Key Points
-
Discusses classification and presentation of the deep overbite.
-
Discusses restorative challenges associated with the deep overbite.
-
Outlines treatment options for patients presenting with deep overbites.
-
Provides a framework for restorative treatment planning related to clinical findings and details the treatment protocol at each stage.
Abstract
A deep overbite is where the vertical overlap of the upper and lower incisors exceeds half of the lower incisal tooth height. Problems associated with the deep overbite can include soft tissue trauma, lack of inter-occlusal space and tooth wear, all of which can present significant challenges for the restorative dentist. While management options very much depend on the nature of the situation and patient's symptoms, options may range from provision of a simple removable appliance or splint and non-surgical periodontal therapy, to multidisciplinary care involving orthodontics, orthognathic surgery and restorative dentistry. Restorative management may involve an increase in the occlusal vertical dimension with fixed restorations or removable prostheses, and careful assessment and treatment planning is essential. This article discusses the aetiology and restorative management strategies for deep and traumatic overbites.
Similar content being viewed by others
Introduction
The majority of deep overbites are asymptomatic and where the appearance is aesthetically acceptable patients are unlikely to seek treatment.1 However, this type of incisal relationship can be problematic to both the patient and the restorative dentist if it results in soft tissue trauma, tooth wear or if missing teeth require replacement. This article aims to provide an overview of the problems associated with this malocclusion and suggests options for restorative management.
Overbite classification
The term overbite refers to the degree of vertical overlap of the upper and lower incisor teeth.2 Where the overlap is greater than half of the lower incisor tooth height, the overbite is considered to be increased or deep. This is a common finding in individuals with Class II incisor relationships and a Class II skeletal pattern.2
A traumatic overbite is where there is damage to the underlying periodontium or the hard tissues of the teeth involved. The prevalence of the traumatic overbite has been reported to be 4.3%.3 The Akerly classification4 of traumatic overbite is shown in Table 1 along with associated common clinical findings. It is not unusual to see patients who present with a combination of aetiological factors and signs and symptoms.
The traumatic overbite
The progression from an asymptomatic deep overbite to symptomatic traumatic overbite in an adult patient may be due to a number of factors.1
Poor plaque control associated with the palatal aspects of the upper incisor teeth can cause inflammation of the palatal gingivae and swelling. Where there is a deep overbite, this may predispose to direct soft tissue trauma from the opposing incisal edges. The resulting discomfort can hinder oral hygiene efforts, increasing the risk of periodontal disease. Food impaction may also occur, which has been described as an aetiological factor in the development of lateral periodontal cysts.5
In situations where the incisal edges occlude onto the gingival margins of the opposing teeth, traumatic stripping of the gingivae and gingival recession may result. Lower incisors are particularly at risk of this where there is a thin gingival biotype and a thin buccal plate of underlying alveolar bone. Recession may also affect the palatal aspects of the upper incisors; the extent of this depends on the level of inflammation present and the degree of trauma.
Loss of posterior occluding units may lead to anterior posturing of the mandible and overclosure. This can result in soft tissue problems as described above, or tooth wear depending on the skeletal and incisal relationship.6 It has also been suggested that following the loss of posterior support, the presence of a strong lower lip may cause lingual tilting of the lower labial incisors, exacerbating the problem further.7
In all patients, parafunctions such as habitual posturing and sleep bruxism can result in painful muscles of mastication, tooth wear and, where periodontal support has been compromised, tooth mobility and migration. Parafunctional habits are also likely to worsen the symptoms of soft tissue trauma associated with a traumatic overbite. Where there is a loss of posterior support and a history of periodontal disease, this situation may be further exacerbated by migration of the upper anterior teeth.
Delivery of restorative treatment
The presence of an increased or deep overbite is often a source of difficulty for the restorative clinician and the following aspects may need to be considered and addressed.
Soft tissue trauma
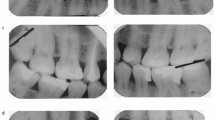
Contact between lower incisors and palatal mucosa rather than tooth-to-tooth contact between the incisor teeth may result in pain and swelling of the mucosa and functional difficulties (Fig. 1).
Lack of inter-occlusal space
Where there are missing teeth, a lack of inter-incisal space means that it is impossible to insert a removable partial denture (RPD) connector of adequate thickness without increasing the occlusal vertical dimension (OVD) (Fig. 2). Unless the posterior teeth are overlayed, this results in the only interocclusal contact occurring between the lower incisors and the connector. This can result in discomfort and difficulty in eating, or repeated fracture of the denture.
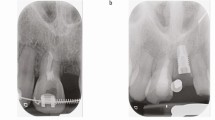
There was palatal soft tissue trauma and tooth surface loss associated with parafunction. The patient complained of sensitivity of the teeth and an inability to tolerate an upper partial denture f-e Crowns were placed on the 11, 16, 21, 24, 25 with rest seats and milled guide planes. Veneers were placed on the 41, 42, 43, 31, 32 and composite bonding to the 12, 13. A CoCr upper partial onlay denture was fabricated at an increased OVD, to provide positive occlusal contacts around the arch. Aesthetics, function and occlusal stability were restored and a lower soft night guard was provided
Similarly, the provision of fixed bridgework to replace missing teeth can be challenging as there may be insufficient space to provide aesthetic pontics that do not interfere with guidance patterns (Fig. 3).8
There was an increased overbite with little inter-arch space for a connector in the 22, 23 region and subsequent difficulty in tolerating a removable partial denture e-h Composite build ups on the 15, 11, 25, 34, 32, 31, 41, 42, 43, and 44 were used to increase the OVD. This created room for the URC to be built up to improve aesthetics and resin bonded bridges to be placed from the 21 and 24 to replace the missing 22 and 23. A lower soft night guard was provided following treatment
Individuals with a deep overbite are often associated with a steep glenoid fossa thus constraining the lateral excursions and only predominately allowing elevation and depression of the mandible.9 Clinically this is seen in patients with Class II div 2 incisal relationships, where the inclination of the teeth provides a very definite, or 'locked in' intercuspal position (ICP). This lack of excursive tendency could be seen as advantageous, as there is less risk of fracture of restorations through eccentric mandibular movements.
Tooth wear
If teeth are worn and extra coronal restorations are indicated, the provision of these within the existing occlusal scheme can be difficult. As these teeth have already lost height, further reduction to allow adequate space for restoration is likely to have implications for pulpal health and produces preparations that lack retention and resistance form.
Management options
The management options for problems associated with a deep overbite very much depend on the presenting situation and the patient's complaints. They may range from the provision of a simple removable appliance to multidisciplinary care involving orthodontics, orthognathic surgery and restorative dentistry. Irrespective of the complexity of treatment planned, it should aim to optimise the periodontal health and improve occlusal stability, function and aesthetics. Management can be split into two broad phases: stabilisation and restorative treatment.
Stabilisation
Periodontal therapy
A fundamental initial step in management of all cases is oral health education and periodontal treatment, aiming to achieve and maintain an excellent standard of oral hygiene and periodontal health. As described previously, gingival inflammation and loss of periodontal support may exacerbate symptoms and worsen compromised tooth positions.
Splint therapy
As an initial step to palliate symptoms, a soft splint can be provided to protect the mucosa or teeth from further damage. This is normally prescribed for night time wear to protect against nocturnal parafunction, however, some patients may benefit from wear at other specific times during the day.
Soft splints are usually made from 2 mm polyvinyl material,10 although newer bilaminar materials are available (Kombiplast, Dreve Dentamid GmbH) with a soft inner layer and harder outer layer. These splints are usually provided for the lower arch where they are more readily tolerated than in the upper arch. Any splint provided should have full arch occlusal coverage to reduce the risk of overeruption of the uncovered teeth. The splint should be well adapted to the teeth to provide good retention and have minimal gingival coverage (Fig. 1b).
When providing a soft splint, it is worth remembering that a proportion of patients find these difficult to tolerate and an existing bruxist habit may be exacerbated.10 In these patients, a hard stabilisation splint could be provided. Hard splints as either a definitive treatment or as a preliminary phase before definitive restorations or prosthesis have been advocated.5,11
In cases where the main presenting features are soft tissue trauma or early tooth wear that does not require restoration, the provision of a splint may be all that is required to alleviate the patient's symptoms and maintain occlusal stability.
Orthodontic treatment
When the periodontal condition is healthy and stable, the decision should be made as to whether to accept the patient's incisal relationship. Orthodontics represents a significant amount of treatment and a level of commitment that is not acceptable to many adult patients.
Orthodontic treatment to reduce the overbite is often technically difficult and lengthy, with results that are difficult to maintain even with long-term orthodontic retention.12 Additionally, the fact that many of these patients present later in life having lost teeth and periodontal support makes orthodontics even more of a challenge. In these cases the use of mini-screw or temporary anchorage devices (TADs) to reinforce anchorage can facilitate treatment.13,14
Where there is a significant underlying skeletal discrepancy, orthodontics alone is unlikely to produce a stable inter-incisal relationship. In these cases multidisciplinary management may be required including:
-
Restorative dentistry: Restorative intervention during these cases is usually limited to the provision of a removable prosthesis, although the use of resin-bonded palatal stops following orthodontic intrusion of the lower incisor teeth has been described. These metal stops extended onto the palatal mucosa from the upper anterior teeth, protecting the mucosa from trauma and preventing relapse of the incisal position.15 Maintaining oral hygiene around this type of restoration presents the patient with a significant challenge and periodontal health should be monitored closely, especially considering that in these cases there may be a history of periodontal compromise. As a result the authors do not advocate this approach.
-
Orthognathic surgery: Orthognathic surgery may also be considered in cases where it is not possible to resolve the patient's traumatic occlusion and achieve a stable result with orthodontics alone.1 This treatment pathway represents a significant commitment for the patient and a detailed multidisciplinary case assessment is required before embarking on treatment, discussion of which is beyond the scope of this paper.
Restorative treatment
If there are teeth requiring replacement, significant tooth wear, or if a splint fails to resolve soft tissue trauma, further restorative intervention may be indicated. This is likely to involve increasing the patient's OVD.
It is important to ensure that any changes to the occlusion are made in a controlled way, otherwise existing problems may be exacerbated. For example, where there is palatal tooth wear or soft tissue trauma, the clinician may be tempted to restore the posterior teeth at an increased OVD, creating inter-incisal space and alleviating symptoms. However, if the lower incisors are left out of occlusion, they are likely to overerupt, resulting in recurrence of the original problem. Similarly, if the incisal edges of the lower teeth are simply adjusted to create space, it is likely that they will erupt to re-establish the previous position if they remain unopposed.
To plan treatment, study models should be articulated on a semi-adjustable articulator using a facebow registration and an interocclusal record, taken in the retruded arc of closure. Articulation of models facilitates the assessment of occlusal relationships and can help in determining the increase in OVD needed to permit the desired treatment. Changes in OVD are generally well tolerated by dentate patients and there is little evidence to define the limits of this technique.16 It is the authors' experience that most treatment can be delivered with increases of between 1-3 mm.
Fixed restorations
Restoration of worn teeth by reorganising the occlusion at an increased OVD is well-documented.17 Where fixed restorations are to be provided, a diagnostic wax-up at this increased OVD can help to plan treatment. It also acts as a useful communication tool and an aid to gaining informed consent.
The occlusal contour of any restorations must be carefully considered and features such as stable occlusal stops and appropriate guidance can be developed in the wax up. The management of guidance patterns can help to protect weaker teeth. Enhancing the palatal contour of upper canines has been suggested in order to facilitate the disclusion of posterior teeth that are heavily restored. Similarly, posterior restorations set up in group function will minimise excursive forces on a compromised canine.8 Once the occlusal scheme has been planned on the articulator it can be reproduced in the definitive restorations.
The decision as to whether to use extra-coronal restorations or composite build ups (Fig. 4) to achieve the desired change in occlusion is dependent largely on the restorative status of the tooth. However, other factors such as the strategic role of the tooth and parafunctional tendency should also be considered. For example, teeth that are abutments for RPDs may benefit from the provision of milled crowns (Fig. 2). Crowns may also be considered for canines, in situations where the maintenance of canine guidance is key and composite resin would undergo more rapid wear compromising this.
Tooth surface loss due to erosion and attrition affected the upper and lower anterior teeth e-g Following stabilisation of the patient's periodontal condition, the incisal edges of the upper anteriors were recontoured and composite bonding was carried out at an increased OVD to restore the worn upper and lower anterior teeth. The appearance of the exposed crown margin and root surface 21 was not visible in the patient's smile. (h) An upper soft night guard was provided following treatment
If, by altering the contour of the palatal surfaces of the upper anterior teeth a definitive cingulum stop (Fig. 5) and stable incisal relationship is achieved, it may be possible to leave the posterior teeth as they are and allow them to overerupt into contact, in accordance with the Dahl principle.18 The use of this technique is not appropriate where the buccal segments are heavily restored, posterior units are unopposed or teeth are not in an adequate functional relationship due an arch size discrepancy. In these situations, restoration of the posterior teeth via direct or indirect onlays or crowns at the new OVD is recommended.
Removable options: the onlay denture
The provision of overdentures and onlay dentures has long been described in the management of patients with congenital and acquired defects of tooth shape, form and number,19,20 as well as those with considerable inter-arch size discrepancies.20
Removable onlay dentures can be used effectively in the management of deep overbites and are particularly indicated in cases where tooth position is such that developing stable tooth-tooth contacts is impossible (Figs 2 and 6).
There was a Class II div 2 malocclusion and a traumatic overbite. The lower anterior teeth had been lost due to periodontal disease, exacerbated by the traumatic overbite and the remaining lower teeth were lingually inclined. The patient had been unable to tolerate a conventional lower partial denture d-f A CoCr tooth-supported onlay denture was provided at an increased OVD, providing occlusal contacts around the arch. (g) Composite was placed over the metal framework in the premolar regions for aesthetic reasons
An additional advantage is that the provision of an onlay denture does not alter the position and height of the teeth: the patient would be able to occlude adequately both with and without the prosthesis in situ. Should the patient fail to tolerate the prosthesis, lose or break it, they will be able to function without it.
The onlay denture should be designed to cover the occlusal surfaces of the remaining teeth. Interim prostheses can be made in acrylic. However, this is likely to be subject to wear, so in the long term a cobalt chromium framework is ideal. The aesthetic implications of this in the upper arch are likely to be minimal. In the lower arch, the occlusal surface of the metalwork can be masked with prosthetic teeth or covered with laboratory formed composite resin where space allows (Fig. 6).
As an onlay denture increases the OVD, it will alleviate soft tissue trauma and create space to allow the restoration of missing teeth. Additionally with careful planning, the framework can be contoured to improve the occlusal table. This is particularly advantageous where there is an arch width discrepancy with poor tooth-to-tooth contacts. The occlusal surface of an upper denture can be extended palatally to improve the contact with the lower teeth (Fig. 2): or in the lower arch, an overlay section could be extended buccally to increase the width of the occlusal table. Upper dentures should be designed with a flat anterior bite place to provide even contact with the lower incisors.6 The denture framework should extend to gain tooth support from the cingulums of the upper anterior teeth and provide an even occlusion with the lower incisor teeth.
Sequencing restorative treatment
Where a removable prosthesis to increase the OVD is planned, the existing teeth and restorations must be fully assessed at the outset to identify any that require replacement, as subsequent 'retro-fitting' of restorations beneath an onlay denture is challenging. If there are multiple teeth to restore then an interim acrylic prosthesis can be provided. This will reduce symptoms related to the traumatic overbite, allow replacement of any missing teeth and allow the patient to trial the new occlusal relationship while this initial phase of treatment is completed.
If the occlusion is to be altered using fixed restorations, this should be attempted in carefully planned stages. Ideally, the anterior teeth should be restored at the new OVD first, to ensure optimal aesthetics and guidance. Following preparation for crowns, temporary restorations can be fabricated using a silicone matrix of the wax-up. Where teeth are to be built up with composite, this can be facilitated by the use of a silicone matrix of the diagnostic wax-up.21,22 In this way, the new restorations exhibit the ideal contours planned on the articulator. If it is not possible to do the same for the posterior teeth at this appointment, the occlusion can be supported by composite 'blobs' on key occluding units, or an interim acrylic overlay denture can be provided.
Once all teeth involved in the plan have been temporised within the new occlusal scheme, definitive restorations can be produced. Where applicable these should be designed to aid the support and retention of any planned CoCr removable prosthesis, with rest seats, guide planes and appropriate undercuts.
Following treatment, it is advisable that the patient continues with the use of a night guard or hard splint. This will promote occlusal stability and reduce the effects of any parafunctional habits. Periodontal health should also be closely monitored using standard methods such as probing depths, bleeding scores and plaque scores. Periodontal maintenance therapy can then be offered as indicated.23
Figure 7 summarises the treatment protocol at each stage based on the possible clinical findings to aid decision making and the planning of treatment.
Conclusion
The problems associated with a deep overbite can undoubtedly present clinical challenges. The initial aims of treatment are to reduce soft tissue trauma and improve periodontal health. Further restorative intervention may be required if there is continued trauma, tooth wear or teeth have been lost. Treatment should aim to improve occlusal stability, function and aesthetics. Some management options may involve lengthy treatment plans, requiring a significant commitment from the patient. Patient tolerance of treatment should be considered when planning treatment, along with the expected longevity and the maintenance burden of various options. Successful rehabilitation of these cases can be achieved with careful planning and management of the occlusion.
References
McDonagh S, Chadwick J C . The combined orthodontic and surgical treatment of traumatic Class II division 2 in the adult. Dent Update 2004; 3: 83–88, 90–91.
Mitchell L . An introduction to orthodontics. 4th ed. Oxford: Oxford University Press, 2013.
Holmes A . The prevalence of orthodontic treatment need. Br J Orthod 1992; 19: 177–182.
Akerly W B . Prosthodontic treatment of traumatic overlap of the anterior teeth. J Prosthet Dent 1977; 38: 26–34.
Nasry H A, Barclay S C . Periodontal lesions associated with deep traumatic overbite. Br Dent J 2006; 200: 557–561.
Cotter S, O'Shea D . Traumatic overbite: a restorative solution. Dent Update 2002; 29: 136–140.
Wragg P F, Jenkins W M, Watson I B, Stirrups D R . The deep overbite: prevention of trauma. Br Dent J 1990; 168: 365–367.
Torbjorner A, Fransson B . Biomechanical aspects of prosthetic treatment of structurally compromised teeth. Int J Prosthodont 2004; 17: 135–141.
Aiello L, Dean C . An introduction to human evolutionary anatomy. London: Academic Press, 1990.
Grey R J, Davies S J . Occlusal splints and temporomandibular disorders: why, when, how? Dent Update 2001; 28: 194–199.
Blair F M, Thomason J M, Smith D G . The traumatic anterior overbite. Dent Update 1997; 24: 144–152.
Millett D T, Cunningham S J, O'Brien K D, Benson PE, de Oliveira C M . Treatment and stability of class II division 2 malocclusion in children and adolescents: a systematic review. Am J Orthod Dentofacial Orthop 2012; 142: 159–169.
Scott P, Fleming P, DiBiase A . An update in adult orthodontics. Dent Update, 2007; 34: 427–436.
Pace A, Sandler J . TADs: an evolutionary road to success. Dental Update, 2014; 41: 242–249.
Barclay S C . Case report: an alternative treatment of deep traumatic overbite. Eur J Prosthodont Restor Dent 1996; 4: 3–6.
Al-Khayatt A S, Ray-Chaudhuri A, Poyser N J et al. Direct composite restorations for the worn mandibular anterior dentition: a 7-year follow-up of a prospective randomised controlled split-mouth clinical trial. J Oral Rehabil 2013; 40: 389–401.
Poyser N J, Porter R W, Briggs P F, Chana H S, Kelleher M G . The Dahl concept: past, present and future. Br Dent J 2005; 198: 669–676.
Dahl B L, Krogstad O, Karlsen K . An alternative treatment in cases with advanced localized attrition. J Oral Rehabil 1975; 2: 209–214.
Ghodsi S, Rasaeipour S, Vojdani M . Oral rehabilitation of a patient with amelogenesis imperfecta using removable overlay denture: a clinical report. J Contemp Dent Pract 2012; 13: 227–231.
Brewer A A, Morrow R M . Overdentures. 2nd ed. St. Louis: The C V, Mosby Company, 1980.
Mizrahi B . A technique for simple and aesthetic treatment of anterior toothwear. Dent Update 2004; 31: 109–114.
Robinson S, Nixon P J, Gahan M J, Chan M F . Techniques for restoring worn anterior teeth with direct composite resin. Dent Update 2008; 35: 551–552, 555–558.
Basic periodontal examination. Selby: British Society of Periodontology, 2011. Online guidelines available at http://www.bsperio.org.uk/publications/downloads/39_143748_bpe2011.pdf (accessed July 2014).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Beddis, H., Durey, K., Alhilou, A. et al. The restorative management of the deep overbite. Br Dent J 217, 509–515 (2014). https://doi.org/10.1038/sj.bdj.2014.953
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.953
This article is cited by
-
Restricted envelope of function
Tandartspraktijk (2016)