Key Points
-
Provides an overview of the profile of entrants to dentistry.
-
Informs dental practitioners who may have school children seeking work experience in preparation for application to dental school.
-
Encourages reflection on how we can encourage access to dental education for young people from under-represented areas.
Abstract
Aim To compare trends in the volume, socio-demography and academic experience of UK applicants and entrants to medicine and dentistry in the UK with university in general, before and after the major increase in university fees in England in 2012.
Methods Descriptive trend analyses of University and College Admissions Services (UCAS) data for focused (preferred subject was medicine or dentistry) and accepted applicants, 2010-14, compared with university in general in relation to socio-demography (age, sex, ethnicity, POLAR 2, region) and academic experience (school type). POLAR2 data provide an indication of the likelihood of young people in the area participating in further or higher education.
Results In 2012 the volume of applicants to medicine and dentistry fell by 2.4% and 7.8% respectively, compared with 6.6% for university overall. Medical applications remained buoyant and by 2014 had risen by 10.2% from 2010 to 23,365. While dental applications fell in both 2012 and 2013, they had increased by 15.6% to 3,410 in 2014, above 2010 levels. Females formed the majority of applicants, and admissions, with the proportion gaining admission to dentistry in 2014 reaching an all-time high (64%), exceeding medicine (56%), and university in general (56%). Mature admissions to dentistry were at their highest in 2010 (29%) falling to 21% in 2014, compared with 22-24% in medicine. Black and minority ethnic group admissions to university, although rising (24% in 2014), are still less than for medicine (34%) and dentistry (48%). In 2013, just over half of the students admitted to dentistry were from BME groups (51%) for dentistry. Among UK applicants <19 years, over 60% of applicants, and 70% of accepted applicants, to medicine and dentistry are from the top two POLAR2 quintiles representing areas of high participation in education; however, in 2014 there was a notable increase in the proportion of applications from the lower two quintiles to dentistry (19%) and medicine (20%), with a very modest increase in those gaining admission over 2012 (14% of both; cf 10% and 12% respectively).
Discussion The findings suggest that the short-term impact of the 2012 rise in fees had a greater influence on the volume and nature of applicants to dentistry than medicine, and that both programmes are gaining in popularity, despite high fees and reduced places. Dentistry remains particularly attractive to Asians, and females, the latter forming an increasing majority of students. While there is some recovery, social inequalities exist and present a challenge for widening participation in the professions.
Similar content being viewed by others
Introduction
Over half of current dentists will have had the enormous privilege of enjoying dental education 'free at the point of delivery' within the United Kingdom. This was one of the benefits of our welfare state under the 1944 Education Act.1 Many will also have enjoyed the benefit of receiving a grant to cover living expenses while attending university; thus leaving with little, or no, debt. Significant public sector reform means that this is no longer the case across much of the UK, with implications for individuals, the profession and society.
Firstly, it is important to note that although the vast majority of third level education in the UK continues to be provided through state/public universities, private establishments, very common in other parts of the world, are now emerging in the academic marketplace.2,3
Secondly, gaining a university degree is increasingly important, and expected, in our knowledge-based economy.4 Government policy promotes third level education, with a target that half of young people should go to university, whilst back in 1945 only 3% attended university.5 Education costs money and someone has to pay, with loans available, and for certain students NHS bursaries in the final year.6 Contemporary neoliberalist political philosophy suggests that students value what they pay for;7 and now they do pay for much of their medical and dental education.8
Thirdly, all governments of whatever shade have supported this change. University tuition fees were introduced in the UK in 1998 by a Labour government at a rate of up to £1,000 per annum. While intervening years brought an increase in fee cap to £3,000 in 2006, with small inflationary rises, a subsequent coalition government permitted a dramatic increase in fees to a maximum of £9,000 per annum from 2012 onwards in England and Wales.9 Fees in Northern Ireland have remained at just over £3,000 plus inflation, while the fees in Scotland (£1,000 plus inflation) are paid by the Student Awards Agency for Scotland;10 hence, students in Scotland do not pay fees. Students in Wales may apply for a fee grant of up to £5,190, which is not repayable, and thus in reality they pay similar levels of fees to Northern Ireland.
The rise to £9K fees resulted in concerns regarding the volume and demography of applicants, in particular those applying from disadvantaged backgrounds. All medical and dental schools in England and Wales elected to charge £9,000 fees and, in turn, had to demonstrate widening participation initiatives to ensure that applicants from disadvantaged backgrounds were encouraged, and supported, to enter university;11,12 this includes schemes such as outreach, national scholarship programmes (NSPs) as well as academic and pastoral support for current students. It is yet to be established whether these schemes are effective.
UK students apply to higher education through a central administrative system run by the Universities and Colleges Admissions System [UCAS], and may select up to five programmes of study. Students applying to medicine and dentistry are restricted in their choice and must make at least one alternative selection. Applications, where the majority of options relate to medicine or dentistry, are referred to as focused applications. Summary information on applications to medical and dental school is available online from UCAS and more detailed data may be purchased for research purposes. UCAS reported a steady increase in the number of applicants to all UK higher education (HE) courses from 2008, with an average increase of 8.8% per annum. In 2012, however, there was a fall of 7.4% in applicants across the UK.13
Medical and dental places are currently capped nationally, and thus competition for entry is present. Numbers of places, having expanded in the noughties,14,15 are now reducing at different rates in each of the devolved UK nations, and the number of graduate entry places has also reduced. In order to protect the economic viability of dental schools, more international entrants are increasingly permitted with Northern Ireland leading the way in recruiting from Malaysia. Previous analysis has established relationships between ethnicity, sex, maturity, social status and school type and an increased probability of acceptance to either medicine or dentistry.16,17 Fair admissions to higher education have been the subject of ongoing debate,18,19,20 and the Minister for Universities and Science has just challenged universities to increase access to higher education among white boys from lower social backgrounds.21,22
UCAS no longer collect information on social status based on socio-economic group (SEG) based on parental occupation and instead publish POLAR (Participation Of Local AReas) data. The latter classification is used by the Higher Education Funding Council [HEFCE] to identify how likely young people applying from different areas of the United Kingdom are to participate in further or higher education (FE/HE) and is regularly updated. This classification has five quintiles with POLAR category 1 being the areas with the least participation through to POLAR category 5, the areas with the highest participation rates.
It is imperative we monitor whether rising fees are inhibiting applicants from varied backgrounds in applying to medicine and dentistry nationally in support of tackling societal inequity. By ensuring that the dental and medical workforce is comprised of individuals with varying demographic characteristics we may be better able to provide appropriate care to a population that is both living longer and becoming increasingly diverse.
Aim
The aim of this study was to compare the demography (age; sex; ethnicity; region) and academic experience (school type; tariff) of focused and accepted applicants (entrants) to medicine and dentistry undergraduate programmes in the UK with university in general, before and after a major increase in university fees in 2012.
Methods
University and College Admissions Services (UCAS) admissions data were obtained, for focused and accepted applicants to medicine and dentistry across the five entrance years 2010-14. Information obtained for all applicants included age and sex. Additional information on ethnicity, school type, POLAR2 category and region (based on postcode of application) was obtained for all UK applicants.
Individual student data are not available for analysis from 2012 onwards; thus, limiting the level of analysis possible. Summary data on all dentistry and medicine programmes were obtained from UCAS and compared with online data for universities and colleges overall.23 Univariate analysis involved comparing proportions of focused and accepted applicants for medicine, dentistry and university overall for each of the variables. In 2014 to further protect student anonymity, there is rounding of student numbers to the nearest '5' of the data sent from UCAS, making trend analysis less precise.
Results
Volume of applications
Table 1 presents the data on applications and admissions from 2010 to 2014. In 2012 the total volume of applicants to medicine and dentistry fell by 2.4% for medicine and 7.8% for dentistry compared with 6.6% for university overall. Medicine showed the least fluctuation across the five years of admissions, 2010-14; having had an increase in focused applicants in 2011 (n = 21,721), and by 2014 applications had risen by a further 10.2% over 2012 levels to 23,365. In contrast dentistry saw a more marked a decline in focused applicants between 2011(n = 3,197) and 2012 (n = 2,949), and a further fall of 1.6% to 2013 (n = 2,902); however, they increased in 2014 by 15.6% over 2012 levels (n = 3,410).
Age
The proportion of mature focused applicants to both medicine and dentistry (>21 years of age) remained relatively stable over the five years with approximately one third of applicants to both courses reported as mature (∼31% to dentistry, and ∼33% to medicine) which is higher than university overall at 26%; however, the proportion of accepted applicants to dentistry decreased from a high of 29% in 2011 to 20% in 2013 and 21% in 2014, while the proportion of accepted medical counterparts remained more stable at 23-24% (Table 1).
Sex
A greater proportion of focused applicants to medicine were female (55-57%), as were accepted applicants (53-56%) (Table 1). However, even higher proportions of focused applicants to dentistry were female (55-61%). Accepted applicants to dentistry were consistently more likely to be female than focused applicants and their medical, or university, counterparts. This increased over time: whereas in 2012 and 2013, 61% were female, by 2014 this had risen to an all-time high of 64%, notably exceeding medicine and university overall (56% for both).
Ethnicity
When UK admissions are considered, medicine and dentistry attract applicants from a variety of ethnic backgrounds but with a distinctly different profile to university overall over the five-year period (Table 2). The proportion of white students applying to medicine has decreased from 61% to 56% and to dentistry from 43% to 39%, with a corresponding rise in BME [Black and minority ethnic group] applicants.
Furthermore, the proportion and volume of students from black and minority ethnic groups accepted to medicine increased between 2010 and 2014 (25% n = 1,780 compared with 28% n = 1,910 respectively). While in medicine this increase is most pronounced in the Asian constituent who rose to 22% in 2014, dentistry has been consistently popular among Asians with 41% in 2013. In 2013, for the first time, just over half of UK accepted applicants to dentistry (51%) were from black and minority ethnic groups (Table 2).
When compared with university admissions overall, it would suggest that Asians are twice as likely to be represented in medicine (22%) and three to four times as likely in dentistry (36-41%), with black and white students under-represented compared with university overall.
The proportion of black applicants to dentistry decreased over the five years from 115 applicants in 2010 to just 85 applicants in 2013, rising to 135 in 2014; however, the number of accepted applicants was low even in 2014 when BME admissions were highest (2%, n = 25). Black students applying to dentistry appear to have been most affected and Asian students applying to medicine least affected by the 2012 fee changes. While 7% of students accepted to university were of black ethnicity in 2014, the corresponding levels for medicine and dentistry were 3% and 2% respectively.
School type
There were major changes in school type during this period which makes comparative analysis difficult. The general trend is a decrease in the number of applicants from grammar and state schools (excluding grammar). However, this fall may be accounted for by the increase in applicants from academies which only emerged from 2012 onwards (Table 3).
Country/region
The proportion of applicants from different regions within England has remained relatively constant during the five-year period (Table 4). The proportion of applicants to university from London (16-17%) is consistently higher than the rest of the country, and notably so for medicine (23-24%) and dentistry (22-23%).
The proportion of accepted students from London was at its highest in 2014 (17%), while admissions to medicine (18%) and dentistry (19%), were slightly higher, they were lower than the level of applications.
The proportions of accepted applicants to medicine from Scotland, Northern Ireland and Wales have not shown significant change during the same period; albeit the numbers have dropped. For dentistry the proportions and number fluctuate over the five-year period and numbers overall are down, except for Wales which appear to have risen from 2011.
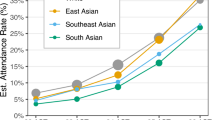
POLAR2
Medicine and dentistry attract considerably higher proportions of applicants from 'areas of higher participation in FE/HE' (Categories 5 and 4), than those from areas of lower participation (Fig. 1). Over the five years, high proportions of applicants to dentistry (63-66%) and medicine (64-67%) are from the upper two quintiles, and even higher levels of admissions: dentistry (70-75%) and medicine (71-74%).
The data for 2014 suggest that applications from areas of low participation have just risen in 2014 for dentistry and medicine (to 19% and 20% respectively), with admissions slightly lower at 14% for both. A caveat for this year is of course the rounding up/down of numbers to the nearest five which can make a difference when small numbers are involved.
Discussion
This paper provides an important insight on the socio-demographic profile of the future medical and dental workforce during a period of reduced medical and dental places, increasing student fees, promotion of widening participation activities, and a background of economic recession. Dentistry appears to have recovered, and medicine to have retained, popularity despite the university fee increase to £9k pa in England and Wales. The odds of gaining admission to study dentistry are still fairly good, at 3:1 overall. Dentistry is now admitting a higher proportion of females than ever and thus males are increasingly under-represented, even more so than for university as a whole. Universities have been challenged to address the under-representation of white males,21,22 and these findings present a particular challenge for dentistry where white and black students are underrepresented. Admissions to medicine and dentistry from areas of 'low uptake of education' reduced in line with the fee increase, but appear to be recovering, albeit that the volume of students from such areas is lower than before, calling into question whether the widening participation agenda can go beyond counteracting the impact of fees to widen access to medical and dental education.
The aim of widening participation strategies is to encourage anyone with the ability to participate in higher education with an opportunity to do so.24 While three decades ago, there were concerns that women were in the minority, it is now men who require active encouragement to participate in higher education, particularly the professions. The new imbalance between males and females is becoming more notable in dentistry and the possible influences and implications should be considered. Could it be in some way related to NHS policies which mean that most graduates will have less hope of running their own business in future, particularly in England and Wales as corporate bodies and contract ownership means that most can only hope to be employees or work for others as associates? There is some evidence that males are significantly more likely than females to be attracted by the ability to run a business.25 Additionally UK dentistry may be a more attractive career option for women due to the potential of flexible and more social working hours, and the potential for 'work-life balance' and 'financial stability'.26,27,28 All have implications for future workforce capacity.
Interestingly, while graduate applications have remained stable, graduate places, have reduced with two schools converting their graduate entry places to the standard five-year programme. This may be responsible for the notable reduction in mature students entering dentistry in 2013 and 2014, compared with 2010.
The ethnic group most affected by the rise in fees appears to be black students. This issue warrants monitoring and action by local dental schools in their widening participation activities to target under-represented groups, and may be informed by further research. In contrast, Asian applicants to university just exceed their proportion in the 18–19-year-old population overall at 11% (cf 9%), the volume of applicants and entrants is over four times higher for dentistry and over twice for medicine. Black and white students are under-represented among both focused and accepted applicants to medicine and, to a greater extent, in dentistry.
Both the dental and medical professions provide long-term career stability with a variety of employment options; a feature which is particularly attractive in times of economic recession. There are, however, implications for student debt which is a major issue for university entrance among low-income and working class backgrounds.20 Fees differ in each of the UK countries with students outside of England paying lower or, as in the case of Scotland, no fees. It could have been expected that these applications would remain constant but they decreased in 2012. This could be explained by the fact that Scottish students receiving education at home do not pay fees and can apply for a means-tested bursary for assistance with living costs. They have to pay fees if they go to university elsewhere, although they are able to apply for a means tested bursary.29 So if they can't, or don't want to, stay at home, students who might otherwise have applied for dentistry in Scotland, may possibly be opting for shorter alternative courses elsewhere in the UK. Similar issues may be occurring among students from Northern Ireland who pay reduced fees at home or in Scotland but full fees in England.
It is important to note that the proportion of admissions to medicine and dentistry from areas of 'low uptake of education' is much worse when compared to the proportion in university overall. The proportion decreased further in line with the fee increase but appears to be recovering. This can be explained by potential students being deterred by fees for programmes which last five or even six years with implications for long-term debt. Further action is required in order to ensure that individuals with the ability to pursue careers in medicine and dentistry are given the support and access they need, regardless of their ability to pay. As the system of loans and grants becomes increasingly complex, it is important that prospective students are aware of the additional grants and financial support available to those from low-income backgrounds, in particular in their UK country of origin and how to apply. Given well-documented social challenges of young people from low income backgrounds entering medicine,30 and university in general,20 research is required into the social and economic challenges of entering dentistry, and action should go beyond a knowledge deficit model and address the environment within which individual life choices are embedded.30
The limitations of this analysis are first our inability to have access to individual data in order to undertake multivariate analysis, due to new restrictions on the data available from UCAS; second, changing categories/coding of data which challenge any trend analysis; and third, the rounding up and down of the data from each school make robust analysis difficult. Nonetheless readers can see very clear patterns within the data upon which we as a profession should reflect, and act, as they have implications for the future medical and dental profession and wider society. The long-term population trends shows that the decline in young population is set to continue until 2021, with the number of 18- to 20-year-olds projected to decrease by 12.3% between 2012 and 2021.31 We should be actively encouraging the brightest and best into dentistry.32
Answering the question posed: yes the introduction of fees did impact on admissions to dental school, numerically and demographically, particularly for dentistry. While there is some recovery, social inequalities exist and present a challenge for widening participation in the professions.
References
UK Parliament. Education Act London: HM Government; 1944. Available online at http://www.parliament.uk/about/living-heritage/transformingsociety/livinglearning/school/overview/educationact1944/ (accessed January 2017).
The City of London Dental School. The City of London Dental School 2016 (accessed 19 March 2016).
University of Buckingham. Medical School 2016. Available online at http://www.buckingham.ac.uk/medicine (accessed January 2017).
Temple P (ed). Universities in the knowledge economy: Higher education organization and global change. Oxon: Routledge, 2012.
Shattock M . Making policy in British higher education. Maidenhead: Open University Press, 2012.
Guide TCU . University tuition fees 2016. Available online at http://www.thecompleteuniversityguide.co.uk/university-tuition-fees/ (accessed 19 April 2016).
Ward S C (ed). Neoliberalism and the global restructuring of knowledge and education. London: Routledge, 2012.
UK Government. Student finance 2016. Available online at https://www.gov.uk/student-finance/overview (accessed 19 April 2016).
UK Government. Student finance: UK Government 2016 Available online at https://www.gov.uk/student-finance (accessed 19 March 2016).
The Complete University Guide. Going to University in Scotland 2016 [19.03.2016]. Available online at http://www.thecompleteuniversityguide.co.uk/university-tuition-fees/going-to-university-in-scotland/ (accessed 19 March 2016).
Office of Fair Access. How to produce an access agreement for 2014-15. London: OFA, 2013.
Office of Fair Access. 2006–2007 Strategy for access and student success. London: OFA, 2006.
Independent Commission on Fees. Analysis of UCAS applications for 2012/13 admissions. London: Independent Commission on Fees, 2012.
Secretary of State for Education. Medical schools: Delivering the doctors of the future. London: Department of Education and Skills, 2004.
Secretary of State for Health. Reforms with bite – 1000 more dentists by October 2005. London: Department of Health, 2004 Reference No 2004/0265.
Gallagher J E, Niven V, Donaldson N, Wilson N H F . Widening access? Characteristics of applicants to medical and dental schools, compared with UCAS. Br Dent J 2009; 207: 433–445.
Niven V, Cabot L B, Gallagher J E . Widening participation - a comparison of the characteristics of successful UK applicants to the five-year and four-year dental programmes in 2007 and 2008. Br Dent J 2013; 214: 117–122.
Schwartz S . Fair admissions to higher education: recommendations for good practice. 2004.
Burke P J (ed). The right to higher education: beyond widening participation. London & New York: Routledge, 2012.
Sitich A E, Freie C . The working classes and higher education: Inequality of access, opportunity and outcome. New York and London: Routledge, 2016.
Department for Business, Innovation & Skills, Jo Johnson MP and Office for Fair Access. Universities told to reach out to students from poorest neighbourhoods under new guidance [press release]. 2016.
Johnson J . Letter of Guidance from the Secretary of State for Business, Innovation and Skills and the Minister of State for Universities and Science to the Director of Fair Access. London: UK Government, 2016.
UCAS. UCAS Undergraduate analysis reports 2015. Available from: https://www.ucas.com/corporate/data-and-analysis/ucas-undergraduate-releases/ucas-undergraduate-analysis-reports (accessed 24 January 2016).
Department for Business, Innovation & Skills, UK Government. Widening participation in higher education 2015. Available online at https://www.gov.uk/government/collections/widening-participation-in-higher-education (accessed January 2017).
Gallagher J E, Patel R, Donaldson N, Wilson N H F . Why dentistry: a quantitative study of final year dental students' views on their professional career? BMC Oral Health 2007; 7: 7.
Gallagher J E, Clarke, W, Eaton, K, Wilson N H F. Dentistry – a professional contained career in healthcare: a qualitative study of vocational dental practitioners' professional expectations. BMC Oral Health 2007; 7: 16.
Gallagher J E, Clarke W, Eaton K, Wilson N H F . Vocational dental practitioners' views on healthcare systems: a qualitative study. IADR; New Orleans, 2007.
Gallagher J E, Clarke W, Eaton K A, Wilson N H F . A question of value: a qualitative study of vocational dental practitioners' views on oral healthcare systems. Prim Dent Care 2009; 16: 29–37.
Council S F . Higher education students and qualifiers at Scottish Institutions 2013-2014. Edinburgh: SFC, 2015.
Greenhalgh T, Seyan K, Boynton P . “Not a university type”: focus group study of social class, ethnic, and sex differences in school pupils' perceptions about medical school. BMJ 2004; 328: 1541.
Universities UK. The funding environment for universities, 2014: Trends on undergraduate recruitment. Universities UK, 2014.
Gallagher J, Wilson N (eds). C U @ Dental Skl. 2nd ed. London: Stephen Hancocks Limited, 2012.
Acknowledgements
The authors wish to acknowledge the data provided by UCAS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
In relation to conflict of interest, three of the authors (JG, VN and LC) are involved in dental education and admissions interviews to dental school. Dr Lyndon Cabot is the lead for dental admissions at KCL. JEG is chair of the Dental Workforce Advisory Group for England; the views expressed in this paper do not represent the views of Health Education England.
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Gallagher, J., Calvert, A., Niven, V. et al. Do high tuition fees make a difference? Characteristics of applicants to UK medical and dental schools before and after the introduction of high tuition fees in 2012. Br Dent J 222, 181–190 (2017). https://doi.org/10.1038/sj.bdj.2017.122
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.122
This article is cited by
-
Economic burden of becoming a dentist in Thailand
BDJ Open (2023)
-
Recruitment and retention in dentistry in the UK: a scoping review to explore the challenges across the UK, with a particular interest in rural and coastal areas
British Dental Journal (2023)
-
Widening Access: what do dental school websites signal to prospective students?
British Dental Journal (2023)
-
Student debt of UK dental students and recent graduates
British Dental Journal (2023)
-
Journey towards a dental career: the career decision-making journey and perceived obstacles to studying dentistry identified by London's secondary school pupils and teachers
British Dental Journal (2023)