Abstract
Background:
There is evidence to suggest that diabetes may increase the risk of incidence and mortality from cancer.
Methods:
In a cohort study using record-linkage health-care datasets for Tayside, Scotland in 1993–2004, we followed up 9577 newly diagnosed patients with type 2 diabetes, and two matched non-diabetic comparators, in the national cancer register.
Results and conclusions:
The risk ratio for any cancer, adjusted for deprivation, was 0.99 (95%CI 0.90–1.09). Significantly increased risks were observed for pancreatic, liver and colon cancer.
Similar content being viewed by others
Main
Whether there was an increased prevalence of cancer associated with insulin use was questioned in the early twentieth century (Marble, 1934), and there is a growing body of evidence suggesting that diabetes increases the risk of the incidence and mortality from certain cancers. These include pancreatic and liver cancer, colorectal cancer, breast cancer, bladder cancer, cancer of the kidney and endometrial cancer (Wideroff et al, 1997; Coughlin et al, 2004; Rousseau et al, 2006; Kuriki et al, 2007). However, the results of studies of diabetes and cancer have been very mixed with many not distinguishing between type 1 and type 2 diabetes (Wideroff et al, 1997), or have defined groups according to treatment (Swerdlow et al, 2005). In some studies, the basis for diabetes diagnosis is self-report (Coughlin et al, 2004), in others it is clinical (Saydah et al, 2003). Studies have been both retrospective (Kuriki et al, 2007) and prospective, with some prospective studies following up from diagnosis of diabetes (Ragozzino et al, 1982); another followed up a cross-sectional sample of patients (Swerdlow et al, 2005). In this study, we present the risks of different cancers following diagnosis of type 2 diabetes in Tayside, Scotland, using a standardised methodology.
Materials and methods
This cohort study was carried out using the datasets of the Health Informatics Centre (HIC), University of Dundee, which developed the record linkage of routinely collected health-care datasets to facilitate epidemiological and other health research in the population of Tayside Health Board, Scotland (approximately population 400 000) (Evans et al, 1995). A diabetes clinical information system was used to identify all patients registered with any Tayside GP practice who were diagnosed with type 2 diabetes in 1993–2004 (Morris et al, 1997). Their date of diagnosis was defined as their study index date. Any patient who had an earlier record of cancer diagnosis on the Scottish national cancer registry (SMR6) was excluded (Scottish Cancer Registry, 2009).
For each eligible patient with type 2 diabetes, two non-diabetic comparators were selected at random from computerised lists of patients registered with primary care, matched for age (within 1 year), sex and GP practice. The index date of the comparator was that of its matched diabetic patient; and the comparator had to be alive and have no earlier cancer diagnosis on this date.
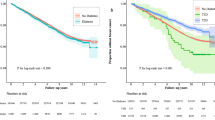
Diabetic patients and their comparators were followed for a maximum of 11 years in a survival analysis to the study end date (1st January 2004). The primary outcome was diagnosis of malignant cancer on SMR6; deaths were also identified. The relationship between type 2 diabetes and cancer was assessed in a Cox regression unadjusted, and then in a multivariable model adjusted for deprivation (measured using deciles of a postcode score for material deprivation) (Carstairs, 1990). This was repeated for specific cancer types according to the ICD10 diagnosis code recorded on SMR6.
Statistical analyses were performed using SPSS (Statistical Package for Social Scientist) 15.0 software programme. All data were anonymised for analysis. Ethical approval was obtained from the Multi-Centre Research and Ethics Committee for Scotland.
Results
The study population comprised 9577 people registered with any Tayside general practice diagnosed with type 2 diabetes between 1993 and 2004, and 19 154 non-diabetic comparators, of these, 53.3% were male, and the mean age at index date was 62 years; 661 (6.9%) of patients with diabetes were diagnosed with cancer, as recorded on SMR6, during follow-up (mean length of follow-up 1417 days), compared with 1364 (7.1%) of the comparators (mean follow-up 1476 days). Of the diabetic patients, 12.5% died and 8.3% of the comparators died.
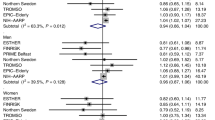
The unadjusted risk ratio for any diagnosis of cancer was 1.01 (95% CI 0.92–1.11) for diabetic patients. After adjusting for deprivation, it reduced to 0.99 (95% CI 0.90–1.09) (Table 1). Risk ratios were determined for specific cancers, presented in Table 1 in decreasing order of frequency (accounting for 79% of all cancers). There were significant increased risks associated with type 2 diabetes and of colon, pancreatic and cancer liver only. The results were largely unchanged after excluding outcomes in the first year of follow-up.
Discussion
This study finds no evidence that patients with type 2 diabetes have an overall increased risk of cancer compared with non-diabetic people, with adjusted risk ratios approaching unity. However, there was an increased risk of certain specific cancers that, because uncommon, did not have a substantial effect on the overall risk ratio.
Patients with type 2 diabetes were three times more likely to develop pancreatic cancer than non-diabetic people, a widely reported association (Coughlin et al, 2004; Rousseau et al, 2006; Kuriki et al, 2007). Although type 2 diabetes could be a risk factor for pancreatic cancer (Wideroff et al, 1997), it is more likely to be a consequence (reverse causality) (Gullo et al, 1994), being stronger among recently diagnosed patients. The three-fold increased risk of liver cancer is also similar to earlier reports (Wideroff et al, 1997; Rousseau et al, 2006), some of which have adjusted for confounding by alcohol and viral hepatitis (Davila et al, 2005). However, the risk is higher after excluding patients diagnosed in the year following diabetes, suggesting that reverse causality is unlikely to be the explanation here.
Our slight increased risk of 1.46 for cancer of the colon is in line with a recent meta-analysis (Larsson et al, 2005). Other studies have observed similar risks, some of which were not significant perhaps owing to small sample size (Wideroff et al, 1997; Coughlin et al, 2004; Rousseau et al, 2006). In contrast, we observed no increased risk for rectal cancer, consistent with the lack of statistically significant increased risk in the Nurses' Health Study (Hu et al, 1999).
This study provided no evidence for associations between type 2 diabetes and other cancer types. A Danish study found increased risks of kidney and endometrial cancer (Wideroff et al, 1997), these cancers were not common in our cohort and larger sample sizes would be needed to detect an associated risk. We also found no increase of breast or bladder cancer, despite a US finding of excess mortality (Coughlin et al, 2004). However, associations with mortality could be confounded by survival-related factors.
We are confident in the validity of our data sources, which have been widely used in epidemiological studies, whereas SMR6 is a national, validated dataset. It also allowed estimation of risks of cancer incidence, using precise dates of diagnosis. The study's main limitation was lack of information on lifestyle-related confounders, although we were able to adjust for deprivation. Patients with diabetes may have a higher prevalence of lifestyle-related risk factors for cancer, such as obesity (Hjartaker et al, 2008). However, we found no increased risks of many cancers despite these potential confounders, thereby increasing confidence in the conclusions.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Carstairs V (1990) Deprivation and health in Scotland. Health Bull (Edinb) 48: 162–175
Coughlin SS, Calle EE, Teras LR, Petrelli J, Thun MJ (2004) Diabetes mellitus as a predictor of cancer mortality in a large cohort of US adults. Am J Epidemiol 159: 1160–1167
Davila JA, Morgan RO, Shaib Y, McGlynn KA, El-Serag HB (2005) Diabetes increases the risk of hepatocellular carcinoma in the United States: a population based case-control study. Gut 54: 553–559
Evans JMM, McDevitt DG, MacDonald TM (1995) The Tayside Medicines Monitoring Unit (MEMO): a record-linkage system for pharmacovigilance. Pharm Med 9: 177–184
Gullo L, Pezzilli R, Morselli-Labate AM (1994) Diabetes and the risk of pancreatic cancer. N Engl J Med 331: 81–84
Hjartaker A, Langseth H, Weiderpass E (2008) Obesity and diabetes epidemics: cancer repercussions. Adv Exp Med Biol 630: 72–93
Hu FB, Manson J.E, Hunter D, Colditz GA, Michels KB (1999) Prospective study of adult onset diabetes mellitus (type 2) and risk of colorectal cancer in women. J Natl Cancer Inst 91: 542–547
Kuriki K, Hirose K, Tajima K (2007) Diabetes and cancer risk for all specific sites among Japanese men and women. Eur J Cancer Prev 7: 89–107
Larsson SC, Orsini N, Wolk A (2005) Diabetes mellitus and risk of colorectal cancer: a meta-analysis. J Natl Cancer Inst 97: 1679–1687
Marble A (1934) Diabetes and cancer. New Engl J Med 211: 339–349
Morris AD, Boyle DIR, MacAlpine R, Emslie-Smith A, Jung RT, Newton RW, MacDonald TM for the DARTS/MEMO Collaboration (1997) The diabetes audit and research in Tayside Scotland (DARTS) study: electronic record-linkage to create a diabetes register. Br Med J 315: 524–528
Ragozzino M, Melton III LJ, Chu CP, Palumbo PJ (1982) Subsequent cancer risk in the incidence cohort of Rochester, Minnesota, residents with diabetes mellitus. J Chron Dis 35: 13–19
Rousseau MC, Parent ME, Pollak MN, Siemiatycki J (2006) Diabetes mellitus and cancer risk in a population-based case-control study among men from Montreal, Canada. Int J Cancer 118: 2105–2109
Saydah SH, Loria CM, Eberhardt MS, Brancati FL (2003) Abnormal glucose tolerance and risk of cancer death in the United States. Am J Epidemiol 157: 1092–1100
Swerdlow AJ, Laing SP, Qiao Z, Slater SD, Burden AC, Botha JL, Waugh NR, Morris AD, Gatling W, Gale EA, Patterson CC, Keen H (2005) Cancer incidence and mortality in patients with insulin-treated diabetes: a UK cohort study. Br J Cancer 69: 2070–2075
The Scottish Cancer Registry. http://www.isdscotland.org/isd/3535.html. Accessed online 24th February 2009
Wideroff L, Gridley G, Mellemkjaer L, Chow WH, Linet M, Keehn S (1997) Cancer incidence in a population-based cohort of patients hospitalized with diabetes mellitus in Denmark. J Natl Cancer Inst 89: 1360–1365
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Ogunleye, A., Ogston, S., Morris, A. et al. A cohort study of the risk of cancer associated with type 2 diabetes. Br J Cancer 101, 1199–1201 (2009). https://doi.org/10.1038/sj.bjc.6605240
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6605240
Keywords
This article is cited by
-
Sex-specific clustering of metabolic risk factors and cancer risk: a longitudinal study in Iran
Biology of Sex Differences (2020)
-
The association between type 2 diabetes mellitus and bladder cancer risk among postmenopausal women
Cancer Causes & Control (2020)
-
Glycemic Status and Prognosis of Patients with Squamous Cell Carcinoma of the Esophagus
World Journal of Surgery (2017)
-
Influence of metabolic syndrome on upper gastrointestinal disease
Clinical Journal of Gastroenterology (2016)
-
Cancer incidence in patients with type 2 diabetes mellitus: a population-based cohort study in Shanghai
BMC Cancer (2015)