Key Points
-
Describes the factors that influence stability following orthodontic treatment.
-
Explains the rationale and evidence for orthodontic retention and the various types of orthodontic retainers.
-
Outlines how general dental practitioners can support their patients wearing orthodontic retainers.
Abstract
Retention is necessary following orthodontic treatment to prevent relapse of the final occlusal outcome. Relapse can occur as a result of forces from the periodontal fibres around the teeth which tend to pull the teeth back towards their pre-treatment positions, and also from deflecting occlusal contacts if the final occlusion is less than ideal. Age changes, in the form of ongoing dentofacial growth, as well as changes in the surrounding soft tissues, can also affect the stability of the orthodontic outcome. It is therefore essential that orthodontists, patients and their general dental practitioners understand the importance of wearing retainers after orthodontic treatment. This article will update the reader on the different types of removable and fixed retainers, including their indications, duration of wear, and how they should be managed in order to minimise any unwanted effects on oral health and orthodontic outcomes. The key roles that the general dental practitioner can play in supporting their patients wearing orthodontic retainers are also emphasised.
Similar content being viewed by others
Introduction
Orthodontic retention is the final stage of orthodontic treatment and aims to maintain the teeth in their corrected positions after the completion of orthodontic tooth movement. Teeth have a tendency to return towards their initial positions due to tension in periodontal fibres, particularly those around the necks of the teeth (inter-dental and dento-gingival fibres). The quality of the final occlusion will also affect the stability of the orthodontic outcome, with unwanted displacing occlusal contacts potentially leading to unfavourable changes in tooth position. Sound orthodontic treatment planning and the achievement of appropriate occlusal and soft tissue treatment goals can help to minimise orthodontic relapse. Nevertheless, some degree of relapse is almost inevitable unless a suitable retention protocol is put in place following removal of active appliances. Unfortunately, patient compliance often decreases as orthodontic treatment progresses1 and poor compliance with retention appliances can often undermine the improvements achieved during treatment. An experimental study has shown significant deterioration in corrected tooth rotations, lower incisor alignment and overjet in only four weeks when retention appliances were not used following orthodontic movement.2
Unwanted tooth movements after treatment can also occur as a result of normal age changes, even in patients who have not had orthodontic treatment. This deterioration in the alignment of their teeth is due to changes in the soft tissue pressures and skeletal structures around the dentition. These soft tissue changes and minor ongoing growth can be regarded as a part of the normal ageing process and are unpredictable. Retainers are therefore indicated not only to resist the tendency of teeth to return to their pre-treatment positions following orthodontic tooth movement, but also to resist unwanted long-term age changes.
In most orthodontic cases, retainers are therefore an essential part of orthodontic treatment. There is no evidence to suggest that the retention regimen for adults should differ from that used for adolescent patients, providing the periodontal supporting tissues are normal. Post-retention outcomes in adults have been shown to be at least as stable as those in adolescents in relation to midline alignment, overjet, overbite, molar relationship and incisor alignment.3,4 There are a small number of occlusal problems for which retention is not required. For example, after correction of posterior and anterior crossbites, the incisor overbite and posterior intercuspation may be adequate for maintaining the correction, and as a result no retention is necessary.5
The general dental practitioner (GDP) has an important role to play in reinforcing the importance of good retainer wear for patients who have completed orthodontic treatment. By supporting the advice given by the orthodontist, the GDP can help ensure that their patients achieve maximum gain from their treatment. The GDP also has a key role in helping the patient to maintain good dental health while wearing retainers (Fig. 1). If retainers are to be worn on a long-term basis then the patient will benefit from input from both the orthodontist who fitted the retainers, and the patient's GDP.
What the patient needs to know
It is important that as part of the informed consent process, patients are made aware of the limitations of orthodontic treatment and the need for retention. Relapse is unpredictable but likely, and patients should only undergo orthodontics if they are willing and capable of following the prescribed retention regimen following active treatment. The orthodontist should explain the patient's long-term responsibilities for the retention phase of their treatment, and the patient must be prepared to accept these responsibilities. Written information is often helpful when working through these issues with patients.
Types of retainers
Retainers can be broadly classified as either fixed or removable. As their name suggests, removable retainers can be removed by patients allowing them to clean fully around the teeth and to wear them on a part-time basis if indicated. However, there are some situations when retainers are required 24 hours a day every day to reduce the chances of relapse and in these situations a fixed retainer is usually required (Fig. 2). These situations will be discussed in more detail later in the article.
Removable vacuum formed retainers
Vacuum formed retainers (VFRs) are relatively inexpensive and can be quickly fabricated on the same day as appliance removal (Fig. 3). They are the retainers most commonly used by orthodontists in the UK and Ireland6 and are also becoming more popular in the USA.7 VFRs are discreet and are well accepted by patients from an aesthetic and comfort perspective.8,9,10,11 There is also evidence that VFRs are more cost-effective and better at retaining the alignment of the anterior teeth than Hawley-type retainers although the sizes of the differences are small.8,12 They can be modified to produce minor active tooth movements if required and prosthetic teeth can be incorporated in cases with hypodontia. Full posterior occlusal coverage, including the most distal molars, is advisable in order to reduce the risk of over-eruption of these teeth during retention.13 It is important to remind patients not to eat or drink with the vacuum-formed retainers in place. This is a particular concern if the patient drinks cariogenic drinks with the vacuum-formed retainer in place (Fig. 4).
Removable retainers with a wire labial bow (Hawley and Begg type retainers)
These types of retainers are robust and, unlike VFRs, Begg and Hawley retainers can be worn when eating without becoming damaged. Hawley retainers (Fig. 5) have the advantage of facilitating posterior occlusal settling during retention.14 However this is of less importance if good posterior intercuspation has been established by the time of appliance removal. The labial bow can be modified to accomplish simple active tooth movements if required and an anterior bite plane can be incorporated to help retain corrected deep overbites.
Fixed bonded retainers (smooth wire, flexible spiral/multi-strand wire)
There are several designs of fixed retainer. A multi-strand wire bonded to all six anterior teeth or a sandblasted round stainless steel wire bonded only to the canines is the most commonly used (Fig. 6). Fixed retainers are discreet and reduce the demands on patient compliance. However, they are associated with a significant long-term failure rate. One study reported that a third of patients experienced retainer failure within 30 months15 with de-bonding from at least one tooth in 22% of patients, and 17% having total retainer loss. Fracture of the retainer wire was uncommon, with less than 1% of patients having this type of failure. Particular care is required when placing upper bonded retainers to minimise occlusal contacts with the opposing lower teeth as such contacts have been shown to increase failure rates. A composite with high filler content is preferred to improve resistance to wear.
Calculus and plaque deposition is greater than with removable retainers16 and concerns exist about the impact of fixed bonded retainers on long-term dental health. However, a review reported that studies completed up to 8.5 years after fixed retainers were placed have found no deleterious effect on the adjacent hard and soft tissues.17 Nevertheless, meticulous attention to detail is required when placing fixed retainers to avoid contact with the gingival tissues by the bonding material. Figure 6 shows an example of a bonded retainer demonstrating that the composite should be placed to cover the wire, but ensuring there is no interference in the inter-dental space to allow cleaning. Any excess composite should be removed with a tungsten carbide bur. It is important to show patients how to look after their bonded retainers and to maintain excellent oral hygiene around them. The use of small inter-dental brushes or superfloss may be a useful adjunct to tooth brushing to help maintain excellent oral hygiene around bonded retainers (Fig. 7).
Since some patients wearing fixed retainers will be required to wear them indefinitely, the GDP has an important role to play in ensuring that the dental tissues adjacent to the fixed retainers remain healthy. When patients attend for their regular dental check-ups with their GDP, their fixed retainers should be carefully inspected, particularly the integrity of the composite attachment to the enamel surface. Repair of most bonded retainer failures can readily be achieved by the GDP using conventional light cured composite and bonding agent. In order to obtain ideal bonding conditions for re-bonding fixed retainers, it is recommended that the bonding site is clean and dry but also free of old composite remnants.18 It is also important to remove any pellicle on the teeth before etching. This can be achieved using a tungsten carbide bur or intra-oral sandblaster. In cases where the wire has fractured, the retainer has completely de-bonded, or where relapse has occurred, advice should be sought from the patient's orthodontist as a decision will need to be made on whether to replace or remove the retainer.
Dual retention
Some orthodontists will prescribe 'dual retention', when a patient wears bonded retainers with the addition of removable retainers overnight. If the bonded retainer fails, the teeth can be held in position by the removable retainer until the bonded retainer can either be replaced or repaired.
Duration of orthodontic retention
In current orthodontic practice, considerable variation exists in the duration of the retention period used. This reflects a number of factors including the preference of the orthodontist, the variability of occlusal, skeletal and soft tissue relationships, as well as the paucity of well-controlled scientific studies.19 A survey carried out in the UK during the 1990s found that the most commonly used retention period was 12 months.20 This approach appears reasonable in the light of histological studies which have shown that the supra-crestal periodontal fibres remain stretched and displaced for more than seven months after the cessation of orthodontic tooth movement.21,22 However, even with retention periods exceeding this duration, changes in tooth position frequently occur in the long term.23,24 Nevertheless, it is known that variations in the duration and intensity of removable retainer wear are clinically acceptable. Although a Cochrane review carried out in 2006 concluded that there was insufficient research data on which to base clinical practice on retention,25 further randomised clinical trials have been published since then. Two studies examining the use of vacuum formed retainers26,27 and one study with Hawley retainers28 have found that part-time wear for a year is as effective in maintaining the treatment outcome as a combination of full time followed by part-time wear.
In view of the practical and ethical barriers to carrying out randomised studies of all of the possible retention regimens, it is unlikely that an accepted definitive recommended duration for retention will be established. Furthermore, the wide variation in the severity and complexity of patients' malocclusions and their orthodontic treatment also militate against establishing a 'one size fits all' approach to retention. Current good orthodontic practice is that a patient's individual retention regimen should be based on an assessment of the specific factors which are known to be more likely to relapse. In particular, the decision to recommend prolonged or indefinite retention (usually with fixed retainers) is based on consideration of the factors detailed below.
Lower incisor alignment
Increases in lower incisor irregularity are common following orthodontic treatment (Fig. 8). Similar changes occur in untreated subjects and are now accepted to be normal rather than exceptional occurrences. A number of studies have confirmed that lower incisor irregularity usually increases during the second, third and fourth decades of life in untreated subjects as well as those who have had previous orthodontic treatment followed by retention.23,24 The greatest changes in untreated occlusions occur before the age of 18 years and it is known that most change will have taken place by the middle of the third decade.29,30,31 This period corresponds to the age-range during which most orthodontic treatment is carried out and further complicates the planning of retention.
As the supra-crestal periodontal fibres take the longest amount of time to reorganise, prolonged retention of corrected tooth rotations can be helpful in reducing relapse. Crowded incisor teeth often have rotations before treatment, and retention of these teeth should be planned for towards the end of the active appliance phase of treatment.
Long-term or indefinite retention may reduce the risk of developing lower incisor irregularity following orthodontic treatment. Nevertheless, it is unclear what duration of retention is adequate to prevent lower incisor crowding. However, retention period in excess of eight years with fixed bonded retainers have been shown to result in better maintenance of lower incisor alignment than other studies which reported shorter retention times.17
An important factor to consider when planning retention is the patient's expectations of the stability of their lower incisor alignment. If a patient is unwilling to accept the risk of deterioration in lower incisor alignment following orthodontic treatment then long-term retention should be considered.
Changes in the antero-posterior position of the lower incisors during orthodontic treatment
Changes in the antero-posterior position of the lower incisors during orthodontic treatment are known to be unstable with a tendency for the lower incisors to return towards their pre-treatment position after retention is discontinued. This can result in deterioration of the alignment of lower incisors. Many orthodontists therefore work to the principle of avoiding proclination or advancement of the lower incisors during treatment if at all possible, although small changes of 1–2 mm may be stable.32 It has been recommended that long-term or indefinite retention should be used following any intentional or unintentional antero-posterior change in lower incisor position of more than this small amount. However, a significant clinical concern is the use of fixed retainers in situations where teeth have been moved to unstable positions due to poor treatment planning.
Patients with a history of periodontal disease or root resorption
Orthodontic patients with previously treated severe periodontal disease and those with root resorption or crestal bone loss have an increased risk of deterioration of tooth alignment following treatment.33 Permanent retention is advisable in these cases. For those with previous minimum to moderate severity periodontal disease, a more routine retention protocol can be used.34
Spaced dentitions
Permanent retention is recommended following orthodontic closure of generalised spacing or a midline diastema in an otherwise normal occlusion.35
Compromised orthodontic outcomes
As part of the informed consent process, patients may be offered orthodontic treatment aimed at achieving a compromised result. This approach, which may address the patient's key aesthetic complaints without achieving a perfect occlusion, has recently been referred to as 'short-term' orthodontics.36 Although this may reduce the length of treatment and the financial and treatment demands on the patient, final occlusal outcomes can be less than ideal, the relapse potential greater, and fixed retainers may therefore be indicated.
Adjunctive techniques
These are soft additional soft tissue or hard tissue procedures that can be undertaken to reduce the risk of relapse.
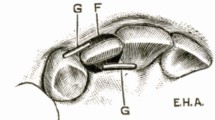
Pericision, sometimes called supra-crestal circumferential fibreotomy, is a soft tissue procedure that aims to cut the periodontal fibres around the neck of the teeth (dento-gingival and inter-dental fibres). These fibres have the tendency to pull the teeth back towards their original position, particularly teeth that were initially rotated.37 It is a simple procedure undertaken under local anaesthetic and requires no periodontal dressing after the procedure.
Interproximal reduction, sometimes known as re-proximation, is a hard tissue procedure that aims to remove small amounts of enamel mesio-distally. This can help to reduce the likelihood of relapse.38 It is not clear why it reduces the relapse, but it may be due to flattening of inter-dental contacts, increasing the stability between adjacent teeth.
Conclusions
-
Long-term age changes in skeletal and soft tissues surrounding the teeth mean that relapse after orthodontic treatment is unpredictable, but likely.
-
As it is difficult to predict which cases will relapse, every case should be treated on the basis that it has the potential to relapse and long-term or life-long retention may be required.
-
Patients should only proceed with orthodontic treatment if they are prepared to wear retainers.
-
Removable retainers allow the patient to remove them to maintain oral hygiene, but their success depends on long-term compliance.
-
In some situations bonded retainers are required as full-time retention is necessary. The patient must maintain excellent oral hygiene around the bonded retainers to reduce the chance of dental disease.
-
The GDP has important roles in orthodontic retention. These include informing patients that they will need to wear retainers after orthodontic treatment; motivating patients to continue wearing their retainers during the retention period; monitoring and if necessary replacing or repairing retainers; and liaising with the orthodontist as required.
-
There remains a need for further randomised clinical trials to evaluate the use of different types of retainers and retention protocols.
References
Richter D D, Nanda R S, Sinha P K, Smith D W, Currier G F . Effect of behavior modification on patient compliance in orthodontics. Angle Orthod 1998; 68: 123–132.
Lyotard N, Hans M, Nelson S, Valiathan M . Short-term postorthodontic changes in the absence of retention. Angle Orthod 2010; 80: 1045–1050.
Harris E F, Vaden J L . Posttreatment stability in adult and adolescent orthodontic patients: a cast analysis. Int J Adult Orthodon Orthognath Surg 1994; 9: 19–29.
Harris E F, Vaden J L, Dunn K L, Behrents R G . Effects of patient age on postorthodontic stability in Class II, division 1 malocclusions. Am J Orthod 1994; 105: 25–34.
Kaplan H . The logic of modern retention procedures. Am J Orthod Dentofacial Orthop 1988; 93: 325–340.
Meade M J, Millett D . Retention protocols and use of vacuum-formed retainers among specialist orthodontists. J Orthod 2013; 40: 318–325.
Pratt M C, Kluemper G T, Hartsfield J K Jr, Fardo D, Nash D A . Evaluation of retention protocols among members of the American Association of Orthodontists in the United States. Am J Orthod Dentofacial Orthop 2011; 140: 520–526.
Hichens L, Rowland H, Williams A et al. Cost-effectiveness and patient satisfaction: Hawley and vacuum-formed retainers. Eur J Orthod 2007; 29: 372–378.
Singh P, Grammati S, Kirschen R . Orthodontic retention patterns in the United Kingdom. J Orthod 2009; 36: 115–121.
Mollov N D, Lindauer S J, Best A M, Shroff B, Tufekci E . Patient attitudes toward retention and perceptions of treatment success. Angle Orthod 2010; 80: 468–473.
Kumar A G, Bansal A . Effectiveness and acceptability of Essix and Begg retainers: a prospective study. Aust Orthod J 2011; 27: 52–56.
Rowland H, Hichens L, Williams A et al. The effectiveness of Hawley and vacuum-formed retainers: a single-center randomized controlled trial. Am J Orthod Dentofacial Orthop 2007; 132: 730–737.
Chate R A, Falconer D T . Dental appliances with inadequate occlusal coverage: a case report. Br Dent J 2011; 210: 109–110.
Sauget E, Covell D A, Boero R P, Lieber W S . Comparison of occlusal contacts with use of Hawley and clear overlay retainers. Angle Orthod 1997; 67: 223–230.
Scheibe K, Ruf S . Lower bonded retainers: survival and failure rates particularly considering operator experience. J Orofac Orthop 2010; 71: 300–307.
Heier E E, De Smit, A A, Wijgaerts I A, Adriaens P A . Periodontal implications of bonded versus removable retainers. Am J Orthod Dentofacial Orthop 1997; 112: 607–616.
Sadowsky C, Schneider B J, BeGole E A, Tahir E . Long-term stability after orthodontic treatment: nonextraction with prolonged retention. Am J Orthod Dentofacial Orthop 1994; 106: 243–249.
van Westing K, Algera T J, Kleverlaan C J . Rebond strength of bonded lingual wire retainers. Eur J Orthod 2012; 34: 345–349.
Littlewood S J, Millett D T, Doubleday B, Bearn D R, Worthington H V . Orthodontic retention: a systematic review. J Orthod 2006; 33: 205–212.
Clark J D, Kerr W J, Davis M H . CASESclinical audit; scenarios for evaluation and study. Br Dent J 1997; 183: 108–111.
Reitan K . Clinical and histologic observations on tooth movement during and after orthodontic treatment. Am J Orthod 1967; 53: 721–745.
Edwards J G . A study of the periodontium during orthodontic rotation of teeth. Am J Orthod 1968; 54: 441–461.
Little R M, Riedel R A, Artun J . An evaluation of changes in mandibular anterior alignment from 10 to 20 years postretention. Am J Orthod Dentofacial Orthop 1988; 93: 423–428.
Little R M . Stability and relapse of dental arch alignment. Br J Orthod 1990; 17: 235–241.
Littlewood S J, Millett D T, Doubleday B, Bearn D R, Worthington H V . Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst Rev 2006; 1: CD002283.
Gill D S, Naini F B, Jones A, Tredwin C J . Part-time versus full-time retainer wear following fixed appliance therapy: a randomized prospective controlled trial. World J Orthod 2007; 8: 300–306.
Thickett E, Power S . A randomized clinical trial of thermoplastic retainer wear. Eur J Ortho 2010; 32: 1–5.
Shawesh M, Bhatti B, Usmani T, Mandall N . Hawley retainers fullor part-time? A randomized clinical trial. Eur J Orthod 2010; 32: 165–170.
Richardson M E . Late lower arch crowding facial growth or forward drift? Eur J Orthod 1979; 1: 219–225.
Richardson M E . Lower incisor crowding in the young adult. Am J Orthod Dentofacial Orthop 1992; 101: 132–137.
Richardson M E, Gormley J S . Lower arch crowding in the third decade. Eur J Orthod 1998; 20: 597–607.
Mills J R E . The stability of the lower labial segment. A cephalometric survey. Dent Pract Dent Rec 1968; 18: 293–306.
Sharpe W, Reed B, Subtelny J D, Polson A . Orthodontic relapse, apical root resorption, and crestal alveolar bone levels. Am J Orthod Dentofacial Orthop 1987; 91: 252–258.
Zachrisson BU . Tooth movements in the periodontally compromised patient. In Lindhe J, Lang N P, Karring T (ed) Clinical periodontology and implant dentistry. 5th ed. pp 1241–1279. Oxford: Blackwell Munksgaard, 2008.
Joondelph D R . Stability, retention and relapse. In Graber L W, Vanarsdall R L, Vig KWL (ed) Orthodontics: current principles and techniques. 5th ed. pp 991–1020. Philadelphia: Elsevier Mosby, 2012.
Chate R A . Truth or consequences: the potential implications of short-term cosmetic orthodontics for general dental practitioners. Br Dent J 2013; 215: 551–553.
Edwards J G . A long-term prospective evaluation of the circumferential supracrestal fiberotomy in alleviating orthodontic relapse. Am J Orthod Dentofacial Orthop 1988; 93: 380–387.
Edman Tynelius G, Bondemark L, Lilja-Karlander E . Evaluation of orthodontic treatment after 1 year of retentiona randomized controlled trial. Eur J Orthod 2010; 32: 542–547.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Johnston, C., Littlewood, S. Retention in orthodontics. Br Dent J 218, 119–122 (2015). https://doi.org/10.1038/sj.bdj.2015.47
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2015.47
This article is cited by
-
Knowledge, attitude and practice of patients towards orthodontic treatment
BMC Oral Health (2023)
-
Impact of occlusal contact pattern on dental stability and oromandibular system after orthodontic tooth movement in rats
Scientific Reports (2023)
-
Restorative dentistry clinical decision-making for hypodontia: peg and missing lateral incisor teeth
British Dental Journal (2023)
-
A survey of patient compliance with removable orthodontic retainer wear in Brunei Darussalam
BDJ Open (2023)
-
Changes in the distribution of occlusal forces in the course of the orthodontic retention phase
Journal of Orofacial Orthopedics / Fortschritte der Kieferorthopädie (2023)