Key Points
-
Summarises the audit process and explains what an audit spiral is.
-
Highlights the benefits of an audit spiral to continually improve patient safety.
-
Summarises the potential issues of wrong site surgery within the current NHS framework.
-
Provides a sample audit spiral example which has been successful over five years.
Abstract
Introduction With an increasing demand to improve patient safety within the NHS, it is important to ensure that measures are undertaken to continually improve patient care. Wrong site surgery has been defined as a 'never event'. This article highlights the importance of preventing wrong tooth extraction within orthodontics through an audit spiral over five years investigating the accuracy and clarity of orthodontic extraction letters at the University Dental Hospital of Manchester.
Aims To examine compliance with the standards for accuracy and clarity of extraction letters and the incidence of wrong tooth extractions, and to increase awareness of the errors that can occur with extraction letters and of the current guidelines.
Method A retrospective audit was conducted examining extraction letters sent to clinicians outside the department.
Results It can be seen there has been no occurrence of a wrong site tooth extraction. The initial audit highlighted issues in conformity, with it falling below expected standards. Cycle two generally demonstrated a further reduction in compliance. Cycle three appeared to result in an increase in levels of compliance. Cycles 4 and 5 have demonstrated gradual improvements. However, it is noteworthy that in all cycles the audit standards were still not achieved, with the exception of no incidences of the incorrect tooth being extracted.
Conclusion This audit spiral demonstrates the importance of long term re-audit to aim to achieve excellence in clinical care. There has been a gradual increase in standards through each audit.
Similar content being viewed by others
Introduction
'Wrong-site tooth extraction' refers to the extraction of a tooth other than the one that was intended for extraction by the referring dentist.1 The National Patient Safety Agency (NPSA), in 2009/2010, issued a list of eight never events, describing a never event as, 'A serious, largely preventable patient safety incident that should not occur if the available preventative measures have been implemented by healthcare providers'.2 The annual publication by the Department of Health lists 25 'never events', describing these as 'unacceptable and eminently preventable'.3 Wrong-site surgery consistently remains the number one never event listed in this document.
Extraction of the incorrect tooth, which is an adverse event, is the most common reason for patients filing medico-legal claims within orthodontics.4 Most cases are preventable.1 There may be several reasons as to why the wrong tooth could be extracted, but specifically it may be linked to poor communication or miscommunication between colleagues, that is, dentists and other dentists or orthodontists.4,5 Mistakes can therefore be limited by improvements in communication, ensuring that correspondence pertaining to extractions is both clear and accurate. Guidelines have been produced by the British Orthodontic Society4 and advice offered by dental defence organisations to help ensure effective communication in extraction letters and avoid wrong tooth extractions.
Despite being seemingly underreported,6 the incidence of wrong tooth extractions remains higher than would be desired. Between 2006 and 2011 the DDU received 138 claims and opened 109 advice files involving allegations of erroneous extractions. Disappointingly, the number of instances of wrong tooth extractions is seemingly increasing, with 57 cases in 2011 compared with 21 in 2006.5 The financial cost of settling 56 claims was over £413,000, which is clearly substantial but could be preventable. One cannot overlook the potential psychological effects of losing a tooth, which can be significant, and even more so if it was the incorrect tooth.
A three-year study carried out in Taiwan between 1996 and 1998 showed the annual incidence for wrong tooth extractions to be 0.026% in 1996, 0.025% in 1997 and 0.046% in 1998.6 The authors concluded that the findings were largely due to lack of communication between the referring dentist and surgeon. Furthermore, a 2010 study of malpractice7 conducted to examine insurance claims from 1993 to 2004 for the wrongful extraction of a tooth found that 49% of referring clinicians were orthodontists. This highlights the importance of orthodontic referrals with regards to the part that they play in wrong tooth extractions.
Over the last 20 years clinical audit has developed to form an integral pillar of clinical governance. The initial inclusion of 'medical audit' within NHS healthcare was in 1989, outlined in the Government White Paper entitled Working for patients.8 Since then the National Institute for Clinical Excellence (NICE) has published Principles for best practice in clinical audit (2002). NICE have defined clinical audit as:
'A quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and the implementation of change. Aspects of the structure, processes, and outcomes of care are selected and systematically evaluated against explicit criteria. Where indicated, changes are implemented at an individual, team or service level and further monitoring is used to confirm improvement in healthcare delivery'.9
The process of clinical audit has been simplified by the diagram of the audit cycle as seen in Figure 1. This breaks the audit cycle down into five stages:
-
1
Identify the audit topic – based on a clinical problem or issue
-
2
Set the standard – usually based on a previously determined ideal
-
3
Collect the data – by observing clinical practice
-
4
Analyse the data and compare it to the standard
-
5
Implement change to clinical practice to allow an improvement.
The process of clinical audit can only become effective once the cycle is repeated, following implementation of recommendations with aims to improve clinical practice. Over a period of time, as the cycle is repeated, the process becomes a 'clinical audit spiral'.10
The University Dental Hospital of Manchester (UDHM) Orthodontic department first conducted an audit in 2009, examining departmental compliance with standards for the accuracy and clarity of extraction letters. The extraction letter is essentially a prescription sent back to the relevant clinician from the orthodontist, outlining which teeth require extraction as part of the orthodontic treatment plan. The audit has since been repeated on a yearly basis with the aim of monitoring and improving clinical practice with the goal to ensure patient care is safeguarded.
The results have formed part of the Central Manchester Foundation Trust Batch Safety Dashboard.10
Aims
The objective of this audit spiral was to assess if the department has seen an improvement in clarity and accuracy of its extraction letters. If there has been no improvement then further measures will need to be taken to ensure standards are met and to reduce the risk of extracting incorrect teeth.
The aims of all the audit cycles were to:
-
Examine compliance with the standards for accuracy and clarity of extraction letters
-
Examine the incidence of wrong tooth extractions – this should never occur
-
Increase awareness of the errors that can occur with extraction letters and of the current guidelines.
After cycle 2 of the audit the following aims were also investigated:
-
Identify whether the actions identified after the previous audit cycle have been successfully implemented, with a resultant increase in adherence to standards.
In the most recent audit, it was also assessed to see if the introduction of a standardised orthodontic extraction letter had improved standards.
Standards
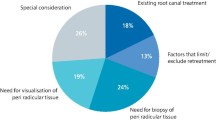
The audit standards are based on Orthodontic extractions risk management guidelines produced by the British Orthodontic Society4 and Dental Defence Union (DDU) Recommendations.5 Both sources stress the need for clear and accurate communication between healthcare professionals to help reduce the risk of an extraction error. They recommend that when communicating teeth to be extracted that they be referred to both in written long hand, and in a dental notation/abbreviation to avoid ambiguity.
Accuracy standards
-
100% of the time the patient details on the letter will be correct
-
100% of the time the teeth for extraction will be documented in the patient's notes
-
100% of the time the teeth for extraction documented in the extraction letter will correspond with the teeth documented in the patient's notes.
By aiming to achieve such standards it is hoped that the correct tooth is to be extracted in the correct patient, thus avoiding extraction errors. To ensure this the patient details should be accurately written in the correspondence to the dental professional undertaking the treatment and the teeth requested for extraction should be correct and correspond to the clinician's notes. When signing the letter the clinician should compare the extraction prescription to the notes to ensure that the two are consistent.
Clarity standards
-
100% of the time the teeth for extraction are clearly identifiable in the extraction letter
-
100% of the time the teeth for extraction are identified by dental notation and written in longhand.
The individual to whom the letter is addressed should be clearly able to ascertain which teeth are required for extraction. There should be no instances where the tooth is not easily identifiable, and to avoid this the teeth should be noted in full with words and with a dental notation/abbreviation.
Overall gold standards
-
There should be 100% overall compliance with the standards for accuracy and clarity of extraction letters
-
There should be no occurrences of wrong tooth extraction.
Materials and method
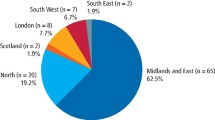
For all five audits, the same method has been used. A retrospective audit was conducted whereby a random sample of 80 extraction letters sent to clinicians outside the department, across all clinicians requesting extractions in the orthodontic department at UDHM, were identified from the secretarial letters database. The letters were cross-referenced with the patients' medical notes. A range of letters were sampled, aiming to capture information regarding all those who write them.
Over the five audit cycles, data has been collected by various specialty registrars, using the same clinical audit pro-forma within the orthodontic department and the medical records libraries at UDHM.
Summary statistics were employed to analyse the data, following which the information regarding the standards was compared to that gathered in previous audit cycles. No issues have been encountered with the methodology.
Results
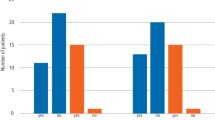
Results for all standards over the five audit cycles can be seen in Table 1. Most importantly it can be seen there has been no occurrence of a wrong site tooth extraction.
The initial audit highlighted issues in conformity, with it falling below expected standards, especially when examining standards relating to clarity of extraction letters. Cycle two generally demonstrated a further reduction in compliance. This led to further action, which in cycle three appeared to result in an increase in levels of compliance. Cycles 4 and 5 have demonstrated gradual improvements. However, it is noteworthy that in all cycles the audit standards were still not achieved, with the exception of no incidences of the incorrect tooth being extracted.
Table 2 demonstrates the distribution of different dental annotations used within extraction letters by the orthodontic team at the UDHM. From this it can be seen there has been an increase in uniformity in the documentation of teeth to be extracted over the five audit cycles.
Discussion
Wrong-site surgery and therefore wrong-site tooth extraction has been outlined as a 'never event' by the Department of Health and falls in the category of a 'serious untoward incident' (SUI).3 Following the publication of the 'serious incident framework' by NHS England, there is an increased need to acknowledge patient safety issues within the NHS. Frameworks have been outlined in the reporting and management of SUIs.11 The framework endorses the application of seven key principles in the management of all serious incidents. These stages are outlined in Box 1. There is a duty of candour to report any incidence of wrong site extraction to the Care Quality Commission under Regulation 20.12 Being highlighted as a serious event, wrong-site extraction could carry potentially significant consequences for the practitioners involved. It is therefore imperative that systematic processes should be implemented to avoid any occurrences of this. This has led to a comprehensive methodology being adopted for this audit, not only to check for incidences of wrong site extraction, but to ensure that all aspects of the correspondence relating to tooth extractions is clear and accurate.
This clinical audit spiral has been repeated on five occasions and it can still be seen that not all standards are being met, however, the most important factor is that there has been no incidence of wrong tooth extraction. There has been a gradual increase in standards through recommendations from each cycle. Due to the severity of the consequences of a potential wrong tooth extraction and its implication from a patient care perspective, it is important the department ensures they dictate clear and accurate prescriptions in the extraction letters. If a wrong tooth extraction was to occur, only by demonstrating 100% compliance to all standards would the department be able to ensure that they were not responsible for the error. Thus, the gold standards of 100% compliance to all standards is a necessity to ensure the risk of wrong tooth extraction is minimised and if this was to occur, then the medico-legal implication for the trust would be simplified.
After the initial audit cycle, it was agreed that the audit methodology was sound. It provided a range of orthodontic extraction letters to be analysed. By sampling 80 letters randomly from secretarial databases, this provided a range of orthodontic extraction letters to monitor these factors to ensure the methodology remains valid each year. In having the same methodology over the audit cycles, it has ensured that direct comparisons can be made between the results. The one addition to the audit methodology for future audit would be to remove the standard that there should be no incidence of wrong tooth extraction as, although the purpose of this audit is to ultimately prevent any wrong tooth extraction, this is not solely in control of the department. For example, if all protocols are followed and the extraction letter meets all standards for accuracy and clarity, it is still possible the clinician undertaking the treatment could extract the incorrect tooth. Thus, it is more appropriate for the standards to be limited to ensuring that all extraction letters meet the clarity and accuracy standards. Incidences of wrong tooth extraction should still be noted and reported in future audits.
The main recommendations from each audit cycle are shown in Figure 2. The first audit identified the wide variation in the way that teeth to be extracted were documented and this could be a source of confusion and thus subsequent errors could occur. From this cycle the main shortcoming was that clinicians were not prescribing teeth for extraction using two forms of notation. The results from this audit were disseminated to staff at a local departmental audit meeting. The second cycle failed to show significant signs of improvement. All standards were down in comparison to audit cycle 1 except for incidence of wrong tooth extraction. Upon investigation after this audit cycle, it was noted that there had been many new clinicians starting within the department who were unaware of the guidelines for extraction letters. The majority of the new clinicians were registrars and postgraduate trainees, who together dictated the greatest number of extraction letters. It was after this audit cycle, that wider discussion with all members of the orthodontic team including clinicians at all grades, nurses and secretaries were held, aiming to improve standards significantly. Following this cycle, it was decided to add this audit to the dental hospital patient safety dashboard. It was also decided to add extraction letter guidelines to the new starter packs given to clinicians upon induction to the department to ensure all clinicians are aware of the extraction letter guidelines. The need to provide education for all new members of the team has been further re-enforced over the five audit cycles. Significant changes were seen in audit cycle 3 and these have been built upon in the further cycles. However, the results indicate that all standards are not being met. After each subsequent audit cycle, the results were discussed at departmental audit meetings, with specific feedback given to groups of clinicians who dictated letters which did not meet standards. This would aim to prevent clinicians from repeating the same errors in future which could lead to wrong tooth extraction.
In the most recent audit cycle there was one incidence of the tooth for extraction not being documented with two forms of notation. An anoymised version of this letter has been included in Figure 3 It can be seen that this letter did not use the standardised extraction letter template. The standard extraction letter template can be seen in Figure 4. By outlining the teeth for extraction clearly with two forms of identification in a bullet point format, it is much easier for the treating clinician to identify which tooth requires extraction when referring to this template letter as opposed to the example shown in Figure 3. When required, clinicians are able to add more information within the standard template letter such as the orthodontic treatment plan. If additional information is included, the layout of the template letter stays such that the teeth for extraction are clearly bullet pointed within the letter under the separate sub-heading 'PLAN', and thus remain easy for the reading clinician to identify. An example of this can be seen in Figure 5, in which the standard template has been modified to allow more information regarding the treatment plan to be included.
There has been an emphasis on ensuring uniformity in the documentation of teeth to be extracted over the last three audit cycles. Introduction of a standard extraction letter has further increased this. An additional benefit of the standardised extraction letter is that it ensures there is a consistent approach to documenting teeth for extraction in long hand and with the same dental notation/abbreviation over all extraction letters. This provides a consistent structure for clinicians to follow to eliminate any potential areas of confusion when documenting teeth requiring extraction.
There has been a wider benefit of the audit cycles on the regional specialist orthodontic services. With many clinicians working in other primary and secondary care units, they have implemented similar good processes in their respective practices and hospitals. This has led to a reduction in risk to other patients in the wider region.
Conclusion
Wrong site surgery is defined as a serious untoward incident by NHS England and thus it is important to ensure measures are in place to prevent this from occurring. This audit spiral demonstrates the importance of long term re-audit to aim to achieve excellence in clinical care. By repeating this over several years and implementing the recommendations from each audit cycle, there has been a gradual increase in standards through each audit. By undertaking this process over an extended time frame, it has been possible to make improvements with the overall aim to safeguard patient care and improve patient safety.
References
Lee J, Curley J, Smith R . Prevention of Wrong-Site Tooth Extraction: Clinical Guidelines. J Oral Maxillofac Surg 2007; 65: 1793–1799.
National Patient Safety Agency. Never Events Annual Report 2009/2010. NHS. Available at http://www.nrls.npsa.nhs.uk/neverevents/?entryid45=83319 (accessed June 2017).
NHS England Patient Safety. Never Events List 2015/2016. Available at https://www.england.nhs.uk/wp-content/uploads/2015/03/never-evnts-list-15-16.pdf (accessed June 2017).
Development and Standards Committee of the British Orthodontic Society. Advice Sheet 12: Orthodontic extractions risk management guidelines. British Orthodontic Society 2001.
DDU. Rise in extraction error claims reports DDU. 2013. Available at https://www.theddu.com/press-centre/press-releases/rise-in-extraction-error-claims-reports-ddu (accessed June 2017).
Chang H, Lee J, Cheng S et al. Effectiveness of an educational program in reducing the incidence of wrong-site tooth extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004; 98: 288–294.
Peleg O, Givot N, Taicher S et al. Wrong tooth extraction: root cause analysis. Quintessence Int 2010; 41: 869–872.
Department of Health. Working for patients. London: The Stationery Office, 1989.
National Institute for Clinical Excellence. Principles of best practice in clinical audit 2002. Abingdon, Oxon: Radcliffe Medical Press, 2002.
Ashley M P, Pemberton M N, Saksena A, Shaw A, Dickson S . Improving patient safety in a UK dental hospital: long-term use of clinical audit. Br Dent J 2014; 217: 369–373.
NHS England. Serious Incident Framework. Supporting learning to prevent recurrence. 2015. Available from http://www.england.nhs.uk/wp-content/uploads/2015/04/seriousincidntframwrk-upd.pdf (accessed February 2017).
Care Quality Commission. Regulation 20: Duty of candour. 2015. http://www.cqc.org.uk/sites/default/files/20150327_duty_of_candour_guidance_final.pdf (accessed June 2017).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Anwar, H., Waring, D. Improving patient safety through a clinical audit spiral: prevention of wrong tooth extraction in orthodontics. Br Dent J 223, 48–52 (2017). https://doi.org/10.1038/sj.bdj.2017.586
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.586
This article is cited by
-
Improving the reporting of orthodontic clinical audits: an evaluation
British Dental Journal (2021)