Key Points
-
Provides a history and examination of patients presenting with trigeminal neuropathy to facilitate clinicians in their assessment.
-
Reviews the literature demonstrating the differing causes of trigeminal neuropathy.
-
Presents a case series to outline the causes seen in our nerve injury clinic.
-
Highlights the importance of identifying red flag symptoms for neoplasia.
Abstract
Introduction Sensory neuropathies of the mandibular division of the trigeminal (V3) nerve can be debilitating, causing difficulty with daily function. It has a variety of causes, including iatrogenic injury, usually caused by third molar removal, local anaesthetic administration, implant placement or endodontic treatment. Non-iatrogenic causes include infection, primary or secondary neoplasia and various medical conditions.
Objective To review the aetiology, evaluation and management of V3 neuropathy in a retrospective case-series of patients referred to a specialist nerve injury clinic over an eight-year period, particularly focusing on the non-iatrogenic causes of this presentation.
Methods A retrospective analysis of the case notes of 372 patients referred to the specialist nerve injury clinic between 2006 and 2014 was carried out to establish the cause of the neuropathy and subsequent management or referral. The assessment protocol of trigeminal neuropathy used in the clinic is also outlined.
Results Most patients (89.5%) presented with neuropathy due to iatrogenic injury. Of the non-iatrogenic causes (10.5%), malignancy accounted for a fifth of presentations, and infection almost two-fifths, demonstrating the importance of prompt identification of a cause and management by the clinician, or referral to the appropriate specialty. Other, more rare causes are also presented, including multiple sclerosis, sickle-cell anaemia and Paget's disease, highlighting the importance to the clinician of considering differential diagnoses.
Conclusions This case series demonstrates the less frequent, but nevertheless important, non-iatrogenic causes which clinicians should consider when assessing patients with trigeminal neuropathy.
Similar content being viewed by others
Introduction
The aims of this article are to review the possible causes of mandibular division trigeminal (V3) sensory neuropathies, present a retrospective case series of patients presenting with such neuropathy and describe recommended evaluation and management of these patients.
Sensory neuropathy is altered sensory perception in the distribution of a nerve, presenting as anaesthesia (complete loss of sensation), paraesthesia (altered sensation), dysaesthesia (unpleasant sensation), neuropathic pain (pain in the distribution of the nerve) or a combination of these symptoms. Sensory neuropathy of the mandibular division of the trigeminal nerve (V3) in particular has been termed 'numb chin syndrome,'1,2 which is an umbrella term encompassing a range of aetiologies including iatrogenesis, infection, metabolic, degenerative, inflammatory, trauma and neoplasia.3
The trigeminal nerve is the 5th and largest cranial nerve, and is a mixed motor and sensory nerve. It is the 'protector' sensory system for the head and neck and the larger sensory part forms the opthalmic, maxillary and mandibular branches that carry afferents sensitive to external or internal stimuli from the skin, muscles, and joints of the face and mouth, and from the teeth (Fig. 1). The mandibular branch is the only branch with a motor component, which supplies the muscles of mastication (Table 1).
The impact of trigeminal neuropathy must not be underestimated. The face has one of the highest concentrations of sensory innervation, making sensory neuropathy in this area more difficult to tolerate compared with other parts of the body.4 Consequences include interference with daily social function, eating, drinking, speaking, kissing, applying makeup, shaving and sleeping;5,6,7 all functions that we take for granted and are the basis for sociability and life enhancement. Patients usually expect and experience significant improvements in jaw function, dental, facial, and overall body image following oral rehabilitation.8 V3 sensory neuropathy has a significant negative effect on the patient's quality of life and when the cause is iatrogenic, the psychological effects can be compounded.4
Causes of V3 sensory neuropathy include; iatrogenic (surgical and medical), infections, neoplasia, systemic pathology and idiopathic causes.
Iatrogenic - surgical
A recent study reported that 63% of cases of V3 sensory neuropathy were attributed to previous dental treatment.9 Iatrogenic injuries to the mandibular division of the trigeminal nerve may be caused by a variety of different treatment modalities such as maxillofacial surgery (for example sagittal split osteotomies, reduction and fixation of mandibular fractures)4 and minor oral surgery (including third molar removal),10 implant placement,11,12 inferior dental block and mental block anaesthesia,13 instrumentation beyond the apex, extrusion of irrigation fluid and filling materials during endodontic treatment.14 Other traumatic iatrogenic causes of trigeminal neuropathy include radiotherapy15 and exposure to chemical agents such as trichloroethylene, stilbamidine, and allopurinol.16 It has been shown that the use of whiteheads varnish and surgicel have temporary effects on peripheral neural function, and Carnoy's solution may have a permanent effect,17 this has most relevance in surgery performed in the region of the inferior dental nerve.
Third molar surgery is a common cause of iatrogenic injury to the mandibular division of the trigeminal nerve10,18,19 although modern management strategies have been found to successfully prevent injuries in high risk cases.20,21 Following administration of an inferior dental block injection, the prevalence of temporarily impaired lingual and inferior alveolar nerve function ranges from 0.15–0.54%;6,22 permanent neuropathy is much less frequent (0.0001–0.01%).6,23 Inferior alveolar nerve injury occurs in 1 in 14,000 inferior dental nerve block injections and is usually temporary (75%) but can persist and become permanent (at three months).24 Likewise, extrusion of endodontic materials or instrumentation beyond the apex in the region of the mental foramen or inferior alveolar nerve may cause severe mechanical and chemical injury resulting in V3 sensory neuropathy.14,25
V3 injury as a complication of implant treatment is becoming a major concern12,26,27 and incidence studies indicate a complication rate not to be ignored.28,29 There are rare reports of resolution of implant related V3 neuropathies at over four years,30 but these are the exception rather than the norm.31 Many authors recommend referral of these injuries within four months,7,32 but this may be too late. We now understand that within three months of injury, permanent central and peripheral neurological changes occur, rendering neurones unlikely to respond to surgical intervention.33
V3 sensory neuropathy has also been reported in connection with mandibular atrophy in the older population, particularly in edentulous individuals.11 Dentures which cause compression of the mental nerve in those with atrophic mandibles are a known cause of paraesthesia in this group.34
Iatrogenic medical
Medication related osteonecrosis of the jaw (MRONJ) has also been documented as a rare cause of V3 sensory neuropathy,3,35 with removal of necrotic bone and antibiotic administration resulting in resolution or improvement of the associated symptoms.36 In cases of suspected MRONJ related neuropathy it is important to rule out a primary or metastatic malignancy as many of these patients have been prescribed the medication for treatment of metastatic disease.
Infection
Local periapical infection of teeth has been reported to cause V3 sensory neuropathy.9,37,38,39,40,41,42 Infection-related neuropathy has been shown to resolve following non-surgical endodontic therapy or extraction of the causative tooth,38,43 supporting the theory that pressure caused by an expanding infection and inflammation can cause paraesthesia.
Viral infections have also been implicated in the development of V3 sensory neuropathy, with herpes zoster reactivation rarely causing neuropathy of the trigeminal nerve. The ophthalmic division is most commonly affected, however, the maxillary and mandibular divisions can also be involved.43
Acute and chronic osteomyelitis are potential causes of V3 sensory neuropathy, if there is involvement of the mandibular canal.15,44 Diffuse sclerosing osteomyelitis of the mandible has been reported as another cause of trigeminal neuropathy, with a small number of patients being successfully treated with bisphosphonate infusions.45 Osteoradionecrosis and superinfection of osteoradionecrosed bone can also cause neuropathy,15,46 as can surgery to treat such cases.46
Neoplasia
Following exclusion of a dental cause, V3 sensory neuropathy is often considered as a 'red flag' symptom because of its frequent association with systemic malignancies.9 When iatrogenic causes are excluded and if the neuropathy is only associated with the mandibular division of the trigeminal nerve it has been suggested that malignancy is the most likely cause.44
Neoplasia local to the nerve, for example odontogenic or non-odontogenic tumours and cysts of the mandible can lead to V3 sensory neuropathies.44,47 These can occur as a result of peripheral nerve sheath neoplasia,48 osteosarcoma of the mandible,1,15 multiple myeloma1,49 and direct extension of a squamous cell carcinoma of the lip.44
A wide variety of intracranial tumours in various locations of the nervous system including the brainstem, meckles cave and the cerebellar pontine angle cause clinical symptoms which can mimic V3 sensory neuropathy.15 These include benign and malignant neoplasms such as epidermoid cysts, schwannomas and gliomas.15,44
Secondary neoplasms affecting the nerve
Although any type of malignancy can metastasise, metastasis to the mandible is a rare event. Charles Bell was probably the first to describe this V3 neuropathy in 1830 in an elderly woman with breast cancer. Further cases of V3 sensory neuropathies among women with breast cancer have been reported more recently.1,44,50 All histological subtypes may be associated with this syndrome, such as:
-
Lung cancer (small cell and non-small cell carcinoma)1,3,44,50
-
Lymphoma (Hodgkin and non-Hodgkin), lymphosarcoma, Waldenstrom1,3,44
-
Squamous cell carcinoma of the lip44
-
Thyroid carcinoma1
-
Uterine carcinoma3
-
Primary intra-osseous carcinoma.1
Lymphomas, breast and lung cancers are however, by far, the most frequently reported.15 No sex predominance is found, the occurrence being due to the sex distribution of the underlining tumours. Brain metastases can also result in symptoms mimicking V3 sensory neuropathy, with the most commonly metastasising tumours to the brain being breast and lung cancer.15
Other medical causes
A presenting symptom of isolated V3 sensory neuropathy can lead to the diagnosis of a wide range of systemic medication conditions.51 These can be grouped into degenerative neurological disease, immunological, haematological, metabolic and endocrine. V3 sensory neuropathy has been described both as an isolated symptom and as part of a disease process such as vasculitis, which can occur secondary to rheumatoid arthritis,50 cerebro-vascular accident (CVA),52 connective tissue diseases,44 demyelinating diseases such as multiple sclerosis,3,44 sarcoidosis,53 Sjögren's syndrome,44,54 syphilis and diabetes mellitus.44,55,56,57 Among the more rare medical causes are sickle cell disease58,59 and Lyme disease.60
Idiopathic trigeminal neuropathy
It has been proposed that V3 sensory neuropathy which cannot be attributed to any underlying cause could be secondary to herpes simplex viral infections.16,51 However, peripheral and or central neoplasias must be excluded.
Background to this study
A dedicated orofacial pain and trigeminal nerve injury service has been running at King's College Hospital for over seven years. Weekly multidisciplinary clinics run by an oral surgeon, neurologist, neurosurgeon, psychiatrist and psychologist assess and manage patients referred by general dental practitioners (GDPs), general medical practitioners (GMPs) and other hospital based dentists and doctors. Over one hundred new referrals are received each year. The clinic also has an online referral service for iatrogenic trigeminal nerve injuries (www.trigeminalnerve.org.uk). This article describes a retrospective case series of consecutive patients referred for management of mandibular division trigeminal sensory neuropathy.
Assessment and clinical history
All patients referred to the clinic with V3 sensory neuropathy were assessed by the same practitioner (TR). A full medical, social and dental history was taken. A detailed history of the probable causative event (for example, wisdom tooth removal) for the neuropathy (if iatrogenic cause suspected) was taken (Table 2).
If a causative event was not linked to the onset of neuropathy, a detailed history was explored to exclude 'red flag' symptoms of neoplasia primarily, (Table 3) but also to consider other potential causes of neuropathy.
Psychological assessment is important in the management of iatrogenic nerve injury as many patients are severely psychologically affected.61 Several validated questionnaires are completed by the patient to establish their psychological state, anxiety or depression, pain intensity and effect on function and daily activity prior to consultation (Table 2). All patients who report changes to their psychological state or mental health issues are assessed by the liaison psychiatrist and may be referred on to the liaison psychologist for further treatment
Clinical examination
It is important to recognise that a patient may be anxious as those presenting with neuropathy are often concerned that they may have cancer or have had a previous traumatic iatrogenic event.
Initial extraoral examination routinely evaluates:
-
Cranial nerves excluding 1 and 8 (with crude identification of any sensory neuropathic area which is more closely investigated later [see text later in methods]).
-
Temporomandibular joints
-
Facial and cervical lymph nodes
-
Asymmetry, swellings or lesions
-
Facial scarring.
Intraoral examination
Initial examination should involve a thorough assessment of dentition, oral hygiene, mucosa, restorations and further testing of dental vitality, percussion, response to thermal stimuli and sensory changes to the teeth and mucosa.3 Any signs of local dental infection, surgical trauma or local malignancies should also be noted.
Vth nerve sensory examination
General sensory assessment of the skin and mucosa of all the divisions can be assessed using subjective function, light touch, moving point discrimination, sharp/blunt discrimination and two point discrimination techniques. This is shown in Figure 2.
Reflexes of the Vth cranial nerve include the jaw jerk reflex, which tests both sensory and motor components of the trigeminal nerve, and the corneal reflex (cornea touched with cotton whisp) which tests both efferent sensory CN5 and afferent motor CN7 resulting in bilateral blinking due to the consensual reflex. This examination identifies the presence of a neuropathy and gives information about the extent of involvement of the nerve. This should be mapped out to demonstrate the area(s) affected for future reference.
Vth nerve motor examination is only undertaken when patients present with obvious motor symptoms or complaints of weakness, trismus or spasms. This should identify normality (no tremor, involuntary chewing or trismus) with symmetry on tightly clenched teeth. Abnormality of motor function (tremor, trismus, involuntary movement and paralysis identified with deviation to the weak side on mouth opening and/or vertical misalignment of central medial incisors) can be detected. This provides information on the extent of the neuropathy, which gives further information about the likely location of a cause.
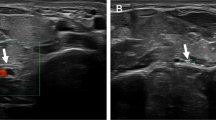
Investigations
The investigations for trigeminal neuropathy depend upon the presentation, with iatrogenic injury focusing on the cause, and spontaneous neuropathy investigations establishing if there is any neoplastic cause first and foremost, then focusing on the other possible medical causes.
Methods
Patient selection
A retrospective analysis of the clinic letters and patient records of all patients referred to the trigeminal nerve injury clinic between January 2006 and January 2014 with V3 sensory neuropathy was undertaken. V3 sensory neuropathy was defined as a patient presenting with subjective altered sensation in the mandibular division of the trigeminal nerve, which was confirmed on clinical neurosensory examination (Fig. 2).
Diagnostic criteria for V3 sensory neuropathy
-
Subjective altered sensation in mandibular division of trigeminal nerve (patient report of numbness, tingling, pins and needles, itching, burning or pain)
-
Change in subjective function in V3 dermatome (reduced or increased)
-
Abnormal clinical neurosensory tests (reduced or increased sensation to light touch, sharp/blunt discrimination and two point discrimination).
Outcome measures
The outcomes recorded included cause of V3 sensory neuropathy:
-
Iatrogenic (surgical)
-
Iatrogenic (medical)
-
Infection
-
Systemic disease process
-
Neoplastic
-
Idiopathic.
Treatment required for symptomatic management of V3 sensory neuropathy:
-
Reassurance and explanation
-
Surgical management of nerve injury
-
Removal of iatrogenic cause (for example, tooth extraction, implant removal)
-
Pharmacological management (local or systemic)
-
Psychological management
-
Resolution of neuropathy
-
Complete resolution
-
Partial resolution
-
No improvement.
Data collection and analysis
Data collection was carried out retrospectively from the clinic letters and patient records of all patients referred to the trigeminal nerve injury clinic with V3 sensory neuropathy between January 2006 – January 2014 by two of the authors (EC and ZY). Data was collected and entered into IBM Statistical Package for Social Sciences (SPSS) Version 22. Descriptive statistical analysis was carried out on the data using the above program to identify the aetiology of V3 sensory neuropathy in this series of patients.
Results
Patient demographics
372 patients (73% females: 27% males) were referred to the trigeminal nerve injury clinic with V3 sensory neuropathy between January 2006 and January 2014. The average age of patients was 45.6 (range 18–85 years [S.D. 13.5]). There was an average delay between onset of symptoms and assessment on the clinic of 16.9 months (range 2.5 weeks – 3 years).
Cause of V3 sensory neuropathy
The causes of V3 sensory neuropathy found in 372 patients who presented to the clinic between January 2006 and January 2014 are shown in Table 3. Results showed that 89.5% of cases had an iatrogenic cause, and 39 (10.5%) had other causes of neuropathy. Malignant causes were rare at eight (2.2%) patients within the case series, accounting for 20.5% of the non-iatrogenic cases. Infection was the identified causative factor in 15 patients (4%) of the cases, and was the most common non-iatrogenic cause at 38.5%. This study focussed on those patients who had non-iatrogenic causes of V3 sensory neuropathy.
Fifty-two percent of the 39 patients with non-iatrogenic V3 neuropathy were referred from their GDP, 38% were referred from a specialist in a tertiary care centre and 6% from their GMP. Owing to the nature of the notes available for the remaining two patients, whom they were referred from was not known. The mean age of the patients who had non-iatrogenic causes of neuropathy was 46.9 years (range 23 – 75), and 70% were female.
Over half of the patients (58%) did not have any other underlying medical condition. Of the six patients with multiple sclerosis, one had a pre-existing diagnosis of this condition and all patients were referred on to neurology services for further investigations, reviews and management. One 64-year old lady, who had been referred to the oral surgery department at KCH privately via a neurologist at Queen's Square received a new diagnosis of Paget's disease of bone.
Symptoms experienced
Patients with non-iatrogenic V3 sensory neuropathy predominately experienced numbness (56%) or tingling (30%) sensations. One patient described their symptoms as a 'floppy swollen feeling', another described it as 'itchiness', whilst another stated it was like 'ants crawling across the area' (or 'formication'). Paraesthesia was reported by 38% of patients, of whom 20% had evoked paraesthesia and 18% experienced spontaneous paraesthesia. One patient experienced both evoked and spontaneous paraesthesia.
Equal numbers of patients experienced evoked pain or spontaneous pain, at 28% of the cases. Three of these patients had both evoked pain and spontaneous pain. The most frequent words used to describe their pain were sharp, shooting and tightness. Other descriptors included pulling, dull, excruciating and radiating. 36% and 32% of patients reported allodynia and hyperalgesia, respectively.
Eighteen patients within the case series experienced some form of allodynia, whereas mechanical allodynia was experienced by 16 of these patients. Eight of these patients reported just mechanical allodynia; four of these patients experienced both extraoral (EO) and intraoral (IO) mechanical allodynia and the other four only had EO mechanical allodynia. One patient experienced only EO heat allodynia.
A mixture of mechanical, cold and/or heat allodynia was experienced by eight of the patients. EO and IO mechanical allodynia were experienced together with EO and IO cold allodynia in three patients. Three other patients only experienced EO mechanical and cold allodynia. Two patients reported a mixture of mechanical, cold and heat allodynia.
Functionality problems
The most common functionality problem reported by 52% of the cases was speech. Eating was the second most common functionality problem, reported by 40% of the patients. Drinking was problematic for 28% of patients and 26% stated that they had problems with kissing. Brushing teeth was difficult for 24% of patients. Other functionality problems included interference with sleep (12%) and work (6%). Make-up application and shaving were affected among 8% and 4% of the patients. Confidence levels and ability to socialise at events were affected among 4% and 6% of patients.
Another problem reported by 6% of patients included interference with the pronunciation of words, with one patient stating that she slurred her words. Dribbling sensations were reported by 12% of patients. Biting the lip was a problem for 8% of the patients and one patient stated that they kept biting their tongue.
Treatment required for symptomatic management of V3 sensory neuropathy:
Reassurance and explanation alone was sufficient in 12 patients without any dysaesthesia or neuropathic pain. The remaining patients had either a single type of treatment, or a mixture of treatments (for example, systemic and/or topical medication with cognitive behavioural therapy (CBT). Nine patients were on more than one treatment method for their pain management.
Surgical management of nerve injury was recommended for two patients. One of these patients was recommended debridement of the area, and it was suggested to the other patient that they potentially have the retained roots removed and exploration of the inferior-dental nerve. Surgery was not appropriate for the other patients either due to a significant delay in referral of greater than six months since the onset of symptoms, they required other dental procedures, or because they were suffering from altered sensations, but not pain, and any surgery could have caused further damage.
Dental procedures were recommended for all of the patients who had infection-related V3 sensory neuropathy. Such procedures included removal of the causative tooth to promote healing (five patients), removal of infected roots (one patient) and a proposed removal of retained roots (one patient) but this was very close to the inferior alveolar nerve and therefore its extraction was high-risk. A dentigerous cyst had to be removed under general anaesthetic for one patient. Re-root canal treatment (RCT) was recommended for six patients, with slight possibility of extractions amongst two of these patients. One patient was recommended possible implant treatment for the ower right second molar. Other dental treatments included the placement of a bridge and one patient was monitored over time to see any changes in radiolucency around the lower left 5 region with the possibility of taking antibiotics (clindamycin) for six weeks.
Pharmacological management of the symptoms of V3 sensory neuropathy was required in 11 patients for ongoing pain. This included use of local and systemic medication for pain management. Topical Versatis (lidocaine 5%) patches were recommended to four patients. Two patients were taking tricyclic antidepressant medication (amitriptyline or nortriptyline) and anticonvulsant medication (gabapentin, pregabalin) was being used by nine patients. Botox injections were not recommended to any of the patients.
Eleven patients required referral to liaison psychiatry and psychology services for cognitive behavioural therapy to aid in pain management. Two of these patients were also using Versatis patches and one patient was taking Gabapentin in addition to CBT. Two patients also had some dental treatment (oral hygiene or RCT) in addition to CBT.
Resolution of neuropathy
Of those patients with a non-iatrogenic cause of their V3 sensory neuropathy, patients who received a new diagnosis of a systemic condition or neoplasia were referred on to the relevant specialty for further investigations and/or management. Complete resolution of the neuropathy occurred amongst seven patients within the whole group of patients with non-iatrogenic V3 sensory neuropathy. These patients who had complete resolution had an infection-related neuropathy and their treatment predominately entailed extraction of the affected tooth to manage the infection. Five patients had partial resolution and 14 reported no change in their symptoms. The outcome for the remaining patients was unknown due to loss to follow-up.
Discussion
A case series of patients presenting with third division trigeminal (V3) sensory neuropathy is discussed in this paper. V3 neuropathy can be caused by a variety of causes, as illustrated in this patient case series, and spontaneous central or peripheral neoplasia must be excluded. Patients presented with underlying neoplasia in 2% of cases, thus clinicians must always be aware of this rare possibility and appropriately refer the patient for appropriate investigations. A recent review of trigeminal neuropathy, 'Numbness matters' highlights the various causalities and diagnostic challenges and suggests a possible assessment pathway.62 Numb chin syndrome is a commonly used term by neurologists referring to V3 neuropathy. This may be a misnomer, as highlighted in this paper, very few patients presenting with V3 neuropathy have anaesthesia or numbness alone. As with most sensory neuropathies the characteristic presentation includes anaesthesia, paraesthesia and elicited or background neuropathic pain.
This case series also highlights six patients (15.4%) presenting with multiple sclerosis presenting with V3 neuropathy. Dentists may not be familiar with non-iatrogenic trigeminal neuropathic and should be aware of red flags indicating likely neoplasia (Table 3) Spontaneous sensory neuropathy is always a clinical sign of concern, however the most common cause of non-iatrogenic cause of third division trigeminal sensory neuropathy in this case series was dental periapical infection. If a tooth root apex is close to the inferior dental canal and the dental pulp becomes necrotic then leakage of necrotic tissue through the apex of the root will irritate and inflame local nerve tissue.
Should a patient present with red flag signs associated with trigeminal neuropathy, once local dental pathology is excluded, prompt referral to a neurologist is essential. Red flags for neoplastic disease are shown in Table 3. More difficult is establishing a medical diagnosis for non-malignant spontaneous neuropathy because, as discussed, there are a plethora of potential medical causes which will rarely present to dentists. Our routine haematological investigations aim to identify haematological causes (haematinic deficiencies), diabetes, thyroid disease and autoimmune diseases. More specific investigations may be required in many conditions presenting with trigeminal neuropathy such as multiple sclerosis (MS), lupus, orofacial granulomatosis and infections including tuberculosis, oral and surgical infections. MS most likely presents with ophthalmic signs before presenting with trigeminal neuropathy or neuralgic pain,63 therefore, trigeminal neuropathy is unlikely to be the first presenting symptom of this condition; however, this has been reported in some patients. If a patient presents with trigeminal neuropathy and has known medical conditions, for example diabetes, then referral to the patient's GMP in the first instance for onward referral to a specialist physician or neurologist is appropriate.
Due to the specialism of the clinic, most of the trigeminal neuropathies seen in the oral surgery clinic were iatrogenic in nature (Table 3). This high proportion of patients with iatrogenic neuropathy is also demonstrated in a previous report,9 which notes that due to increasingly invasive dentistry many patients suffer from iatrogenic trigeminal neuropathy. Neurologists who are referred these patients may not be aware of the prevalence of this condition, and the range of potential dental causes of third molar removal, local anaesthetic administration, implant placement, endodontics and dental infection.
Iatrogenic trigeminal neuropathy risk factors, clinical profile and management have been previously reported.64,65,66,67 Other causes found in this case series highlight the importance of understanding the principles of history and examination in patients presenting with neuropathy affecting the trigeminal nerve, and consideration of how the onset of symptoms may be related to the cause. Trigeminal sensory neuropathy may present with hypofunction (partial or complete numbness) or hyperfunction with altered sensation (paraesthesia, dysaesthesia) and/or neuropathic pain (allodynia – pain on touch or hyperalgesia- increased pain with painful stimuli).51 Examination often cannot differentiate the iatrogenic from the spontaneous neuropathies. The history is therefore essential to discern the cause of the symptoms. General dental practitioners need to have an understanding of the potential causes of trigeminal neuropathy, and therefore identify if there is a dental cause, which, (in the case of infection) they could potentially treat, or refer to the appropriate clinician for other iatrogenic, neoplastic and medical causes of these symptoms. Infections were implicated in 4% of cases.
A detailed history of any previous traumatic or medical event that may be related to the neuropathy is paramount. Investigating certain risk factors may also reinforce your diagnosis of iatrogenic neuropathy. For those patients with spontaneous neuropathy a variety of causes have been reported and confirmed in this case series. Importantly, neoplasia must be suspected and excluded where possible, should no iatrogenic cause be implicated. Our case series demonstrates that although more uncommon, neoplasia can also contribute towards the number of non-iatrogenic causes of neuropathy at approximately one fifth of cases. This highlights the importance of differentiating iatrogenic from non-iatrogenic causes early so that these cases are not missed, and managed appropriately.
For patients presenting with iatrogenic neuropathy, depending upon mechanism and duration of the cause of the neuropathy, various management strategies are recommended.64 As with other iatrogenic neuropathies, acute medical management may be appropriate. This can involve step down steroids (prednisolone 50, 40, 30, 20 and 0 mg over five days) and non-steroidal anti-inflammatories (NSAIDs) (ibuprofen 600 mg QDS), in addition vitamin B complex injections.3,68,69,70 Treatment of post-surgical neuropathy does not have recommended evidence-based care and is usually managed symptomatically using systemic medications which can cause a plethora of complications and are often poorly tolerated by the patient. A topical approach to treating patients with chronic neuropathic orofacial pain may be more useful for such cases, especially in the avoidance of side effects. Such topical treatment may include the use of topical lidocaine patches,71 topical capsaicin,72,73 and topical local anaesthetic creams.74,75 Whilst there is some evidence that these topical methods provide pain relief, additional large controlled clinical trials are required in order to provide further clinical evidence for their use in pain management and to monitor any side effects of using these topical methods.71,76,77
This study did not endeavour to analyse the differences between clinical presentation of iatrogenic versus other causes. Further research would benefit clinicians in identifying pain history, clinical, neurological and psychological differences between various causes of trigeminal neuropathy.
This patient case series emphasises that iatrogenic causes for trigeminal neuropathy are more common than most clinicians realise. If there is no recent surgical event and dental pathology has been excluded, then systemic medical conditions and neoplasia must be considered. Prompt referral to medical specialty (preferably neurology) via the GMP is advised.
Summary
This paper reports on a case series of patients presenting with trigeminal neuropathy in eight years to a specialist trigeminal neuropathy dental service. It is highlighted that the majority of these neuropathies are iatrogenic in nature and rarely caused by neoplasias or other medical conditions. However, an appropriate assessment and, most importantly, thorough history will enlighten the treating clinician and enable appropriate investigations and referral, significantly improving the outcome for these patients.
References
Colella G, Giudice A, Siniscalchi G, Falcone U, Guastafierro S . Chin numbness: a symptom that should not be underestimated: a review of 12 cases. Am J Med Sci 2009; 337: 407–410.
Divya K S, Moran N A, Atkin P A . Numb chin syndrome: a case series and discussion. Br Dent J 2010; 208: 157–160.
Assaf A T, Jurgens T P, Benecke A W et al. Numb chin syndrome: a rare and often overlooked symptom. J Oral Fac Pain Head 2014; 28: 80–90.
Akal Ü, Sayan N, Aydogan S, Yaman Z . Evaluation of the neurosensory deficiencies of oral and maxillofacial region following surgery. Int J Oral Maxillofac Surg 2000; 29: 331–336.
Hillerup S, Hjørting-Hansen E, Reumert T . Repair of the lingual nerve after iatrogenic injury: a follow-up study of return of sensation and taste. J Oral Maxillofac Surg 1994; 52: 1028–1031.
Harn S, Durham T . Incidence of lingual nerve trauma and post injection complications in conventional mandibular block anaesthesia. J Am Dent Assoc 1990; 121: 519–523.
Ziccardi V B . Trigeminal nerve injuries. J New Jersey Dent Assoc 2000; 71: 41–44.
Kiyak H A, Beach B H, Worthington P, Taylor T, Bolender C, Evans J . Psychological impact of osseointegrated dental implants. Int J Oral Maxillofac Implants 1990; 5: 61–69.
Kalladka M, Proter N, Benoliel R, Czerninski R, Eliav E . Mental nerve neuropathy: patient characteristics and neurosensory changes. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106: 364–370.
Bataineh A . Sensory nerve impairment following mandibular third molar surgery. J Oral Maxillofac Surg 2001; 59: 1012–1017.
Wismeijer D, van Waas M A, Vermeeren J, Kalk W . Patients' perception of sensory disturbances of the mental nerve before and after implant surgery: a prospective study of 110 patients. Br J Oral Maxillofac Surg 1997; 35: 254–259.
Kraut R, Chahal O . Management of patients with trigeminal nerve injuries after mandibular implant placement. J Am Dent Assoc 2002; 133: 1351–1354.
Hillerup S, Jensen R . Iatrogene nerveskader opstået i almen tandlægepraksis. Hyppighed, årsager og symptomer. Tandlaegebladet 2001; 105: 614–622.
Grotz K, Al-Nawas B, Aguiar Ed, Schulz A, Wagner W . Treatment of injuries to the inferior alveolar nerve after endodontic procedures. Clin Oral Investig 1998; 2: 73–76.
Becker M, Kohler R, Vargas M I, Viallon M, Delavelle J . Pathology of the trigeminal nerve. Neuroimag Clin North Am 2008; 18: 283–307.
Cavanagh J B, Buxton P H . Trichloroethylene cranial neuropathy: is it really a toxic neuropathy or does it activate latent herpes virus? J Neurol Neuro Psych 1989; 52: 297–303.
Loescher A R, Robinson P P . The effect of surgical medicaments on peripheral nerve function. Br J Oral Maxillofac Surg 1998; 36: 327–332.
Loescher A, Smith K, Robinson P . Nerve damage and third molar removal. Dent Update 2003; 30: 375–380.
Carmichael F, McGowan D . Incidence of nerve damage following third molar removal: a West of Scotland Oral Surgery Research Group Study. Br J Oral Maxillofac Surg 1992; 30: 78–82.
Pogrel M, Lee J, Muff D . Coronectomy: a technique to protect the inferior alveolar nerve. J Oral Maxillofac Surg 2004; 62: 1447–1452.
Umar G, Obisesan O, Bryant C, Rood J . Elimination of permanent injuries to the inferior alveolar nerve following surgical intervention of the 'high risk' third molar. Br J Oral Maxillofac Surg 2013; 51: 353–357.
Krafft T, Hickel R . Clinical investigation into the incidence of direct damage to the lingual nerve caused by local anaesthesia. J Craniomaxillofac Surg 1994; 22: 294–296.
Haas D, Lennon D . A 21 year retrospective study of reports of paresthesia following local anaesthetic administration. J Can Dent Assoc 1995; 61: 319–330.
Renton T, Janjua H, Gallagher J E, Dalgleish M, Yilmaz Z . UK dentists' experience of iatrogenic trigeminal nerve injuries in relation to routine dental procedures: why, when and how often? Br Dent J 2013; 214: 633–642.
Morse DR . Infection-related mental and inferior alveolar nerve paresthesia: literature review and presentation of two cases. J Endod 1997; 23: 457–460.
Worthington P . Injury to the inferior alveolar nerve during implant placement: a formula for protection of the patient and clinician. Int J Oral Maxillofac Implants 2004; 19: 731–734.
Chaushu G, Taicher S, Halamish-Shani T, Givol N . Medicolegal aspects of altered sensation following implant placement in the mandible. Int J Oral Maxillofac Implants 2002; 17: 413–415.
Dao T, Mellor A . Sensory disturbances associated with implant surgery. Int J Prosthodont 1998; 11: 462–469.
Bartling R, Freeman K, Kraut R . The incidence of altered sensation of the mental nerve after mandibular implant placement. J Oral Maxillofac Surg 1999; 57: 1408–1412.
Elian N, Mitsias M, Eskow R et al. Unexpected return of sensation following 4.5 years of paresthesia: case report. Implant Dentistry 2005; 14: 364–370.
Robinson P . Observations on the recovery of sensation following inferior alveolar nerve injuries. Br J Oral Maxillofac Surg 1988; 26: 177–189.
Hegedus F, Diecidue R J . Trigeminal nerve injuries after mandibular implant placement-practical knowledge for clinicians. Int J Oral Maxillo Implants 2006; 21: 111–116.
Clark A K, Old E A, Malcangio M . Neuropathic pain and cytokines: current perspectives. J Pain Res 2013; 6: 803–814.
Szewka A J, Purdy H, Topel J, Jhaveri M D . Teaching neuroimages: numb chin syndrome in an edentulous patient. Neurology 2011; 77: e38.
Zadik Y, Benoliel R, Fleissig Y, Casap N . Painful trigeminal neuropathy induced by oral bisphosphonate-related osteonecrosis of the jaw: a new etiology for the numb-chin syndrome. Quintessence Int 2012; 43: 97–104.
Otto S, Hafner S, Grotz K A . The role of inferior alveolar nerve involvement in bisphosphonate-related osteonecrosis of the jaw. J Oral Maxillofac Surg 2009; 67: 589–592.
Cavallito C DFF, Arduino P G, Broccoletti R, Carbone M . Numb chin syndrome. Annali di Stomatologia 2013; 4: 1–48.
Di Lenarda R, Cadenaro M, Stacchi C . Paresthesia of the mental nerve induced by periapical infection: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90: 746–749.
Ozkan B T, Celik S, Durmus E . Paresthesia of the mental nerve stem from periapical infection of mandibular canine tooth: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 105: e28–31.
Giuliani M, Lajolo C, Deli G, Silveri C . Inferior alveolar nerve paresthesia caused by endodontic pathosis: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 92: 670–674.
Barrett A P, Buckley D J . Selective anesthesias of peripheral branches of the trigeminal nerve due to odontogenic infection. Oral Surg Oral Med Oral Path 1986; 62: 226–228.
Morse D . Infection-related mental and inferior alveolar nerve paresthesia: literature review and presentation of two cases. J Endodontics 1997; 23: 457–460.
Elliston N K, Hoen M M . Infectious transient dental-related paresthesia. Gen Dent 1996; 44: 66–69.
Dumas M, Perusse R . Trigeminal sensory neuropathy: a study of 35 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999; 87: 577–582.
Urade M, Noguchi K, Takaoka K, Moridera K, Kishimoto H . Diffuse sclerosing osteomyelitis of the mandible successfully treated with pamidronate: a long-term follow-up report. Oral Surg Oral Med Oral Path Oral Rad 2012; 114: e9–e12.
Jacobson A S, Zevallos J, Smith M et al. Quality of life after management of advanced osteoradionecrosis of the mandible. Int J Oral Maxillofac Surg 2013; 42: 1121–1128.
Bodner L, Oberman M, Shteyer A . Mental nerve neuropathy associated with compound odontoma. Oral Surg Oral Med Oral Pathol 1987; 63: 658–660.
Schmidt R F, Yick F, Boghani Z, Eloy J A, Liu J K . Malignant peripheral nerve sheath tumors of the trigeminal nerve: a systematic review of 36 cases. Neurosurgical Focus 2013; 34: E5.
Vincent S D, Lilly G E, Hupp J R . Paresthesia of the mandibular division, trigeminal nerve. J Oral Maxillofac Surg 1993; 51: 565–569.
Alentorn A, Montero J, Vidaller A, Casasnovas C . Numb chin syndrome as an early symptom of primary and secondary vasculitis. Joint Bone Spine 2011; 78: 427–428.
Penarrocha M, Cervello M A, Marti E, Bagan J V . Trigeminal neuropathy. Oral Dis 2007; 13: 141–150.
Katsuno M, Teramoto A . Secondary trigeminal neuropathy and neuralgia resulting from pontine infarction. J Stroke Cerebrovascular Dis 2010; 19: 251–252.
Poate T W, Sharma R, Moutasim K A, Escudier M P, Warnakulasuriya S . Orofacial presentations of sarcoidosis-a case series and review of the literature. Br Dent J 2008; 205: 437–442.
Delalande S, de Seze J, Fauchais A L et al. Neurologic manifestations in primary Sjogren syndrome: a study of 82 patients. Medicine 2004; 83: 280–291.
Cruccu G, Agostino R, Inghilleri M, Innocenti P, Romaniello A, Manfredi M . Mandibular nerve involvement in diabetic polyneuropathy and chronic inflammatory demyelinating polyneuropathy. Muscle Nerve 1998; 21: 1673–1679.
Takayama S, Osawa M, Takahashi Y, Iwamoto Y . Painful neuropathy with trigeminal nerve involvement in type 2 diabetes. J Int Med Res 2006; 34: 115–118.
Kochar D K, Agarwal N, Thanvi I, Joshi A, Jain N . Isolated bilateral fifth cranial nerve paralysis with autonomic neuropathy in a case of insulin dependent diabetes mellitus. J Assoc Physic India 1998; 46: 975–976.
Hamdoun E, Davis L, McCrary S J, Eklund N P, Evans O B . Bilateral mental nerve neuropathy in an adolescent during sickle cell crises. J Child Neurol 2012; 27: 1038–1041.
Konotey-Ahulu FI . Mental-nerve neuropathy: a complication of sickle-cell crisis. Lancet 1972; 2: 388.
Maillefert J F, Dardel P, Piroth C, Tavernier C . Mental nerve neuropathy in Lyme disease. Revue du rhumatisme (English ed). 1997; 64: 855.
Smith J G, Elias L A, Yilmaz Z et al. The psychosocial and affective burden of posttraumatic neuropathy following injuries to the trigeminal nerve. J Orofacial Pain 2013; 27: 293–303.
Smith J H, Cutrer F M . Numbness matters: a clinical review of trigeminal neuropathy. Cephalalgia 2011; 31: 1131–1144.
Gallien P, Gich J, Sanchez-Dalmau B F, Feneberg W . Multidisciplinary management of multiple sclerosis symptoms. Euro Neurol 2014; 72 (Suppl 1): 20–25.
Renton T . Oral surgery: part 4. Minimising and managing nerve injuries and other complications. Br Dent J 2013; 215: 393–399.
Coulthard P, Kushnerev E, Yates J M et al. Interventions for iatrogenic inferior alveolar and lingual nerve injury. Cochrane Database Syst Rev 2014; 4: Cd005293.
Renton T, Yilmaz Z . Managing iatrogenic trigeminal nerve injury: a case series and review of the literature. Int J Oral Maxillofac Surg 2012; 41: 629–637.
Renton T, Yilmaz Z . Profiling of patients presenting with posttraumatic neuropathy of the trigeminal nerve. J Orofacial Pain 2011; 25: 333–344.
Dworkin RH, O'Connor A B, Kent J et al. Interventional management of neuropathic pain: NeuPSIG recommendations. Pain 2013; 154: 2249–2261.
Lin M . Therapeutic effects of the point-injection therapy on primary trigeminal neuralgia-an observation of 103 cases. J Tradit Chin Med 2003; 23: 195–196.
Yatsuhashi T, Nakagawa K, Matsumoto M et al. Inferior alveolar nerve paresthesia relieved by microscopic endodontic treatment. Bull Tokyo Dent Coll 2003; 44: 209–212.
Khawaja N, Yilmaz Z, Renton T . Case studies illustrating the management of trigeminal neuropathic pain using topical 5% lidocaine plasters. Br J Pain 2013; 7: 107–113.
Derry S, Sven-Rice A, Cole P, Tan T, Moore R A . Topical capsaicin (high concentration) for chronic neuropathic pain in adults. Cochrane Database Syst Rev 2013; 2: CD007393.
Webster L R, Nunez M, Tark M D et al. Tolerability of NGX-4010, a capsaicin 8% dermal patch, following pretreatment with lidocaine 2.5%/prilocaine 2.5% cream in patients with post-herpetic neuralgia. BMC Anesthesiol 2011; 11: 25.
Sawynok J . Topical analgesics in neuropathic pain. Curr Pharm Design 2005; 11: 2995–3004.
Somberg J C, Molnar J . Retrospective Evaluation on the Analgesic Activities of 2 Compounded Topical Creams and Voltaren Gel in Chronic Noncancer Pain. Am J Therapeutics 2015; 22: 342–349.
Derry S, Wiffen P J, Moore R A, Quinlan J . Topical lidocaine for neuropathic pain in adults. Cochrane Database Syst Rev 2014; 7: CD010958.
Humble S R, Dalton A J, Li L . A systematic review of therapeutic interventions to reduce acute and chronic post-surgical pain after amputation, thoracotomy or mastectomy. Euro J Pain 2015; 19: 451–465.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Carter, E., Yilmaz, Z., Devine, M. et al. An update on the causes, assessment and management of third division sensory trigeminal neuropathies. Br Dent J 220, 627–635 (2016). https://doi.org/10.1038/sj.bdj.2016.444
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2016.444
This article is cited by
-
Does the addition of cone-beam CT to panoral imaging reduce inferior dental nerve injuries resulting from third molar surgery? A systematic review
BMC Oral Health (2022)
-
Articaine: friend or foe?
British Dental Journal (2017)
-
Erratum
British Dental Journal (2016)