Key Points
-
The patient's expectations of crown and bridgework must be assessed, particularly when cosmetic treatment is planned.
-
Appropriate care needs to be taken with tooth preparation.
-
Patients should be warned regarding risk of loss of vitality with fixed restorations.
-
Occlusal problems are common precipitators of complaints, particularly when reduction of opposing teeth is carried out without consent.
Abstract
Provision of indirect restorations is associated with more complaints and litigation than any other area of dentistry. In the third part of this series we identify possible causes of such complaints. We explore each of the stages from clinical assessment to treatment, highlighting areas which may trigger litigation when they are not addressed carefully – particularly in relation to cosmetic dentistry. The article is illustrated with clinical examples drawn from the authors' personal experience. With patients' ever-increasing expectations, the pressure to deliver quality dentistry has never been higher and will not diminish.
Similar content being viewed by others
Introduction
Crown and bridgework is responsible for the greatest proportion of negligence claims against dentists, accounting for the largest element of all damages and legal costs. Understandably, the professional indemnity agencies issuing this information are reluctant to publish detailed comparative figures for commercial reasons. However, the Dental Complaints Service (DCS) of the General Dental Council (GDC), which deals with complains about private dentistry, confirms that the largest proportion (23%) of 1,559 complaints received in their first year was related to crown and bridge treatment, and this continued to rise in subsequent years.1
These figures may reflect the progressive increase in the number of teeth restored with indirect restorations, as more and more patients retain their teeth into later life.2 However, such teeth are often heavily restored and failing and may not always provide a reliable foundation for high quality restorations. More importantly, there is a clear trend for more and more dentists to become increasingly involved in the practice of cosmetic dentistry, tempted by the potential profit and an increasing demand from patients to carry out cosmetic procedures. Clinicians who claim to have special expertise in aesthetic/cosmetic dentistry risk exposing themselves to litigation when their treatments fail to deliver what was promised or meet patients' expectations which may not always be realistic. The pressures on practising dentists have never been higher, and will not diminish.
The aim of this article is to identify possible causes of complaints and litigation in relation to the provision of crowns and other extra-coronal restorations, which were the subject of a previous BDJ series.3 The article will also make reference to bridgework but excludes implant-supported and retained restorations. Specific examples of problems leading to litigation have been drawn from personal involvement of the authors.
What can lead to an allegation of negligence?
It is reassuring to know that the majority of medical patients do not complain or sue should something go wrong. The 'Harvard Study'4,5 showed that while up to 4% of patients attending hospitals in the United States experienced an adverse outcome, of which roughly a quarter were the result of negligence, only a relatively small fraction of these patients sued (1 in 8).
The prospect of litigation is increased when a combination of precipitating and predisposing factors exists.6 These factors have an aggravating effect in dentistry, especially when the predisposing factors, which largely reflect the clinician's attitude, leave patients feeling abused or ignored. In relation to the provision of crown and bridgework, the main factors precipitating complaints and allegations of negligence can be summed up as follows:
-
Pain
-
Early failure and need for remedial treatment
-
Perceived aesthetic deficits (eg unexpected display of metal)
-
Overprescribing/over-treatment (eg patients feeling that they have been talked into treatment that they did not need, or which was of little benefit to them)
-
Under-treatment/supervised neglect (before criticising a previous dentist's work and precipitating litigation, the new dentist needs to bear in mind that he or she may not have the full background behind the situation)
-
Escalating or unexpected cost (patients have a right to know in advance how much their dental treatment is likely to cost with an explanation of potential situations which may necessitate costs to be revised).
How to avoid litigation
An allegation of negligence in relation to crown and bridge treatment may result from any stage of the management of the patient and may not necessarily relate to the technical quality of the final restoration. Proceeding too hastily with poor communication, insufficient clinical data from clinical examination and appropriate investigations, improper treatment planning or poorly executed tooth preparation can be very difficult to defend when treatment proves to be unsuccessful. This can be seen in Case 1.
Case 1
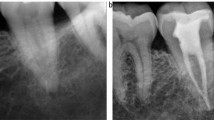
Two years previously Mr A had received an extensive course of crown and bridgework, which caused immediate problems with pain, infection and failure of restorations (decementation). These problems had not been resolved despite him returning to the providing dentist on several occasions. Out of frustration, the patient eventually visited another practitioner who immediately referred him for a specialist opinion. He presented with soreness and a discharging sinus related to 22 and two loose bridge retainers. Clinical and radiographic examination (Fig. 1) showed the following deficiencies in treatment:
-
Perforated post preparation 22
-
Decemented bridge retainers 13 and 27 (conventionally cemented gold inlay)
-
Caries 16, 15, 14, 35, 47
-
Defective margins on newly placed inlays (17, 15, 27, 35, 45) and crowns (13, 11, 21, 22, 25)
-
Defective root canal treatments 13, 21, 22, 25, 45.
There was no justification for the poor standard of work or for failing to rectify the resulting problems, which were significant. Normally, clinical problems are identified for patients without criticising the dentist involved. However, the problems here were unusually extensive and at the very least indicative of a dereliction of the dentist's duty of care.
The patient was keen to pursue redress, but it was advised that it was too late to do so through the NHS system. The patient was advised that the only course for redress would be legal action. An out of court settlement was eventually made for an amount which covered a consideration for the resulting inconvenience, pain and suffering, and the cost of private treatment to replace the deficient work.
In this article each of the stages of clinical assessment and treatment will be considered, highlighting areas which may trigger litigation when they are not addressed carefully. Further advice on good practice can be found in the 'Guidelines for crown and bridge' published by the British Society of Restorative Dentistry (BSRD) (http://www.bsrd.org.uk) and in the reports and risk assessment modules published by some dental indemnity agencies.
Most courses of dental treatment start with a medical and dental history, an examination and any relevant investigations. A diagnosis and provisional treatment plan is then formulated and discussed with the patient, treatment options are explained and considered as part of the consent process, and only then should treatment proceed. As noted in part two of this series,7 in giving consent the patient needs to be aware that it may not always be possible to make a definitive treatment plan until the response to an initial phase of care is known. Clinical wisdom suggests that, when planning care, consideration should be given to the patient as a whole initially, then the mouth and finally the tooth.
Patient assessment
Assessment of patient attitude to, and expectation of, the proposed dental treatment is crucial, not least when veneers or crowns are being considered for purely cosmetic reasons. The patient must be given full information and made aware of the treatment options available and the prognosis and limitations of what can be achieved. A common dento-legal scenario is where a patient claims an inadequate understanding of the proposed treatment and that, had it been fully understood, he or she would not have agreed to the treatment in the first place, especially when sound teeth are damaged in the pursuit of a cosmetic ideal. Where the practitioner feels that expectations cannot be met or modified, it is better to decline to provide treatment or to make an appropriate referral, rather than risk later retribution. It has often been said that in such situations, one should 'only treat a friend'. In other words, one should take time to know one's patient in order to understand fully their motivation and expectation for requesting a particular treatment, ensuring that they understand what it is possible to achieve in any given clinical situation and the long-term sequelae of the restorations.
When extensive crowns or bridgework are planned, it is important to draw the patient's attention to the number, length and frequency of appointments to complete treatment, along with the need for interim temporary restorations. The practitioner should resist the temptation to cut corners in order to fulfil a patient's wish to have work completed in time for a wedding photograph or before going away on holiday.
Assessment of the mouth
The mouth should be thoroughly assessed for active disease resulting from poor oral hygiene or diet. Where problems are found, inform the patient about them but avoid judgemental comments on other colleagues' work, which may precipitate unjustified claims of supervised neglect. A properly conceived treatment plan would be expected to start with the arrest of active disease, improvement of oral hygiene and thorough dietary analysis and counselling. This should be followed by a period of maintenance and monitoring to assess patient compliance before considering whether fixed restorations are desirable, necessary or even appropriate. Embarking upon irreversible treatment too soon can be a recipe for premature failure of any crown and bridgework.
Information obtained from the dental history about caries susceptibility, periodontal risk, temporomandibular joint or muscle pain or parafunctional habits, or history of repeated fracture of teeth or restorations will warrant the need for further investigation. Detailed examination should be carried out and recorded contemporaneously in the patient's notes, including charting of teeth present, extent and condition of restorations, attachment loss, tooth mobility, occlusal assessment, pulp tests and appropriate radiographic examinations. It is often sensible to supplement examination by recording study models, preferably mounted and with clinical photographs. This will be of great assistance should a dentist's decisions be challenged, such as by the familiar allegation of crowning sound teeth unnecessarily.
Where bridgework is being considered, the form, contour and dimensions of the edentulous ridge needs to be assessed in relation to prescribing an appropriate design of pontic. Teeth receiving indirect restorations or acting as bridge abutments should be thoroughly assessed for the following:
-
Tooth morphology and anatomy
-
The quantity and location of residual tooth tissue (note that this can often only be done by removing existing restorations and replacing them before planned tooth preparation)
-
The state of existing restorations including cores
-
Periodontal status and bone support
-
Pulpal and periradicular status
-
In the event that the tooth is non-vital, the quality of the endodontic care
-
Static and functional occlusal relationships
-
Cosmetic requirements
-
The prognosis of the tooth following restoration.
Remember during the assessment that inadequate retention and resistance form of a preparation may directly or indirectly lead to early failure. As well as being able to detect and manage teeth with short crown height, dentists should be confident of their ability to prepare teeth and that the teeth chosen for preparation are fit for purpose. Dentists also need to design the tooth preparation to be suitable for the proposed restoration. Sufficient tooth reduction is needed for structural durability of the restoration, periodontal and aesthetic reasons, but not so much that the pulp or strength of the tooth is compromised.8 In this respect, it is worth considering the usage of preparation matrices to gauge the appropriate amount of tooth reduction, especially when the shape of tooth is to be changed by the restoration. If part of the plan for care does involve altering the orientation of the crown of a tooth, a careful assessment needs to be made as to whether or not there is a risk of pulpal exposure and hence whether elective endodontics would be a sensible option.
In the following sections, we consider in more detail the periodontal, endodontic, occlusal and aesthetic factors important in ensuring success and avoiding litigation.
Periodontal status
This pre-operative assessment must include whether the periodontal disease is progressing or whether treatment of it has produced a stable state. As part of the patient's periodontal treatment, overhangs on any restoration should be removed to allow access for cleaning. Crowns with defective margins are best removed, followed by the provision of well-fitting and properly contoured provisional restorations to allow the health of the gingival margin to improve and its position to stabilise before the impressions are taken for the definitive restorations. Following periodontal or apical surgery and surgical crown lengthening procedures, the tissues will also need time to stabilise.9 This may take up to six months,10 before adjusting the preparation margins and taking the final impressions. If the final impression is rushed without allowing appropriate stabilisation of the gingival tissue, further recession may occur. The resultant exposed root and crown margins may be unacceptable to the patient, especially where this occurs in the aesthetic zone of the anterior part of the mouth.
Periodontal health is often compromised by defective indirect restorations, which may prompt patients to take legal action against the dentist who fitted them. Ill-fitting margins and poor emergence profiles can result in gingival problems, as can restriction of embrasure spaces and reducing access for cleaning by the presence of incorrectly contoured bridge pontics and connectors. A common problem is when insufficient tooth tissue is removed at the preparation stage (Fig. 2), resulting in the technician over-contouring the definitive restoration to achieve an adequate thickness of ceramic for aesthetics.
Ideally, all crown margins should be placed supragingivally to facilitate monitoring and maintenance, however margin position is influenced to a large extent by the patient's aesthetic demands. When a subgingival margin is indicated, this should be thought of and planned for. In particular, it should be placed within the limits of the gingival sulcus, rather than encroaching upon the biological width leading to unsightly gingival recession or inflammation. Furthermore, the placement of finishing lines subgingivally may result in damage to the gingival tissue by the bur and can make accurate impression recording difficult. A useful rule of thumb is not to extend subgingivally more than half the depth of the sulcus.8
Poorly contoured restorations or residual luting cement left around temporary or definitive restorations may also result in gingival inflammation.11 Such lack of attention to detail reflects badly on the dentist and causes patient distress through the resulting pain, swelling and bleeding or in other cases recession and margin exposure.
Pulpal and periapical status
It is important to recognise that crowns should rarely be made for intact teeth; rather they are made to protect and restore teeth that have been damaged by wear, trauma, or cycles of caries and repair. Therefore at the planning stage, all teeth presumed either to have healthy pulps or that have previously been root-treated should be assessed thoroughly by recording vitality tests and periapical radiographs respectively. Unfortunately, despite taking the usual precautions during tooth preparation and temporisation, abutment teeth may still become non-vital after the definitive crown or bridge has been cemented.12,13 Frustrating as that might seem to the patient and embarrassing to the dentist, there is no reliable way of predicting which teeth are going lose vitality after cementing the final restoration, unless of course the tooth has been overheated by inadequately cooled rotary instruments. This caveat applies as much to veneer as to crown preparations where we have observed that minimal involvement of dentine has not immunised against pulp necrosis in multiple teeth.
To describe why the pulp dies unexpectedly, researchers have coined the term 'the stressed pulp';14 after a lifetime of cumulative insults, crown preparation is viewed as the last straw. In this respect pulp capped teeth are likely to be at greater risk and it is prudent to root treat before fitting indirect restorations.
Clearly, removal of the old restoration will help the operator decide whether a previous exposure exists. However, subtle radiographic changes (eg canal sclerosis or focal sclerosis in the periapical bone) may precipitate the decision to root treat before crowning. Given the difficulty and the challenging task of accessing pulp chambers through cemented crowns, elective root canal treatment should also be considered for teeth whose pulps are at risk of exposure during crown preparation (for example, where re-orientation of the crown is planned). In addition, root canal treatment may be indicated for vital teeth that cannot be restored without using the pulp chamber and root canals for retention and support.15
Even in the absence of symptoms, inadequately root-treated teeth, short or poorly condensed root fillings, or teeth with persistent periradicular pathology do not provide a predictable foundation for crown and bridgework until the root canal treatment is revised. Repeat root canal treatment is also indicated where the root filling has been exposed to the mouth either through leaking restoration margins or loss of coronal restorations for more than three months.15 Teeth with post-retained crowns are particularly vulnerable in this respect. It is worth informing patients that repeat of root canal treatment does not carry as high success rate as for teeth root filled for the first time,16 which may guide a decision to consider other treatment options, eg extraction and implant placement.
From a dento-legal perspective and according to the dental indemnity bodies, root treated teeth and especially those restored with posts feature regularly in their annals of failed crown and bridgework that are subject to litigation.17 The main areas of risk that the clinician should be aware of when using post crowns either as single units or as bridge abutments are:
-
Angulation of the post (leading to perforations)
-
Length (if too short leading to loss of retention and decementation or if too long it can disturb the apical seal)
-
Strength (risk of post fracture)
-
Design (shape and profile) and associated risks of either root or post fracture
-
Data would suggest that post-retained crowns have the poorest performance as bridge abutments.18
Occlusion
Failure to identify problematic occlusal interferences or introducing excursive contacts that are not in harmony with anterior guidance and jaw movement can cause significant problems during provision of crown and bridgework, including:
-
1
Decementation and fracture of crowns
-
2
Increased tooth mobility
-
3
Tooth migration (eg splaying of crowned or veneered anterior teeth with bulky guidance surfaces)
-
4
Dental pain
-
5
Temporomandibular disorders (TMD).
A common occlusal problem with anterior restorations is the incorporation of incorrect anterior guidance. Patients may complain of discomfort from the crowned or veneered teeth, which may also show fremitus – a characteristic vibration which can be felt by the dentist's finger when the teeth are brought into occlusion. In the longer term, the teeth may drift labially resulting in the appearance of unsightly gaps. If patients grind on the interfering restorations, they are at risk of fracturing the restoration or excessive wear to the opposing teeth. Correct management of anterior guidance is therefore particularly important but often overlooked in planning anterior cosmetic dentistry.
When extensive crown and bridgework is undertaken, the risk of precipitating such problems is increased, especially if the operator loses control of the occlusion as in Case 2, below. Being able to recognise potentially difficult or troublesome cases before starting treatment is a useful skill to develop. In this way, dentists can either plan to avoid problems or refer the patient to someone who has appropriate expertise.
The three main problem areas are:
-
1
Management of wear and parafunction
-
2
TMD and occlusion
-
3
'Phantom bite'.
Case 2
Mr B attended as an emergency referral on a specialist diagnostic clinic. He was extremely distressed by the pain and mobility of the bridge replacing 24, which had been fitted by his dentist only a week previously. This fixed-fixed conventional bridge had ceramo-metal crowns at 23 and 25. The 23 was grade III mobile. He explained that this bridge was the second one fitted by his dentist in the past month. The first one gave similar problems, which the dentist had tried to rectify by removing it and replacing it for a period with an acrylic provisional bridge. Unfortunately this did not resolve the pain, mobility and parafunction, which were centred on tooth 23.
Examination showed a similar bridge had been fitted replacing 14 and ceramo-metal crowns on all his upper incisors. There was no periodontal or periapical disease to explain the mobility at 23, but occlusal examination showed the guidance surface on the crown to be convex (Fig. 3a). As guidance surfaces are usually concave this suggested a possible interference in lateral excursion (at this stage the effect of the occlusal contact on harmonious jaw movement could not be judged simply by using articulator paper as the abutment was so mobile). Furthermore, there was a large deflective contact at 15. Nevertheless, the appearance and fit of the crown and bridgework was good.
Diagnosis was made of parafunctional activity apparently exacerbated by the changes in occlusion associated with the new crown and bridgework. An occlusal stabilisation splint was provided which required adjustment over eight visits before achieving a stable pattern of occlusal contact (Fig. 3b). The deflective contacts were then removed from both bridges and a provisional bridge made to provide a concave guidance surface at 23 (Fig. 3c). Further occlusal adjustments were required over another five appointments before replacing the definitive bridge. Management was complicated by the degree of psychological upset and by the patient's neuromuscular system having become exquisitely sensitive to any occlusal changes.
This case illustrates the significant disruption that can occur when occlusal changes are coupled with parafunctional activity. Mr B started legal proceedings against his dentist for negligence. After several months of anxiety, the case was dropped as the judge ruled that the dentist had taken reasonable measures to try and resolve matters. However, this was a near miss and better occlusal management, avoiding the incorporation of occlusal discrepancies in the new restorations, would almost certainly have prevented the problem.
Management of wear and parafunction
Dentists need to be vigilant when dealing with the worn dentition as the destructive factors (parafunction or erosion or both) may still be active after the restorations have been fitted, resulting in catastrophic failure. Sometimes damage due to nocturnal parafunctional activity occurs in surprisingly eccentric excursions but the 'sawn-off' appearance of the anterior teeth may provide a clue (Fig. 4).
His history of active nocturnal parafunction indicated restorations would potentially be subject to the same or greater forces during marked protrusive excursion (there was a 7 mm overjet). As there was no sensitivity, we recommended that his dentist simply smooth rough edges, provide a splint for night wear and casts for baseline records. The patient understands the associated risks if restorations are eventually prescribed
The combination of heavy occlusal forces and short clinical crown height are particularly challenging, requiring strategies to improve restoration retention (eg choice of material, crown lengthening and adhesive cementation) and prevent wear (prophylactic occlusal splint). Patients with active bulimia often have problems with caries under crowns and loss of cementation if restored prematurely. Such disappointment can be avoided by using interim restorations of adhesively retained composite until the eating disorder is under control.
TMD and occlusion
Another cause for concern is the risk of dental treatment precipitating TMD. Some patients appear to have a greater predisposition to TMD than others so before providing crown and bridgework, patients should be screened for underlying muscle tenderness, limitation of opening and temporomandibular joint problems including pain, clicking or crepitus. The findings, even if negative, should of course be recorded. By recording positive findings dentists can avoid the accusation that restorative treatment 'caused' a patient's TMD, however they would be expected to have explained to patients beforehand that their symptoms may be aggravated by treatment – at least in the short-term. By recording negative findings dentists will have demonstrated that they performed their duty of care by examining the masticatory system before embarking on treatment.
Sometimes legal proceedings can result from patients being encouraged to believe that their TMD can be managed solely through occlusal adjustments or rehabilitation. Current evidence supports the use of reversible conservative management for TMD such that dentists embarking on irreversible treatment as the first line of approach are at risk of litigation by patients whose conditions worsen or remain unchanged. It is best to treat active TMD conservatively and then, should occlusal adjustments and rehabilitation be required, to justify these on their own merits (eg removal of a deflective contact on a tooth to be crowned for functional or restorative reasons). The diagnosis and management of TMD is discussed in a future chapter.
Phantom bite
This unusual condition can cause dentists real problems and normally starts after dental work involving occlusal surfaces.19 Patients have the following characteristics:
-
1
Utterly preoccupied with the way their teeth meet
-
2
Symptoms described in an often exaggerated and bizarre way, sometimes with written and drawn explanations
-
3
Symptoms may not match with dentist's examination findings.
Subsequent replacement of restorations and occlusal adjustments are ineffective and may worsen the condition, with an increasingly dissatisfied patient moving from one dentist to another in search of a physical cure. It is a poorly understood disorder of perception and notoriously difficult to treat effectively. Patients are best referred for specialist dental and, where available and where acceptable to the patient, psychological management.
Pre-operative records
Generally, there is less risk of causing occlusal problems if the existing intercuspal position (ICP) and anterior guidance can be maintained. When restoring to ICP hand-held casts may usefully supplement the occlusal examination to identify guiding and holding contacts.
However, with treatments that are more ambitious it may be necessary to consider reorganising the patient's occlusion around centric relation (CR), which requires greater knowledge and skill. When reorganising the occlusion it is wise to record two sets of casts. One set is kept as baseline evidence of the pre-treatment condition while the other is articulated on an average value or semi-adjustable articulator using a CR jaw registration and facebow. This second set is used for diagnostic adjustments and waxing to create a blueprint to guide treatment and which can be shown to the patient during consultation – an approach which can be very useful for planning aesthetic changes.
Aesthetics
The increase in demand for aesthetic/cosmetic dentistry by many patients is easy to understand, encouraged by the looks portrayed by celebrities, glossy magazines and television makeover programmes. Many patients believe their teeth affect their self-image, self-confidence, physical attractiveness and employability. Some patients will even request veneers, crowns or bridges solely on aesthetic grounds without understanding fully the irreversible and possibly damaging consequences of the treatment. Coupled with this rise in patient demand is the trend for more and more dentists to venture into the practice of aesthetic/cosmetic dentistry, tempted by the prospect of charging significant fees or goaded by the feeling that they are falling behind their competitors. Inevitably, there will be an increased risk of litigation when dentists embark on such treatments with little in the way of appropriate clinical training or without undertaking the appropriate steps in examining, assessing and understanding the patient's concerns, demands, hopes and expectations. Moreover, these cases may be more difficult than might appear at first sight and benefit from a multidisciplinary approach, for example initial orthodontic treatment to redistribute space and upright inclined/rotated teeth.
Particular care needs to be taken when the clinician is the one recommending the treatment and consideration must be given to the balance between aesthetics and the biological cost of tooth tissue loss when irreversible and extensive treatment is planned, especially if virgin teeth are to be prepared, as can be seen in Case 3, below.
The aesthetics of indirect restorations rely on many different components and dissatisfaction can result from deficiencies in any of them, either in isolation or in combination. These aspects and methods of testing various aesthetic schemes before tooth preparation (eg diagnostic waxing and provisional restorations) are considered elsewhere.20 However, two aesthetic issues that often lead to litigation are:
-
1
Lack of patient agreement and consultation in relation to shade selection and the proposed changes to teeth shape and appearance
-
2
Areas of visible metal either on the occlusal or lingual/palatal surfaces of fixed restorations, either through lack of communication between dentist and patient or between dentist and technician. Metal occlusal surfaces and 'metal islands' (Fig. 5) may distress patients if they do not understand their rationale, particularly if they arise inadvertently through adjustment of occlusal porcelain.
The principle that the dentist has an ethical obligation to act in the patient's best interest and to do no harm is of paramount importance with aesthetic procedures. If dentist and patient cannot agree on the best treatment modality, it is best for all concerned not to proceed. Experience shows that patients often become highly litigious when they feel dentists have abused their trust. A further pitfall occurs if the patient is not willing to accept the final restoration, resulting in disputes between dentist and technician over who is responsible for the cost of remake.
Case 3
Miss G was 16 when she attended a new dentist, expressing herself dissatisfied with the appearance of her front teeth. The main issue appeared to be the prominence of her 11 and 21 and associated spacing. Orthodontic correction for this problem had been attempted between the ages of 13 and 15, but her compliance had been poor. She was not prepared to undergo further lengthy orthodontics and wanted the teeth to be crowned. Two previous practitioners had refused to provide her with the treatment she requested.
Her new dentist was willing to comply with her request, offering crowns as the only treatment and not discussing previous treatment or the refusal of others to provide the treatment. The dentist promised her a lifespan of 15-20 years from the restorations. Following preparation of the two incisors in an attempt to reduce their buccal prominence, the dentist's records indicated exposure of both pulps. However, the patient denied being advised of this as a possible consequence of the treatment or having been told that it had actually occurred during the procedure. The temporary crowns were both lost over the ten days following tooth preparation and the patient experienced increasing pain and sensitivity. Symptoms resolved immediately after the cementation of the all-porcelain crowns, but four to five months later she noted that 'gaps appeared at the top of the crowns' and she was aware of 'increasing thermal sensitivity'.
Miss G reported that she was unhappy with the aesthetics of the crowns insofar as although the teeth were less prominent, they were not aligned with the adjacent teeth and 'perfect' as she had hoped. She was also unhappy with the shade and surface finish. Thereafter, an abscess developed on 11 leading to swelling in the right infraorbital region.
The patient changed her dentist and discovered, unsurprisingly, that both teeth were non-vital. Her new dentist prescribed several courses of antibiotics to treat her abscesses but she resisted having definitive root canal treatment on the advice of her solicitor. After three years service, the crown on tooth 11 fractured while on holiday with the palatal aspect of tooth 21 fracturing shortly after.
As a result, the patient had a catalogue of complaints amounting to a claim of negligence, including poor treatment planning, loss of vitality, poor appearance and function and failure of the provided restorations. Careful examination, thorough communication and a willingness to express a professional opinion regarding the appropriateness of the patient's request would have saved the practitioner the significant upset of a protracted case. Litigation found ultimately in favour of the claimant, who required extensive reparative work which eventually still provided only a partial improvement to her aesthetic concerns.
Problems encountered on fitting definitive restorations
In addition to unacceptable aesthetics, the other two most common problems encountered when fitting fixed restorations are related either to the marginal fit or to the occlusion.
Assessment of the marginal fit
The fit of restorations needs to be assessed carefully around the entire margin. Understandably, patients object to being able to see a defective margin or feel it with their tongue, floss or fingernail after the restorations have been cemented. Maintaining a high clinical standard has long-term advantages: defective margins may render teeth more susceptible to cement dissolution, recurrent caries, plaque retention and compromise gingival health. Best practice dictates that restorations with open margins or negative ledges be remade to avoid litigation, while over-extended margins and positive ledges can be adjusted at the chairside to allow complete seating of restorations and smooth passage of the probe. Clinicians should critically assess the causes of poor marginal fit. These may be associated with poor tooth preparation, resulting in lipped finishing lines where the resulting die fractures easily, or an inadequate impression technique.21 Alternatively, there may be laboratory-based problems such as poor die trimming, handling and identification of finishing margins. However, incomplete restoration seating and poor marginal adaptation may also result after cementation due to a lack of lute cement spacer on the die. Alternatively, using too much or too viscous a cement or not applying sufficient force for long enough may be other reasons.
Assessment of the occlusion
Once the restorations are fully seated, occlusal assessment should be carried out using shim stock and articulating paper. It is best to check which teeth are in contact both in the intercuspal position and in excursions with the restorations removed. In this way premature contacts and interferences can more easily be identified and then eliminated. Failure to do so can lead to the crowned tooth being overloaded, which in turn can lead to pain, mobility, fracture or decementation. Minor adjustment to restorations is a common occurrence; however patients are usually wary of extensive occlusal adjustments and reluctant to accept an unplanned adjustment of the opposing teeth to accommodate the occlusion of a new crown or bridge at the time of fitting, which they regard as an attempt by the dentist to fit a poor quality restoration. Another cause of patient dissatisfaction and possible litigation is when occlusal adjustment of a crown leads either to perforation or exposure of the underlying metal or unsightly core porcelain.
Prevention and maintenance issues
Whenever fitting fixed restorations, dentists should advise their patients of the importance of maintaining a high standard of plaque control and its beneficial effect on oral health and restoration longevity. The most appropriate cleaning techniques should be demonstrated, bearing in mind differences in patients' manual dexterity. In particular, patients need to be shown how to clean under bridge pontics and connectors. A patient's response to instruction should be monitored at each follow-up appointment.
Caries risk is directly related to both plaque and diet. Clinicians need to be vigilant for cariogenic changes in a patient's diet resulting in caries in those parts of the mouth where plaque might be retained. An especially damaging situation is where a bridge retainer becomes decemented but is held in place by the other bridge retainer(s). The inevitable plaque retention is often followed by rapid and unseen carious destruction beneath the decemented retainer. The dentist has at his or her disposal a full armamentarium of approaches to reduce the development of caries around restorations, including hygiene, dietary advice and the appropriate use of fluoride and varnishes. It is worth recording such advice and activity in the patient's notes to counter claims of supervised neglect.
Conclusion
The provision of indirect restorations is associated with more complaints and litigation than other areas of dentistry. Dentists therefore need to be aware of potential pitfalls, how to avoid them and how to react when things go wrong. The trend to an increased provision of cosmetic dentistry brings with it new risks from heightened and sometimes unrealistic patient expectations, as some dentists who have ventured into this area are beginning to discover.
References
Smith H. Dental complaints service – update. GDC Gazette 2007; Summer: 8–9.
Steele J G, Wassell R W, Walls A W G . Changing patterns and the need for quality restoration. Br Dent J 2002; 192: 144–148.
Wassell R W, Steele J G, Walls A W G . Crowns and other extra-coronal restorations: introduction. Br Dent J 2002; 192: 143.
Brennan T A, Leape L L, Laird N M, Herbert L E, Localio A R, Lawthers A . Incidence of adverse events and negligence in hospitalized patients: results of the Harvard Medical Practice Study I. N Engl J Med 1991; 324: 370–376.
Localio A R, Lawthers A G, Brennan T A, Laird N M, Herbert L E, Peterson L M . Relationship between malpractice claims and adverse events due to negligence in hospitalized patients: results of the Harvard Medical Practice Study III. N Engl J Med 1991; 325: 245–251.
Bunting R F J, Benton J, Morgan W D . Practical risk management; principles for physicians. J Healthc Risk Manag 1998; 18: 29–53.
D'Cruz L. Risk management in clinical practice. Part 2. Getting to 'yes' – the matter of consent. Br Dent J 2010; 209: 69–72.
Blair F M, Wassell R W, Steele J G . Crowns and other extra-coronal restorations: preparations for full veneer crowns. Br Dent J 2002; 192: 561–571.
Brägger U, Lauchenauer D, Lang N . Surgical lengthening of the clinical crown. J Clin Periodontol 1992; 19: 58–63.
Wise M D. Stability of gingival crest after surgery and before anterior crown lengthening. Br Dent J 1985; 53: 20–23.
Wassell R W, George G S, Ingledew R P, Steele J G . Crowns and other extra-coronal restorations: provisional restorations. Br Dent J 2002; 192: 619–630.
Valderhaug J, Jokstad A, Ambjornsen E, Norheim P W . Assessment of the periapical and clinical status of crowned teeth over 25 years. J Dent 1997; 25: 97–105.
Saunders W P, Saunders E M . Prevalence of periradicular periodontitis associated with crowned teeth in an adult Scottish subpopulation. Br Dent J 1998; 185: 137–140.
Abou-Rass M. The stressed pulp condition: an endondontic-restorative diagnostic concept. J Prosthet Dent 1982; 48: 264–267.
Whitworth J M, Walls A W G, Wassell R W . Crowns and extra-coronal restorations: endodontic consideration: the pulp, the root-treated tooth and the crown. Br Dent J 2002; 192: 315–327.
Friedman S. Treatment outcome and prognosis of endodontic therapy. In Ørstavik D, Pitt Ford T R (eds) Essential endodontology: prevention and treatment of apical periodontitis. Oxford: Blackwell Science, 1998.
Dental Protection Ltd. It's in the post. Riskwise UK 2003; 25: 1.
De Backer H, Van Maele G, Decock V, Van den Berghel . Long-term survival of complete crowns, fixed dental prostheses, and cantilever fixed dental prostheses with posts and cores on root canal-treated teeth. Int J Prosthodont 2007; 20: 229–234.
Jagger R G, Korszun A . Phantom bite revisited. Br Dent J 2004; 197: 241–244.
Nohl F S A, Steele J G, Wassell R W . Crowns and other extra-coronal restorations: aesthetic control. Br Dent J 2002; 192: 443–450.
Wassell R W, Barker D, Walls A W G . Crowns and other extra-coronal restorations: impression materials and technique. Br Dent J 2002; 192: 679–690.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Maglad, A., Wassell, R., Barclay, S. et al. Risk management in clinical practice. Part 3. Crowns and bridges. Br Dent J 209, 115–122 (2010). https://doi.org/10.1038/sj.bdj.2010.675
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2010.675
This article is cited by
-
Minimally invasive direct restorations: a practical guide
British Dental Journal (2017)