Key Points
-
Highlights the need for general dental practitioners to improve the awareness of the importance of oral healthcare advice in patients with diabetes.
-
There is a need for education and training on the importance of oral healthcare for non-dental health professionals involved in diabetes care.
-
There is a potential need for the inclusion of dental care in diabetes care pathways.
Abstract
Objective To investigate oral health awareness, oral hygiene and attitudes towards general dental practitioners' (GDP) involvement in diabetes screening in adults with diabetes.
Design Self-completion questionnaire.
Setting General medical practices in Warwickshire.
Subjects and methods Adults with diabetes attending clinics run by practice or diabetes nurses in general medical practices.
Results Two hundred and twenty-nine of 615 (37.2%) questionnaires were completed in 14 general medical practices. The majority of respondents (79.8%, 178/223) visited a dentist once or twice a year, but oral care varied; 67.2% (133/198) reported brushing at least twice a day, whereas only 15.3% (29/190) flossed daily. Awareness of oral health risks was limited: 69.1% (150/217) had never received any oral health advice related to their diabetes. Over half of respondents supported the idea of dentists offering screening for diabetes (121/226, 53.5%).
Conclusions Many adults with diabetes have poor awareness of oral care and health complications associated with diabetes, and are receiving limited advice from healthcare professionals. Training and advice for both healthcare professionals and patients concerning the importance of good oral health in patients with diabetes is needed. The role of dentists in diabetes screening and support requires further investigation.
Similar content being viewed by others
Background
An estimated 2.6 million people in the UK have been diagnosed with diabetes, and a further 0.5 million are estimated to have undiagnosed diabetes.1 Around 90% of adults with diabetes have type 2 diabetes.1 Diabetes and its complications account for approximately 10% of annual NHS spending.2 Long-term poor glycaemic control in both type 1 and type 2 diabetes can lead to major complications including diabetic nephropathy, retinopathy, coronary heart disease and strokes.3 People with diabetes are also at higher risk of developing oral health problems4 and there appears to be a bidirectional relationship between levels of periodontal disease and glycaemic levels.5 Inflammatory responses produced by inflamed periodontal tissue can increase the severity of diabetes, worsen cardiovascular outcomes and increase mortality.6 However, a meta-analysis reported that treatment of periodontal disease by scaling/root planning and oral hygiene in people with diabetes resulted in a mean reduction in HbA1c levels of 0.4%.7 Despite growing evidence about the associations between oral health problems in patients with diabetes, there is limited research investigating oral health awareness in patients with diabetes.
Oral health problems and poor glycaemic control
In addition to periodontitis, persistent poor glycaemic control has been associated with increased incidence and progression of gingivitis and alveolar bone loss,8,9 salivary gland dysfunction,10,11 taste disturbances12 and orofacial neurosensory disorders (eg burning mouth syndrome).13 People with diabetes have also been shown to be at greater risk of developing certain oral mucosal disorders such as lichen planus, recurrent aphthous stomatitis and oral fungal infections.14 There is also evidence that people with diabetes have an increased risk of oral cancer and oral pre-malignancies.15
Effective oral self-care, such as correctly-conducted tooth brushing and flossing, along with regular dental checks, is critical in the prevention of oral disease. However, several studies,16,17,18 conducted worldwide, have shown that people with diabetes often lack important knowledge about the oral health complications of diabetes, and have poor levels of oral self-care.
Dental teams and diabetes care
Recent UK government policy has encouraged the expansion of the role of dental professionals to include wider general health promotion.19,20 The dentist is well placed to carry out risk assessment and screening for diabetes, including emphasising the importance of maintaining oral health, especially for people who have infrequent contact with other health professionals. However, patient acceptability of dentists' involvement in diabetes screening and care is unknown.
Study objectives
The study aimed to survey a community-based sample of adults with diabetes concerning: 1) oral health awareness; 2) oral hygiene practices; and 3) attitudes towards dentists' involvement in screening for diabetes.
Methods
A questionnaire study was carried out between January and June 2010. South Staffordshire Research Ethics Committee approved the study.
Setting
The study was carried out in clinics run by practice or diabetes nurses in general medical practices in Warwickshire. Warwickshire is a mixture of urban and rural communities. The population is ageing at a faster rate than the national average and health inequalities exist between the relatively deprived north and more affluent south of the county.21 The number of people diagnosed with diabetes is slightly lower than the national average (3.97% compared to 4.30%).21
GP practices were chosen because all patients with diabetes are likely to be registered with a GP, whereas only a minority attend specialist clinics. All 76 practices in Warwickshire, covering a broad sociodemographic population, were informed about the study by letter, of which 14 agreed to participate.
Questionnaire
A four-page self-completion questionnaire was developed following a scoping review of the literature and informal discussions and structured feedback with diabetes users attending the Warwick Diabetes Research and Education User Group. The following topics were covered in the questionnaire: a) current dental care and oral hygiene behaviour; b) awareness of oral health problems associated with diabetes; c) oral health advice received; and d) the role of dentists in diabetes care. Forty-eight questionnaires were piloted in one practice during a one month period (response rate 24/48, 50%). No changes were made to the questionnaire or the administration process following the pilot.
Eligibility and consent
Patients attending participating practices were eligible to participate in the study if they had any type of diabetes, were aged 18 years or over, were well enough to participate and able to consent. Up to 60 eligible patients attending a clinic with a designated nurse at their general medical practice were asked by the nurse if they would like to participate in the study. Those who agreed were given an envelope containing an information sheet, consent form and the oral health questionnaire. Patients had the opportunity to complete the questionnaire either immediately following the clinic or at home. Post boxes in practices and pre-paid envelopes were provided. Questionnaires were available in English only, however telephone interpretation was made available to all participants.
Results
A total of 615 adults with diabetes were given the oral health questionnaire; 229 completed forms were returned yielding a response rate of 37.2%. The mean number of questionnaires returned by each participating practice was 16.4 (SD 12.7). Respondents were typically older adults who stated that they were from a White British ethnic background. Eighty-seven percent (194/223) reported that they had type 2 diabetes, and the remainder had type 1 diabetes. Respondent characteristics are shown in Table 1.
Dental care and hygiene
Respondents' use of professional dental care and oral hygiene behaviours are shown in Table 2. Of dentate respondents, 86.8% (165/190) reported that they were currently registered with a dentist, compared with only 69% (20/29) of edentate respondents. The majority of respondents reported that they visit the dentist once (25.6%, 57/223) or twice (54.3%, 121/223) a year. Cost (43.9%, 76/173), lack of need (37.6%, 65/173) and finding visits to the dentist unpleasant (19.1%, 33/173) were the main reasons for not visiting a dentist more often.
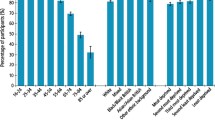
Just over two thirds of respondents (67.2%, 133/198) reported they brushed their teeth two or more times a day, whereas only 15.3% (29/190) reported that they flossed at least once a day. Dental and oral self-care tasks were rated as less important than other diabetes self-care tasks (Fig. 1) such as taking prescribed medication or having regular eye checks. Approximately one third of patients (35.4%, 73/206) rated daily flossing as the least important health-related activity.
Oral health awareness
Respondents were most aware of mouth dryness (43%, 92/214) and delayed healing in the mouth (23.9%, 51/213) being associated with diabetes, but awareness of all other complications, such as swollen or tender gums (13.1%, 28/213) and loose teeth (12.8%, 27/211) was much lower. The majority of respondents reported that they had never received advice on oral hygiene tasks in relation to diabetes from a health professional (69.1%, 150/217). The majority of respondents stated that their dentist should inform them about the importance of good oral health because they have diabetes (70.5%, 158/224). However, only 30.2% of respondents (68/225) stated that they had talked to their dentist about diabetes. Oral health awareness and advice received are shown in Table 3.
Dentists screening for diabetes
Over half of respondents (53.5%, 121/226) supported the idea of dentists' involvement in diabetes screening, although 23.5% (53/226) were uncertain about this. However, only 20.9% (45/215) of respondents reported they would be willing to pay for diabetes screening in a dental setting (see Table 4).
Discussion
Adults with diabetes were found to have poor awareness of oral care and limited awareness of the oral health complications associated with diabetes. Variability in daily brushing and flossing frequency was reported. Indeed, dental care activities were not rated as important self-care tasks in comparison to other diabetes self-management activities. These results confirm the findings of other studies16,17,18 showing a limited awareness of the importance of good oral health in patients with diabetes. Although the majority of respondents were registered with a dentist and attended one or more appointments per year, some were not receiving professional dental care, particularly edentulous patients.
Respondents demonstrated poor awareness of the oral health complications associated with diabetes. Highest awareness was of mouth dryness being associated with diabetes, although less than half were aware of this, which supports previous findings.18 Lack of awareness and poor oral self-care may be partly explained by the fact that over two thirds (69.1%) of respondents reported that they had never received any oral care advice from any health professional in relation to their diabetes, despite high levels of dental attendance. This suggests that general dental practitioners (GDPs) do not routinely discuss how diabetes can affect oral health and self-care prevention measures with patients. Likewise, patients do not appear to have been encouraged to discuss oral health issues associated with diabetes with their GDP, although the majority felt that dentists should be informing them about oral health risks.
The lack of oral health awareness in the current sample may also, in part, be due to limited education and training for non-dental health professionals involved in diabetes care. National guidance on oral health in diabetes education management is limited. The Diabetes National Service Framework22 states that the importance of oral hygiene and regular dental checks should be explained to patients, although training and resources for non-dental health professionals to support this are lacking.
The present findings should be interpreted with caution as respondents may have been biased towards adults with a greater interest in oral healthcare or those with poorer oral health histories; patients with more complex illnesses or with significant diabetes complications, if recruited from secondary care services, may have had different responses to the questionnaire. In addition, measures of ill-health in Warwickshire are generally better than the regional and England average21 so the sample may not be representative of those from other settings.
Despite the study's limitations, the current findings suggest that patients are receiving inadequate oral health advice from dental and non-dental health professionals involved in their care. It is important that patients receive relevant risk and oral self-care instruction so that oral health complications associated with diabetes are minimised. Further development and evaluation of educational resources for both patients and professionals is required, and inclusion of dental care in diabetes care pathways needs to be considered.
There was some support for dentists' involvement in screening. Further research should consider whether people with undiagnosed diabetes would consider paying for this service if dental teams were prepared and trained to provide screening.
Conclusions
Adults with diabetes are receiving limited advice about the oral health complications associated with diabetes, have poor awareness of oral health risks and their oral self-care may not be satisfactory in preventing oral disease. The role of dentists in diabetes screening and support requires further investigation. Consideration of training and advice for both healthcare professionals and patients concerning the importance of good oral health in patients with diabetes is needed.
References
Diabetes UK. Diabetes in the UK 2010: key statistics on diabetes. London: Diabetes UK, 2010.
Department of Health. Turning the corner: improving diabetes care. London: Department of Health, 2006.
Gadsby R . Epidemiology of diabetes. Adv Drug Deliv Rev 2002; 54: 1165–1172.
Tsai C, Hayes C, Taylor G W . Glycaemic control of type 2 diabetes and severe periodontal disease in the US adult population. Community Dent Oral Epidemiol 2002; 30: 182–192.
Taylor G W . Bidirectional interrelationships between diabetes and periodontal diseases: an epidemiologic perspective. Ann Periodontol 2001; 6: 99–112.
Skamagas M, Breen T L, LeRoith D . Update on diabetes mellitus: prevention, treatment, and association with oral diseases. Oral Dis 2008; 14: 105–114.
Simpson T C, Needleman I, Wild S H, Moles D R, Mills E J . Treatment of periodontal disease for glycaemic control in people with diabetes. Cochrane Database Syst Rev 2010; (5): CD004714.
Taylor G W, Burt B A, Becker M P, Genco R J, Shlossman M . Glycaemic control and alveolar bone loss progression in type 2 diabetes. Ann Periodontol 1998; 3: 30–39.
Grossi S G . Treatment of periodontal disease and control of diabetes: an assessment of the evidence and need for future research. Ann Periodontol 2001; 6: 138–145.
Chavez E M, Borrell L N, Taylor G W, Ship J A . A longitudinal analysis of salivary flow in control subjects and older adults with type 2 diabetes. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 91: 166–173.
Gilbert G H, Heft M W, Duncan R P . Mouth dryness as reported by older Floridians. Community Dent Oral Epidemiol 1993; 21: 390–397.
Settle R G . The chemical senses in diabetes mellitus. In Getchell T V, Doty R L, Bartoshuk L M, Snow J B Jr (eds) Smell and taste in health and disease. pp 829–844. New York: Raven Press, 1991.
Moore P A, Guggenheimer J, Orchard T . Burning mouth syndrome and peripheral neuropathy in patients with type 1 diabetes mellitus. J Diabetes Complicat 2007; 21: 397–402.
Guggenheimer J, Moore P A, Rossie K et al. Insulin-dependent diabetes mellitus and oral soft tissue pathologies: II. Prevalence and characteristics of Candida and Candidal lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 89: 570–576.
Auluck A . Diabetes mellitus: an emerging risk factor for oral cancer? J Can Dent Assoc 2007; 73: 501–503.
Allen E M, Ziada H M, O'Halloran D, Clerehugh V, Allen P F . Attitudes, awareness and oral health-related quality of life in patients with diabetes. J Oral Rehabil 2008; 35: 218–223.
Please M M . Patient knowledge of the link between diabetes and periodontal diseases. J Dent Hyg 2007; 81: 90.
Yuen H K, Wolf B J, Bandyopadhyay D, Magruder K M, Salinas C F, London S D . Oral health knowledge and behaviour among adults with diabetes. Diabetes Res Clin Pract 2009; 86: 239–246.
Department of Health. NHS dentistry: options for change. London: Department of Health, 2002.
Department of Health. Modernising NHS dentistry: implementing the plan. London: Department of Health, 2000.
Warwickshire Observatory. Health profile 2010. Warwick: Warwickshire Observatory, 2010.
Department of Health. National service framework for diabetes. London: Department of Health, 2001.
Acknowledgements
We gratefully acknowledge the input of the Warwick Diabetes Research and Education User Group in all aspects of the development and conduct of this study. The study was funded by NHS Warwickshire.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Bowyer, V., Sutcliffe, P., Ireland, R. et al. Oral health awareness in adult patients with diabetes: a questionnaire study. Br Dent J 211, E12 (2011). https://doi.org/10.1038/sj.bdj.2011.769
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2011.769
This article is cited by
-
A systematic review investigating patient knowledge and awareness on the association between oral health and their systemic condition
BMC Public Health (2021)
-
Oral health knowledge, attitudes and care practices of people with diabetes: a systematic review
BMC Public Health (2018)
-
The Impact of Oral Health on General Health: Educating Professionals and Patients
Current Oral Health Reports (2017)
-
Type 2 diabetes risk screening in dental practice settings: a pilot study
British Dental Journal (2014)
-
Summary of: Patients' attitudes towards screening for diabetes and other medical conditions in the dental setting
British Dental Journal (2014)