Key Points
-
Highlights that climate change will negatively affect health service provision.
-
Warns that resources may become scarce due to extreme weather events causing supply and transport problems, which may cause costs in dentistry to rise
-
Suggests that dentists need to plan for resilience against reduced resources.
-
Highlights the financial benefits to efficient and environmentally safe use of resources and rationalisation of waste.
Abstract
Objective To understand the attitudes and behaviour of staff in dental practice towards adopting a reduce, reuse, recycle approach to resource management.
Design A qualitative interview study.
Setting The site for the study was a mixed NHS/private dental practice in North Devon.
Subjects All disciplines from one dental practice.
Methods (1) A practice scoping exercise – provided context and identified an interview sample. (2) Qualitative interviews with practice staff – explored knowledge and attitudes about sustainability and identified opportunities and limitations for the sustainable management of resources.
Results The main issue raised by staff was the amount of waste generated. There was a strong desire to implement changes, but deep concerns were expressed about the impact of challenging current guidance on infection control.
Conclusions Primary care dentistry provides both surgical and non-surgical care to more than half the UK population. Therefore, lessons learned from general dental practice can encourage positive change. More research is needed across dental practice in order to generalise these findings.
Similar content being viewed by others
Objective
Primary dental care services form a significant element of NHS provision; in England these cost in the region of £3.6bn per year.1 Primary care dental practitioners provided 39.8 million courses of treatment in 2013/14.1 The reach of dental services is considerable with 29.9 million patients being seen over the 24 months up to June 2014 (56% of the total population).2 There is increasing emphasis on infection control and quality of care in dental practices, however, the wider impact of this focus in primary dental care services, particularly in relation to the environmental impact, remains poorly understood and is rarely investigated. Dental practices use a more extensive variety of materials and instruments than many other health care services which adds unique aspects to our investigations.
There are certain general environmental regulations that apply to any business (including dental practice) in the UK.3 Moreover, dental practices (similar to other businesses) are encouraged to take a socially responsible approach to the delivery of health services. A few years ago, primary care dentists requested an evidence review about how to minimise the environmental impact in their practice.4 The evidence review did not identify any well-conducted studies which evaluated the environmental sustainability of dental practices nor what lead to unsustainable practice.5 Despite increased interest in this topic, there is a clear uncertainty around the nature of the problem, factors contributing to it and best approaches to address them.
This lack of an understanding of the nature of the problem needs to be addressed. Qualitative research offers an opportunity to explore and understand the views and behaviours of people6 and as such is valuable as a starting point in developing an evidence base from one dental practice. Although the results of qualitative research cannot be generalised, the themes identified through analysis of the data offer an indication of the questions a larger study might ask in order to fully understand the factors inhibiting and enabling sustainable practice.
This qualitative study explored knowledge and awareness of sustainability in one dental practice, in North Devon. We collected data on the day to day running of the dental practice along with interviews with all the staff in the practice. This provided context information for the second quantitative part of the study where we piloted and evaluated an innovative approach to conduct a waste audit.7
Design
A qualitative approach was used to explore the knowledge and attitudes of staff in dental practice towards sustainability, and their understanding of reduce, reuse, recycle approaches to resource use.
The purpose of collecting qualitative data was to get a more in-depth understanding8 of the barriers to, and potential for, sustainable resource management in a dental practice.
The data collection was in two parts:
-
1
A practice scoping exercise – provided context to the study and identified an interview sample representing all staff employed by the practice
-
2
Qualitative interviews with practice staff – assessed the current knowledge in the practice and the opportunities and limitations in relation to resource management.
These methods have been tested in recent research by the Sustainability Society and Health Research Group (SSHRG) at Plymouth University on NHS procurement.9
Setting and subjects
The site for the study was a mixed NHS/private dental practice in North Devon. In order to ensure maximum variation in the sample, all members of the practice from all disciplines were invited to take part in the interviews. Table 1 provides an overview of the staff who agreed to be interviewed. The male/female mix is a reflection of the staff in the practice; there being many more females than males employed.
Ethical approval
Activities took place using the code of practice for research developed through Plymouth University's Faculty of Health and Human Sciences Research Ethics Committee. All data collected was anonymised to protect the participants and maintain confidentiality. Patients were aware of researchers in the building.
Data collection
Staff were fully informed of the details and purpose of the project. An information sheet was provided to all staff with contact details should they need further information from the researchers. The researchers visited the practice to discuss dates, times and processes and to clarify that the information gathered was not focused on individual behaviour, but on how to improve learning in the practice.
A reflective log noting any issues that impacted on study design or practical issues of data collection was maintained throughout the study period. This was used to make any necessary revisions to inform a possible larger study involving a more diverse range of dental practices.
To gather background and context information a scoping exercise (Table 2) was undertaken to collect data about the day to day running of the practice. This involved gathering information about staffing levels, procurement practices and costs. This process was important as it served to identify questions which could be used in the topic guide for the qualitative interviews.
Semi-structured qualitative interviews were carried out with members of the practice from different disciplines. Interviews were conducted using a topic guide, which was developed as a result of the scoping exercise and previous research.10 Interviews explored:
Knowledge and awareness of climate change and the need for sustainable behaviours
The opportunities and limitations for sustainable dental practice.
All participants who agreed to be interviewed signed a consent form; all names were changed to protect the participants' identities. Data were stored on a password protected computer. Interviews lasted between 30-45 minutes and were digitally recorded. First the participants were asked two questions about their knowledge and understanding of climate change and sustainability and then specific questions were asked about their behaviour in the practice, and they were encouraged to raise any concerns or ideas they had about these issues.
Data analysis
Thematic content analysis8 was used to analyse the transcripts from the qualitative interviews with practice staff. Initial codes were identified by repeated reading of the transcript. Codes were discussed in a project meeting and a framework developed to allow for further analysis.
Minimising the risk of bias
The focus of the study was the use and disposal of dental consumables and not an examination of treatment so the potential for bias was reduced. All data was thematically analysed and coded by two members of the research team. An audit trail was kept for all aspects of the project.
Results
Part 1: scoping exercise
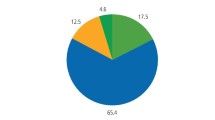
Both quantitative and qualitative data were collected. The quantitative data concerned the number and type of staff; the number and types of clinical sessions; demographics and mission statement; and the financial cost of materials and waste removal. Of relevance to this study was that since 2010:
-
Turnover increased by 13% but profitability decreased by 3%; overall expenses increased by 18%; material costs (including consumables) increased by 14%
-
Waste removal costs increased by 58% (predominantly due to increased production).
The practice manager and one dentist were asked about how decisions were made in the practice with regard to materials purchasing and waste management:
-
Purchasing – historical purchasing from a suppliers list
-
Decision making – decisions are affected by the training, experience and the perception of clinical need of the clinicians. The practice manager provides a summary of the direct and indirect costs and material usage. Monthly ordering enables strict stock control and reduces waste from items going out of date
-
Current waste arrangements - policies are written by the dental nurses who manage the waste. Once the stock arrives the cardboard waste is removed first and sent for recycling. Clinical waste is removed at the end of each day and general waste is left for the council waste collectors
-
Training – all staff have mandatory training annually (for example, hand washing, waste management). Bi-monthly training sessions and, every six months, basic life support (bls) medical emergency training.
Meetings – bi-monthly clinical meetings; monthly partnership meetings.
Part two: qualitative interview results
The interviews contained two sections. First, all participants were asked about their knowledge and attitudes toward climate change and sustainability. Previous research carried out by the NHSSDU (now SDU)11 suggested that health services should aim to achieve 'Values (that) are redefined to encompass health and wellbeing linked to an acceptance of finite resources.' Current opinion focuses on the need to manage resources through a reduce, reuse recycle approach. It seems that identifying increased and more frequent extreme weather events as the result of climate change, or using the word sustainability, has created uncertainty with the tendency towards inaction as a result. We were interested in ascertaining whether approaches to sustainable resource management were motivated by either, a general understanding of the link between the overuse of vulnerable materials and the resultant effect on climate, or whether staff simply followed rules without considering the reason why vulnerable materials needed to be managed. The participants interviewed for this study expressed a range of attitudes from interest to denial and some participants had decided to avoid resource management because of the lack of a uniform approach and clear guidance.
In the second section questions focused on insights into the interest, willingness and motivations toward potential behaviour change. The results presented here do not have identifiers attached because of concern about confidentiality in such a small participant group.
Section one: attitude to climate change
The participant responses in this study reflected the range of negative to positive attitudes previously noted in other research.12 For example:
'I don't really know, not convinced one way or another [sic].'
'We are not in touch with our natural roots anymore living in houses that are heated.'
Those whose attitudes are reflected in the first quote tended to be uninterested or unconvinced about the links between climate change and its link to resource management, whereas those with a commitment to the natural environment related their resource management at home to that at work and were very aware of the link.
Section one: sustainability
Most participants recycled the waste required by the council. Some felt that they needed more information about what and how to recycle at home. A few participants grow their own vegetables and bring the surplus to work to share. These participants were the most concerned about climate change and the need to live sustainably. All participants were asked about their motivations for recycling at home and the responses were related to their interest in sustainability:
'We have a compost heap and recycle cardboard and all the usual things and I have pigs. They are great at recycling! [...] we have chickens. I do it because its normal and I don't like waste'.
'Because I have to - I don't really think about the environment really and I am naughty sometimes'.
Current opinion focuses on the need to manage resources through a reduce, reuse recycle approach.10 Participants were also asked about why some people did not recycle. Some said:
'People don't think where the waste is going as long as it's gone from their house in a black bag they don't think about it.'
While others had decided to avoid or ignore advice because of the lack of a uniform approach and clear guidance.
'So I think that's where the confusion comes from and I'm not entirely sure that's a definitive answer. HTM01-05 is a best practice guidance document but three people can read it and come up with six different ideas. Some things are definite, this is the temperature you sterilise at, this is what you should be doing, but lots of the others are in between areas'
Section two: opportunities and limitations for sustainable practice
All the participants were aware of the recycling of paper, cardboard and plastic that takes place at the practice although some had no idea what happened to it when it left the practice. There were also conflicting views about the degree to which recycling was discussed with some saying it was discussed and decisions made while others said it was never discussed.
Those who were making the positive comments were the same people who were making the positive comments about recycling. This suggests that people who do recycle discuss the issue and those who have no interest are not engaged in the conversation.
There were several key issues that emerged from the transcripts:
Perception of conflicting guidance
In a qualitative study conducted with health service managers12 participants described their concern and confusion about guidance in relation to clinical waste and indicated their frustration where infection control policies seemed to conflict with waste management. In this study regulations which directly relate to the practice of dentistry had a profound influence on the behaviour of the staff, and this was most evident in relation to infection control.13 The senior staff voiced frustration at the perceived burden of unnecessary regulation, but recognised that despite their protestations they had little alternative but to comply.
'We do try to change it [how the guidance is prepared], we don't get anywhere, but you do have to try. There was quite a lot of resistance to HTM01-05 to begin with, but that didn't seem to make any difference. I would hope we can change it.'
The senior staff recognised there was confusion and blamed the guideline's lack of flexibility and clarity:
'HTM01-05 is a best practice guidance document but three people can read it and come up with six different ideas.'
More junior staff described how they just follow the procedure. They might think that there was unnecessary waste, but the concern about the preparation for and the visits of the Care Quality Commission's (CQC) inspections was tangible:
'I am only getting information from a book and I don't know if I am doing it right. It would be so nice to know how we can reduce our clinical waste. The clinical waste is always an issue because we haven't the space to store it.'
More specific confusion related to the fact that everything in the practice rooms was considered clinical waste, (including paper forms, sterile wrapping and tissues not used in treatment) despite the fact that there might be potentially infectious material outside the rooms too:
'Anything that leaves the clinical area has to go into clinical waste so that if I blew my nose that tissue would have to go into clinical waste whereas at home I'd just put it in the bin. I don't get the difference.'
It was explained to the researcher that the reason why everything was treated as clinical waste was because of the potential for contamination through droplet infection. However there were inconsistencies:
'So in theory you shouldn't have a fan when it's hot in summer because that is moving the contaminated air around and everything that contaminated air comes into contact with is in theory [...] contaminated and therefore should be treated as clinical waste.'
When asked about the reasons why staff followed orders and didn't question potentially unnecessary behaviours the responses were clear:
'Fear of 'getting it wrong' – when we had the CQC come round I was absolutely bricking it.'
As in previous research,11 information about what constitutes clinical waste was often provided by the waste contractors themselves. There may, therefore, be a perverse incentive among some waste contractors to encourage the use of clinical waste bags over more economical forms of waste disposal.
There also seemed to be uncertainty among staff about when to wear non sterile gloves and how they should be disposed of. For example, in the sterilising room there was awareness of the need to avoid unnecessary cross contamination:
'I get through so many gloves. I don't touch any clean instruments after I have touched dirty so I have to think about how I do things.'
In other areas staff commented that they put on gloves 'automatically' for every task from cleaning to treatment. The concern seemed to come from how to dispose of gloves appropriately when they had been used:
'Everything that goes into a surgery goes to clinical waste except things like our boxes from our gloves we recycle them not in clinical– they contradict themselves massively. If I dry my hands on a towel in the surgery it goes to clinical waste but if I use one upstairs in the bathroom it goes to general waste.'
Ideas for change
Staff had various areas they wanted more information on and more opportunity to discuss current practice:
'I think there needs to be a discussion to get things into perspective, eg what is the risk of cross contamination from two metres away if it goes into general waste. What is the risk to the general public?'
The bagging of instruments was a particular area of concern and participants felt they would like to challenge current procedure in the practice. Evidence for the amount of waste produced because of repeated bagging of instruments is shown in the waste audit results published elsewhere.8 Reduction in bagging could have a significant effect on the amount of waste paper and plastic wrap produced from each treatment session and would have a significant impact on staff time costs:
'I would like some independent person to come in and say these things need to be bagged and these things don't need to be.'
There was also general concern about the amount of cardboard that arrived at the practice and one participant felt it could be managed better in collaboration with the suppliers:
'They could send it in crates that we would send back the following week and pick up the wrapping at the same time.'
There was a degree of enthusiasm for gaining a green credential for the practice, but ultimately the sense of being constrained and almost oppressed by the infection control guidelines and the CQC meant that until they were provided with new information about what to do when, or encouraged to challenge how the guidelines had been written, the status quo would be maintained and reduce individual autonomy in practices.
Conclusion
The role of primary care dentistry in providing both surgical and non-surgical care to more than half the population means that any lessons learned from general dental practice have the potential to highlight areas which might impact resource management. In addition, this could provide a useful starting point for translation to a wide range of other health service settings.
Various strategies can be implemented to support a more environmentally sustainable approach within dentistry by embracing the three R's – reduce, reuse and recycle. One of the specific areas highlighted repeatedly within the interviews, was the amount of sterile wrapping being thrown in clinical waste bags. It was generally assumed that this situation was generated by the introduction of the HTM01-05 infection control guidelines.9 The interview study identified a strong desire to implement changes, but deep concerns were expressed by the staff about potentially undertaking actions to reduce waste within the clinical setting. This was related to the concerns over audit1 and the potential for being the 'one who let the practice down', should an individual be identified for not having followed guidelines. At no point in the interviews was there an indication that there was a lack of awareness of current infection control guidelines. What appeared to be concerning was how those guidelines were interpreted by some members of staff despite having discussed them with the Care Quality Commission directly. Contradictory messages came from the CQC audit visits and from the waste removal contractors. Staff talked of their uncertainty and anxiety and this was true of all grades both clinical and administrative. It is suggested that this issue needs to be reviewed with some urgency and either sterile packaging is removed before treatment is started, and therefore discarded in a general waste bag, or use re-usable packaging which can be re-sterilised at the end of the treatment session.
Clear guidance is also needed on how and when gloves are really needed, as the interviews suggested that gloves were put on 'automatically' for every task from cleaning to treatment. An awareness and understanding of appropriate glove use would enable a further reduction in waste. This need to 'think before you act' is also valuable in the use of paper tissues which was mentioned in relation to their disposal inside and outside the clinical areas. All paper tissues that come into contact with body fluids must be disposed of in the clinical waste bin. But tissues used for general cleaning may not need to be, and regular discussions among practice staff which lead to jointly made and agreed decisions may allay some of the current anxiety. This is an area explored in greater detail through a study on waste audit published in a subsequent article.7
There are few manufacturers offering 'green' products, so carbon reduction can be achieved by accessing products with fewer travel miles. Dentists could work with manufacturers to identify more re-useable products; increasing demand may prompt the manufacturers to identify further products which could be produced more sustainably. Negotiations about a reduction in packaging is also seen as essential and, as suggested by one member of staff, manufacturers could remove the cardboard on delivery or deliver items in re-useable plastic crates.
Based on the findings from the scoping and qualitative interviews, the following steps, specifically related to the dental practice used in the study, are recommended:
-
1
Review current purchasing and identify whether some items could be bought closer to the practice
-
2
Work with local manufacturers to improve packaging
-
3
Encourage discussion among staff about internal processes
-
4
Invite infection control experts and waste management companies together to discuss safe working practices
-
5
Revisit the interpretation of current guidance about all items inside treatment rooms being regarded as clinical waste
-
6
Reduce packaging of sterile instruments
-
7
Reduce tissue and glove use.
References
CQC. A Fresh Start for the regulation and inspection of primary care dental services. Care Quality Commission. Available online at http://www.cqc.org.uk/sites/default/files/fresh_start_dental_signposting_statement_august_2014.pdf (accessed July 2015).
Health and Social Care Information Centre. Available online at https://www.gov.uk/government/organisations/health-and-social-care-information-centre (accessed June 2015).
Waste and Environmental impact (This page is 'Environmental management'. Please confirm the URL is correct). Available online at https://www.gov.uk/topic/environmental-management (accessed June 2015).
BDA. Curious about. British Dental Association. Available online at https://www.bda.org/curiousabout (accessed April 2015).
Nasser M, Evidence summary: can plastics used in dentistry act as an environmental pollutant? Can we avoid the use of plastics in dental practice? Br Dent J 2012; 212: 89–91.
Maykut P, Moorhouse R . Beginning Qualitative Research a Philosophic and Practical Guide. pp 45. RoutledgeFalmer: London, 2004.
Richardson J, Grose J, Manzi S, et al. What's in a bin: A case study of dental clinical waste composition and potential Green House Gas emission savings. Br Dent J 2015; 220: 61–66.
Richardson T, E. Handbook of Qualitative Research Methods. pp 25. Biddles Ltd: London, 1997.
Grose J, Richardson J . Report on raw materials risk in healthcare supply chains. WRAP, 2012. Available online at http://www.wrap.org.uk/content/report-raw-materials-risk-healthcare-supply-chains (accessed April 2015).
Grose J, Richardson J . Strategies to identify future shortages due to interruptions in the healthcare procurement supply chain: a method from the English National Health Service. J Heal Serv Res Pol 2012.
National Health Service Sustainable Development Unit. Saving Carbon Improving Health. NHS Carbon Reduction Strategy for England. Cambridge, 2009. Available online at http://www.sduhealth.org.uk/documents/publications/1237308334_qylG_saving_carbon,_improving_health_nhs_carbon_reducti.pdf (accessed January 2016).
Grose J, Richardson J . Managing a sustainable, low carbon supply chain in the English National Health Service: The views of senior managers. J Heal Serv Res Pol 2013; 18: 83–89.
Department of Health. Health Technical Memoranda 01–05: Decontamination in primary care dental practices. 2013. Available online at www.gov.uk/government/uploads/system/uploads/attachment_data/file/170689/HTM_01-05_2013.pdf (accessed January 2016).
Acknowledgements
We would like to thank the Institute for Sustainability Solutions Research at Plymouth University for funding this study, and staff in the practice for their time, patience and support during data collection.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Grose, J., Richardson, J., Mills, I. et al. Exploring attitudes and knowledge of climate change and sustainability in a dental practice: A feasibility study into resource management. Br Dent J 220, 187–191 (2016). https://doi.org/10.1038/sj.bdj.2016.136
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2016.136
This article is cited by
-
How sustainable is your dental workplace?
British Dental Journal (2022)
-
Environmentally sustainable dentistry: a brief introduction to sustainable concepts within the dental practice
British Dental Journal (2019)
-
Environmental sustainability and waste within the dental practice
BDJ Team (2019)
-
Environmental sustainability and waste within the dental practice
British Dental Journal (2019)
-
Green dentistry: a systematic review of ecological dental practices
Environment, Development and Sustainability (2019)