by the DCIS grade. In those patients who underwent eventual successful breast conservation after an initial unsuccessful conservation procedure, 54% showed a radiological size that was less than the pathological size against 71% of patients who were finally treated by mastectomy. This difference is highly significant (P⩽0.0001).
Excluded graded diagnostic biopsies
Of the 304 diagnostic biopsies where data on histological grade of DCIS was available, which were excluded from the study, 126 (41%) had no further surgery, suggesting that these were in fact intended therapeutic procedures. There was a higher proportion (25%) of low-grade DCIS in this group than in the study group (7%) (P⩽0.0001). The data relating to this group are summarised in Table 5.
Discussion
For a patient to have a successful single breast-conserving operation for DCIS, there is a requirement for accurate preoperative mapping of the extent of disease. The bulk of this burden falls on the radiologists, although this can be improved by using targeted core biopsies to map the full extent of the DCIS. Furthermore, inserting localisation wires at either end of the area of DCIS may assist the surgeon undertaking the resection. This is particularly useful when both benign and malignant microcalcification are known to be present.
This study examines two methods of measuring the size of DCIS – radiological and pathological. We have used the Altman–Bland plot as the statistical technique to compare the differences between radiological and pathological size assessment. For each pair of data items, the Altman–Bland plot compares the difference between the two measurements with the mean of those measurements. It therefore focuses very closely on differences. The Altman–Bland bias is the mean of these differences. A bias value of 0 indicates no difference, whereas increasing values represent greater differences. The 95% confidence intervals are also calculated. In contrast, a correlation coefficient is a measure of the degree of association between two quantities; it does not measure how closely they agree. Its use in comparing two methods that claim to measure the same parameter is inappropriate. In this context, we have restricted our use of P-value calculations to the comparison of radiological–pathological size differences in the subgroups analysed and radiological size estimations in the two BCS groups and the comparison of some frequencies between categorical variables.
In those patients who had successful primary BCS, there is a close agreement between radiological and pathological DCIS size, both in terms of median values and the Altman–Bland measures of bias. At all grades, the bias is in favour of radiological size, with pathological size being marginally smaller. The greatest mismatch is for low-grade disease. This is likely to be due to less calcification being associated with this grade of DCIS (Evans et al, 1994; de Roos et al, 2007); however, we urge some caution against overinterpreting the data on low-grade disease because of the relatively small numbers of cases in these subgroup analyses. Screen-detected DCIS in the United Kingdom is graded by nuclear morphology alone, as guided by the NHSBSP Reporting Guidelines (Ellis et al, 2005). The overall incidence of low-grade DCIS in the present series was 7%. We excluded patients with recorded coexistent atypical ductal hyperplasia and/or lobular in situ neoplasia because of the potential for the extent of microcalcification to exaggerate the extent of DCIS. The incidence of low-grade DCIS is lower than that reported previously from an earlier cohort of this series (11%) (Thomas et al, 2008) and is partly due to the exclusion of cases with coexistent atypical ductal hyperplasia/lobular in situ neoplasia in this study group. This low incidence may also reflect the application of stringent diagnostic criteria for grading DCIS as a result of the ongoing comprehensive training programmes required for pathologists reporting NHSBSP screen-detected cancers, as well as the recognised preponderance of detection of high-grade DCIS in the NHSBSP.
In terms of successful BCS, a small radiological overestimate of the extent of disease will guide the surgeon appropriately with the likelihood that the DCIS in question will be excised completely by one breast-conserving operation. We acknowledge that overestimation of DCIS size radiologically could lead to unnecessarily extensive surgery, but our data show that in the successful primary BCS group the radiological overestimation of DCIS size is generally small (1–3 mm) and is therefore unlikely to be detrimental in this context.
Comparison between those patients who have had one-operation BCS and primary mastectomy shows a similar bias in favour of radiological size, but allows comment to be made on the accuracy of pathologists in determining DCIS disease extent under these circumstances. Accepting that the disease process is the same in the two types of operative specimen, and that the match between the radiological and pathological size in one-operation BCS specimens is very close, it is likely that specimen handling is the major reason for the difference in estimating DCIS extent in patients having a mastectomy. This view is supported by the improvement in radiological–pathological agreement when slice radiography is used, which holds true for all tumour grades and is particularly marked for low-grade disease. Pathologists are encouraged to make use of slice radiography for cases in which microcalcification is the principal feature and these data lend support to that view (Ellis et al, 2005).
In those cases in which BCS was unsuccessful, median pathological size is substantially greater than radiological size for all tumour grades. This is the reverse of the situation for successful one-operation BCS procedures. This is almost certainly due to diminished microcalcification in association with the DCIS in this group of patients, even though the crude statement on the Sloane Project radiology data form ‘No calcification on mammogram’ was answered in the negative in 10% of successful primary BCS cases and in only 7% of failed primary BCS cases. There is no significant difference in the median specimen weights for the two groups, indicating that the amount of tissue removed in the two groups were comparable. However, radiological size is, unsurprisingly, significantly greater in those cases in which initial BCS was unsuccessful compared with one-operation BCS cases, at all histological grades. In the group of patients who had an unsuccessful attempt at a single surgical BCS procedure, however, the larger radiological size described here, and the increased proportion of high-grade DCIS seen (71% compared with 60% in the successful one-operation group), is not sufficiently different to be able to guide the surgeon as to whether further imaging is required to map the extent of disease. It is apparent from our data that underestimation of DCIS extent radiologically need not necessarily lead to a failed primary conservation procedure. Surgical guidelines recommend re-excision for positive margins and we have made the assumption that these cases were disease free at the margins.
The meticulous studies of Holland et al comparing radiological and pathological disease extent indicated that radiology systematically underestimated DCIS size and run counter to the data presented here (Holland et al, 1990; Holland and Hendricks, 1994). Holland's series of cases from one surgical unit is very different from the wide cross-section seen in the Sloane Project; in the former series, there were much smaller numbers (83 and 119, respectively) and the specimens were all mastectomies. In our series, this radiological underestimation of DCIS size only applies to the subset of failed primary BCS cases (about 30% of conservation cases). The remaining 70% were surgically clear with a close agreement between radiological and pathological size.
Our data from primary mastectomies show underestimation of disease extent by pathologists who are, overall, unlikely to have emulated Holland's very detailed approach. A comparable study of 109 mastectomy specimens showed no significant difference between radiological and pathological measurements of DCIS extent (Sato et al, 2002). A more recent study of 174 cases of DCIS showed a correlation between increasing pathological–radiological size discrepancy and the requirement for more than one operation (Chakrabarti et al, 2006). That study failed to show a relationship between size discrepancy and grade, although case numbers were considerably lower than reported here. Ultimately the significance of these mismatches and the relevance of margin clearances will be resolved when outcome data (recurrence and survival) emerge for the Sloane Project cohort.
Although the Sloane Project pathology data form requests details regarding the cut-up method used by pathologists, there is no opportunity for the pathologist to describe his/her measurement technique. It is much easier to measure the size of a lesion in a wide local excision specimen because the sections can either be re-assembled like a jigsaw puzzle to give an overall size or large sections can be used that allow direct measurements. Such use of large block histology has been shown to improve the agreement between radiological and pathological lesion size (Jackson et al, 1994), but in this series there were insufficient cases following the various exclusions to be able to confirm this finding. Alternatively, the pathologist can relate the disease to its distance from margins and then calculate the extent from the overall dimensions of the specimen (Lester et al, 2009). It has also been suggested that the size may be estimated by the number of blocks containing DCIS multiplied by a factor, but a recent study has cast doubt on the accuracy of this approach (Dadmanesh et al, 2009). Inconsistency among pathologists in measuring DCIS extent has also been previously reported (Sloane et al, 1999).
We have not analysed the margin status or width in this study, believing this to be much more pertinent to a future analysis of the Sloane Project data examining outcomes, particularly local recurrences, when longer follow-up is available. The overwhelming majority of patients receiving a single successful conservation operation have negative margins, as defined by the particular centre. In some cases, a positive margin will not result in further surgery – most commonly anterior or posterior margins in full-thickness procedures. It should be appreciated that exactly what defines a negative margin (‘complete excision’) differs from centre to centre and that variation will itself enable an evaluation of optimal margin clearance when outcome data become available.
Are there any developments that could lead to a reduction of re-operation rates for DCIS? The College of American Pathologists has recently issued guidelines on specimen handling for DCIS that lay down stringent standards for this area of practice (Lester et al, 2009). These explicit recommendations are most likely to improve pathological assessment of disease extent and reproducibility of grade of DCIS and may improve detection of invasive disease. They will however do nothing to affect accurate preoperative assessment of disease extent, unless accompanied by the rigorous application of radiological–pathological size correlation of both operative and core biopsy specimens (e.g., if multiple cores are taken from areas of microcalcification with associated pathological–radiological mapping). More detailed discussion at the multidisciplinary meeting of the extent of calcification within the DCIS (in one or multiple core biopsies) can be correlated with how well the extent of disease is likely to be represented by the mammographic appearances, particularly in intermediate and low-grade DCIS. The use of wide-bore, vacuum-assisted, needle biopsy may also improve diagnosis and assessment in difficult cases (Pijnappel et al, 2004).
Studies have suggested that magnification views can aid the prediction of extent of low-grade DCIS (Asjoe et al, 2007; Di Saverio et al, 2008). Our data show that the size discrepancies leading to failed primary BCS occur across all tumour grades and that, numerically, low-grade disease is uncommon (<10% of cases). The overall impact of this approach to low-grade disease alone would therefore be small. Furthermore, it has been reported that the mammographic appearances do not correlate sufficiently with histological grade to assist preoperative identification of this subset of problem cases (de Roos et al, 2004). Histological reporting of the grade of DCIS in the core biopsy specimen, however, may prove of assistance in highlighting cases in which size discrepancy may be greatest, as core biopsy grade of DCIS has been shown to reflect the subsequent DCIS grade seen in surgical excision (Bagnall et al, 2001).
Recently, attention has been focused on the value of magnetic resonance imaging (MRI) in determining disease extent of DCIS. A number of recent studies have compared the ability of MRI and mammography to detect and size DCIS lesions. The results are conflicting; a number favouring MRI (Schouten van der Velden et al, 2006; Kim et al, 2007; van Goethem et al, 2007), another finding the performance of MRI and mammography were similar (Sardanelli et al, 2008) and yet another finding that the combination of mammography and MRI was significantly better than either of the modalities alone (Santamaría et al, 2008).
The main limitation of this study relates to the inevitable range of practice from centre to centre. Although this is minimised by the availability of practice guidelines that have been in place in the NHSBSP for the past 20 years, there is bound to be a degree of variability. We have not attempted to review the data from individual centres at this time because the numbers of cases from each centre will be too small to analyse, but this will be possible in the future as the Sloane Project case accrual grows and that will allow differences in practice to be compared against the outcomes. To minimise the effects of such variation, we have restricted our analyses to very broad groupings of cases with large numbers in each.
Conclusions
In a large series of screen-detected DCIS, we have shown that current approaches to preoperative imaging undersize the extent of disease in patients selected for BCS in up to 30% of cases, with the consequence of failed primary conservation surgery. Nevertheless, breast conservation can still be achieved in two-thirds of this group and by the second operation in 90% of cases.
Multidisciplinary team working is likely to have made a substantial contribution to effective management of breast cancer over the past 20 years and could be expected to have an impact on DCIS. Further improvements in preoperative assessment should include detailed discussion between surgeon, radiologist and pathologist about radiological–pathological size correlation, particularly the extent of colocation of microcalcification and DCIS. Our data suggest that such discussion should be particularly targeted at intermediate and low-grade disease.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Altman DG, Bland JM (1983) Measurement in medicine: the Analysis of Method Comparison Studies. Statistician 32: 307–317
Asjoe FT, Altinas S, Colpaert C, Marck EV, Vermorken JB, Tjalma WA (2007) The value of the Van Nuys prognostic index in ductal carcinoma in situ of the breast: a retrospective analysis. Breast J 13: 359–367
Bagnall MJ, Evans AJ, Wilson AR, Pinder SE, Denley H, Geraghty JG, Ellis IO (2001) Predicting invasion in mammographically detected microcalcification. Clin Radiol 56: 828–832
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1 (8476): 307–310
Chakrabarti J, Evans AJ, James J, Ellis IO, Pinder SE, Macmillan RD (2006) Accuracy of mammography in predicting histological extent of ductal carcinoma in situ (DCIS). EJSO 32: 1089–1092
Dadmanesh F, Fan X, Dastane A, Amin MB, Bose S (2009) Comparative analysis of size estimation by mapping and counting number of blocks with ductal carcinoma in situ in breast excision specimens. Arch Pathol Lab Med 133: 26–30
de Roos MA, van der Vegt B, de Vries J, Wesseling J, de Bock GH (2007) Pathological and biological differences between screen-detected and interval ductal carcinoma in situ of the breast. Ann Surg Oncol 14: 2097–2104
de Roos MAJ, Pijnappel RM, Post WJ, de Vries J, Baas PC, Groote LD (2004) Correlation between imaging and pathology in ductal carcinoma in situ of the breast. World J Surg Oncol 2: 4
Di Saverio S, Catena F, Santini D, Ansaloni L, Fogacci T, Mignani S, Leone A, Gazzotti F, Gagliardi S, De Cataldis A, Taffurelli M (2008) 259 patients with DCIS of the breast applying USC/Van Nuys prognostic index: a retrospective review with long term follow up. Breast Cancer Res Treat 109: 405–416
Dunne C, Burke JP, Morrow M, Kell MR (2009) Effect of margin status on local recurrence after breast conservation and radiotherapy for ductal carcinoma in situ. JCO 27: 1615–1620
Ellis IO, Pinder SE, Bobrow L, Buley ID, Coyne J, Going JJ, Humphreys S, Jasani B, Lakhani S, Lowe J, Miller K, Rhodes A, Walker RA, Wells CA . Pathology Reporting of Breast Disease. NHS Cancer Screening Programmes, (2005), Sheffield, UK
Evans A, Pinder S, Wilson R, Sibbering M, Poller D, Elston C, Ellis I (1994) Ductal carcinoma in situ of the breast: correlation between mammographic and pathological findings. Am J Roentg 162: 1307–1311
Faverly DR, Burgers L, Bult P, Holland R (1994) Three dimensional imaging of mammary ductal carcinoma in situ: clinical implications. Semin Diagn Pathol 11: 193–198
Holland R, Hendricks JH (1994) Microcalcifications associated with ductal carcinoma in situ: mammographic-pathologic correlation. Semin Diagn Pathol 11: 189–192
Holland R, Hendricks JH, Veebek AL, Mrarunac M, Schurmans Stekhoven JH (1990) Extent, distribution and mammographic-pathologic correlations of breast ductal carcinoma in situ. Lancet 335: 519–522
Jackson PA, Cook MG, Merchant W, McCormick CJ (1994) A comparison of large block macrodisectioning and conventional techniques in breast pathology. Virch Arch 425: 243–248
Kim do Y, Moon WK, Cho N, Ko ES, Yang SK, Park JS, Kim SM, Park IA, Cha JH, Lee EH (2007) MRI of the breast for the detection and assessment of the size of ductal carcinoma in situ. Korean J Radiol 8: 32–39
Lester SC, Bose S, Chen Y-Y, Connolly JL, de Baca ME, Fitzgibbons PL, Hayes DF, Kleer C, O’Malley FP, Page DL, Smith BL, Weaver DL, Winer E, for the Members of the Cancer Committee and College of American Pathologists (2009) Protocol for the examination of specimens from patients with ductal carcinoma in situ of the breast. Arch Pathol Lab Med 133: 15–25
Pijnappel RM, van den Donk M, Holland R, Mali WPThM, Peterse JL, Hendriks JHCL, Peeters PHM (2004) Diagnostic accuracy for different strategies of image-guided breast intervention in cases of nonpalpable breast lesions. Br J Cancer 90: 595–600
Santamaría G, Velasco M, Farrús B, Zanón G, Fernández PL (2008) Preoperative MRI of pure intraductal carcinoma – a valuable adjunct to mammography in assessment cancer extent. Breast 17: 186–194
Sardanelli F, Bacigalupo L, Carbonaro L, Esseridou A, Giuseppetti GM, Panizza P, Lattanzio V, Del Maschio A (2008) What is the sensitivity of mammography and dynamic MR imaging for DCIS if the whole-breast histopathology is used as a reference standard? Radiol Med (Torino) 113: 439–451
Sato M, Fukutomi T, Akashi-Tanaka S, Miyakawa K, Yamamoto N, Hasegawa T (2002) Accuracy in assessing tumour extension according to mammographic subtypes in patients with ductal carcinoma in situ. Jpn J Clin Oncol 32: 157–161
Schouten van der Velden AP, Boetes C, Bult P, Wobbes T (2006) The value of magnetic resonance imaging in diagnosis and size assessment of in situ and small invasive breast carcinoma. Am J Surg 192: 172–189
Silverstein MJ, Lagios MD, Martino S, Lewinsky BS, Craig PH, Beron PJ, Gamagami P, Waisman JR (1998) Outcome after invasive local recurrence in patients with ductal carcinoma in situ of the breast. JCO 16: 1367–1373
Sloane JP, Amendoeira I, Apostolikas N, Belklocq JP, Bianchi S, Boecker W, Bussolati G, Coleman D, Connolly CE, Eusebi V (1999) Consistency achieved by 23 European pathologists from 12 countries in diagnosing breast disease and reporting prognostic features of carcinomas. Virchows Archiv 434: 3–10
The Sloane Project (2009) Specimen handling protocols and reporting guidelines. http://www.sloaneproject.co.uk/ Accessed on 1 April
Thomas JS, Hanby AM, Pinder SE, Ellis IO, Macartney JM, Clements K, Lawrence G, Bishop HM (2008) Implications of inconsistent measurement of ER status in non-invasive breast cancer: a study of 1684 cases from the Sloane Project. Breast J 14: 33–38
van Goethem M, Schelfout K, Kersschot E, Colpaert C, Verslegers I, Biltjes I, Tjalma W, De Schepper A, Weyler J, Parizel P (2007) MR mammography is useful in the preoperative locoregional staging of breast carcinomas with extensive intraductal component. Eur J Radiol 62: 273–282
Vicini FA, Kestin LL, Goldstein NS, Baglan KL, Pettinga JE, Martinez AA (2001) Relationship between excision volume, margin status, and tumor size with the development of local recurrence in patients with ductal carcinoma-in-situ treated with breast-conserving therapy. J Surg Oncol 76: 245–254
Acknowledgements
The Sloane Project is indebted to Julietta Patnick, CBE through her support of the NHS Breast Screening Programme. We are grateful to Dr Gill Kerr, Senior Medical Statistician, Edinburgh University, for statistical advice. We are particularly grateful to all colleagues in the contributing Breast Cancer Screening Units of the UK, where there is a participation rate of over 80%. Without their continuing support and hard work contributing to the data, the work of the Sloane Project could not proceed. We are also indebted to our patients. We are grateful to the NHS Breast Screening Programme and the Breast Cancer Research Trust for financial support. The Sloane Project has previously been supported by Pfizer Pharmaceuticals. All funding sources, past and present, have had no input into the writing of this paper or the decision to submit it for publication. The Steering Group listed in the appendix give their time voluntarily to the Sloane Project.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
This paper was presented at the Spring Meeting of the Association of Breast Surgeons at BASO, York, 17 March 2009.
Appendix
Appendix
Membership of the Sloane Project Steering Group:
Mr Hugh Bishop, Consultant Surgeon, Royal Bolton Hospital, Bolton (Chair), UK.
Mr Rob Carpenter, Consultant Breast Surgeon, St Bartholomew's and the London Hospitals, London, UK.
Ms Karen Clements, West Midlands Cancer Intelligence Unit, Birmingham, UK.
Dr John Dewar, Consultant Clinical Oncologist, Ninewells Hospital, Dundee, UK.
Dr Hilary Dobson, Director, West of Scotland Breast Screening Service, UK.
Professor David Dodwell, Consultant Clinical Oncologist, Leeds Teaching Hospitals, Leeds, UK.
Professor Ian Ellis, Professor of Tumour Pathology, City Hospital, Nottingham, UK.
Professor Andrew Evans, Professor of Breast Imaging, Ninewells Hospital, Dundee, UK.
Professor Andrew Hanby, Consultant Breast Pathologist, St James’ University Hospital, Leeds
Ms Olive Kearins, West Midlands Cancer Intelligence Unit, Birmingham, UK.
Dr Gill Lawrence, Director, West Midlands Cancer Intelligence Unit, Birmingham, UK.
Mr Martin Lee, Consultant Surgeon, University Hospital, Coventry, UK.
Dr Anthony Maxwell, Consultant Radiologist, Royal Bolton Hospital, Bolton, UK.
Mr Stewart Nicholson, Consultant Surgeon, York Hospitals, York, UK.
Professor Sarah Pinder, Professor of Breast Pathology, Guy's and St Thomas’ Hospitals, King's College London, London, UK.
Mr Terry Roberts, West Midlands Cancer Intelligence Unit, Birmingham, UK.
Dr Jeremy Thomas, Consultant Breast Pathologist, Western General Hospital, Edinburgh, UK.
Dr Matthew Wallis, Consultant Radiologist, Addenbrooke's Hospital, Cambridge, UK.
Mrs Margot Wheaton, Programme Manager, Warwick, Solihull and Coventry Breast Screening Service, UK.
Participating Screening Units in the Sloane Project as per October 2009
Avon
Barking, Havering, Brentwood and Redbridge
Barnsley
Basingstoke and District
Bedfordshire and Hertfordshire
Bolton, Bury and Rochdale
Breast Test Wales – North
Breast Test Wales – South East
Breast Test Wales – South West
Cambridge and Huntingdon
Central and East London
Chelmsford and Colchester
Chester
City, Sandwell and Walsall
Cornwall
Crewe
Doncaster
Dorset
Dudley and Wolverhampton
East Berkshire
East Scotland
East Sussex
Gateshead
Gloucestershire
Great Yarmouth and Waveney
Greater Manchester
Hereford and Worcester
Humberside
Isle of Wight
Jarvis
Leeds and Wakefield
Leicestershire
Liverpool
Macclesfield
Maidstone
Medway
Milton Keynes
Newcastle-Upon-Tyne
Norfolk and Norwich
North and East Devon
North Cumbria
North East Scotland
North Lancashire and South Cumbria
North London
North Nottinghamshire
North Staffordshire
North Yorkshire
Northampton
Nottingham
Oxford
Pennine (Bradford)
Peterborough
Portsmouth
Rotherham
Sheffield
Shropshire
South Birmingham
South Derbyshire
South Devon
South East London
South East Scotland
South Essex
South Staffordshire
South West London
South West Scotland
Southampton and Salisbury
Warrington
Warwickshire, Solihull and Coventry
West Berkshire
West Devon and East Cornwall
West Essex and Redbridge
West London
West Scotland
Western Breast Screening Unit, Northern Ireland
Wiltshire
Wirral
Wycombe
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Thomas, J., Evans, A., Macartney, J. et al. Radiological and pathological size estimations of pure ductal carcinoma in situ of the breast, specimen handling and the influence on the success of breast conservation surgery: a review of 2564 cases from the Sloane Project. Br J Cancer 102, 285–293 (2010). https://doi.org/10.1038/sj.bjc.6605513
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605513
Keywords
This article is cited by
-
Accuracy of cone-beam computed tomography, digital mammography and digital breast tomosynthesis for microcalcifications and margins to microcalcifications in breast specimens
Scientific Reports (2022)
-
The characteristics associated with upgrade on surgical pathology of conventional imaging occult DCIS diagnosed by MRI
Breast Cancer Research and Treatment (2021)
-
Active surveillance of women diagnosed with atypical ductal hyperplasia on core needle biopsy may spare many women potentially unnecessary surgery, but at the risk of undertreatment for a minority: 10-year surgical outcomes of 114 consecutive cases from a single center
Modern Pathology (2018)
-
Performance characteristics of specimen radiography for margin assessment for ductal carcinoma in situ: a systematic review
Breast Cancer Research and Treatment (2017)
-
Impact of full-field digital mammography on pre-operative diagnosis and surgical treatment of mammographic microcalcification
Breast Cancer Research and Treatment (2014)