Key Points
-
Reviews NICE recommendations for sedation practice for patients under 19 years of age for procedures across medicine and dentistry in 2010.
-
Compares current UK dental sedation practice to recommendations on training, techniques and setting.
-
Reports agreement in many areas as well as some interesting opinions relating to the appropriate person for provision of advanced sedation.
Abstract
Aim Describe current dental sedation practice for under 19-year-olds in the UK and compare it with the recommendations of NICE guidance 112.
Method Members of the Society for the Advancement of Anaesthesia in Dentistry and members of the Dental Sedation Teachers Group were invited to participate in an online survey.
Results Two hundred and sixty-six dentists and doctors completed the survey. Eighty-two percent were operator and sedationist (operator-sedationist). Ninety-five percent provided written information and 94% obtained written consent. Eighty-four percent kept a written or electronic sedation record. Eighty-six percent complied with life support training expectations. Eighty-six percent had immediate access to resuscitation equipment. Sixty-seven percent of sedationists reported that treatment could not be completed under sedation for <10% of cases during the previous year. When sedation was unsuccessful, 61% said they would schedule general anaesthesia and 54.5% would schedule advanced sedation care. Forty-nine percent believed that a dentist was an appropriate person to provide advanced sedation for 12–18 years. Only 24% thought a dentist should provide advanced sedation for children <12 years, with 75% preferring an anaesthetist. The appropriate setting for advanced sedation was thought to be primary care by 33% and secondary care by 68%.
Conclusions We found good agreement between the current practice of sedation and the recommendations of the NICE guidance 112.
Similar content being viewed by others
Introduction
The practice of conscious sedation has been one of the most controversial and highly regulated areas of dentistry in the UK over the past 25 years. Since the Wylie report in 1978,1 there have been many documents providing guidance, guidelines and expert opinion on this area of practice. There are more documents produced by more committees for this area of practice than any other area of dentistry. A list of documents produced in the UK since 1978 is given in Table 1.
Despite all the documentation, confusion and controversy still abound. There is debate regarding which techniques should be used, by whom and where. The National Institute for Health and Care Excellence (NICE) published guidance on sedation in children and young people (clinical guidance 112) in 2010.2 This document offered recommendations on the care of patients under the age of 19 years receiving sedation for diagnostic and therapeutic procedures across all specialties in medicine and dentistry. Its key priorities for implementation related to assessment, consent, personnel, training and clinical environment.
An Independent Expert Group on Training and Standards for Sedation in Dentistry (IEGTSSD) was formed in 2011 in the UK and has published standards, training recommendations and syllabi for advanced sedation techniques for adult and paediatric patients.3,4 The adult and paediatric syllabi are based on recommendations contained in three publications: Conscious sedation and the provision of dental care – report of an expert group on sedation for dentistry, Department of Heath Standing Dental Advisory Committee (2003),5 Standards for conscious sedation in dentistry: alternative techniques, the Standing Committee on Sedation for Dentistry, Royal College of Surgeons of England (2007)6 and Sedation in children and young people, NICE (2010).2 All these documents have been accepted by the healthcare professions. However, none contained a training syllabus for practitioners wishing to practice either basic or advanced conscious sedation techniques.
The members of IEGTSSD wished to investigate current sedation practice in dentistry for patients under 19 years of age and compare this to the advice offered by the NICE guidance 112. This would be the first description of dental sedation practice for under 19-year-olds in the UK since the implementation publication of the NICE guidance and would provide information about the opinions and practice of sedationists working in this area.
We used the classification of basic and advanced sedation techniques, as published in 2007 by the UK Standing Committee for Sedation in Dentistry (Table 2) in our study.6 The terms standard and alternative have also been used in the past to distinguish between the more commonly recommended and used techniques and those required by a smaller minority of patients. In general terms the basic techniques are the same as those that were previously described as standard, and the advanced techniques are the same as those called alternative. These describe particular techniques and drugs used.
The NICE guidance 112 uses the following definitions of sedation based on the American Society of Anaesthesiologists. These describe levels of sedation rather than particular techniques or drugs required to achieve these levels.
-
Minimal sedation: awake and calm responding to command with ventilatory and cardiovascular function unaffected
-
Moderate sedation: sleepy but responding to command with adequate spontaneous ventilation and cardiovascular function maintained
-
Conscious sedation: similar to moderate and the term preferred and used in dentistry
-
Deep sedation: asleep and not easily roused but respond to painful stimuli. Ability to maintain ventilatory function impaired and may require assistance. In the UK this is described as light general anaesthesia.
We present the findings of an on-line survey.
Method
Members of the Society for the Advancement of Anaesthesia in Dentistry (SAAD) and members of the Dental Sedation Teachers Group (DSTG) were invited to participate in an on-line survey. These two groups attract clinicians (dental and medical) who have a special interest in dental sedation practice. The membership of each of these groups was informed of the study by newsletter and invited to complete the questionnaire as a means of measuring current practice. An online survey (Survey Monkey tool) was developed and piloted by IEGTSSD with the support of NICE. Descriptive statistics were produced with Excel. NICE guidance 112 was published in December 2010 and the survey was undertaken in March 2013. Our questions covered a range of the most significant or controversial recommendations of the NICE guidance 112.
Results
The online survey was completed by 266 individuals, 225 (95.8%) of whom had a dental qualification, 11 (4.1%) were medical and five (1.9%) held both qualifications. Males accounted for 143 (53.8%) of the sample and 123 (46.2%) were female. Twenty-four respondents were under 30 years of age, 164 were 30–50 years of age and 77 were over 50 years of age. Six respondents graduated within two years, 41 within 3–8 years, 94 within 9–20 years and 127 more than 20 years earlier. The majority of respondents (205, 77.1%) were practising in England, with nine (3.4%) in Wales, 35 (13.2%) in Scotland and 11 (4%) in Northern Ireland. The majority (139, 52%) were working in primary care, with 69 (25.9%) in the salaried services and 93 (34.9%) in the secondary care environment. Eight (3.0%) dentists worked in practice alone, 118 (44.4%) reported working with one to four others, and 127 (47.7%) worked with five or more others. Regarding postgraduate (PG) qualifications, 80 respondents had a PG Certicate, 84 a PG Diploma and 20 had an MSc.
Basic sedation training
Inhalational sedation with nitrous oxide and oxygen training had been undertaken by 224 (84.2%) respondents. Training in the use of intravenous sedation with midazolam had been undertaken by 231 (86.8%) individuals and in the use of oral or transmucosal midazolam by 131 (49.2%) individuals. The responses indicate that the majority of those who answered the question had received training in more than one basic sedation technique.
Advanced sedation training
Training in advanced sedation techniques had been undertaken by a much smaller number of the respondents. Only 85 (31.9%) of the 266 sample had undergone training in any of the advanced sedation techniques and these showed agreement with those undertaking advanced sedation techniques (as in Table 3). The majority of the 85 had undergone training in more than one of the advanced sedation techniques as shown in Table 4.
Resuscitation training
In response to the question, 'When did you last attend a course in life support skills?' 230 (86.4%) indicated within the previous year, 23 (8.6%) within the previous three years and six (2.2%) stated more than three years. Basic life support (BLS) training had been undertaken by 127 (48.0%), intermediate life support (ILS) by 134 (50.4%), advanced life support (ALS) by 35 (13.2%) and paediatric advances life support (PALS) by ten (3.7%). A number of those who answered the question had undertaken more than one level of training in life support skills.
Pre-sedation assessment
Clinicians were asked, 'How do you assess patients before sedation?' A medical history form, completed by the patient and checked by the dentist, was used by 196 (73.7%) respondents. A medical history form completed by the dentist was reported by 92 (34.6%). An anxiety questionnaire was used by 97 (36.4%). A physical examination was undertaken by 171 (64.2%).
Written information
When asked 'Do you provide written information for all patients receiving sedation?', 252 (94.7%) reported doing so and only two (0.7%) reporting that they did not. The information sheets included advantages (211, 79.3%), disadvantages (189, 71.0%), benefits (208, 78.2%) and risks of the sedation (203, 76.3%).
Consent and working practice
Nearly all (250, 93.9%) respondents obtained written consent for the procedure including the sedation. Most (219, 82.3%) dentists worked as operator and sedationist. Of those that did, the majority (222, 83.5%) had an appropriately trained assistant. Training was described as Certificate in Dental Sedation Nursing (CDSN) (121, 45.5%), SAAD (86, 32.3%), other course (47, 17.7%), and in-house (88, 33.1%).
Frequency of sedation for young people and types of sedation
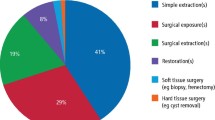
Table 4 shows the number of young people under 19 years of age that were sedated by respondents and the type of sedation technique used.
Monitoring and resuscitation equipment
Pulse oximetry was used by 201 (75.6%) dentists and non-invasive blood pressure (NIBP) by 133 (50.0%). Fewer used other types of monitoring equipment: 12 (4.7%) used ECG or BIS, and ten (3.7%) used capnography. The majority of dentists (224, 84.2%) kept a written or electronic sedation record.
Two hundred and twenty-nine (86.1%) dentists reported having immediate access to resuscitation equipment.
Sedation efficacy
One hundred and seventy-eight (66.9%) sedationists reported that they were unable to complete treatment under sedation for <10% of children and young people during the previous year. Single sedationists (0.4%) reported being unable to complete treatment in over 50% children and young people. Nineteen (7.1%) sedationists reported inability to complete treatment for 10–20% of patients. The majority (162, 60.9%) of dentists scheduled completion of treatment using general anaesthesia, but others (25, 9.3%) were referred to a psychologist or (22, 8.3%) scheduled for an advanced sedation technique. Another 39 (14.7%) dentists indicated alternative but unspecified management. One hundred and sixty-two (60.9%) sedationists audited their service.
Appropriate person and setting for advanced sedation
One hundred and twenty-nine (48.5%) respondents thought that a dentist was an appropriate person to provide advanced sedation techniques for 12–18-year-old young patients and 30 (11.3%) thought that this should be a doctor: one hundred and fifty-six (27.5%) specified that an anaesthetist was the appropriate person. In respect of patients <12 years of age then the respondents choosing a dentist reduced to 65 (24.4%) and also reduced for a doctor (28, 10.5%) but appreciably increased for anaesthetist (200, 75.2%).
The setting for advanced sedation techniques was considered to be primary care by 87 (32.7%), salaried services by 98 (37.5%), and secondary care services by 183 (68.7%). Opinion changed a little when asked about advanced sedation techniques for those under 12-years of age to 54 (20.3%) for primary care, 72 (27.1%) for salaried services and 202 (75.9%) for secondary care.
Respondents opinion about appropriate management of under 12-year-olds
The survey asked, 'Which of the following do you consider to be the appropriate management strategy for children aged 12 or under who cannot be managed under local anaesthetic with either nitrous oxide/oxygen or midazolam alone?'. Over 50% of respondents thought that advanced sedation would be appropriate (Table 5).
Discussion
The SAAD and DSTG have a combined membership of almost 2,000. With 266 respondents completing the survey, we posit that this is representative of the membership of SAAD and DSTG, as the statistical margin of error is 5.6% at 95% level of confidence. Thus, the result presented provides a broad range of experience, practice and opinion among the membership.
Males accounted for 54% of the sample and 46% were female, which is representative of the dental profession taking into account the age ranges with the majority being under 50 years of age. Six respondents graduated within two years, 41 within 3–8 years, 94 within 9–20 years and 127 more than 20 years earlier. The majority of respondents (77%) were practicing in England, with 3% in Wales, 13% in Scotland and 4% in Northern Ireland. This suggests that Wales was slightly underrepresented in the sample. The majority of respondents (52%) were working in primary care, with 26% in the salaried services and 35% in the secondary care environment. Only 3% of dentists worked in practice alone, with 44% working with one to four others, and 47% working with five or more others. This latter figure, which seems high, is probably explained by those working in secondary care in large teams.
Sedation training
A large number of individuals working in the area of sedation in dentistry have university qualifications, including higher degrees. Several clinical academic university departments offer courses that provide clinical experience or training alongside academic study. Eighty respondents had a PG certicate, 84 a PG diploma and 20 had an MSc. Sedation training is also incorporated into several dental specialist training programmes such as oral surgery and paediatric dentistry although we did not enquire about this. Training is otherwise available via groups such as SAAD, or other groups or individuals who run CPD-type training but may also offer clinical supervision or mentoring.7
Inhalational sedation with nitrous oxide and oxygen training was reported by 224 respondents. Training in the use of intravenous sedation with midazolam alone was undertaken by 231 individuals and in the use of oral or transmucosal midazolam by 131 individuals. These figures were not unexpected given that the majority of conscious sedation for dental procedures involves the use of a single drug, either nitrous oxide with oxygen, or midazolam. These techniques are considered to be 'basic' techniques and are the basis of undergraduate teaching in conscious sedation in UK dental schools.8 Many PG courses are also available offering training in these techniques.7
Just over half (55%) of the respondents reported having undergone no training in the different types of advanced sedation. Many clinicians do not offer advanced sedation techniques and so would not be expected to have undergone training in this area. Of the 45% of respondents that had undergone training in advanced techniques, similar proportions had undergone training in sedation for under 12-year-olds other than nitrous oxide and oxygen, a benzodiazepine in addition to another intravenous sedative drug, propofol sedation, inhalational sedation using an alternative agent to nitrous oxide, and combined routes such as intravenous and inhalational. Many of these individuals had undergone training in several different types of advanced technique rather than a single technique. Courses are likely to offer training in multiple techniques rather than a single techniques.
NICE recommend that healthcare professionals delivering sedation should have knowledge and understanding of sedation techniques and practice. We found very good evidence that sedation delivery in dentistry was compliant with this recommended training.
Resuscitation training
In response to the question, 'When did you last attend a course in life support skills?' the majority (86%) indicated that they had undertaken this within the previous year. The General Dental Council require dentists to follow the guidance on medical emergencies and training updates issued by the Resuscitation Council (UK).9,10 The latter state that dental staff should undergo regular training in the management of medical emergencies and that staff should update their skills annually. Not all respondents were dentists but the General Medical Council have similar expectations. It is therefore disappointing that 9% surveyed stated that they had not undergone update training within the previous year but had only done so within three years and 2% stated that it was more than three years since they underwent training. This resuscitation training requirement is for all UK dentists and the dental team and is not specific to those providing sedation but is none the less disappointing. BLS training is the level of training that is required on at least an annual basis and this had been undertaken by 48%. The certification lasts one year for BLS as it does for ILS which was undertaken by 50%. ALS was undertaken by 13% and PALS by 4%. These advanced courses are not a requirement of dental practice although some elect to undergo this training and we found that a significant proportion of sedationists had done this.
Dental practitioners and dental care professionals are all expected to undergo training in cardiopulmonary resuscitation, basic airway management and the use of an AED with regular practice using simulated emergencies. NICE guidance 112 advises that all members of the sedation team should have basic life support skills and those involved in delivering moderate sedation should have intermediate life support skills. We were not specific in our question about level of training as 'life support skills' implies intermediate training in dentistry. We found that the majority of respondents confirmed that they complied with life support training expectations but of concern were the small number who did not.
Pre-sedation assessment
Clinicians were asked, 'How do you assess patients before sedation?'. The majority (74%) used a medical history form completed by the patient. A medical history form completed directly by the dentist was reported by 35%. It is important that the dentist interprets the medical history if provided on a form completed by the patient, so that the dental management can take this into account as appropriate and use the information for risk assessment. NICE 112 recommends that assessment should include current medical condition, weight, current and previous medications, physical status and psychological status. We found very good evidence that sedationists were obtaining a valid medical and drug history. We did not enquire about obtaining weight.
An anxiety questionnaire was used by 36% which is not surprising as dental anxiety is the most common indication for sedation, however it has not always been routine to use such a questionnaire in clinical practice. These scales have been commonly used in clinical research. We did not enquire as to the nature of the anxiety measure used. This suggests that objective assessment of psychological status should take place alongside routine history and observation, which is more than is advised by NICE.
Around the time of the survey there were a series of publications describing a novel indicator of sedation need (IOSN) tool incorporating the modified dental anxiety scale but also taking account of patient medical and behavioural indicators and the anticipated treatment complexity. This has been promoted to support individual clinician decision making and also to enable commissioners to identify those who need conscious sedation in order to plan and deliver sedation services.11,12,13 This IOSN tool was not published until just before the survey was undertaken and so was unlikely to have had an effect on clinical practice as reported in our results. The IOSN is a validated tool for use in adults and is currently under development in children under 16 years of age.14
A large proportion (64%) reported undertaking a physical examination. A full physical examination before dental treatment would be seen to be unnecessary and inappropriate outside a hospital setting. However, measurement of blood pressure is recommended for those patients requiring basic intravenous sedation and advanced sedation techniques this. Also, some may measure heart rate, high and weight to calculate BMI. The proportion of respondents undertaking a physical examination is in keeping with proportion of those undertaking intravenous and advanced sedation techniques.
Written information
When asked 'Do you provide written information for all patients receiving sedation?' nearly all respondents reported doing so and patient information sheets included advantages, disadvantages, benefits and risks by the vast majority. As a most frequent indication for sedation is patient anxiety, it is important to provide information in a written format as they are unlikely to remember everything that they have been told. This patient information sheet is also important in providing information to the patients escort and ensuring safe care of the patient. NICE 112 advises that for a child, young person, their parent or carer to make an informed decisions they should have been offered verbal and written information describing the proposed technique and alternatives and associated risks and benefits. We found excellent agreement with this standard.
Consent and working practice
Nearly all respondents obtained written consent for the procedure including the use of sedation as part of the consent process. This practice has been common in hospital practice for some years but has been less common in other settings. Being very clear about the planned treatment is very important and the plan cannot change during sedation as the patient is not then competent. Using a form can be helpful to summarise and agree the planned treatment and confirm communication. It is especially important in hospital practice when a patient is very likely to be seen by multiple health care professionals along their care pathway. Although a signature on a form is important in verifying that a patient has given consent, it is the discussions that take place with the patient that determine whether the consent is valid and these should be recorded in the medical records. Patients might want to know options for treatment, the risks and the potential benefits; why a particular treatment is necessary and appropriate for them; the consequences, risks and benefits of the treatment proposed; the likely prognosis; the cost of the proposed treatment. The GDC would expect dentists to provide such information in written form when sedation or general anaesthesia is required for patient care.9 NICE 112 recommends obtain and documenting informed consent for sedation and we found excellent agreement with this in practice.
A large proportion (82%) of dentists worked as operator and sedationist which is common practice in dentistry when the emphasis has been conscious sedation with basic techniques. The majority of dentists had an appropriately trained assistant. Training was described as being provided by CDSN, SAAD, other course, and in-house. NICE 112 recommends that an assistant trained in delivering and monitoring sedation in available during the sedation. This has been recommended by numerous dental sedation reports previously and we found that this practice was being adhered to by the majority.
Frequency of sedation for young people and types of sedation
A similar number of dentists reported sedating young people aged 12–18 years and young people under 12 years of age. A small proportion of our sample (12%) was sedating more than 100 young people aged 12–18 years and a similar small proportion (9%) was sedating more than 100 young people under 12 years of age. Patients aged 12–18 years show a wide range of psychological maturity and cooperation for dental treatment. This must be assessed by the dental team in determining the appropriate management strategy. Many can be treated in the same way as adults and certainly require adult drug doses given that their physiological reserve is similar to adults. Others however do require special management and this may even include general anaesthesia.
Similar number of respondents were providing advanced sedation techniques for young people aged 12–18 years and young people under 12 years of age. A very small number (5%) were providing advanced sedation for more than 100 young people aged 12–18 years and the same number (5%) were providing advanced sedation for more than 100 young people under 12 years of age. Similar drugs were used for these two different age ranges and a similar number of dentists were using each of these for the different age ranges except for midazolam. Similar numbers were used for nitrous oxide, opioid, propofol, ketamine and sevoflurane sedation. Nitrous oxide with oxygen alone is described as a basic rather than advanced technique but in this context is described as advanced as it was being used in combination with another drug or drugs in addition to oxygen. Forty percent of respondents had used midazolam for sedation in young people aged 12–18 years but only 16.5% used midazolam for those aged under 12 years of age. While there are many techniques available there is insufficient high quality evidence comparing the efficacy of one with another.15,16 This is acknowledged in the NICE 112 guidance. The IEGTSSD consider that continuing access to a range of effective and safe sedation techniques is necessary in order to provide appropriate care for patients who are unable to tolerate treatment without sedation and also to avoid the unnecessary use of general anaesthesia.17 NICE also indicate that some procedures are very common and that healthcare providers need to understand under which circumstances either sedation to anaesthesia is most cost effective. The guidance also recognises that a failed and abandoned sedation caused distress for the young person or child, delay in treatment while arranging anaesthesia and greater cost.
Monitoring and resuscitation equipment
Pulse oximetry was used by 76% of respondents and NIBP by 50%. Fewer used other types of monitoring equipment with only 5% using ECG or BIS, and 4% using capnography. It is usual practice to use clinical monitoring of sedation and minute volume by observation of a reservoir bag with nitrous oxide sedation. As contemporary machines do not permit administration of less than 30% oxygen and nitrous oxide does not impair respiration then pulse oximetry monitoring would not offer any useful information and is not recommended. Pulse oximetry and other forms of monitoring would only be used if a patient was sufficiently medically compromised to warrant monitoring during dental treatment as might also be used for treatment under local anaesthesia alone.6 NIBP is not recommended as monitoring when sedating with nitrous oxide or midazolam as a single drug unless a patient is hypertensive as baseline assessment. ECG is only recommended when appropriate to the patient medical compromise. BIS is a useful tool to measure and record level of unconsciousness during general anaesthesia but is less helpful when using conscious sedation.
NICE 112 recommends monitoring oxygen saturation during moderate sedation in addition to clinical monitoring of sedation depth, respiration, pain, coping and distress. Electrocardiogram, capnography and blood pressure are only recommended during deep sedation. We found very good compliance against this standard.
The majority of respondents (84%) kept a written or electronic sedation record which is good practice and advised by NICE 112. Only 3% reported not keeping such a record. There is no justification for not keeping a record. The majority of sedationists (86%) reported having immediate access to resuscitation equipment and 2% stated that they did not. It is mandatory for all sedationists to have immediate access.
Sedation efficacy
The purpose of using a basic or advanced sedation technique is to enable dental treatment to be carried out that would otherwise not be able to be carried out. On some occasions the treatment may need to be abandoned because of inadequate cooperation.18 Sixty-seven percent of sedationists reported that they were unable to complete treatment under sedation for under 10% of children and young people during the previous year. This indicates that treatment was completed successfully in more than 90% of cases which is excellent. A single sedationist reported being unable to complete treatment in over 50% children and young people which seems extraordinary and we wonder whether this could be a misunderstanding of the question by that practitioner. A small number (7%) of sedationists reported inability to complete treatment for 10–20% of patients. The majority (61%) of these abandoned cases were scheduled for completion of treatment with general anaesthesia. Others (9%) referred to a psychologist or (8%) scheduled for an advanced sedation technique. Another 15% indicated alternative management and were invited to specify but did not do so. Sixty-one percent of sedationists indicated that they audited their service. Audit is an important tool in improving the quality of service and patient care. Isolated 'audits' are usually undertaken and audit practice is becoming part of the culture of healthcare especially the NHS although is relatively new and there are not universal data collection systems in place to capture information readily. While a failed sedation is unfortunate for the reasons described above, a 90% success rate would seem very reasonable.
Opinion of appropriate person and setting for young person sedation
Forty-nine percent of respondents were of the opinion that a dentist was an appropriate person to provide advanced sedation techniques for 12–18-year-old young patients and 11% were of the opinion that this should be a doctor. 27.5% specified that an anaesthetist was the appropriate person. When asked the same question about advanced sedation for patients less than 12 years of age then the number indicating dentist reduced to 24% and also reduced for doctor 0.5%, but significantly increased for anaesthetist (75%). Decision making and opinion about which is the most appropriate professional to provide particular types of patient care is complex and may take into account the principals of scope of practice, history, attitudes and professional protectionism among other factors. Ninety-five percent of our sample were dentally qualified and 4% were medically qualified with 2% holding both qualifications. The contemporary view of the GDC is that an individual should only carry out a task or type of treatment for which that individual has been appropriately trained, demonstrated competence for has indemnity. It is anticipated that individuals may expand their scope of practice by developing new skills, developing knowledge in particular areas and choosing more specialist practice. Clearly the view of the respondents was a preference for sedation by an anaesthetist for advanced sedation of children under 12 years of age.
When asked about opinion of the most appropriate setting for advanced sedation techniques, 33% indicated primary care, 37.5% indicated salaried services, and 68% secondary care services. Opinion changed a little when asked about advanced sedation techniques for those under 12 years of age to 20% for primary care, 27% for salaried services and 76% for secondary care. Interestingly, there was significant support for primary care to be maintained for under 12-year-olds even though there was a preference for an anaesthetist to provide the service. Primary health care provides the first point of contact in the health care system. In the NHS, the main source of primary health care is general practice. Secondary care is the health care services provided by specialists and other health professionals who generally do not have first contact with patients. The 'secondary care' is sometimes used synonymously with 'hospital care'. However many secondary care providers do not necessarily work in hospitals, such as Specialists in Oral Surgery or Consultants in Special Care Dentistry. There is some evidence of this style of delivery of sedation services for dentistry. Depending on the organisation and policies of the national health system, patients may be required to see a primary care provider for a referral before they can access secondary care. The United States operates under a mixed market health care system, some physicians might voluntarily limit their practice to secondary care by requiring patients to see a primary care provider first, or this restriction may be imposed under the terms of the payment agreements in private/group health insurance plans. In other cases medical specialists may see patients without a referral, and patients may decide whether self-referral is preferred. In the UK and Canada, patient self-referral to a medical or dental specialist for secondary care is rare as prior referral from another physician (either a primary care physician or dentist) is considered necessary, regardless of whether the funding is from.
Respondents opinion about appropriate management of under 12-year-olds
We asked, 'Which of the following do you consider to be the appropriate management strategy for children aged 12 or under who cannot be managed under local anaesthetic with either nitrous oxide/oxygen or midazolam alone?'. The most common response was to schedule general anaesthesia (61%) but a similar number suggested arranging advanced sedation care (54.5%). A smaller number suggested arranging cognitive-behavioural therapy (37%). These figures were a little different when compared with an earlier question in the survey asking about how sedationists would manage those under 19 years of age at 'first attempt'. Only 8% indicated referral to psychologist although it is reasonable for this figure to increase if pharmacological basic sedation has been attempted and failed. Similarly, only 8% suggested advanced sedation initially but would after failure be more inclined to recommend this. A similar number indicated general anaesthesia.
Discussion summary
NICE 112 advises that for a child or young person, their parent or carer to make an informed decisions they should have been offered verbal and written information describing the proposed technique and alternatives and associated risks and benefits. We found excellent agreement with this standard and also with documentation of informed consent.
NICE 112 recommends monitoring oxygen saturation during moderate sedation in addition to clinical monitoring of sedation depth, respiration, pain, coping and distress. Electrocardiogram, capnography and blood pressure are only recommended during deep sedation. We found very good compliance against this standard.
The majority of respondents (84%) kept a written or electronic sedation record. Only (3%) reported not keeping such a record. We found that the majority (86%) of respondents confirmed that they complied with life support training expectations but it is of concern that there were a small number who did not. The majority of sedationists (86%) reported having immediate access to resuscitation equipment but not all.
On some occasions dental treatment may need to be abandoned because of inadequate cooperation. Sixty-seven percent of sedationists reported that they were unable to complete treatment under sedation for fewer than 10% of children and young people during the previous year. This indicates that treatment was completed successfully in more than 90% of cases which is excellent. On abandoning a sedation technique, 61% said they would schedule general anaesthesia and 54.5% said they would schedule advanced sedation care.
Sixty percent of respondents were of the opinion that a dentist was an appropriate person to provide advanced sedation techniques for 12–18-year-old young patients, but only 24% thought that this was appropriate for patients under 12 years of age, with 75% preferring an anaesthetist. When asked about opinion of the most appropriate setting for advanced sedation techniques, 33% indicated primary care, 37.5% indicated salaried services, and 68% secondary care services. Opinion changed a little when asked about advanced sedation techniques for those under 12 years of age to 20% for primary care, 27% for salaried services and 76% for secondary care. Interestingly, there was significant support for primary care to be maintained for those under 12-years-old even though there was a preference for an anaesthetist to provide the service.
Conclusions
Our data support the view that most sedation delivery in dentistry was compliant with NICE 112 recommendations on training, assessment, consent, monitoring and efficacy.
References
The Wylie report. Report of the working party on training in dental anaesthesia. Br Dent J 1981; 151: 385–388.
National Institute for Health and Care Excellence. Sedation in children and young people: sedation for diagnostic and therapeutic procedures in children and young people. 2010. Online information available at https://www.nice.org.uk/guidance/cg112 (accessed March 2015).
Independent Expert Group on Training Standards for Sedation in Dentistry. Advanced conscious sedation techniques for adult dental patients. Society for the Advancement of Anaesthesia in Dentistry, 2011. Online information available at http://www.saad.org.uk/wp-content/uploads/2012/11/Adult-Sylabus-Text-Cropped.pdf (accessed March 2015).
Independent Expert Group on Training Standards for Sedation in Dentistry. Advanced conscious sedation techniques for paediatric dental patients. Society for the Advancement of Anaesthesia in Dentistry, 2011. Online information available at http://www.saad.org.uk/wp-content/uploads/2012/11/Paediatric-syllabus-for-website.pdf (accessed March 2015).
Department of Health. Conscious sedation in the provision of dental care: report of an expert group on sedation for dentistry. Standing Dental Advisory Committee, 2003. Online information available at http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4074705.pdf (accessed March 2015).
Royal College of Anaesthetists. Standards for Conscious sedation in dentistry: alternate techniques. Standing Committee on Sedation for Dentistry, 2007. Online information available at https://www.rcseng.ac.uk/fds/publications-clinical-guidelines/docs/SCSDAT%202007.pdf (accessed March 2015).
Dental Sedation Teachers Group. Conscious sedation in dentistry: standards for postgraduate education. 2008. Online information available at http://www.saad.org.uk/wp-content/uploads/2012/11/dstg-pg-standards.pdf (accessed March 2015).
Dental Sedation Teachers Group. Sedation in dentistry: undergraduate training. 2012. Online information available at http://www.dstg.co.uk/sedation-in-dentistry-undergraduate-training/ (accessed March 2015).
Resuscitation Council UK. Medical emergencies and resuscitation: standards for clinical practice and training for dental practitioners and dental care professionals in general dental practice. 2006, revised 2012. Online information available at http://www.resus.org.uk/pages/medental.htm (accessed March 2015).
General Dental Council. Standards for the dental team. 2013. Online information available at http://www.gdc-uk.org/Dentalprofessionals/Standards/Pages/standards.aspx (accessed March 2015).
Coulthard P, Bridgman C, Gough L, Longman L, Pretty I A, Jenner T . Estimating the need for dental sedation – paper 1. The indicator of sedation need (IOSN) - a novel assessment tool. Br Dent J 2011; 211: E10.
Pretty I A, Goodwin M, Coulthard P, Bridgman C, Gough L, Sharif M O . Estimating the need for dental sedation - paper 2: Using IOSN as a health needs assessment tool. Br Dent J 2011; 211: E11.
Goodwin M, Coulthard P, Pretty I A, Bridgeman C, Gough L, Sharif M O . Estimating the need for dental sedation - paper 4. Using IOSN as a referral tool. Br Dent J 2012; 212: E9.
Coulthard P . The indicator of sedation need. SAAD Digest 2012; 28: 9–12.
Lourenço-Matharu L, Ashley P F, Furness S . Sedation of children undergoing dental treatment. Cochrane Database Syst Rev 2012; 3: CD003877.
Ashley P F, Williams C E C S, Moles D R, Parry J . Sedation versus general anaesthesia for provision of dental treatment in under 18 year olds. Cochrane Database Syst Rev 2012; 11: CD006334.
Independent Expert Group on Training Standards for Sedation in Dentistry. A guide to maintaining professional standards in conscious sedation for dentistry. Society for the Advancement of Anaesthesia in Dentistry, 2011. Online information available at http://www.saad.org.uk/wp-content/uploads/2012/11/CPD-Document-Text-Cropped.pdf (accessed March 2015).
Hosey M T, UK National Clinical Guidelines in Paediatric Dentistry. Managing anxious children: the use of conscious sedation in Paediatric Dentistry. Int J Paediatr Dent 2002; 23: 359–372.
Acknowledgements
This study was undertaken by IEGTSSD and was funded by the SAAD, 21 Portland Place, London, W1B 1PY.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Coulthard, P., Craig, D., Holden, C. et al. Current UK dental sedation practice and the 'National Institute for Health and Care Excellence' (NICE) guideline 112: sedation in children and young people. Br Dent J 218, E14 (2015). https://doi.org/10.1038/sj.bdj.2015.338
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.338
This article is cited by
-
The Path to Safety in Dental Anesthesia
Current Anesthesiology Reports (2024)
-
Recommended procedures for the management of early childhood caries lesions – a scoping review by the Children Experiencing Dental Anxiety: Collaboration on Research and Education (CEDACORE)
BMC Oral Health (2020)
-
Carers’ and paediatric dentists’ perceptions of children’s pain during restorative treatment
European Archives of Paediatric Dentistry (2020)
-
Conscious sedation: is this provision equitable? Analysis of sedation services provided within primary dental care in England, 2012–2014
BDJ Open (2016)