Key Points
-
Investigates the current use and knowledge of the index of orthodontic treatment need (IOTN) in Scotland and evaluates changes in patterns prior to mandatory introduction in 2011.
-
Assesses the factors which influence use and knowledge of IOTN.
-
Makes recommendations for the implementation of the index into clinical practice.
Abstract
Objectives To evaluate the use and knowledge of the index of orthodontic treatment need (IOTN) by general dental practitioners (GDPs) working within Scotland.
Setting Scottish general dental services (SGDS).
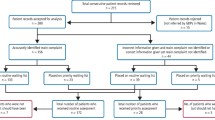
Methods Questionnaires were posted to randomly selected dentists (n = 356) working within the SGDS for self-completion and return.
Main outcome measures Use of IOTN.
Knowledge of IOTN Participants were asked to match 12 malocclusions to the correct IOTN category. Kappa statistics evaluated agreement to a gold standard.
Results The overall response rate was 64%. Sixty-one percent of respondents did not use IOTN. The most common reason for using the index was to assess treatment eligibility (40.2%). The main reason for non-use was that it was only considered suitable for secondary dental care (27%). Over half (56%) of respondents had received IOTN training at undergraduate level. Knowledge of the index was found to be low - the mean level of agreement was k = 0.42 (fair). 10.5% of respondents scored k ≥0.61(substantial). The factors most likely to contribute to both use and knowledge of IOTN were having a postgraduate qualification and carrying out orthodontic treatment in practice.
Conclusion Overall use and knowledge of IOTN among GDPs in Scotland appears to still be low. More resources need to be directed towards improving both undergraduate and postgraduate orthodontic training with the focus on IOTN in particular.
Similar content being viewed by others
Introduction
Oral health can be defined as the standard of health of the oral and related tissues which enables an individual to eat, speak and socialise without active disease, discomfort or embarrassment and which contributes to general well-being.1
Malocclusion is an important contributor to oral health but differs from the majority of medical and dental conditions in that it is a spectrum of dental deviations, rather than a disease, and orthodontic treatment does not cure a condition but rather corrects variations from an arbitrary norm.2
Deciding on a cut-off point as to where a specific malocclusion should be treated has been the subject of much dispute.3 However, rational planning, assessing and allocating the resources required for orthodontic intervention is essential, particularly where such resources are finite and publically funded. The current method in use within the UK to allocate orthodontic services is the index of orthodontic treatment need (IOTN).4 In Scotland, those scoring IOTN grade three (dental health component) combined with grade six (aesthetic component) and above, can be considered for treatment under Scottish general dental services (SGDS) arrangements. The index became a mandatory part of NHS dental services in England and Wales in April 2006, with NHS Scotland implementing it in October 2011. It is estimated that 90% of dental care takes place in general dental practices in Scotland, with the remaining (10%) in specialist or secondary care services.5 As a result, the majority of orthodontic treatment is carried out following initial referral from general dental practitioners (GDPs).
IOTN's implementation in Scotland had two aims: to allocate finite orthodontic treatment resources to those most in need, and to provide a consistent metric for general dentists when referring patients for NHS orthodontic treatment.
The provision of orthodontic treatment is highly reliant on appropriate referrals, however, little information exists to evaluate whether dentists use IOTN post-implementation, or whether they have sufficient knowledge to do so. This is despite the promise of relevant training being made available.6 Given the role of GDPs as 'gatekeepers' in recommending for specialist treatment, it is important to evaluate if they can correctly score IOTN grades to initiate an appropriate referral. Quantifying this information may indicate the use and perceived usage of IOTN in a general practice setting, highlighting the need for further resources allocated to awareness and training.
Aims of the study
-
To evaluate the current use and knowledge of IOTN by GDPs in Scotland
-
To assess changes in patterns of use after mandatory introduction in 2011
-
To investigate which factors, if any, influence the use and knowledge of IOTN by GDPs.
Materials and methods
A self-completed questionnaire was designed and posted to GDPs working within Scotland (Appendix 1). Two pilot surveys were carried out to test for face and content validity of the questionnaire. Minor changes were subsequently made and the final questionnaire was sent to randomly selected GDPs working within the SGDS. The study was carried out from 30 September until 23 December 2013. The methods, conduct and design of the survey were informed by evidence based methodology.7,8
Ethical approval
Advice was sought from the East of Scotland Research Ethics Service, which indicated that no ethical approval was required for this study.
Questionnaire design
The questionnaire consisted of four sections. Section one investigated the current use of IOTN, specifically reasons for use or non-use; questions were included to allow direct comparison with a previous questionnaire conducted before mandatory introduction.9 Section two aimed to evaluate dentists' agreement with the IOTN's Dental Health Component (DHC) and their ability to allocate patients into the correct treatment need category. Twelve statements describing various malocclusion features were taken from the DHC of IOTN. The grades were removed and the various statements were arranged in a random order. Participants were asked to classify each malocclusion into the correct treatment need category from one to five, where grade one indicated no need for treatment and grade five indicated a great need for treatment. Section three examined previous training in IOTN and opinions on future training. Section four collected demographic information relating to the professional background of the respondents; participants were further able to provide any additional comments in a free-text response format.
Sampling
Permission was granted by the Practitioners Services Division, NHS Scotland, for a distribution list of all dental practitioners (n = 3,033) within Scotland to be accessible to the chief investigator (AP). This formed a sample frame. From this list the following were excluded: those who had already taken part in related pilot studies and those who were listed as practitioners restricted to orthodontic practice. A sample size of 356, based on a previous study was estimated.9 This was set to detect an 8% prevalence of use. The assumption that there would be no reduction in IOTN use since mandatory introduction was made.
Computer software (Excel 2007) was used to randomise the SGDP list order and then randomly select the 356 potential respondents. In order to conceal the allocation of participants, a researcher independent to this study carried this out.
Each questionnaire was given a code so that non-respondents could be targeted for a follow-up contact. This included postage of a reminder letter and a copy of the questionnaire. All respondent questionnaires were anonymous.
Statistical analysis
Data were extracted manually from the returned questionnaires and entered into SPSS software (version 19) for statistical analysis.
Simple descriptive statistics (frequencies and percentages) were used to determine the distribution and range of GDPs' responses to each question. For comparison of two or more categorical variables, the chi-square test was used. For continuous variables, comparison of the means between two groups was by use of a Student t-test; and for three or more groups one way analysis of variance (ANOVA) was used. The significance level of p <0.05 was used in all tests.
Knowledge of IOTN was determined by asking participants to allocate various malocclusion features into the correct treatment need category, as determined by the DHC of IOTN. The scores were compared against the gold standard previously established by the consensus of orthodontists who developed the index.4,10 Cohen kappa statistics were calculated for each dentist to assess the level of agreement from their scores compared to the gold standard. This was termed the 'IOTN knowledge score'. The Cohen's kappa represents the proportion of agreement over and above chance alone.
Binary logistic regression analysis was conducted in order to determine factors influencing the use of IOTN, giving odds ratios. Multiple linear regression analysis was used to reveal factors which best explained knowledge level of IOTN.
Results
A total of 231 questionnaires were returned, giving an overall response rate of 65%.
Respondent demographics
Out of the total respondents, 125 (54%) were male, and 106 (46%) were female. The majority of respondents were most likely to have qualified from one of three Scottish universities: Glasgow (n = 94, 41%), Dundee (n = 63, 27%) and Edinburgh (n = 24, 10%) (Fig. 1). The range for time in practice was between 1–43 years. More than one third of respondents (n = 81, 35%) had obtained their primary qualification within the last ten years.
Overall, 28% of respondents had a postgraduate qualification; the most commonly held postgraduate qualification (81%) was a diploma from one of the Royal Colleges. The remainder tended to be in the form of a Master's degree from a university.
The majority of respondents carried out mainly NHS dental work (n = 125, 54%); 37% (n = 85) carried out a mixture of NHS and private dental work, and 9% (n = 21) of respondents carried out mainly private work.
Only 17% (n = 40) of respondents said they carried out some orthodontic treatment in their practice. For the majority, this was in the form of simple treatment normally involving a removable appliance (n = 30, 16%). Ten GDPs (5%) said they provided private orthodontic techniques, such as Invisalign®, Inman aligners® and 6-Month Smiles®.
Use of IOTN
Most respondents did not use IOTN (n = 142, 61%), while 39% (n = 89) said they did. The most frequently reported reason for using IOTN was to assess eligibility for treatment (n = 66, 40.2%). Other reported reasons were for communication with patients (n = 39, 24%); inter-colleague communication (n = 34, 21%) and assessing case complexity (n = 25, 15%) (Fig. 2).
The most common reported reason for not using the index was that it was only suitable for secondary care (n = 65, 27%). Twenty-one percent of respondents reported they did not have the necessary training. Other reasons for not using IOTN were due to the fact that no fee was provided; other procedures took priority; it was too complex or too time consuming to use. Four dentists said they had never heard of IOTN (Fig. 3).
Training
The majority of dentists had received previous training in using IOTN (n = 134, 58%), mainly obtained during undergraduate dental school (n = 106, 63%). Other methods were through attending a course on the index; via journals or online literature searches or from a visiting local orthodontic practitioner. The majority of respondents felt there should be more training in IOTN (74%). GDPs were further asked what methods they considered would most encourage use. Most felt there should be more courses available (n = 100, 37%). Others wanted better publicity for existing courses and more educational material available online. Free text responses from four GDPs recommended having IOTN posters up in surgeries to encourage further use of the index.
Knowledge of IOTN
All respondents completed this section and subsequently no adjustment for missing data was necessary. There was a wide range of performance among respondents: the mean kappa (IOTN knowledge score) for all respondents was 0.416, with a range of -0.15–1. Based on the guidelines from Landis and Koch,11 a kappa of 0.416 represents a fair to moderate strength of agreement. The percentage of respondents with a substantial agreement (0.61 or above) was 10.5%. Seven respondents (3%) had a kappa value of less than zero, indicating no agreement (Fig. 4).
Factors likely to promote use of IOTN
The use of the IOTN and the knowledge score were cross tabulated against GDP characteristics, specifically: gender, year qualified, dental school, type of treatment undertaken, previous training in IOTN, postgraduate qualifications and whether orthodontic treatment was carried out. It was found that gender, undergraduate training, years qualified and type of treatment provided had no statistically significant relationship with both use and overall knowledge of the IOTN (p >0.05).
The two variables in the logistic analysis that were found to have a significant effect on the use of IOTN were:
-
Whether or not the GDP had a postgraduate qualification - GDPs with a postgraduate qualification were more than twice as likely to use IOTN
-
Whether orthodontic treatment was done in the practice – these GDPs were more than four times as likely to use the index if they carried out some form of orthodontics in practice (Table 1).
Three variables were found which best explained the level of IOTN knowledge were whether or not the GDP carried out orthodontic treatment; had a postgraduate qualification and used IOTN (Table 2).
Discussion
High response rates generate accurate and reliable results to surveys - response rates of over 70% are desirable. Low response rates may be related to questionnaire topics which are perceived as irrelevant, and tend to yield a lower response rate than those judged 'salient'.12
It is contended that the 65% overall response rate in this survey does provide an acceptable representation from the selected sample, given the salience of the topic.7,8,9 This is also a significant (20%) improvement in response rate versus the pre-introduction survey and may indicate an increased level of salience within the SGDS.9,13,14,15,16,17 The results from this study indicate relatively low penetration of IOTN in SGDS, with only 38.5% of GDPs reporting ever using the index.
These figures compare less favourably to those obtained from surveys conducted in secondary and tertiary care;14,15,16 however, an improvement has been found upon comparison to surveys carried out in primary dental care previously.9,17 In particular, the 2003 national Scottish survey estimated only 10% of GDPs used IOTN and a significant 48% had never heard of it. Additionally, a West Sussex survey found only 5.7% of GDPs reported always using the index, 17% often using it and 5.2% had never heard of it.9,17 Logically, the most likely factor increasing use is the introduction of mandatory use for SGDS eligibility in Scotland in 2011. Furthermore, there appears to be an enhanced awareness of dental aesthetics among the public, together with the greater acceptability for orthodontic appliances. This has resulted in higher demands being placed upon the limited resources of publicly funded systems of care.18
When the index was used, it tended to be for one of its core purposes - the assessment of eligibility for publically funded orthodontic treatment (40.2%). Approximately 15% of GDP respondents inappropriately used IOTN to grade case complexity; this continues to be a persistent issue.
When asked why IOTN was not used, the majority of respondents said it was only suitable for use after referral (27%) indicating that someone else should carry out the grading, thereby exhibiting evidence of abdicating the 'gatekeeper' role. This is consistent with previous findings.13
Knowledge of the IOTN was found to be low. The mean kappa for all respondents was 0.41, indicating only a fair to moderate agreement. Only 10.5% of respondents were found to have a kappa score of 0.61 (substantial agreement) or above. Again, these results do not significantly differ from previous studies which have found generally low orthodontic knowledge among GDPs.17
The main factors which appeared to contribute to higher knowledge and use of the index were whether or not the GDP had a postgraduate qualification and unsurprisingly, whether or not any orthodontic treatment was carried out within practice.
The most commonly held postgraduate qualification by GDPs tended to be in the form of a diploma qualification from one of the Royal Colleges of Surgeons. These qualifications are based on the document 'A curriculum for UK dental foundation programme training', which informs the requirement of individuals to be competent in carrying out an orthodontic assessment using IOTN. It is predicted that this qualification should have resulted in improved knowledge and confidence in the use of occlusal indices, which was perhaps not achieved during undergraduate training.
Access to and participation in postgraduate education has been found to have a similar value in promoting use versus remuneration or imposed use.9 Previous undergraduate training, years since qualification and dental school of training did not appear to have a statistically significant effect on the use and knowledge of the IOTN. This may support the contention that undergraduate training alone is not sufficient to enable the confident clinical application of orthodontic skills, that resources should be directed at improving undergraduate training and in the provision of postgraduate education.
In relation to orthodontics being undertaken within practice, a total of 17% of GDPs said they carried out such treatment. The majority of these treated less than ten patients per year, and most used removable appliances. However, a small number of GDPs reportedly provided commercial, privately funded orthodontic techniques, such as Invisalign®, Inman aligners® and 6-Month Smiles®. Individuals carrying out such treatment will have been expected to attend various certified commercial or corporate courses, which should have increased awareness in assessment, diagnosis and eligibility for orthodontic treatment. However the focus of these courses will naturally be on the commercial aspects of whichever system they are promoting and not on eligibility for NHS orthodontics.
Previous studies have also promoted the dissemination of orthodontic guidelines to help improve the competence skills in orthodontic assessment and diagnosis before referral.17,19 The currently available orthodontic guidelines have perhaps failed to reach at least one of their target groups.22,23
Conclusions
-
The current use of IOTN among GDP's in Scotland appears to be low. In addition, knowledge relating to overall orthodontic treatment need was less than satisfactory, with only 10.6% of GDP's conforming to the gold standard
-
While there is an increase in the perceived salience of IOTN compared to previous studies, presumably due to mandatory introduction, GDPs continue to place a relatively low value on the utility of it; most prefer a specialist to make the necessary grading. This seems to relate to a continued lack of general orthodontic knowledge
-
Previous undergraduate training, years since qualification and dental school of training did not appear to have a statistically significant effect on the use and knowledge of the IOTN
-
There appears to be an explicit value in formal, non-commercial, dental postgraduate education which positively impacts on applied knowledge, enhancing the engagement of GDPs with IOTN use.
Commentary
In the current political climate, we are constantly being told of the 'difficult economic times' in which we live. NHS resources are 'at crisis point' and efficiency appears to be the watchword of the day. As such, it is important that there are clear criteria for referral to specialist care services and access to treatment for these cases. However, the value of these criteria are only useful if used appropriately by the gatekeepers of these services, the general dental practitioner. The IOTN has been in use for over 25 years and is an integral part of undergraduate orthodontic teaching. In order to ensure that resources are directed to the patients most in need, it is important that the GDP is fully aware of IOTN. Failure in this would lead to unnecessary referrals to NHS services, loading an already stretched budget. Currently, it may only be necessary for the GDP to know that a patient with an IOTN of 3.6 is eligible for NHS funded treatment but in the advent of managed clinical networks, a more nuanced understanding of which cases can be seen in specialist practice and which are appropriate for hospital services may become necessary.
In this article, the authors ask a very important question, which is relevant to all secondary care services. If the gatekeepers are unsure of when to 'open the door', how useful are these referral criteria, particularly when all children have the right to an NHS orthodontic consultation. Steps such as the recent orthodontic themed issue of the BDJ will help raise awareness as well as articles such as these. Our instinct may be to institute training courses and CPD events but with increasing mandatory and strongly recommended CPD in medical emergencies, radiography, infection control, ethics, complaints, safeguarding and oral cancer screening, it is all too easy to see how orthodontic referral criteria drops down the to-do list.
The authors of this paper have raised some very important issues regarding the role of GDPs within our future orthodontic provision and, like most good research, have probably left us with more questions than answers.
Sameer Patel Specialty Registrar Eastman Dental Hospital UCLH NHS Foundation Trust.
Author questions and answers
1. Why did you undertake this research?
The IOTN became a mandatory part of NHS dental services in England and Wales in April 2006, with NHS Scotland implementing it in 2011. General dental practitioners have a vital role in acting as 'gatekeepers' in referring for specialist treatment, however little information is available to evaluate if they can correctly score IOTN grades to initiate an appropriate referral.
2. What would you like to do next in this area to follow on from this work?
In future it may be beneficial to review any trends in GDPs' awareness and attitude towards orthodontic screening, particularly for publically funded orthodontic services within Scotland and the UK as a whole. One interesting finding in this study was the number of GDPs providing alternative private orthodontic treatment for adult patients. This is an area that may well continue to grow in the future and studies could investigate this type of treatment modality in relation to previous orthodontic training, as well as its impact on GDP referral patterns. Finally, due to the relatively poor penetration of the IOTN into general dental services, future studies could investigate the most useful and effective methods to improve adoption of guidelines into day-to-day clinical practice. This would allow the appropriate strategies to be put into place to allow for a more efficient, transparent and robust healthcare system.
References
Department of Health. An oral health strategy for England. 1994. Online information available at http://webarchive.nationalarchives.gov.uk/+/dh.gov.uk/en/publicationsandstatistics/publications/publicationspolicyandguidance/dh_4123251 (accessed March 2015).
O'Brien C, Benson P E, Marshman Z . Evaluation of a quality of life measure for children with malocclusion. J Orthod 2007; 34: 185–193.
Turbill E A, Richmond S, Wright J L . A critical assessment of high-earning orthodontists in the General Dental Services of England and Wales (1990–1991). Br J Orthod 1998; 25: 47–54.
Brook P H, Shaw W C . The development of an index of orthodontic treatment priority. Eur J Orthod 1989; 11: 309–320.
NHS Quality Improvement Scotland. National standards for dental service 2006. Online information available at: http://www.healthcareimprovementscotland.org/previous_resources/standards/standards_for_dental_services.aspx (accessed March 2015).
Scottish Government Health Directorates. Index of orthodontic treatment need update. 2011. Online information available http://www.psd.scot.nhs.uk/professionals/dental/news/index-of-orthodontic-treatment-need.html (accessed March 2015).
McColl E, Jacoby A, Thomas L et al. Design and use of questionnaires: a review of best practice applicable to surveys of health service staff and patients. Health Technol Assess 2001; 5: 1–256.
Edwards P, Roberts I, Clarke M et al. Increasing response rates to postal questionnaires: systematic review. Br Med J 2002; 324: 1183–1185.
Ho-A-Yun J, Crawford F, Clarkson J . The use of the Index of Orthodontic Treatment Need in dental primary care. Br Dent J 2009; 206: 418–9.
Richmond S, Shaw, WC, O'Brien K D et al. The relationship between the index of orthodontic treatment need and consensus opinion of a panel of 74 dentists. Br Dent J 1995; 178: 370–374.
Landis J R, Koch G G . The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–174.
Heberlein T A, Baumgartner R . Factors affecting response rates to mailed questionnaires: a quantitative analysis of the published literature. Am Sociol Rev 1978; 43: 447–462.
Fleming P S, Dowling P A . A survey of undergraduate orthodontic training and orthodontic practices by general dental practitioners. J Ir Dent Assoc 2005; 51: 68–72.
De Oliveira C M . The planning, contracting and monitoring of orthodontic services, and the use of the IOTN index: a survey of consultants in dental public health in the United Kingdom. Br Dent J 2003; 195: 704–706.
Willmot D R, Dibiase D, Birnie D J, Heesterman R A . The Consultant Orthodontists Group survey of hospital waiting lists and treated cases. Br J Orthod 1995; 22: 53–57.
Holmes A, Willmot D R . The Consultant Orthodontists Group 1994 survey of the use of the Index of Orthodontic Treatment Need (IOTN). Br J Orthod 1996; 23: 57–59.
Jackson O A, Cunningham S J, Moles D R, Clark JR . Orthodontic referral behaviour of West Sussex dentists. Br Dent J 2009; 207: 430–431.
Holmes A . The subjective need and demand for orthodontic treatment. Br J Orthod 1992; 19: 287–297.
O'Brien K, Wright J, Conboy F et al. Orthodontics: the effect of orthodontic referral guidelines: a randomised controlled trial. Br Dent J 2000; 188: 392–397.
Grimshaw J M, Thomas R E, MacLennan G et al. Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess 2004; 8: 1–72.
General Dental Council. The first five years. Second edition 2002; third edition 2008. Online information available at http://www.gdc-uk.org/Aboutus/education/Documents/TheFirstFiveYears.pdf (accessed March 2015).
British Orthodontic Society. Guidelines for referrals for orthodontic treatment. 2008. Online information available at http://www.chapelroad.co.uk/PDF%27s/Appendix%203%20-%20Guidelines-for-referrals.pdf (accessed March 2015).
Royal College of Surgeons. Clinical guidelines. Online information available at https://www.rcseng.ac.uk/fds/publications-clinical-guidelines/clinical_guidelines (accessed March 2015).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Puri, A., Ho-A-Yun, J. & McGuinness, N. Use and knowledge of IOTN among GDPs in Scotland. Br Dent J 218, 399–404 (2015). https://doi.org/10.1038/sj.bdj.2015.247
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.247
This article is cited by
-
Helping general dental practitioners use the Index of Orthodontic Treatment Need: an assessment of available educational apps
British Dental Journal (2023)
-
Expert view: Kathryn Derringer
British Dental Journal (2022)
-
An investigation into the reliability of a mobile app designed to assess orthodontic treatment need and severity
British Dental Journal (2022)
-
Can dental registrants use the Index of Orthodontic Treatment Need accurately? Part 2. Factors influencing knowledge of IOTN among dental registrants
British Dental Journal (2016)
-
Orthodontic referrals: why do GDPs get it wrong?
British Dental Journal (2016)