Key Points
-
Analyses bisphosphonate-related osteonecrosis of the jaw (BRONJ) in order to help healthcare professionals to provide the best patient care and to avoid exposure to liability claims.
-
Provides a detailed list of the duties of care and corresponding obligations of all the individuals involved from drug prescription through to the occurrence of BRONJ.
Abstract
Bisphosphonate-related osteonecrosis of the jaw (BRONJ) is an adverse reaction that may occur in patients administered with bisphosphonates (BP). This condition can cause high morbidity and hinder quality of life. Its treatment is complex and often unsatisfactory, and prevention strategies may have limited effectiveness, if any. Thus, managing patients treated with BP may result in exposure of the practitioner to legal liability or malpractice claims: legal actions pursuant to BRONJ are reported to be underway on three continents. Nonetheless, the attribution of liability, if any, is a complex process requiring, on the basis of current knowledge, a robust and pragmatic approach to the facts, which must be identified from the point of view of the time, place and individuals involved. This means a comprehensive consideration of the sequence of actions from bisphosphonates prescription to BRONJ occurrence (as well as immediately after, and any action potentially related to its causation or worsening) is required in order to determine if a breach in informing, diagnosing, managing or referring the patient took place, as well as determining if the patient was compliant in attending to prescriptions and follow-up programmes.
Similar content being viewed by others
Introduction
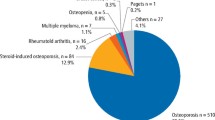
Bisphosphonates (BP) are frequently used in the treatment of skeletal diseases; they are particularly effective in reducing malignancy-related skeletal events,1,2 as well as in preventing complications caused by osteoporosis3 and other bone diseases characterised by unbalanced bone turnover.
Recently, it has been reported that patients administered with BP, particularly cancer patients receiving intravenous amino-bisphosphonates and undergoing invasive oral procedures,4 may be affected by an adverse reaction causing very high morbidity and impairment to their quality of life,5 namely the bisphosphonate-related osteonecrosis of the jaw (BRONJ). This disorder has been the subject of significant attention in the literature due to the growing evidence of BRONJ occurrence,6,7 the high associated morbidity, the difficulties in patients clinical management,6,7,8,9 and the wide and effective use of BP10 as both therapeutic and preventive agents (malignancy, hypercalcaemia, bone metastases, osteoporosis).11,12,13 In addition, increasing attention is being drawn to BRONJ in patients taking oral BP for the prevention/treatment of osteopenia/osteoporosis.13,14,15,16,17
The pathogenesis of BRONJ is still poorly understood.18,19 Thus, in patients treated with BP, clinical management aimed at reducing the risk of BRONJ and maintaining/improving oral health and comfort, may be problematic. In addition, whenever BRONJ does occur, treatment of related oral lesions and symptoms is complex and often unsatisfactory.20 As a consequence, managing patients treated with BP, whether affected by BRONJ or not, may expose the practitioner to legal liability or malpractice claims; in fact, legal actions pursuant to BRONJ are reported to be underway in three continents.21
Types of possible negligence claims have already been highlighted.22,23,24 However, the attribution of legal liability in clinical practice, if any, is a complex process requiring, on the basis of current knowledge, a careful and a comprehensive consideration of a number of aspects which will be addressed in this paper.
BRONJ factual analysis
Legal issues are fact-dependent and can be determined on a case basis by means of a robust and pragmatic approach to the facts. Facts, as well as the related events in the case, must be identified from the point of view of the time, place and individuals involved.
In the particular case of BRONJ, facts are, in general, as follows: a physician prescribes the BP to treat/prevent complications of malignant diseases or bone disorders; BP administration is known to potentially cause BRONJ; there is no way to define the risk to develop BRONJ in the single patient, nonetheless, some risk factors are known (Table 1); the patient takes the drug; treatment is long lasting or chronic; the oral health of the patient may change over time; and BRONJ may occur both as spontaneous manifestation or (often) triggered by invasive dental/periodontal procedures performed by a dental professional.
Attributing legal liability in BRONJ
The basis for a patient to obtain compensation in a civil court is: a duty of care has been breached by a healthcare practitioner, thus, causing harm or injury to the patient. Thus, the proven existence of two elements is mandatory:
Liability: the healthcare practitioner(s) must have been found to have acted in a manner in which no other similar professional(s) would have done, or notwithstanding current and accepted scientific evidence. This is also known as 'clinical negligence' (or formerly medical negligence) and will be addressed in this paper in the particular case of BRONJ. Other forms of potential liability and their applicability to BRONJ, if any, (for example, product liability and contractual liability), will be not discussed.
Causation: the harm or injury suffered by the patient was a consequence of the clinical negligence; in other words, the harm or injury would not otherwise have occurred. For civil cases, on the balance of probability, the clinical negligence was more than 50% likely to have caused the harm: this is applicable to Italy and England, but other countries and jurisdictions may have their own specific laws and criteria to assess and establish causation.
In this paper, we will focus on liability because: i) it is strictly related to scientific evidence, and, as such has a general applicability; and ii) it is the premise for the causation assessment. On the other hand, we do not deal specifically with the causation assessment, since it is so related to regional jurisdictions and their specific laws, and, in addition, can be only performed on a strict case-by-case basis.
Attributing legal liability, in general, deals with the evaluation of clinicians' conduct and their fulfilment of the standard of care. Traditionally, the legal standard of care in English law has been determined according to the Bolam test.25 However, this has received criticism26 and is not applicable in civil law jurisdictions; thus, we will refer to current scientific evidence regarding BRONJ, bearing in mind that the legal standard of care is generally determined by a court through reference to what the medical profession views as the accepted practice for a given situation.
Where the sequence of actions leading to cause or favour the onset, or worsening, of an unwanted condition ultimately causing damage to the patient, concerns more than one healthcare provider, the process of separating and attributing potential or actual liability, as well as causation, is more complicated.
Thus, in the particular case of BRONJ, which is a known adverse reaction to BP administration, the attribution of liability, if any, requires a comprehensive consideration of the sequence of actions before BRONJ occurrence (Table 2),23 as well as immediately after, and which are potentially related to its causation or deterioration. In particular, it must be determined if a duty of care exists, and if so, when it was breached and who was(were) the person(s) responsible for such a breach.
Now, assuming that we have a patient who received the diagnosis of a disorder whose treatment of choice is BP, from that point in time the sequence of actions detailed in Table 2 begins. Each of these actions is performed by various individuals. These individuals have specific duties of care and corresponding obligations relevant to BRONJ, the breaching of which may be linked to causation and/or worsening of BRONJ and may well set the stage for liability claims.
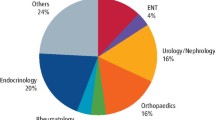
Considering the individuals listed in Table 2, it appears that BRONJ is not only a matter of clinical and potential legal concern for dental professionals. Though, dental professionals, from a chronological point of view, are, in general, the most closely related to BRONJ occurrence (in most cases BRONJ seems to be triggered by invasive dental procedures4), this does not imply that all legal obligations and causation should be implicitly attributed to dental professionals. Since BRONJ is a known adverse reaction of BP, prescription of such drugs is the first action of a chain potentially leading to the occurrence of BRONJ. Thus, the physicians who prescribe BP24 have a number of duties both in ascertaining risk factors at the beginning of treatment and in re-evaluating patients during and after treatment.
Legal obligations relevant to BRONJ pertain to the following aspects that may become the source of liability: i) knowledge of BRONJ and related issues; ii) information to the patient; iii) BRONJ prevention; and iv) BRONJ diagnosis. The inclusion of treatment in this list may be questionable because of considerations that will be discussed in a later section of this paper. Healthcare practitioners (both physicians and dental professionals) need to have a thorough understanding of these issues in order to practice successfully in the current litigious climate.
Sources of liability in BRONJ
Knowledge of BRONJ and related issues
BRONJ is a relatively recently recognised adverse reaction to BP administration.27 A recent survey by López-Jornet et al.,28 in the autonomous community of Murcia, Spain, showed that 50% of students participating in the survey and 68.36% of dentists with well-established professional activity had up-to-date knowledge of BRONJ, and most correctly identified its risk factors. However, only 13.33% of students and 33.33% of dentists knew how to treat osteonecrosis once established. Obviously, these data are strictly regional and no inference can be carried out as regards their applicability in other countries; nonetheless, they are quite worrisome because they suggest that there may be dentists who are still not informed, or at least not adequately informed, about BRONJ and how to manage it. Lack of knowledge and/or up-to-date information has evident implications from a medico-legal point of view. In particular, it is a specific and generally applicable duty of prudent practitioners to remain current by reading the latest peer-reviewed scientific publications and attending continuing education courses. In addition, relying on outmoded diagnostic and therapeutic modalities is suggestive of negligence.
It is also worth noting that liability may arise not only for a lack of or incomplete knowledge but also for incorrect knowledge. Under this point of view, a survey conducted in our institution (unpublished data) on 75 dentists participating in postgraduate training programmes showed that 24% of respondents were unable to distinguish between amino-bisphosphonates and non-aminobisphosphonates. This is extremely relevant since from the first reports29 it clearly emerged that BRONJ was associated with aminobisphosphonates administration; failing in understanding this key point could expose healthcare providers to legal liability for a lack of due diagnostic and/or preventive procedures (for example, antibiotic administration) as well as incorrect patient information.
Information to the patient
Information provided to the patient is another pivotal medico-legal issue in cases where BP are administered. A recent study by Migliorati et al.30 investigated whether patients taking BP knew about the medical indication for the therapy, its duration and possible adverse reactions (including BRONJ). The results showed that 84% of participants could recall being informed why they were receiving BP, 80% did not know or were uncertain about the duration of the treatment (an important risk factor for BRONJ), and, surprisingly, 82% said that they had not been told about the possible side effects of taking BP.
However, it is difficult to determine, from this survey, whether or not this lack of information was attributable to healthcare providers or to patients' inability to recall information received. Nonetheless, it is necessary to stress that, in general, failing in accomplishing the mandatory tasks of informing the patient and obtaining his/her informed consent sets the stage for legal liability.31,32 These obligations are generally applicable and, in the particular case of BRONJ, absolutely require the provision of specific, complete and understandable information as regards the benefits of treatment with BP,13,33 possible side effects (ie BRONJ),13,34 treatment alternatives and risks of no treatment. Since BRONJ is a known adverse reaction to BP, providing such information is a must for the prescribing physician. Dental professionals are also obliged to provide information regarding the risk that the observed oral condition and/or the required dental procedure may trigger BRONJ. An effective communication between all healthcare providers (prescribing physicians, dentists) and the patient is required for the information process to be effective and understandable, and for the consent to be valid. In addition, the information provided should be duly recorded on the 'informed consent form' signed by the patient (although written informed consent is not mandatory in some countries; for example Italy, for the particular case of BRONJ), which is a proof that the information was provided. If the information is lacking, inadequate, incomplete or its provision is non-demonstrable, the patient is fully entitled to damages. In such a case, the healthcare provider may be held liable on both ethical and legal grounds and the damages related to: i) not respecting the patient's right to self-determination: that is, no rational decision can be made by the patient without knowing and understanding the risks of proposed treatments; and ii) unwanted outcomes experienced by the patient to whom information was not given.
Prevention
Pathogenetic mechanisms of BRONJ are still not clearly understood,35,36 thus the only preventive approach is the control, whenever feasible, of local,37,38,39,40 systemic41,42,43,44,45 and drug-related risk factors (Table 1).46,47 On this basis, current prevention strategies46,48,49,50,51,52,53 may have limited effectiveness, if any. It should be kept in mind that the evidence behind such putative prevention strategies is often quite low;54 hence, the word prevention is probably not applicable in the particular case of BRONJ and it would be more reasonable to speak of risk reduction, although it is not possible to determine the amount of reduction and/or the residual risk on the basis of current evidence.
Bearing this in mind, what are the legal obligations, if any, of healthcare providers in relation to BRONJ 'prevention'? The prevention, if feasible, of known adverse reactions and complications of drug administration is a legal obligation of the prescribing physician. In the particular case of BP and BRONJ, this only implies trying to reduce the likelihood of known risk factors by means of careful attention and control, if feasible and consistent with the underlying disease requiring BP. These tasks require, or at least make opportune as well as clinically and legally sensible, the appropriate referral of the patient.
Dental professionals have the responsibility to ask the patient about their medical and drug history. If the patient is being treated (or has been ever treated) with BP, dental professionals need to inform the patient about BRONJ, its manifestation and the risks related to dental procedures. In addition, whenever surgical oral procedures are required, appropriate 'preventive strategies', if any, need to be taken into account.
Not all dental procedures are burdened with the same risk of triggering BRONJ;46 thus, only dental procedures with a significant potential risk (especially surgical procedures) may benefit from the adoption of 'prevention strategies'; nonetheless, it should be noted that this is not imperative since there is no standard of care currently defined. The scientific evidence behind such strategies is somewhat lacking,54 and the 'prevention strategies' themselves (for example, suspension of BP, antibiotic administration) may expose the patient to additional risks related to their own complications, which the managing practitioner is responsible for.
The patient is requested to maintain a strict adherence to dental/oral hygiene programmes in order to minimise the necessity to perform invasive dental procedures required by the onset and/or progression of undiagnosed and/or untreated dental/periodontal disorders. A well-informed, non-compliant patient who fails to act prudently by following responsible advice and instructions, and/or refusing speciality referrals may be adjudged negligent; this can be defined as contributory negligence (on the part of the patient/claimant) and may limit or exclude, according to the specific jurisdiction, healthcare practitioners' liability.
Diagnosis
BRONJ is currently defined as the occurrence of exposed bone in the maxillofacial region persisting for more than 8 weeks in a patient currently or previously treated with BP and with no history of radiation therapy to the jaw.55 Recently, this case definition has received some criticism56 due to increasing evidence that though bone exposure is an important sign of the disorder, it can be absent, at least in an early phase.6
Failure to diagnose BRONJ may be one of the complaints in litigation lawsuits; obviously, if a completely established BRONJ neglect occurs, there will be an inexcusable liability for the negligent practitioner.
On the other hand, diagnostic delay claims are also possible, which may be favoured by the lack of general agreement on the early manifestations of the disease. Thus, it would be sensible for the prudent and diligent practitioner to take into account early signs/symptoms of BRONJ, as well as signs/symptoms of unexposed forms of BRONJ, and, accordingly, provide adequate information to the patient and follow-up programmes. This is a duty for both prescribing physicians and dental professionals. In fact, when a correctly prescribed medication (or a correctly executed dental procedure) produces adverse reactions (or complications) in a well-informed patient, although the prescribing physician (or dental professional) is not liable for such occurrence, negligence may be attributed to the physician (or to the dental professional) if he/she fails to diagnose the reaction (or the complication) and to manage it accordingly. Appropriate actions should be undertaken to this end; in the particular case of BP administration and BRONJ, patients should be recalled on a regular basis:
-
1
By the prescribing physician in order to re-evaluate BP therapy indications consistently with the underlying condition; check the control of established risk factors, screen for the onset of new risk factors; check compliance with follow-up programmes for oral health maintenance and early BRONJ diagnosis; and check for early signs/symptoms of BRONJ
-
2
By dental professionals in order to check for and diagnose early signs/symptoms of BRONJ.
It is worth noting that legal obligations regarding BRONJ diagnosis also involve the patient. In fact, when a properly informed patient expresses his/her willingness to undertake risks inherent in treatment, he/she is required to be compliant with follow-up programmes and avoid missing and scheduling recall visits, otherwise the patient is liable for his own injuries. In addition, the patient who has been correctly informed of BRONJ manifestations should promptly alert the physician/dental professional of any suspected sign/symptom compatible with BRONJ, thus, favouring an early diagnosis.30,57
Treatment
When BRONJ is established the treatment may be challenging.35 Various treatment concepts have been proposed: conservative treatment includes pain control and local disinfection by mouth rinses, antibiotic therapy as well as superficial debridement (removing unfixed necrotic bone). On the other hand, surgical treatment includes any invasive surgical procedure aimed at resecting necrotic bone. The overall level of evidence concerning treatment strategies for BRONJ is rather low and, although the growing body of knowledge seems to contradict the common idea that surgery is contraindicated or less favourable, no sound evidence is actually available. Comparison of results between conservative and surgical treatment seems to show no difference regarding the success of treatment (for example, 60.5% vs 60.4%).58
Thus, it seems quite difficult for physicians and dental professionals to be held liable for the choice of a specific treatment concept (conservative vs surgical). In fact, a patient who sues a physician/dentist/oral surgeon must prove that a violation of the standard of care caused an injury (or a worse result). However, the standard of care is still undefined and answering the question as whether the result would have been better with another treatment option is still not feasible. Nonetheless, legal liability may occur if the selected treatment option is not performed with due diligence.
Conclusions
Whenever a claim for malpractice is made in a BRONJ case, it is mandatory to adequately weigh and attribute liability, if any, to the specific figure(s) by a comprehensive consideration of the chain of action leading up to the case, and potentially related to BRONJ. This can only be carried out on a case-by-case basis by careful analysis of any breach in informing, diagnosing, managing or referring the patient, together with the patient's behaviour in attending to prescriptions and follow-up programmes. Establishing liability is the premise for causation assessment of potential damages; this should also be performed on a case-by-case basis, and according to the laws and criteria of the specific jurisdiction. Whenever both liability and causation have been proved, the claimant is entitled for compensation.
References
Aapro M, Monfardini S, Jirillo A, Basso U . Management of primary and advanced breast cancer in older unfit patients (medical treatment). Cancer Treat Rev 2009; 35: 503–508.
Terpos E, Cibeira M T, Blade J, Ludwig H . Management of complications in multiple myeloma. Semin Haematol 2009; 46: 176–189.
Alonso-Coello P, Garcia-Franco A L, Guyatt G, Moynihan R . Drugs for pre-osteoporosis: prevention or disease mongering? BMJ 2008; 336: 126–129.
Lazarovici T S, Yahalom R, Taicher S, Elad S, Hardan I, Yarom N . Bisphosphonate-related osteonecrosis of the jaws: a single-centre study of 101 patients. J Oral Maxillofac Surg 2009; 67: 850–855.
Miksad R A, Lai K C, Dodson T B et al. Quality of life implications of bisphosphonate-associated osteonecrosis of the jaw. Oncologist 2011; 16: 121–132.
Fedele S, Porter S R, D'Aiuto F et al. Nonexposed variant of bisphosphonate-associated osteonecrosis of the jaw: a case series. Am J Med 2010; 123: 1060–1064.
Walter C, Grotz K A, Kunkel M, Al-Nawas B. Prevalence of bisphosphonate associated osteonecrosis of the jaw within the field of osteonecrosis. Support Care Cancer 2007; 15: 197–202.
McLeod N M, Davies B J, Brennan P A . Bisphosphonate osteonecrosis of the jaws; an increasing problem for the dental practitioner. Br Dent J 2007; 203: 641–644.
Statz T A, Guthmiller J M, Humbert L A, Johnson G K . Intravenous bisphosphonate-associated osteonecrosis of the jaw. J Periodontol 2007; 78: 2203–2208.
Bilezikian J P . Osteonecrosis of the jaw – do bisphosphonates pose a risk? N Engl J Med 2006; 355: 2278–2281.
Wu S, Dahut W L, Gulley J L . The use of bisphosphonates in cancer patients. Acta Oncol 2007; 46: 581–591.
Silverman S L, Maricic M . Recent developments in bisphosphonate therapy. Semin Arthritis Rheum 2007; 37: 1–12.
Khosla S, Bilezikian J P, Dempster D W et al. Benefits and risks of bisphosphonate therapy for osteoporosis. J Clin Endocrinol Metab 2012; 97: 2272–2282.
Nase J B, Suzuki J B . Osteonecrosis of the jaw and oral bisphosphonate treatment. J Am Dent Assoc 2006; 137: 1115–1119; quiz 69–70.
Dello Russo N M, Jeffcoat M K, Marx R E, Fugazzotto P . Osteonecrosis in the jaws of patients who are using oral biphosphonates to treat osteoporosis. Int J Oral Maxillofac Implants 2007; 22: 146–153.
Koka S, Clarke B L, Amin S, Gertz M, Ruggiero S L . Oral bisphosphonate therapy and osteonecrosis of the jaw: what to tell the concerned patient. Int J Prosthodont 2007; 20: 115–122.
Black D M, Bauer D C, Schwartz A V, Cummings S R, Rosen C J . Continuing bisphosphonate treatment for osteoporosis – for whom and for how long? N Engl J Med 2012; 366: 2051–2053.
Hoefert S, Schmitz I, Tannapfel A, Eufinger H . Importance of microcracks in aetiology of bisphosphonate-related osteonecrosis of the jaw: a possible pathogenetic model of symptomatic and non-symptomatic osteonecrosis of the jaw based on scanning electron microscopy findings. Clin Oral Investig 2010; 14: 271–284.
Reid I R, Cornish J . Epidemiology and pathogenesis of osteonecrosis of the jaw. Nat Rev Rheumatol 2012; 8: 90–96.
Bonacina R, Mariani U, Villa F, Villa A . Preventive strategies and clinical implications for bisphosphonate-related osteonecrosis of the jaw: a review of 282 patients. J Can Dent Assoc 2011; 77: b147.
Knight R J, Reddy C, Rtshiladze M A, Lvoff G, Sherring D, Marucci D . Bisphosphonate-related osteonecrosis of the jaw: tip of the iceberg. J Craniofac Surg 2010; 21: 25–32.
Lo Russo L, Lo Muzio L, Buccelli C, Di Lorenzo P . Bisphosphonates-related osteonecrosis of the jaws: medicolegal issues. Oral Dis 2013; 19: 425–426.
Lo Russo L, Lo Muzio L, Buccelli C, Di Lorenzo P . Reply to 'Medicolegal considerations in bisphosphonate-related osteonecrosis of jaw'. Oral Dis 2013; 19: 629–630.
Lo Russo L, Lo Muzio L, Buccelli C, Di Lorenzo P . Bisphosphonate-related osteonecrosis of the jaws: legal liability from the perspective of the prescribing physician. J Bone Miner Metab 2013; 31: 601–603.
Samanta A, Samanta J . Legal standard of care: a shift from the traditional Bolam test. Clin Med 2003; 3: 443–446.
Sooriakumaran P . The changing face of medical negligence law: from Bolam to Bolitho. Br J Hosp Med 2008; 69: 335–338.
Marx RE . Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg 2003; 61: 1115–1117.
Lopez-Jornet P, Camacho-Alonso F, Molina-Minano F, Gomez-Garcia F. Bisphosphonate-associated osteonecrosis of the jaw. Knowledge and attitudes of dentists and dental students: a preliminary study. J Eval Clin Pract 2010; 16: 878–882.
Woo S B, Hellstein J W, Kalmar J R . Narrative [corrected] review: bisphosphonates and osteonecrosis of the jaws. Ann Intern Med 2006; 144: 753–761.
Migliorati C A, Mattos K, Palazzolo M J . How patients' lack of knowledge about oral bisphosphonates can interfere with medical and dental care. J Am Dent Assoc 2010; 141: 562–566.
Dantas E . When consent is not enough: the construction and development of the modern concept of autonomy. Med Law 2011; 30: 461–475.
Bal B S, Choma T J . What to disclose? Revisiting informed consent. Clin Orthop Relat Res 2012; 470: 1346–1356.
Henk H, Teitelbaum A, Kaura S . Evaluation of the clinical benefit of long-term (beyond 2 years) treatment of skeletal-related events in advanced cancers with zoledronic acid. Curr Med Res Opin 2012; 28: 1119–1127.
Filleul O, Crompot E, Saussez S . Bisphosphonate-induced osteonecrosis of the jaw: a review of 2400 patient cases. J Cancer Res Clin Oncol 2010; 136: 1117–1124.
McLeod N M, Brennan P A, Ruggiero S L . Bisphosphonate osteonecrosis of the jaw: a historical and contemporary review. Surgeon 2012; 10: 36–42.
Pazianas M . Osteonecrosis of the jaw and the role of macrophages. J Natl Cancer Inst 2011; 103: 232–240.
Ficarra G, Beninati F, Rubino I et al. Osteonecrosis of the jaws in periodontal patients with a history of bisphosphonates treatment. J Clin Periodontol 2005; 32: 1123–1128.
Ruggiero S L, Mehrotra B, Rosenberg T J, Engroff S L . Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg 2004; 62: 527–534.
Marx R E, Sawatari Y, Fortin M, Broumand V . Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg 2005; 63: 1567–1575.
Badros A, Weikel D, Salama A et al. Osteonecrosis of the jaw in multiple myeloma patients: clinical features and risk factors. J Clin Oncol 2006; 24: 945–952.
Miyazaki H, Nishimatsu H, Kume H et al. Leukopenia as a risk factor for osteonecrosis of the jaw in metastatic prostate cancer treated using zoledronic acid and docetaxel. BJU Int 2012; 110: E520–525.
Otto S, Schreyer C, Hafner S et al. Bisphosphonate-related osteonecrosis of the jaws – characteristics, risk factors, clinical features, localization and impact on oncological treatment. J Craniomaxillofac Surg 2012; 40: 303–309.
Chiu C T, Chiang W F, Chuang C Y, Chang S W . Resolution of oral bisphosphonate and steroid-related osteonecrosis of the jaw – a serial case analysis. J Oral Maxillofac Surg 2010; 68: 1055–1063.
Wilkinson G S, Kuo Y F, Freeman J L, Goodwin J S . Intravenous bisphosphonate therapy and inflammatory conditions or surgery of the jaw: a population-based analysis. J Natl Cancer Inst 2007; 99: 1016–1024.
Jadu F, Lee L, Pharoah M, Reece D, Wang L . A retrospective study assessing the incidence, risk factors and comorbidities of pamidronate-related necrosis of the jaws in multiple myeloma patients. Ann Oncol 2007; 18: 2015–2019.
Campisi G, Lo Russo L, Agrillo A, Vescovi P, Fusco V, A B. BRONJ expert panel of the Italian Societies for Maxillofacial Surgery (SICMF) and Oral Pathology and Medicine (SIPMO) on bisphosphonate-related osteonecrosis of the jaws: risk assessment, preventive strategies and dental management. Ital J Maxillofac Surg 2011; 1–7.
Hoff A O, Toth B, Hu M, Hortobagyi G N, Gagel R F . Epidemiology and risk factors for osteonecrosis of the jaw in cancer patients. Ann N Y Acad Sci 2011; 1218: 47–54.
Ruggiero S, Gralow J, Marx R E et al. Practical guidelines for the prevention, diagnosis, and treatment of osteonecrosis of the jaw in patients with cancer. J Oncol Pract 2006; 2: 7–14.
Bagan J, Blade J, Cozar J M et al. Recommendations for the prevention, diagnosis, and treatment of osteonecrosis of the jaw (ONJ) in cancer patients treated with bisphosphonates. Med Oral Patol Oral Cir Bucal 2007; 12: E336–340.
Edwards B J, Hellstein J W, Jacobsen P L et al. Updated recommendations for managing the care of patients receiving oral bisphosphonate therapy: an advisory statement from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 2008; 139: 1674–1677.
Khan A A, Sandor G K, Dore E et al. Canadian Consensus Practice Guidelines for bisphosphonate associated osteonecrosis of the jaw. J Rheumatol 2008; 35: 1391–1397.
Ruggiero S L . Bisphosphonate-related osteonecrosis of the jaw (BRONJ): initial discovery and subsequent development. J Oral Maxillofac Surg 2009; 67(Suppl 5): 13–18.
McLeod N M, Patel V, Kusanale A, Rogers S N, Brennan P A . Bisphosphonate osteonecrosis of the jaw: a literature review of UK policies versus international policies on the management of bisphosphonate osteonecrosis of the jaw. Br J Oral Maxillofac Surg 2011; 49: 335–342.
Fedele S, Kumar N, Davies R, Fiske J, Greening S, Porter S . Dental management of patients at risk of osteochemonecrosis of the jaws: a critical review. Oral Dis 2009; 15: 527–537.
Ruggiero S L, Dodson T B, Assael L A, Landesberg R, Marx R E, Mehrotra B . American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws – 2009 update. J Oral Maxillofac Surg 2009; 67(Suppl 5): 2–12.
Colella G, Campisi G, Fusco V . American Association of Oral and Maxillofacial Surgeons position paper: Bisphosphonate-related osteonecrosis of the jaw – 2009 update: the need to refine the BRONJ definition. J Oral Maxillofac Surg 2009; 67: 2698–2699.
Bedogni A, Fusco V, Agrillo A, Campisi G . Learning from experience. Proposal of a refined definition and staging system for BRONJ. Oral Dis 2012; 18: 621–623.
Kuhl S, Walter C, Acham S, Pfeffer R, Lambrecht J T . Bisphosphonate-related osteonecrosis of the jaws- A review. Oral Oncol 2012; 48: 938–947.
Acknowledgements
Nothing in this article is intended nor should be construed to create or provide any legal standard of appropriate care or practice or to provide legal advice. Rather, every factual scenario must be evaluated on its own merits as to any proper standard of care and with regard to any potential specific causal link to injury.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Russo, L., Ciavarella, D., Buccelli, C. et al. Legal liability in bisphosphonate-related osteonecrosis of the jaw. Br Dent J 217, 273–278 (2014). https://doi.org/10.1038/sj.bdj.2014.806
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.806