Key Points
-
Outlines non-invasive treatment options for non-cavitated occlusal caries lesions.
-
Explores the uptake of minimal intervention dentistry in France.
-
Suggests changes to remuneration in dentistry would have a positive effect on the delivery of non-invasive treatment.
Abstract
Epidemiological data on dental caries show that prevention and treatment needs have evolved significantly over the past two decades. In younger patients the distribution of caries lesions is mainly found on the occlusal surfaces. The treatment approaches utilised by dentists must evolve to integrate preventive and treatment solutions tailored to the care needs, which are straightforward to implement in the dental office and whose effectiveness is underpinned by scientific evidence. This article aims to describe the principles of non-invasive management of non-cavitated (initial) occlusal caries lesions, based on evidence from recent studies published in the international literature.
Similar content being viewed by others
Introduction
Epidemiological data on dental caries show that prevention and treatment needs have evolved significantly over the past two decades.boxed-text
The prevalence and severity of dental caries has decreased in young people over the last 20 years, both in France and in other industrialised countries.1 For example, in 1987 11.9% of French children aged 12 were 'caries-free' in their permanent teeth, compared to 55.9% in 2006, while the DMFT (D = decayed, M = missing, F = filled, T = teeth) decreased from 4.2 to 1.2 respectively.2 These results are encouraging, however, since the DMFT records only cavitated caries lesions and does not include the earlier non-cavitated stages of caries lesions, these results significantly underestimate the reality.3 Although it appears essential, both from an epidemiological and clinical point of view, to take into account all caries lesions, whatever the stage of development, currently in France only one study has included the assessment of non-cavitated carious lesions.1
Epidemiological studies show that care needs are concentrated in certain sectors of the population who have high levels of caries. Kaste et al. in 1996 reported that, in the United States, 80% of caries lesions were concentrated in about 25% of children and adolescents aged 6-15 years.4 Moreover, in 2004, Macek et al. confirmed this trend reporting that 33% of a population of six-year-olds accounted for 75% of caries lesions.5 These data illustrate that dental caries is concentrated in risk groups defined in particular by social disadvantage or special needs such as those with disabilities and the elderly.6
Epidemiological trends have also been observed in the distribution of caries lesions in the mouth, today preferentially affecting the occlusal surfaces among the young.7
The treatment approaches utilised by dentists must evolve to integrate preventive and treatment solutions tailored to the care needs, which are straightforward to implement in the dental office and whose effectiveness is underpinned by scientific evidence (evidence-based interventions). This article will describe the principles of non-invasive management of non-cavitated (initial) occlusal caries lesions, based on evidence from recent studies published in the international literature.
Terminology
Beauchamp et al.8 describe a non-cavitated caries lesion in pits and fissures as a lesion in fully erupted teeth 'that may display discolouration not due to extrinsic staining, developmental opacities or fluorosis. The discolouration may be confined to the size of a pit or fissure or may extend to the cusp inclines surrounding a pit or fissure. The tooth surface should have no evidence of a shadow indicating dentinal caries, and, if radiographs are available, they should be evaluated to determine that neither the occlusal nor proximal surfaces have signs of dentinal caries'. It might be questioned why this definition did not incorporate non-cavitated caries lesions with dentinal involvement since when the lesion is confined to the outer third or the middle third of the dentine the non-invasive treatment options are the same - usually a therapeutic sealant.9
There remains confusion due to terminology used. Initial lesions, early lesions, pre-cavitated lesions, non-cavitated lesions, hidden caries lesions (without collapse of the enamel) are all terms that can be defined differently according to different interpretations and classifications. Does 'initial' mean that the caries lesion is confined to enamel? Similarly, does 'early' mean that the caries lesion is non-cavitated affecting both the enamel and dentine? What is the difference between pre-cavitated and non-cavitated?
In clinical terms and in terms of lesion management it seems more pertinent to make a distinction between cavitated and non-cavitated lesions; the latter term includes all those stages in the evolution of a caries lesion from the first signs of demineralisation (early lesions, initial lesions) through to the presence of a dentine lesion without cavitation (Fig. 1).10
What treatment choices? Restorative treatment, therapeutic sealant or simple follow-up? a) Longitudinal section of a non-cavitated occlusal caries lesion limited to the external half of the enamel; b) Longitudinal section of a non-cavitated occlusal caries lesion extending to the dentino-enamel junction. Photograph courtesy of Dr Marie Maltrait (UFR d'Odontologie, Clermont-Ferrand, France)
The conceptual basis for non-invasive management of non-cavitated caries lesions
Invasive treatment involving the placement of a restoration, even when a minimal invasive approach such as air-abrasion or micro-preparation is used, condemns the tooth irreversibly to a repeat restoration cycle, since no restoration can be considered permanent and will ultimately need to be replaced.11 The replacement of a restoration often involves additional tissue loss that in turn affects the long-term prognosis with respect to the vitality and longevity of the tooth.12 Invasive treatment should only be provided when the potential to halt the progression of the caries process has failed or when the residual tooth tissue is weak and at risk of fracture. Clinically, therefore, the threshold for restoration usually corresponds to a level of caries progression reaching the middle third of the dentine and/or the occurrence of definitive cavitation through the overlying enamel.
Currently, a non-invasive approach to the management of non-cavitated occlusal caries lesions appears to be the most ethical since even if it might eventually fail, that is, the caries lesion progresses, one can always resort to a minimally invasive restorative approach. In France this non-invasive approach is part of several best practice recommendations, including those of the French High Authority for Health (HAS), which states that an invasive approach to the management of enamel lesions in pits and fissures is not advocated.13 Unfortunately these recommendations are rarely applied in routine dental practice since studies have shown that non-invasive treatment is implemented in an anecdotal manner and that the threshold for intervention with restorative treatment is low with many French practitioners providing restorations for enamel lesions that could have been managed from non-invasive treatment.14 Similar findings have been reported in other countries such as the United States where a questionnaire survey on the use of sealants (preventive and therapeutic) conducted in 2011 showed that less than 40% of practitioners sealed fissures with non-cavitated caries lesions. Moreover, less than 4% of practitioners would use a sealant for a non-cavitated caries lesion extending radiographically into the outer one-half of dentine.15
Detection and classification
Tools for the detection of caries using a variety of technologies including dyes, transillumination, fluorescence, laser fluorescence, electrical conductance and others continue to multiply on the dental marketplace, but no single one in isolation replaces the two traditional techniques – visual examination and bitewing radiographs. Indeed, the ideal detection tool must meet three criteria: sensitivity (ability to detect all cases), specificity (ability to reduce false positives) and reproducibility of results (the ability to produce the same results irrespective of operator). Visual examination and bitewing radiographs, used together, remain the most pertinent caries detection tools in clinical practice.16,17
The recently developed International Caries Detection and Assessment System II (ICDAS II) lists the visual stages of caries and correlates these with histological changes in the lesion to propose a classification with six severity codes (http://www.icdas.org/). The ICDAS II system has the advantage in that it can draw clinicians' attention to the need to identify the various stages in the development of caries lesions, particularly non-cavitated lesions, so that the most appropriate management can be applied. It should, however, be noted that:
-
Codes 1 and 2 differentiate between the first visual changes in enamel and a distinctive visual change in enamel, the former after cleaning and prolonged air-drying, the latter visible without air-drying. The clinical relevance of this distinction may be questioned since both types of lesion can be managed with the same non-invasive treatment
-
Currently, no therapeutic guide is still associated with this system, thus making it unattractive for clinical practice
-
Detailed training is required to ensure the reproducibility of results and especially the distinction between non-cavitated stages of caries.
Non-invasive management of non-cavitated occlusal caries lesions
This section will deal with:
-
The two main therapeutic approaches: remineralisation and therapeutic sealants. Remineralisation involves the use of agents aimed to promote the regeneration of hard tissue while therapeutic sealants aim to halt the caries process by depriving the bacteria in the lesion of fermentable substrate
-
Caries lesion monitoring, a strategy to consider if the diagnosis, that is, the presence of a lesion and its activity, is equivocal.
Some authors recommend the use of antibacterial agents, such as chlorhexidine, to halt the caries process.18 If the preventive action is certain, the therapeutic efficacy for non-cavitated caries lesions has yet to be shown.
Remineralisation
Fluoride for remineralisation of caries lesions is the most widely described agent in the literature and the most extensively used. There are several forms of fluoride used including NaF, Acidulated fluorophosphate APF, SnF2, that may be used in various concentrations either for professional topical application (varnish, gel) or home use (toothpaste, mouthwash, gel).19
Many studies have confirmed the effectiveness of fluoride as a means of preventing caries lesions, but fluoride can also play an important role in the process of remineralisation of non-cavitated caries lesions.
Fluoride toothpastes
The cario-preventive effect of fluoride toothpastes is well established as is their potential to arrest the caries process in the case of root caries lesions, proximal lesions and certain dentinal lesions.20,21,22,23 Unfortunately, no data are currently available regarding the effectiveness of fluoride toothpastes on the remineralisation of non-cavitated occlusal lesions.
Toothpastes are available with different concentrations of fluoride; from 500 ppm to 13,500 ppm. The most commonly used concentration in adults is between 1,000 and 1,500 ppm, but it is pertinent to increase the fluoride concentration to potentiate the preventive effect in cases presenting with a high risk of caries or for the remineralisation of caries lesions.20
Note: The lack of evidence regarding the effectiveness of fluoridated toothpaste with over 1,000 ppm of fluoride on the remineralisation of non-cavitated occlusal caries lesions should not hinder them from being prescribed in so much as their preventive effect and their potential to remineralise other types of lesion has been established.21 The prescription of high fluoride toothpastes must be based on the level of caries risk of the patient.
Fluoride varnishes
Fluoride varnishes were introduced on the market in the 1960s.24 A review of the literature on the subject, published by the Cochrane group, concluded that there was a non-negligible cario-preventive effect of varnish both in the primary and permanent dentition although more research needs to be conducted to discern the contribution from fluoride toothpastes from that of fluoride varnish.25 Other systematic reviews of the literature, however, are less optimistic about the level of evidence available as well as their long-term cario-preventive effect.26
The effect of fluoride varnishes on non-cavitated carious lesions remains to be clearly established, although some evidence is available concerning their use for arresting the caries process both in primary and permanent teeth.27,28 It appears, however, that sealants provide better clinical results when compared to varnishes.29
Note: Fluoride varnishes do not currently provide the most appropriate therapeutic solution for the management of non-cavitated occlusal caries lesions. While it is likely that fluoride varnishes have the potential to arrest the progression of non-cavitated occlusal caries lesions, the in vivo evidence is limited. Moreover, other factors that must be taken into account concerning the use of varnishes is the cost-effectiveness of this therapeutic approach as well as the need for the cooperation of patients who will need to have the varnish professionally applied at least twice a year.
CPP-ACP and CPP-AFCP
Recently, products containing CPP-ACP (casein phosphopeptide–amorphous calcium phosphate) and CPP-AFCP (casein phosphopeptide–amorphous calcium phosphate fluoride) have been introduced. These agents appear to be promising in the non-invasive management of carious lesions by promoting phosphate remineralisation, but the current lack of clinical studies do not permit any firm conclusions to be drawn about the effectiveness of these agents.30,31
Therapeutic sealants
Pit and fissure sealants were developed in the 1960's. Their cario-preventive efficacy (primary prevention) has been widely documented over the years and has been the subject of several systematic reviews.32,33
A study published by Heller et al. in 1995 helped to define guidelines for the use of preventive sealants targeted at patients with high caries risk and therapeutic sealants in the case of non-cavitated carious lesions.34 This retrospective study investigated the benefits of sealants on the evolution of the caries process for sound occlusal surfaces and surfaces with non-cavitated caries lesions in first permanent molars. After five years, for initially sound surfaces, 12.5% of non-sealed surfaces developed caries lesions compared to 8.1% for sealed surfaces. In contrast, the results were particularly interesting concerning the therapeutic sealants of non-cavitated occlusal lesions where only 10.8% of the sealed lesions had progressed against 51.8% for non-sealed lesions. This study helped in the development of the concept of targeted use of sealants as a preventive measure for high caries risk patients and the use of therapeutic sealants to manage non-cavitated carious lesions.
It is now accepted that sealants occupy a place in the minimum intervention therapeutic armamentarium and are, in fact, indicated not only for cases of non-cavitated occlusal caries lesions but also for sealing open margins of old restorations.35,36,37 When used in such cases, they are defined as 'therapeutic' sealants and can be likened to a form of secondary prevention.
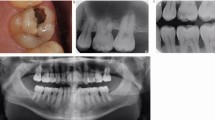
The sealing of caries lesions (Fig. 2)
a) Clinical view of a lower first permanent molar; note the presence of enamel opacities without drying suggesting a caries lesion extending through all the thickness of the enamel of ICDAS score 2 (ICDAS II); the absence of a dark zone in the adjacent dentine confirms it is an enamel lesion and a lesion of ICDAS score 4. b) A therapeutic sealant was provided using a high viscosity glass ionomer (FUJI IX® - GC) using the ART 'press-finger' technique.46 Photograph courtesy of Dr Soraya Leal (University of Asa Norte, Asa Norte, Brazil)
In 2008, Griffin et al. published a systematic review on the effectiveness of therapeutic sealants in preventing the progression of non-cavitated caries lesions of the pits and fissures of permanent teeth.9 Based on six randomised clinical trials, it was concluded that therapeutic sealants were indicated for the management of non-cavitated carious lesions in permanent teeth in children, adolescents and young adults with a reduced probability of annual increase of occlusal caries lesions after sealing versus unsealed (a factor of about three).
In the American Dental Association (ADA) recommendations on sealant use they are recommended for non-cavitated occlusal lesions but not for teeth with 'evidence of a shadow indicating dentinal caries' or radiographic evidence of occlusal or proximal signs of dentinal caries.8 These recommendations are obviously cautious considering the evidence base relating to sealed caries lesions. It is therefore plausible that the use of therapeutic sealants could be extended to more advanced lesions. In this respect, Bakhshandeh et al. state: 'cavity formation with exposed dentine does not make it mandatory to restore a lesion automatically.'38 Their study conducted in adults showed a success rate of 90% over a period of two to three years with the arrest of the caries process following the placement of a sealant for lesions extending to the middle-third of dentine with some lesions exhibiting cavitation. Moreover, Borges et al. in 2010 presented results comparing therapeutic sealants and no treatment for non-cavitated occlusal lesions caries extending as far the middle third of dentine in permanent teeth.39 They found that over a period of a year 96% of non-treated lesions progressed compared to only 3.8% of sealed lesions and that caries progression in the treated teeth only occurred when the sealant had been lost. These results were maintained over a three-year period.40
Although sealants are most often associated for use in younger patients, they also have a use in both preventive and therapeutic applications for adults as stipulated by the ADA recommendations based on a high level of evidence.8 In this respect, there is an ever-growing scientific evidence base that the placement of therapeutic sealants result in the isolation of cariogenic bacteria from their source of nutrition, which leads to their inactivation. The caries process is then stopped41 or even reversed.42,43,44
Different types of materials are available for the placement of therapeutic sealants: resin composite sealants, glass ionomer cements (GIC) especially high viscosity or resin modified GICs (RMGIC), and compomers.
Beauchamp et al. reported in a recent systematic review that although glass ionomer sealants show lower retention rates compared to composite resin sealants, there is limited and conflicting evidence that glass ionomer cement reduces caries incidence.8,45 Glass ionomer sealants have the advantage of being easier to place under difficult operating conditions since they are less sensitive to moisture. In addition, they adhere spontaneously to even demineralised enamel.45 Their low mechanical strength characteristics have been improved through the introduction on the market of high viscosity glass ionomer cements and these are used with atraumatic restorative treatment (ART) sealants.46
Compomers made their appearance in the 1990s. Unlike conventional glass ionomers, the fluoride release of these materials is questionable, and there are not enough studies to validate their effectiveness as sealants.8
Composite resin sealants are mechanically strong and provide very good adhesion to the enamel when it is mineralised and supported by underlying dentine.8 Beauchamp et al. recommend composite resin as the material of choice for sealants and advocate the use of glass ionomer only as an 'interim preventive agent' for circumstances when conditions are unfavourable to the use of a composite resin sealant, such as when isolation of the operating field is difficult.8
Notes:
-
The isolation of the operating site is often cited as a significant factor influencing the clinical success of sealants and some recommend the use of a rubber dam for the placement of sealants. The scientific evidence does not, however, support this recommendation to the extent that studies have shown similar clinical results irrespective of whether the isolation has been effected with a rubber dam or with cotton wool rolls. Dental practitioners must therefore act pragmatically. For instance, when composite resin sealants are being used and saliva control cannot be effectively achieved using cotton wool rolls, then the use of a rubber dam might be advisable. Likewise, even if high viscosity glass ionomers are less sensitive to moisture than composite resins at the time of placement, their use still requires adequate salivary control
-
It is traditionally recommended to prepare the surface to be sealed by polishing with a mixture of pumice and water. Once again, the clinical evidence that this is necessary is lacking and current recommendations are only to clean the surface to be sealed with a rotating brush or to use a toothbrush.
The sealing of marginal gaps of restorations (restoration repair) (Fig. 3)
a) Clinical view in 2003; b) Clinical view in 2004 with therapeutic sealant placed; c) Clinical view in 2005; d) Clinical view in 2007. Photographs kindly supplied by Dr G. Moncada (University of Chile, Santiago, Chile), Dr V. Gordan (University du Chile, Santiago, Chile) and Dr I. Mjör (University of Florida, Gainesville, USA)
When restorations are replaced, healthy dental tissue is permanently removed47 with a potential impact on the longevity of the tooth in the arch.12 For this reason, and when it is possible, it is always better to attempt to repair a restoration rather than to undertake a full replacement.
In many countries, a non-negligible part of the working time of dentists involves the replacement of so-called 'defective restorations' and restorations with recurrent caries lesions. The main reason given for failure of restorations is the development of recurrent caries lesions.48 It is important to note that the diagnosis of these lesions is difficult and often arbitrary,49 for example, the blue-grey colouring on the margins of amalgam restorations is an unreliable indicator of the presence of secondary caries lesions50 and the presence of a marginal gap on a restoration are correlated to the presence of recurrent caries only when they are greater than 0.5 mm wide, which is extremely difficult to assess clinically.51
Several methods can be used to repair defective restorations including polishing the edges of the margins, the sealing of the gap, or a partial replacement of the restoration.52 These approaches are an integral part of the therapeutic armamentarium of minimal intervention but unfortunately remain rarely used despite their obvious benefits.35
The sealing of a marginal gap can be achieved using a resin sealant, a flowable glass ionomer cement or a resin composite following routine clinical protocols for each material.
Monitoring of 'suspected' or arrested caries lesions
Monitoring is another option to consider with a suspected caries lesion, where clinical and radiographic findings do not allow one to confirm or rule out the presence of a lesion with certainty, or where a lesion appears to be stable or arrested. This does not imply that one leaves an initial lesion to progress since this monitoring option must be part of overall caries disease management, taking into account risk factors and specific recommendations for each clinical case.53 Many practitioners are reluctant to take this option considering it to be 'risky'. It is true that it is difficult to predict the likelihood of progression of caries lesions and the literature provides only limited data. However, the risk is low to the extent that, even if the caries process is not completely halted the progression of both enamel and dentine caries lesions is relatively slow in those with exposure to fluoride.54,55
Monitoring should be considered when there is a doubt about the presence of a lesion and when it is possible to manage the patient's risk factors. It is better to delay an invasive intervention for a few years to confirm that a suspected lesion has progressed than to expose the patient to over-treatment from the outset. If the patient's risk factors cannot be managed, it is preferable to consider the placement of a sealant on the occlusal surfaces.
The realities of non-invasive management of caries in general dental practicein France
In general, there is very little data on use of non-invasive or minimally invasive care for dental caries in general practice in France. The little data that are available are quite disappointing in terms of the adoption of rational concepts of caries management.
Remineralisation treatment
No data are available regarding the use of this technique in general practice in France.
Sealants
A study conducted in Germany and France in the late 1990s showed that 63.2% of children aged 12 years in Heidelberg had at least one tooth sealed against only 6.8% in Montpellier.56 This study, however, took place before the Nomenclature Générale des Actes Professionnels (NGAP), the list of treatment items that can be reimbursed by the French social security, had incorporated preventive sealants for the first and second permanent molars in patients under 14 years and with high caries risk, a modification that took place in 2001. Analysis of the database of the National Health Insurance Fund for Salaried Workers (CNAMTS) showed that up till June 2004, the inclusion of sealants in the NGAP had increased the number of sealants provided.13 Even so, according to Lupi-Pegurier in 2005, sealants accounted for less than 13% of conservative dentistry acts among children aged six to eight years.57 The reimbursement for preventive sealants was upgraded in 2006, but the effect of this measure has not yet been investigated.
The limited use of preventive and non-invasive techniques for caries management in France was shown from a survey conducted in 2004 where 26 general practitioners working in the Auvergne region were asked to describe their professional practices relating to conservative dentistry.58 Of 921 items of treatment provided for vital teeth, 608 were primary treatment items divided into 516 restorations, only 80 sealants and 12 other forms of treatment.
There is no data available regarding the use of therapeutic sealants in general practice in France. An analysis of international literature shows that there is growing evidence for the importance of therapeutic sealants. For example, the American Dental Association recommends sealing of non-cavitated occlusal caries lesions in children and young adults. Even so American dentists are reluctant to leave decayed tissue under adhesive restorations and generally they do not apply these recommendations.8,15,59,60
Repair of restorations (Fig. 3)
In the 1980s, Mjor showed that the ratio of re-restoration/restoration was high: 80/20 for composite resins and 70/30 for amalgam.61 Data collected more recently are more encouraging with a ratio of about 50/50, with variations depending on the country and the population studied.48
A 2002 study by the URCAM (Union nationale des caisses d'assurance maladie) in the French region of Franche Comté showed that 22% of the restorations examined on average 7.5 months after their completion had a major flaw (secondary caries, dentine exposure, tooth fracture or restoration loss) that required urgent attention.62
A survey of dentists practising in the Auvergne region of France showed that of 921 treatments provided for vital teeth, 313 were replacement restorations and the percentage of these in relation to the total volume of restorative care (invasive or non-invasive) ranged from 4.8% to 62.9% depending on the practitioner. The amount of non-invasive treatment provided was anecdotal, involving the polishing of nine restorations, two repairs through partial replacement of a restoration and one sealant.62
Despite the publication in France of guidelines on prevention that incorporate aspects of minimal intervention (HAS 2010), the practice of dentistry continues to place emphasis on restorative treatment at the expense of preventive care. The reasons for the delay in integrating new concepts in everyday practice in France are certainly multiple and include:
-
The lack of training in the area of minimal intervention
-
The failure to recognise therapeutic sealants in the NGAP, the list of treatments that can be reimbursed by the social security: preventive sealants provided after the age of 14 years and therapeutic sealants are not listed and can only be provided after a quotation has been given to the patient
-
The failure of the NGAP to recognise remineralisation techniques and lesion monitoring – again these acts are subject to the acceptance by the patient of a quotation
The difficulty in proposing non-reimbursed forms of treatment to French patients who are used to go to the dentist for restorative treatment rather than pay for remineralisation treatment, sealants, or to receive advice on prevention, the use of appropriate fluoride products, nutrition counselling, and the monitoring of lesion remineralisation, etc.
Would it not make sense to provide a reimbursement fee for non-invasive procedures whose effectiveness is recognised rather than continuing to promote invasive procedures that are notoriously iatrogenic?
Conclusion
The appropriate management of occlusal caries lesions is highly relevant considering the epidemiological changes in the pattern of dental caries and the preventive and treatment options now available. The techniques discussed in this article should be considered in clinical practice for the management of non-cavitated occlusal caries lesions involving the enamel or involving the outer third of dentine. It can now be considered to be ethically incorrect to systematically undertake invasive treatment involving cavity preparation and placement of a restoration for these lesions. Non-invasive treatment should not, however, be considered in isolation but must be part of a comprehensive minimal intervention treatment plan incorporating the assessment and management of risk factors, early detection of caries lesions, treatment methods that respect and conserve healthy tooth tissue and pulp vitality, prevention and tailored recall.
Currently there is an ethical dilemma in France. It is difficult to propose clinically appropriate preventive and non-invasive management of caries lesions when this treatment is not reimbursed by the health system, a system that only reimburses invasive restorative treatment where the longevity is often uncertain and the effect on the caries process virtually nil. This aspect of public health would be resolved if the profession could be mobilised to demand a revision of the fee scales based on current scientific knowledge and would permit patients to benefit from care appropriate to their needs.
Additional note
This article was originally prepared for French dental practitioners working within the healthcare system as it currently exists in France. For that reason the article refers to data pertinent to France with respect to epidemiological findings and reimbursement for dental procedures.
While there is little up-to-date data on the use of sealants generally in France, their use appears to lag behind the United Kingdom where the 2003 survey of children's dental health showed that 13% of 8-year-olds and 30% of 15-year-olds had sealants on permanent teeth.64 Unfortunately, this data does not stipulate what proportion of these sealants constituted therapeutic sealants.
This current article complements a recent article published in the British Dental Journal by Deery on caries detection and diagnosis, sealants and management of the possibly carious fissure.65 Both articles highlight the need to adopt non-invasive methods through a minimal intervention approach for the management of non-cavitated occlusal caries lesions both in children and adults.
References
Joseph C, Velley A M, Pierre A, Bourgeois D, Muller-Bolla M. Dental health of 6-year-old children in Alpes Maritimes, France. Eur Arch Paediatr Dent 2011; 12: 256–263.
Hescot P, Roland E . La santé dentaire en France: les enfants de 6 et 12 ans. UFSBD 2006.
Pitts N B, Fyffe H E . The effect of varying diagnostic thresholds upon clinical caries data for a low prevalence group. J Dent Res 1988; 67: 592–596.
Kaste L M, Selwitz R H, Oldakowski R J, Brunelle J A, Winn D M, Brown L J . Coronal caries in the primary and permanent dentition of children and adolescents 1–17 years of age: United States, 1988–1991. J Dent Res 1996; 75: 631–641.
Macek M D, Heller K E, Selwitz R H, Manz M C . Is 75 percent of dental caries really found in 25 percent of the population? J Public Health Dent 2004; 64: 20–25.
Haut Comité de la Santé Publique. La progression de la précarité en France et ses effets sur la santé. Edited by the l'ENSP. Rennes: Haut Comité de la Santé Publique, 1998.
McDonald S P, Sheiham A . The distribution of caries on different tooth surfaces at varying levels of caries: a compilation of data from 18 previous studies. Community Dent Health 1992; 9: 39–48.
Beauchamp J, Caufield P W, Crall J J et al. Evidence-based clinical recommendations for the use of pit-and-fissure sealants: a report of the American Dental Association Council on Scientific Affairs. J Am Dent Assoc 2008; 139: 257–268.
Griffin S O, Oong E, Kohn W et al. The effectiveness of sealants in managing caries lesions. J Dent Res 2008; 87: 169–174.
Ekstrand K R . Improving clinical visual detection-potential for caries clinical trials. J Dent Res 2004; 83: C67–71.
Elderton R J . Clinical studies concerning re-restoration of teeth. Adv Dent Res 1990; 4: 4–9.
Brantley C F, Bader J D, Shugars D A, Nesbit S P . Does the cycle of rerestoration lead to larger restorations? J Am Dent Assoc 1995; 126: 1407–1413.
Haute Autorité de la Santé. Appréciation du risque carieux et indications du scellement prophylactique des sillons des premières et deuxièmes molaires permanentes chez les sujets de moins de 18 ans. Saint Denis La Pleine: HAS, 2005.
Doméjean-Orliaguet S, Tubert-Jeannin S, Riordan P J, Espelid I, Tveit A B . French dentists' restorative treatment decisions. Oral Health Prev Dent 2004; 2: 125–131.
Tellez M, Grey S L, Grey S, Lim S, Ismail A I . Sealants and dental caries: dentists' perspectives on evidence-based recommendations. J Am Dent Assoc 2011; 142: 1033–1040.
Guerrieri A, Gaucher C, Bonte E, Lasfargues J J . Détection et diagnostic des lésions carieuses initiales. Réalités Cliniques 2011; 22: 141–156.
Haute Autorité de la Santé. Guide des indications et des procédures des examens radiologiques en odontostomatologie. Recommandations pour les professionnels de santé. Saint Denis La Pleine: HAS, 2006.
James P, Parnell C, Whelton H . The caries-preventive effect of chlorhexidine varnish in children and adolescents: a systematic review. Caries Res 2010; 44: 333–340.
Newbrun E . Topical fluorides in caries prevention and management: a North American perspective. J Dent Educ 2001; 65: 1078–1083.
Nordstrom A, Birkhed D . Preventive effect of high-fluoride dentifrice (5,000 ppm) in caries-active adolescents: a 2-year clinical trial. Caries Res 2010; 44: 323–331.
Walsh T, Worthington H V, Glenny A M, Appelbe P, Marinho V C, Shi X . Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2010; CD007868.
Schwarz E, Lo E C, Wong M C . Prevention of early childhood caries-results of a fluoride toothpaste demonstration trial on Chinese preschool children after three years. J Public Health Dent 1998; 58: 12–18.
Lynch E, Baysan A . Reversal of primary root caries using a dentifrice with a high fluoride content. Caries Res 2001; 35: 60–64.
Chu C H, Lo E C . A review of sodium fluoride varnish. Gen Dent 2006; 54: 247–253.
Marinho V C, Higgins J P, Logan S, Sheiham A . Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev 2002; CD002279.
Petersson L G, Twetman S, Dahlgren H et al. Professional fluoride varnish treatment for caries control: a systematic review of clinical trials. Acta Odontol Scand 2004; 62: 170–176.
Autio-Gold J T, Courts F . Assessing the effect of fluoride varnish on early enamel carious lesions in the primary dentition. J Am Dent Assoc 2001; 132: 1247–1253.
Seppa L, Hausen H, Tuutti H, Luoma H . Effect of a sodium fluoride varnish on the progress of initial caries lesions. Scand J Dent Res 1983; 91: 96–98.
Hiiri A, Ahovuo-Saloranta A, Nordblad A, Makela M . Pit and fissure sealants versus fluoride varnishes for preventing dental decay in children and adolescents. Cochrane Database Syst Rev 2010; CD003067.
Cochrane N J, Cai F, Huq N L, Burrow M F, Reynolds E C . New approaches to enhanced remineralization of tooth enamel. J Dent Res 2010; 89: 1187–1197.
Azarpazhooh A, Limeback H . Clinical efficacy of casein derivatives: a systematic review of the literature. J Am Dent Assoc 2008; 139: 915–924.
Ahovuo-Saloranta A, Hiiri A, Nordblad A, Makela M, Worthington H V . Pit and fissure sealants for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database Syst Rev 2008; CD001830.
Gooch B F, Griffin S O, Grey S K et al. Preventing dental caries through school-based sealant programmes: updated recommendations and reviews of evidence. J Am Dent Assoc 2009; 140: 1356–1365.
Heller K E, Reed S G, Bruner F W, Eklund S A, Burt B A . Longitudinal evaluation of sealing molars with and without incipient dental caries in a public health programme. J Public Health Dent 1995; 55: 148–153.
Tyas M J, Anusavice K J, Frencken J E, Mount G J . Minimal intervention dentistry: a review. FDI Commission Project 1–97. Int Dent J 2000; 50: 1–12.
Simonsen R J . From prevention to therapy: minimal intervention with sealants and resin restorative materials. J Dent 2011; 39 (Suppl 2): S27–33.
Fernandez E M, Martin J A, Angel P A, Mjor I A, Gordan V V, Moncada G A . Survival rate of sealed, refurbished and repaired defective restorations: 4-year follow-up. Braz Dent J 2011; 22: 134–139.
Bakhshandeh A, Qvist V, Ekstrand K R . Sealing occlusal caries lesions in adults referred for restorative treatment: 2–3 years of follow-up. Clin Oral Investig 2011; 16: 521–9.
Borges B C, Campos G B, da Silveira A D, de Lima K C, Pinheiro I V . Efficacy of a pit and fissure sealant in arresting dentin non-cavitated caries: a 1-year follow-up, randomized, single-blind, controlled clinical trial. Am J Dent 2010; 23: 311–316.
Borges B C, de Souza Borges J, Braz R, Montes M A, de Assunção Pinheiro I V . Arrest of non-cavitated dentinal occlusal caries by sealing pits and fissures: a 36-month, randomised controlled clinical trial. Int Dent J 2012; 62: 251–255.
Gore D R . The use of dental sealants in adults: a long-neglected preventive measure. Int J Dent Hyg 2010; 8: 198–203.
Oong E M, Griffin S O, Kohn W G, Gooch B F, Caufield P W . The effect of dental sealants on bacteria levels in caries lesions: a review of the evidence. J Am Dent Assoc 2008; 139: 271–278.
Mertz-Fairhurst E J, Curtis J W Jr., Ergle J W, Rueggeberg F A, Adair S M . Ultraconservative and cariostatic sealed restorations: results at year 10. J Am Dent Assoc 1998; 129: 55–66.
Alves L S, Fontanella V, Damo A C, Ferreira de Oliveira E, Maltz M . Qualitative and quantitative radiographic assessment of sealed carious dentin: a 10-year prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010; 109: 135–141.
Splieth C H, Ekstrand K R, Alkilzy M et al. Sealants in dentistry: outcomes of the ORCA Saturday Afternoon Symposium 2007. Caries Res 2010; 44: 3–13.
Holmgren C J, Roux D, Doméjean S . Minimal intervention dentistry: part 5. Atraumatic restorative treatment (ART) – a minimum intervention and minimally invasive approach for the management of dental caries. Br Dent J 2013; 214: 11–18.
Gordan V V . In vitro evaluation of margins of replaced resin-based composite restorations. J Esthet Dent 2000; 12: 209–215.
Mjor I A . Clinical diagnosis of recurrent caries. J Am Dent Assoc 2005; 136: 1426–1433.
Merrett M C, Elderton R J . An in vitro study of restorative dental treatment decisions and dental caries. Br Dent J 1984; 157: 128–133.
Magalhaes C S, Freitas A B, Moreira A N, Ferreira E F . Validity of staining and marginal ditching as criteria for diagnosis of secondary caries around occlusal amalgam restorations: an in vitro study. Braz Dent J 2009; 20: 307–313.
Kidd E A, Joyston-Bechal S, Beighton D . Marginal ditching and staining as a predictor of secondary caries around amalgam restorations: a clinical and microbiological study. J Dent Res 1995; 74: 1206–1211.
Gordan V V, Riley J L 3rd, Blaser P K, Mondragon E, Garvan C W, Mjor I A . Alternative treatments to replacement of defective amalgam restorations: results of a seven-year clinical study. J Am Dent Assoc 2011; 142: 842–849.
Anusavice K . Clinical decision-making for coronal caries management in the permanent dentition. J Dent Educ 2001; 65: 1143–1146.
Lawrence H P, Benn D K, Sheiham A . Digital radiographic measurement of approximal caries progression in fluoridated and non-fluoridated areas of Rio de Janeiro, Brazil. Community Dent Oral Epidemiol 1997; 25: 412–418.
Mejare I, Stenlund H, Zelezny-Holmlund C. Caries incidence and lesion progression from adolescence to young adulthood: a prospective 15-year cohort study in Sweden. Caries Res 2004; 38: 130–141.
Schulte A, Rossbach R, Tramini P . Association of caries experience in 12-year-old children in Heidelberg, Germany, and Montpellier, France, with different caries preventive measures. Community Dent Oral Epidemiol 2001; 29: 354–361.
Lupi-Pegurier L, Poullie A, Martel P, Muller-Bolla M. Scellement prophylactique des sillons des premières et deuxièmes molaires permanentes. Rev Odont Stomat 2008; 37: 199–207.
Domejean-Orliaguet S, Leger S, Auclair C, Gerbaud L, Tubert-Jeannin S. Caries management decision: influence of dentist and patient factors in the provision of dental services. J Dent 2009; 37: 827–834.
Chapko M K . A study of the intentional use of pit and fissure sealants over carious lesions. J Public Health Dent 1987; 47: 139–142.
Primosch R E, Barr E S . Sealant use and placement techniques among paediatric dentists. J Am Dent Assoc 2001; 132: 1442–1451.
Mjor I A . Placement and replacement of restorations. Oper Dent 1981; 6: 49–54.
Bonte E, Dupuis S, Bouter D, Lasfargues J J . Evaluation des restaurations coronaires posteérieures en pratique geéneéraliste. Rev Odont Stomat 2004; 33: 177–190.
Doméjean-Orliaguet S, Tubert-Jeannin S . Re-intervention in conservative dentistry. Sevilla: ConsEuro, 2009.
Pitts N, Harker R . Obvious decay experience. Children's dental health in the United Kingdom, 2003. London: Office for National Statistics, 2005.
Deery C . Caries detection and diagnosis, sealants and management of the possibly carious fissure. Br Dent J 2013; 214: 551–557.
Acknowledgements
The authors would like to thank Claudie Damour-Terrasson, publishing director of the Groupe Information Dentaire, Paris, France, for the authorisation of translation and publication of the series in the BDJ; Dr Avijit Banerjee for his support; Dr G. V. Moncada, Dr S. M. Gordan, Dr I. Mjör, Dr S. Leal and Dr M. Maltrait for kindly providing photographic material.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Holmgren, C., Gaucher, C., Decerle, N. et al. Minimal intervention dentistry II: part 3. Management of non-cavitated (initial) occlusal caries lesions – non-invasive approaches through remineralisation and therapeutic sealants. Br Dent J 216, 237–243 (2014). https://doi.org/10.1038/sj.bdj.2014.147
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2014.147
This article is cited by
-
Clinical practice guideline adaptation for risk-based caries management in 18–55 year-old Iranian adults
BMC Oral Health (2023)
-
Top tips for minimally invasive dentistry in primary care
British Dental Journal (2023)
-
Infiltration and sealing for managing non-cavitated proximal lesions: a systematic review and meta-analysis
BMC Oral Health (2021)
-
Quaternary ammonium compound as antimicrobial agent in resin-based sealants
Clinical Oral Investigations (2020)
-
Is preventing micro-cavities in dentine from progressing with a sealant successful?
British Dental Journal (2019)