Key Points
-
The dental team is a key part of the multidisciplinary care team for older adults.
-
Support with preventive and prosthodontic care can be critical following a stroke.
-
People with Parkinson's disease experience a number of oral health problems.
-
The progression of dementia varies enormously, as does the ability to cope with dental treatment.
-
The dental team may have a role in identifying elder abuse.
Abstract
This article looks at three common neurological conditions associated with later years: stroke, Parkinson's disease and dementia. All of them impact on oral health, access to dental services and delivery of dental care, and treatment goals need to be adapted to take into account patients' changing needs, medical status, pattern of recovery or the stage of dementia that they have reached. The article concludes by considering the topic of elder abuse. The dental team may have a role both in identifying abuse and ensuring appropriate action is taken.
Similar content being viewed by others
Main
This article looks at three common neurological conditions associated with later years. The first, stroke, is an event with varying outcomes from death, through degrees of disability to full recovery. The other two conditions, Parkinson's disease and dementia are progressive conditions which usually, although not always, commence in later years, and over a number of years cause increasing disability and frailty. All of them impact on oral health, access to dental services and delivery of dental care. The article ends by considering the topic of elder abuse, as the groups of vulnerable older people described in the article fall into the 'at risk' category. The dental team may have a role both in identifying abuse and ensuring appropriate action is taken.boxed-text
1. Stroke
Stroke is a generic term for cerebrovascular accident (CVA) resulting in a sudden or rapidly progressing neurological defect causing various impairments in areas such as motor function, speech and cognition, which do not resolve within 24 hours.1,2,3 Most strokes are ischaemic in nature due to cerebral thrombosis or embolism and some are the result of intra-cerebral, sub-dural or extra-dural haemorrhage.2,3,4
Stroke is the third highest cause of death in the UK, after ischaemic heart disease and all cancer types combined.1 Around 150,000 people have a stroke every year. Of these, 1,000 are under 30 years of age,1 but most people affected are over 65. There is a mortality rate of 38-47% in the first month post-stroke and by 2020, stroke mortality is expected to double, mainly as a result of the increase in the older population and the future effects of current smoking and lifestyle patterns.1,2,4 Stroke also has a high morbidity and 50% of survivors require special support or residential care. With over 250,000 people in the UK living with disabilities caused by stroke, it is the leading cause of acquired severe disability in adults.1
Transient ischaemic attacks (TIA) are commonly known as 'mini-strokes' and are similar in presentation, but the symptoms resolve fully within 24 hours.1,3 They must always be taken seriously as they are a clear warning that further TIAs may occur and a second episode often causes more damage than the first. Around one person in every 2,000 in the UK experiences a TIA each year. If untreated, one in ten of those people will have a stroke within the next year.3
The effects of stroke are variable (see Table 1), but principally result in unilateral numbness, weakness and partial or complete paralysis of the arm, leg and/or face on the side of the body contra-lateral to the affected side of the brain.1,4 Recovery is varied and mostly takes place in the first 12 to 18 months, and some people with residual disability are able to live relatively independently with the right support (Fig. 1).4 Treatment addresses prevention of further strokes by controlling risk factors (see Table 2) and via hospital/community delivered multidisciplinary rehabilitation programmes with the goal of achieving maximum function and independence.1 The long-term effects of stroke can have a profound effect on individuals and their families who have to deal with residual disabilities and negotiate access to specialist services.1
Oral care and dental treatment
It has been suggested that elective invasive dental care should be deferred for six months after a stroke. However, support with preventive and sometimes prosthodontic care, can be critical in this interim period.3 Stroke survivors often feel helpless, dependent and have a low sense of self-worth,1,3 and tolerance, compassion and reassurance are needed when providing dental care.5
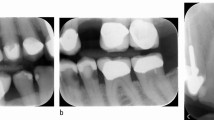
For those patients able to undertake self-care and care of dentures, advice should be offered regarding toothbrush adaptations that takes account of hemiplegia and/or loss of manual dexterity.6 Furthermore, carers or family can be shown how to provide oral care when appropriate (Fig. 2).7 For patients with a unilateral facial palsy (Figs 3a and b),3 where clearance of the oral cavity is reduced due to lack of sensation and control of the musculature of the tongue, lips and cheeks,5 this includes advice on clearing lodged food from the buccal sulcus. This is best done using gauze wrapped round the fingers to sweep the sulcus clean.7
Numbness, weakness and paralysis are associated with stroke4 and can affect the following areas:
a) Mobility
Limited mobility due to disability and/or driving licence restrictions can make it difficult or impossible for an individual to get to, or be taken to, a dental surgery. Thus, they may require a domiciliary assessment for initial advice or care.6 Furthermore, those individuals who can be taken to the surgery in a wheelchair may not be able to transfer to the dental chair without the use of transfer aids or a hoist.6 Guidance on accessing the surgery and the dental chair for patients with physical disabilities has been covered in detail in the first article in this series.6 Practitioners who cannot offer accessible facilities or deliver care in an alternative way should ensure ongoing dental care is organised in an alternative accessible facility.6
b) Swallowing
Dysphagia occurs in many stroke patients.8 A high proportion of people regain their swallowing ability after a few weeks. However, during this time aspiration pneumonia can occur because the gag reflex and palatal movement are diminished, disrupting the normal relationship between respiration and swallowing.9 If dysphagia persists, patients are at continued risk of pulmonary aspiration of saliva and food, etc, and subsequent chest infections.9 They may need to be fed by percutaneous endoscopic gastrostomy (PEG) or nasogastric means to ensure adequate nutrition.10 Aspiration pneumonia is even more prevalent in the presence of poor oral hygiene as dental plaque becomes a reservoir for respiratory pathogens.11,12
Training in swallowing is usually undertaken while the patient is still in hospital or via day-care services and is performed by an inter-disciplinary team including a speech and language therapist and a dentist.1,8,9 As part of this procedure, palatal training appliances (PTAs) can be fabricated to initiate involuntary swallowing. A variety of designs have been described in the literature including modification of the patient's own denture, or fabrication of an appliance retained via Adam's cribs, with either an acrylic palatal extension or wire loop support to aid with swallowing and speech rehabilitation.5,13,14
c) Denture wearing
Older people who have strokes may be edentulous or partially dentate and have dentures which they cannot manage post-stroke.5,8 This is mainly due to loss of muscle control of the cheek and tongue or loss of sensation on one side of the mouth.5 Consequently, following a stroke, complete denture wearers often complain about loose dentures and attribute it to weight loss rather than loss of their previously good muscle skills used to control the dentures.5 Unfortunately, because the patient perceives the dentures as no longer fitting, they can be discarded, lost, or even disposed of, resulting in the loss of valuable information which would have aided the likely success of future dentures.5
Immediately post-stroke, no dentures may be better than very loose ones as it may be easier to talk and eat without this additional problem.5 However, if they are not worn for significant periods of time, denture-wearing skills can be lost and dietary intake compromised. Where denture problems are exclusively due to poor fit, the goal is to improve denture retention.5 This can be achieved temporarily by use of a silicone resilient relining material or permanently by rebasing or relining the original dentures. Wright advocated pouring duplicate dentures which can be modified and then copied in order to construct new dentures, rather than making irreversible changes to the patient's existing dentures.5
When there are no previous dentures for reference, new denture provision requires great care. Fully extended bases with rolled borders provide maximum retention whilst reducing the likelihood of ulceration in areas of reduced oral sensation.5 However, many people who have worn under-extended dentures (particularly lower ones) will take time to adapt to well-extended bases.5 Wright suggests that setting the lower denture teeth more buccally helps to compensate for the denture being displaced towards the side of facial weakness by the active muscles of the unaffected side.5
Partial dentures should be designed with stability and retention in mind. Wright suggests that the denture design includes as few clasps as possible, that teeth are placed in the zone of least interference, and that flanges are shaped to minimise both displacement by the soft tissues and food stagnation. People who have had strokes can have difficulty inserting and removing partial dentures because of poor spatial orientation as well as because of only being able to use one hand. A groove cut in the buccal flange can help the individual to gain purchase on the denture with a fingernail, making its removal from the mouth easier, but in some instances the help of a carer will be required.5
d) Root surface caries
This can develop after a stroke as a result of:
-
Xerostomia,2 which can be a side-effect of anti-hypertensive or anti-depressant medication (Fig. 4)
-
Impaired ability to maintain oral hygiene15 and increasing plaque accumulation
-
Decreased oral clearance and increased food stagnation5
-
Dietary changes, because of dysphagia, to frequent, high calorie, small meals and use of energy rich food supplements, which tend to have a high sugar content.16
An early preventive programme of effective oral hygiene, the use of fluoride and chlorhexidine varnish application to exposed root surfaces can be invaluable in preventing, and in some cases reversing, cervical caries.17 Swallowing difficulties and muscle paralysis may exclude the use of mouthwashes.7,18
e) Communication
There are a number of cognitive and communication disorders associated with strokes, including aphasia, dysphasia and dysarthria.19 Furthermore, patients may initially exhibit agnosia, which results in confusion and an inability to recognise the function of everyday objects such as a toothbrush or denture.4,9 These disorders limit the individual's ability to communicate and to express their wishes. Communication becomes more time consuming and it can be frustrating for the individual, who knows what they want to say but is unable to express themselves, sometimes leading to emotional outbursts.3 Various aids can be used to facilitate communication and engaging the assistance of a carer who understands the individual well is prudent. Strategies for effective communication have been covered in detail in article 2 of this series.19
Medical problems
A stroke patient may present challenges other than those created by the stroke and must be assessed according to their individual needs.5 Pre-morbid risk factors1,2 for stroke include hypertension, diabetes, ischaemic heart disease and obesity, which if present before the stroke will continue to affect the delivery of dental care thereafter. Dental treatment may be further complicated by the use of anticoagulants such as warfarin, ticlopedine or aspirin to prevent further thrombolic episodes.2,3 Guidance for management of these conditions has been outlined in article 5 of this series.20,21 Furthermore as a result of their CVA, stroke patients may suffer from epilepsy.2,3 Treatment goals should be adapted to take into account the patient's changing needs, medical status and degree of recovery.3
Pain and anxiety control
Anxiety, fear and frustration are common emotions for patients who have experienced a stroke.1 Dental pain can compound this situation as the individual is likely to be poorly rested and anxious regarding impending dental treatment. As a result, it is not uncommon for patients seeking dental care to have elevated blood pressure.22 Pain and anxiety management is therefore extremely important in patients who have had a stroke, as is monitoring their blood pressure.3 Explanation, reassurance and the provision of positive feedback is recommended.5 Where available, the use of inhalational sedation using nitrous oxide and oxygen is beneficial in both reducing anxiety and maintaining good oxygenation.2,3,23
Effective local analgesia is important, however it is recommended that vasoconstrictor usage is minimised, especially in older individuals who have reduced resiliency of the cardiovascular system.22 While there is no official maximum dose for use of local anaesthetic with vasoconstrictors, two to three cartridges maximum is considered safe in most instances.22 Treatment planning should take account of this and may need to limit the number of procedures planned for any one visit.3,5 There is general agreement that the use of retraction cords containing epinephrine should be avoided in patients with hypertension.19
Patients taking medication for hypertension are at risk of developing orthostatic or postural hypotension.22 When a patient has been supine or reclined during dental treatment it is prudent to raise the chair slowly and allow them to rest for a moment after uprighting to prevent syncope and falling, with any associated injury.22
Stroke is a possible cause of sudden loss of consciousness or collapse in the dental surgery or waiting room.3 It can be recognised by the signs detailed earlier, especially the characteristic one-sided weakness. Calmly administering oxygen along with protection of the airway and calling for emergency services is the advised course of management.24
2. Parkinson's disease
Parkinson's disease (PD) is a progressive neurological disorder caused by the degeneration of dopaminergic neurones in the substantia nigra of the basal ganglia of the brain. With the depletion of dopamine-producing cells, these parts of the brain that control movement are unable to function normally.25
The aetiology of PD remains unknown, although most researchers believe it is likely to be multi-factorial and have focused on genetic and environmental factors.26 The risk of developing PD increases with age. Symptoms often appear after the age of 50, with some people not being diagnosed until they are in their 70s or 80s. PD occurring before the age of 40 is known as young-onset PD, and if it occurs before the age of 20 it is known as juvenile PD, although this is extremely rare.25 PD affects men and women equally, with an incidence of 1 in 500 in the general population, rising to 1 in 100 in the over 60 age group.27 Around 10,000 people in the UK are diagnosed with PD each year and one in 20 of them (500) will be under 40 years of age.25
PD symptoms are classified as motor and non-motor. It is a very individual condition, with each person experiencing different symptoms. However, the three cardinal signs of PD are motor, and are:
-
Dyskinesia – tremor or involuntary movement
-
Bradykinesia – slow movement
-
Akinesia – muscular rigidity.28
They result in a lack of facial expression with a characteristic 'mask-like' face (Fig. 5), drooling, a quiet monotone voice, slurring of speech, tremor, slow reactions and responses, characteristic short shuffling steps and gait instability.27,28 Various non-motor symptoms include sleep disturbances, urinary urgency, psychoses and depression.25 An increased incidence of Alzheimer's disease (AD) has been reported, occurring in 25-33% of the PD population compared with 10% in the general population.29,30 Increasingly there is evidence from epidemiological investigations, neuro-imaging and genetic and neuropathological studies to support PD dementia as distinct from AD.31
PD tends to develop gradually and it can be months or even years before the symptoms become obvious enough to consult the doctor.25 The dental team may be well placed to notice early symptoms in regular patients. People with suspected PD should be referred, untreated, to a specialist with expertise in the differential diagnosis of PD within six weeks.32 Diagnosis is based on medical history, clinical examination and exclusion of other conditions with PD-like symptoms,25 and should be reviewed every 6-12 months.32
Treatment
There is currently no cure for PD and drugs are used to try to control symptoms. The main aims of drug treatment are to increase the level of dopamine that reaches the brain, stimulate the parts of the brain where dopamine works, or to block the action of other chemicals that affect dopamine.25 Table 3 sets out the main groups of drugs used, their actions, advantages and disadvantages. Levodopa remains the gold standard drug, despite the problems with 'on'/'off' periods such that when the drug is working or 'on' the symptoms are switched 'off', and vice versa. With long-term use, levodopa becomes less reliable and can wear off before the next dose is due or working. This can lead to sudden switches from being 'on' and able to move to being 'off' and immobile.25
Surgical treatment of PD is available, although not common, and includes deep brain stimulation via electrodes implanted into the thalamus, globus pallidus or subthalamic nucleus and connected to a subcutaneous, implantable pulse generator (IPG). Switched on, the IPG produces electrical signals which are sent to the brain to stop or reduce the PD symptoms.25
Good nutrition plays an important role in the management of PD as it can lessen the symptoms and improve the efficiency of drug therapy.25 Dietary advice aims to achieve optimal nutrition by encouraging the person to consume more nutrients and energy in the form most acceptable to them. This can involve frequent small meals and snacks, food enrichment, and the addition of nutritional supplements such as energy-dense, protein-enriched foods and beverages which often have a high sugar content. This regime can have a detrimental effect on oral health. General and dental dietary advice can be conflicting and confusing so it is important that the dental team and the dietician work together with the aim of achieving improved nutritional intake and maintaining good oral health.27
Oral health issues
People with PD experience a number of oral health problems.33,34 These include access to oral healthcare services, xerostomia and root caries,35,36 denture problems,29 and poor oral hygiene and increased periodontal disease due to compromised manual dexterity as a result of muscle rigidity and random movements.37
Xerostomia
Xerostomia occurs in up to 55% of people with PD compared with 3-5% of the total population and 20% of the older population.36 It is due to a decreased quantity or quality of saliva, which is commonly associated with PD drugs alone or a polypharmacy of drugs that older PD patients are taking, rather than the PD itself. Xerostomia impacts on oral health, leading to an increased risk of caries, exacerbation of periodontal disease and poor denture retention, as well as oral discomfort.27
Burning mouth
Burning mouth (BM) is reported by up to 24% of people with PD and is five times as common as in the general population.35 BM has been attributed to a number of factors including xerostomia. However, in PD it seems to be particularly associated with levodopa medication, which promotes parafunctional, purposeless chewing.35 Up to 96% of people with PD reporting BM were taking levodopa, and none of them had experienced BM before the onset of PD.27,38
Root caries
Root caries is a risk for older people with PD for several reasons, including exposed root surfaces, xerostomia, use of high calorie dietary supplements to maintain body weight, and the difficulty of achieving good standards of daily oral hygiene.27 Root caries can be rapid and destructive and the best treatment is to prevent it in the first place by managing the xerostomia (Table 4), ensuring measures to prevent dental disease are in place, and providing dietary advice which is compatible with general and oral health.
When restorations are required, the selection of a conventional or resin-modified glass ionomer provides several advantages.39 Most notably are the abilities of these restoratives to chemically bond to tooth structure and to provide significant fluoride release and uptake, properties that are not present in amalgam, composites, or compomers.39 Additionally, the material itself is relatively easy to use, provides an effective zone of caries inhibition around the margins of the restoration, is not as sensitive to moisture as conventional resin composites or compomers, thus providing a better bond to tooth structure and margination in areas where moisture control is troublesome, and the polymerisation shrinkage is not as great as resin composites, which should also improve marginal integrity.39 Clinical studies have demonstrated longevity of ten years or greater as well as success in xerostomic patients.39
Dysphagia and drooling
Swallowing problems are common in PD, with 50-80% of people developing dysphagia. Several aspects of swallowing can fail. In the oral phase there may be poor lip seal, tongue rigidity, excessive mastication and repetitive tongue pumping actions. In the pharynx there can be delayed swallowing, irregular movements of the epiglottis and inadequate closure of the vocal cords. Consequent aspiration of liquids, food and/or saliva is often silent without the obvious signs of coughing or choking. In the oesophagus, sphincters may operate incorrectly and peristalsis may be impaired, leading to gastro-oesophageal reflux (affecting 54%), heart burn and chest pain and dental erosion.9 These swallowing problems can lead to weight loss, anxiety and stress for people with PD and their carers at meal times, poor compliance with medication, and reduced social contact.40
Paradoxically, although many people with PD have xerostomia, a significant number also experience sialorrhoea and problems with drooling.41 Sialorrhoea can cause social embarrassment, and because saliva pools in the mouth, may lead to aspiration pneumonia. In a questionnaire survey of 105 people with PD, the social and emotional consequences of drooling were reported by 17% and 77% respectively.42 Sialorrhoea is thought to be caused by impaired or infrequent swallowing, rather than hypersecretion. Oral medications, botulinum toxin injections, surgical interventions, radiotherapy and speech therapy have all been advocated to treat sialorrhoea in PD.41 Fuster Torres et al. report that the injection of botulinum toxin A into salivary glands (usually the parotids) reduces salivation for a period of 1.5 to 6 months, with adverse effects such as dysphagia, xerostomia and chewing difficulties being reported in 30% of the studies they reviewed.43 Although botulinum toxin is currently considered the most effective treatment option for PD related sialorrhoea,44 radiotherapy is also considered useful.42 The resultant xerostomia requires proactive management with a rigorous preventive regime (see article 4 of this series).7
Dentures and implants
As the success of dentures depends, to a large extent, on the wearer's ability to control them with their oral musculature and the presence of an adequate quantity and quality of saliva, the muscle inco-ordination, rigid facial muscles and xerostomia of PD conspire to jeopardise denture retention and control.27,35,45,46,47 Denture problems can influence nutritional intake, dietary enjoyment, self-esteem, social interaction and social acceptability, as well as causing embarrassment to the individual. They are likely to compound the existing difficulties that people with PD have when eating and swallowing.27,48
Conventional methods of denture provision have limited success for people with PD and it is likely that dental implants would be more advantageous. However, there is little evidence for the use of implants in PD. One report, based on three cases of edentulous people with PD, describes implant supported dentures as having a positive impact on gastro-intestinal symptoms,49 while another describes the use of magnets for an implant supported overdenture to improve retention.50 Neither paper explores other factors, such as those related to quality of life. Recently Packer et al. investigated the use of implant fixed bridges and implant supported overdentures in a group of nine people with PD. Using the 'Dental Impact on Daily Living Assessment' prior to implant surgery, and at three and twelve months after provision of the final prosthesis, they demonstrated a significant improvement in the domains of eating and satisfaction with the prosthesis after three months, which was maintained at the twelve month review.51 They also found a significant, gradual improvement in oral well-being over the 12 month period, demonstrating that the oral health quality of life of people with PD was improved by the use of dental implants, indicating it as a viable treatment option.51
Oral hygiene
The prevention of dental disease is the most important aspect of dental care for people with PD. Maintaining independence for as long as possible is an important part of the general management of PD and is to be encouraged in oral care wherever possible. Toothbrush handle adaptations can help retain independence for teeth or denture cleaning (see article 4 of this series).7 Some people find the extra weight of an electric toothbrush helps to reduce hand and arm tremors, however for others, muscle weakness may mitigate their use. Dental gels, such as chlorhexidine and fluoride, and dentifrices can be used as normal but mouthrinses should be avoided due to the increased risk of silent aspiration.
The recruitment of a family member or carer to supervise and provide support for daily oral hygiene measures is required when the individual can no longer provide self-care. With advice and support from an empathic dental team, many of the anxieties that carers experience in providing mouth care can be allayed. Finnerty, in association with the Parkinson's Disease Society of the UK, has addressed the issue of oral awareness in a useful booklet entitled Parkinson's and dental health.52
Communication in PD
Communication is jeopardised by the 'mask-like', expressionless face which robs the individual of much of their non-verbal communication; the monotone, quiet speech which makes a person both difficult to hear and to listen to; and the slowness of response that can lead to the person being incorrectly labelled as cognitively impaired. Depression or dementia can further erode the ability to communicate. These communication difficulties can affect the ability to access dental services and to voice needs and wants. The Parkinson's Disease Society leaflet carries the title Just a little more time (Fig. 6), and this is one of the main requirements of people with PD in the dental setting.25 Sufficient time avoids the sense of rushing, which will only delay communication further. Waiting for a response is important, as asking the question again may incur a further time lag in response. The use of questions which require 'yes'/'no' responses can both aid the flow of information and reduce the time taken to obtain it. The time required by some people with PD is best accommodated by the use of a salaried dental service.
Dental management
Appointments should be scheduled for the individual's best time of day, linked to when their drugs are working to avoid them getting 'stuck', and be as short and stress-free as possible to minimise tremors and random movements.27 Control of movements can be difficult during operative dentistry and the use of mouth props and cradling the person's head in the operator's arm at the elbow for stability have both been advocated.53 Care is required when giving an injection to avoid damage to the patient or needle-stick injury to the operator. On occasions it may be in the interests of all parties to defer treatment in the hope that the next appointment will be on a 'less mobile' day.
During operative dentistry, particularly if using conscious sedation, airway protection is a prime concern because of the impaired swallowing reflex and the risk of pulmonary aspiration of saliva and debris. The dental chair should not be reclined more than 45° and the use of rubber dam, with additional suction behind the dam to cope with salivary secretions, is recommended.27
At the end of treatment, the chair should be raised slowly to avoid problems with loss of balance or postural hypotension. On leaving the dental chair, the characteristic slow movements and shuffling gait of PD can make it difficult for the person to get moving. Reminding the person to 'take big steps' helps to initiate the walking process.27
Access
Cost, anxiety and access to dental premises have been identified as the three major barriers to dental care for people with PD.36 Dental services need to take account of the current mobility of the individual and their likely mobility throughout the life of their disease process. This requires the consideration of the individual's access to the dental surgery while they remain ambulant, if they become a wheelchair user, and the possible eventual need for domiciliary dental care.
People with PD need to be made aware of the importance of good oral health and care as early as possible after their diagnosis. Those who already have a general dental practitioner (GDP) should alert the dentist to their diagnosis and continue with regular dental care. People without a dentist need to be put in contact with a GDP or a salaried service practitioner, as appropriate. Individuals should be provided with high quality, low maintenance dental care in the early stages of PD when they are more amenable to dental treatment.27 Also, it is important to initiate preventive measures to minimise the need for further dental treatment.
The dental team is an important part of the PD multidisciplinary care team as a healthy mouth can reduce the problems associated with PD and help to maintain the individual's self-esteem and quality of life. Key people to liaise with are the dietician, the speech and language therapist and the specialist PD nurse.
3. Dementia
Dementia is a progressive, neurodegenerative disease that affects the ability to perform daily living activities. It has been described as a variety of syndromes rather than a sign or a symptom or a disease,54 and there are a number of types of both reversible and irreversible dementia (Table 5).
There are currently 700,000 people with dementia in the UK, of whom 15,000 have early onset dementia, ie onset before the age of 65. This is considered a major underestimate by up to three times because of the way the data relies on referrals to services. Two thirds of people with dementia are women. Also, two thirds of people live in the community and one third live in care homes. Of people living in care homes, 64% have a form of dementia.55
Most of the dental literature relating to dementia is specific to Alzheimer's disease (AD). This is probably because AD is one of the most protracted forms of dementia and thus, oral health is likely to be an issue at some stage during its process. The clinical features, symptoms and the principles that would be used in providing oral healthcare for people with AD and other types of dementia are similar, although the timescale of the dementia process may be different and in some cases accelerated, eg CJD-related dementia.56 For these reasons this article tends to refer to AD, although the information can be equally well applied to any type of dementia.
Aetiology
The immediate cause of AD is the loss of neurones. Its aetiology is unknown but a number of risk factors are recognised. The greatest is age, with the risk of developing AD increasing with age from 1 in 1,000 below the age of 65 to 5-10 in 100 over the age of 65, and 1 in 5 by the age of 80 years.55 Other risk factors include inherited family risk, severe or repeated brain damage and Down's syndrome.21,56,57
Diagnosis
Diagnosis usually occurs over a period of time and is made on a differential diagnosis of ruling out other types of dementia, recording symptoms over time and the results of cognitive/memory tests.56 Confirmation of diagnosis is made postmortem when the specific pathology of senile plaques and neurofibrillary tangles are identified in the brain.58
Clinical features and symptoms
Dementia has been famously described as 'an embuggerance' by the author Terry Pratchett, who in the early stages of dementia continues to write but describes how his once decent touch-typing has deteriorated to 'hunt and peck' two fingered tapping.59 Clinical features characterising AD are generally described as memory loss, language deterioration, impaired visuo-spatial skills, poor judgment, indifferent attitude, but preserved motor function.56 AD is a progressive disease, appearing first as memory decline and, over several years, destroying cognition, personality and ability to function (Table 6).58 The type, severity, sequence, and progression of mental changes vary widely, although AD is usually slowly progressive, starting with mild memory problems and ending with severe brain damage over an average period of 8-10 years from diagnosis. The commonest cause of death is infection and 60,000 deaths a year are directly attributable to dementia.55 Its onset is insidious and, in the early stages, a person in their familiar home environment may be able to pass off the symptoms as forgetfulness. With time a pattern of problems emerges and, as AD progresses, the individual may:
-
Experience short-term memory loss and routinely forget recent events, appointments, names and faces
-
Have difficulty in understanding what is said
-
Become confused by routine activities such as handling money, driving a car or using a washing machine
-
Become increasingly disorientated in time, place and, eventually, person
-
Undergo personality changes, becoming agitated, irritable and sometimes verbally abusive or becoming apathetic and non-responsive
-
Experience delusions, illusions and/or hallucinations.56
In the advanced stages people may adopt unsettling behaviour such as getting up in the middle of the night and/or wandering off from home and becoming lost. Finally, the personality disintegrates and the person becomes totally dependent on others for daily living activities.
Management
Management is aimed at maintaining quality of life. Whilst there is no cure, drugs which slow down or stabilise the symptoms of dementia are now available (Table 7).60 Drugs are also used to control the depression, agitation and challenging behaviour associated with AD. Antipsychotics such as risperidone (Risperdal) and antiepileptics such as carbamazepine (Tegretol) may improve behavioural symptoms. Memory aids and familiar routines are helpful in maintaining as normal a life for as long as possible but as AD progresses, the individual will need more support and eventually is likely to need close supervision and, ultimately, nursing care.56
Oral health
It is well recognised that oral health declines as AD progresses. The impact of the disorder, especially in the latter stages, leads to poor oral hygiene with an increase in periodontal disease,61,62,63 higher levels of coronal and cervical decay62,64,65 and a greater incidence of other dental problems such as denture wearing or the ability to comply with oral care procedures.62,63,66,67,68,69,70,71
Risk factors for dental decay in this group of people have been identified as sex (male), dementia severity, high carer burden, oral hygiene difficulties, use of neuroleptic and other medication causing xerostomia, and previous caries experience.62 The commonest medications used in AD have the potential to cause xerostomia and, if medications are syrup-based, the potential for the development of caries is increased. Additionally, people with poor cognitive function have a four times higher risk of not using dental services regularly.64
Assessment for dental treatment
The decision making process in planning oral healthcare for people with dementia and/or other cognitive impairments presents challenges to the dental team. Ideally a dentist should be part of the multidisciplinary care team from diagnosis so that oral care can be planned throughout the disease process and does not become crisis management in the final phase of the condition. Treatment planning must take account of the stage of the illness and the level of cognitive impairment. Before assessing the oral/dental status and formulating an individualised treatment plan, it is prudent to carry out a comprehensive patient assessment, including the level of cognitive impairment, ablity to carry out daily living activities, and level of social functioning.54 Cognitive function is a changing phenomenon and may alter from day to day or if the patient is disorientated. In some cases, an educated and eloquent manner can be misleading of the level of understanding, so consultation with members of the multidisciplinary psychiatric team, relatives and carers is essential to obtain an accurate assessment. Article 3 in this series discusses how to assess capacity to consent.72
Niessen et al. describe an index of dental management based on an assessment of observed behaviour and ability which provides useful guidance on treatment planning approaches (Table 8). The Guidelines for the development of local standards of oral health care for people with dementia sets out an algorithmic approach to decision making and treatment planning for patients with cognitive impairment that provides clinical guidance.56 It can act as an aid to the clinician in developing treatment options that are realistic and based on wide-reaching consultation with family, carers and the multi-disciplinary team.
Lapeer urged the dental profession to treat, rather than ignore, any oral health problems as people in the late stage of AD are often unable to communicate dental symptoms of pain and dysfunction,73 which may manifest as a sudden change or worsening in behaviour (Table 9).54,63 If people with dementia present with oral and/or facial trauma, the question of non-accidental injury (NAI) must be considered.74 While there is no evidence to support the role of dental disease in precipitating NAI, the possibility that it may be the direct result of challenging behaviour due to dental pain should not be underestimated.
General principles for oral healthcare
Oral healthcare planning should take account of caregivers' perceptions and knowledge about oral health and hygiene as they represent the primary providers to these patients as dementia progresses.75,76 It is important to remember that many carers are spouses or siblings of a similar age to the individual with dementia and the care burden can be heavy (Fig. 7). Consequently oral health may not always be a priority, and support from an empathic dental team can be invaluable. Where people live in care homes, it is important, if it is not already in place, to introduce a routine oral health assessment tool that can be used by care staff. Further information and assessment tools can be found in the Guidelines for the development of local standards of oral health care for people with dementia.56
The following guidelines are useful when considering strategic, long-term, oral care planning for people with AD:
-
Instigate appropriate preventive measures as early as possible
-
Undertake dental intervention in the early stages of the condition to manage outstanding dental treatment needs
-
Ensure dentures are named,7,56,77 cleaned professionally on a regular basis and renewed using a duplication technique when their replacement is necessary
-
Instigate regular reviews tailored to the individual's needs to maintain the oral status quo, avoid pain and minimise further interventions
-
Ensure that fear, stress and embarrassment for the individual and their carer are minimised by adopting an 'open door' approach and providing back-up and support
-
Provide the carer with relevant information such as the Alzheimer's Society Dental Care and Dementia Factsheet.77
Coping with dental treatment
The progression of dementia varies enormously, as does the ability to cope with dental treatment. Some people are comfortable with a visit to the dentist, while others find the whole experience very distressing. People who have had regular dental treatment often remember what they are expected to do in a dental surgery and have little difficulty co-operating with simple procedures until their dementia is advanced. For other people the journey to the surgery, the strange environment and the unfamiliar faces of the dental team can exacerbate their confusion, making treatment difficult or impossible. In these circumstances domiciliary dental care should be considered, as seeing the person in their familiar and 'safe' environment can enhance co-operation. For further information on domiciliary care, the reader is referred to the British Society for Disability and Oral Health's guidelines.78
Types of dental treatment
Dental treatment provision may be dictated by the stage of dementia that the individual has reached.
In the early stages of dementia most types of dental care are still possible. Treatment should be planned bearing in mind that the individual will eventually be unable to look after their own teeth. Key teeth may be identified and restored. Advanced restorative treatment (such as crowns, bridges and implants) should only be considered if someone is prepared to carry out daily hygiene measures on behalf of the individual with dementia when they reach the stage where they can no longer self-care. At times it may be necessary to consider the use of physical intervention, sedation or general anaesthesia, although this requirement is likely to be more common as the disease process progresses. Preventing further dental disease through establishing a rigorous preventive regime is critical at this stage. Article 4 in this series provides information on this subject.7
In the middle stage of dementia the person is often relatively physically healthy but has lost cognitive skills. The focus of dental treatment is likely to change from restoration to the prevention of further dental disease. Some people may find the acceptance of dental treatment beyond their tolerance and require sedation or general anaesthesia for their dental treatment. The decision will be based on the individual's ability to co-operate and their dental treatment needs, general health and social support.
In the later stages of dementia the person is severely cognitively impaired and often physically frail or disabled. Treatment at this stage focuses on prevention of oral disease, maintaining oral comfort and provision of emergency treatment.
It is beyond the scope of this article to provide detailed information on the provision of different types of dental treatment for people with dementia and the reader is referred to the Oral health guidelines for the development of local standards of oral health care for people with dementia for further information.56
4. Elder abuse
Elder abuse (EB) and neglect (mistreatment) are increasingly acknowledged as a social problem in the UK. Until last year when the UK study of abuse and neglect of older people was published, there was an absence of any sound data on its extent.79 According to this study, 2.6% of people aged 66 and over living in private households (including sheltered housing) reported that they had experienced mistreatment involving a family member, friend or care worker during the past year. This equates to about 227,000 people or one in 40 of the older population.79
Considering mistreatment in the past year involving family, close friends and care workers, the predominant type of mistreatment reported was neglect (1.1%), followed by financial abuse (0.7%). The prevalence of psychological and physical abuse was similar (both 0.4%) and sexual abuse was the least reported type (0.2%).79 Table 10 sets out the five types of mistreatment with examples. Women were more likely to say that they had experienced mistreatment than men – 3.8% and 1.1%, respectively. Mistreatment increases with declining health status, disability, depression and loneliness.79 Just over half the episodes involved a spouse or partner, 49% another family member, 13% a care worker and 5% a close friend (respondents could mention more than one person).79
People who are physically, emotionally or psychologically frail and dependent on others for care are most at risk of elder abuse. It happens in the home as well as in care homes, nursing homes and hospitals. It is important that members of the dental team, particularly those members doing domiciliary visits and seeing people in their own environment, know how to recognise mistreatment (Table 11) and how to act upon this knowledge. The dental team may also notice signs, particularly of physical abuse, in older patients visiting the dental practice.
If elder abuse is suspected, try to speak to the older person about what you have noticed, being as open and honest as possible.80 Give them the opportunity to talk, listen carefully to what they have to say, and offer to seek help if that is appropriate. Some people may ask you to promise not to tell anyone else about the abuse. Always be honest and never make false promises as sometimes, as in a care home, the abuse might affect more than one person and there is a responsibility to other people too. Explain who might be able to help, eg GP, social care professionals or the police. Ask what they want you to do and perhaps offer to approach one of these agencies on the person's behalf.80
If you were correct in your concerns or still have strong suspicions, ring the Action on Elder Abuse (AEA) helpline for advice. It is available weekdays 9am-5pm on freephone 0808 808 8141 and is staffed by specially trained staff and volunteers, to provide confidential support and advice for people who have been abused or know someone who may be suffering abuse. Alternatively contact the local social services. In England and Wales you should say that you want to talk about an adult protection issue as both these countries have special arrangements in place. In Scotland you should speak to the social work department and explain you are concerned about elder abuse. If concerned about poor practice or abuse in a care home or by domiciliary care services, contact the appropriate organisation, details of which can be found via the AEA website or helpline. However, if you believe a crime has been committed you should contact the police.80
References
The Stroke Association. Information webpage. http://www.stroke.org.uk/information/index.html (accessed 18 September 2008).
Scully C, Cawson R . Medical problems in dentistry. Chapter 17. Oxford: Wright, 1999.
Scully C, Dios P D, Kumar N . Special care in dentistry: handbook of oral healthcare. pp 412–418. Edinburgh: Churchill Livingstone, 2007.
Warlow C, Sudlow C, Dennis M, Wardlaw J, Sandercock P . Stroke. Lancet 2003; 362 (9391): 1211–1224.
Wright S . Denture treatment for the stroke patient. Br Dent J 1997; 183: 179–184.
Dougall A, Fiske J . Access to special care dentistry, part 1. Access. Br Dent J 2008; 204: 605–616.
Dougall A, Fiske J . Access to special care dentistry, part 4. Education. Br Dent J 2008; 205: 119–130.
Ostuni E . Stroke and the dental patient. J Am Dent Assoc 1994; 125: 721–727.
Selley W, Ellis R, Flack F C . The role of the dental surgeon in the management of dysphagia following a stroke. Gerodontic Study Group Newsletter 1995.
Löser C, Aschl G, Hébuterne X et al. ESPEN guidelines on artificial enteral nutrition – percutaneous endoscopic gastrostomy (PEG). Clin Nutr 2005; 24: 848–861.
Terpenning M, Taylor G, Lopatin D, Kerr C, Dominguez B . Aspiration pneumonia: dental and oral risk factors in an older veteran population. J Am Geriatr Soc 2001; 49: 557–563.
Leibovitz A, Plotnikov G, Habot B, Rosenberg M, Segal R . Pathogenic colonization of oral flora in frail elderly patients fed by nasogastric tube or percutaneous entrogastric tube. J Gerontol 2003; 58: 52–55.
Selley W, Roche M, Pearce V, Ellis R, Flack F . Dysphagia following strokes; clinial observations of swallowing rehabilitation employing palatal training devices. Dysphagia 1995; 10: 32–35.
Ono T, Hamamura M, Hondu K, Nokubi T . Collaboration of a dentist and speech-language pathologist in the rehabilitation of a stroke patient with dysarthria: a case study. Gerodontology 2005; 22: 116–119.
Wilkins E M . Patients with special needs. In Clinical practice of the dental hygienist. 9th ed. Boston: Lippincott, Williams & Wilkins, 2004.
Griffiths J, Boyle S . Holistic oral care – a guide for health professionals. Chapter 13. London: Stephen Hancocks Ltd, 2005.
Brailsford S, Fiske J, Gilbert S, Clark D, Beighton D . The effects of the combination of chlorhexidine/thymol and fluoride containing varnishes on the severity of root caries lesions in frail institutionalised elderly people. J Dent 2002; 30: 319–324.
Ahlborg B . Practical prevention. In Nunn J (ed) Disability and oral care. London: FDI World Dental Press, 2000.
Dougall A, Fiske J . Access to special care dentistry, part 2. Communication. Br Dent J 2008; 205: 11–21.
Dougall A, Fiske J . Access to special care dentistry, part 5. Safety. Br Dent J 2008; 205: 177–190.
Lewis D, Fiske J, Dougall A . Access to special care dentistry, part 8. Special care dentistry services: seamless care for people in their middle years – part 2. Br Dent J 2008; 205: 359–371.
Herman W, Konzelman J, Prisant M . New national guidelines for hypertension – a summary for dentistry. J Am Dent Assoc 2004; 135: 576–579.
Boyle C . Sedation and general anaesthesia in special care dentistry. In Fiske J, Dickinson C, Boyle C, Rafique S, Burke M Special care dentistry. pp 139–146. London: Quintessence Publishing, 2007.
British national formulary. London: BMJ Publishing Group/RPS Publishing, 2008.
Parkinson's Disease Society. What is Parkinsons? webpage. http://www.parkinsons.org.uk/about-parkinsons/what-is-parkinsons.aspx (accessed 19 September 2008).
Stuart D A . Pathology, aetiology and pathogenesis. In Playfer J R, Hindle J V (eds) Parkinson's disease in the older patient. pp 11–29. London: Arnold, 2001.
Fiske J, Hyland K . Parkinson's disease and oral care. Dent Update 2000; 27: 58–65.
Macphee G . Diagnosis and differential diagnosis. In Playfer J R, Hindle J V (eds) Parkinson's disease in the older patient. pp 43–76. London: Arnold, 2001.
Lieberman A, Dziatolowsky M, Kupersmith M . Dementia in Parkinson's disease. Ann Neurol 1979; 6: 335–339.
Aarsland D, Tandberg E, Larsen J . Frequency of dementia in Parkinson's disease. Ann Neurol 1996; 53: 538–542.
Farlow M, Cummings J . A modern hypothesis: the distinct pathologies of dementia associated with Parkinson's disease versus Alzheimer's disease. Dement Geriatr Cogn Disord 2008; 25: 301–308.
National Institute of Health and Clinical Excellence. Parkinson's disease: diagnosis and management in primary and secondary care. London: NICE, 2006. Clinical Guideline 35.
Nakayama Y, Washio M, Mori M . Oral health conditions in patients with Parkinson's disease. J Epidemiol 2004; 14: 143–150.
Anastassiadou V, Katsarou Z, Naka O, Bostanzopoulou M . Evaluating dental status and prosthetic need in relation to medical findings in Greek patients suffering from idiopathic Parkinson's disease. Eur J Prosthodont Restor Dent 2002; 10: 63–68.
Clifford T, Warsi M, Burnett C, Lamet P J . Burning mouth in Parkinson's disease sufferers. Gerodontology 1998; 15: 73–78.
Clifford T, Finnerty J . The dental awareness and needs of a Parkinson's disease population. Gerodontology 1995; 12: 99–103.
Schwarz J, Heimhilger E, Storch A . Increased periodontal pathology in Parkinson's disease. J Neurol 2006; 253: 608–611.
Lamey P . Burning mouth syndrome: approach to successful management. Dent Update 1998; 25: 298–300.
Turner E, Shook L, Lackey M . Accessing and restoring root caries: a case report. J Tenn Dent Assoc 2007; 87: 20–22.
Boaden E . The science and practice of multidisciplinary care in Parkinson's disease and Parkinsonism: swallowing problems. British Geriatrics' Society Parkinson's Disease Special Interest Group Meeting, London, 1998.
Chou K, Evatt M, Hinson V, Kompoliti K . Sialorrhea in Parkinson's disease: a review. Mov Disord 2007; 22: 2306–2313.
Kalf J, Smit A, Bloem B, Zwarts M, Munneke M . Impact of drooling in Parkinson's disease. J Neurol 2007; 254: 1227–1232.
Fuster Torres M, Berini Aytés L, Gay Escoda C . Salivary gland application of botulinum toxin for the treatment of sialorrhea. Med Oral Patol Oral Cir Bucal 2007; 12: E511–E517.
Molloy L . Treatment of sialorrhoea in patients with Parkinson's disease: best current evidence. Curr Opin Neurol 2007; 20: 493–498.
Persson M, Österberg T, Granérus A K, Karlsson S . The influence of Parkinson's disease on oral health. Acta Odontol Scand 1992; 50: 37–42.
Hyland K, Fiske J, Matthews N . Nutritional and dental health management in Parkinson's disease. J Community Nurs Online 2000; 14 (1). http://www.jcn.co.uk/journal.asp?MonthNum=01&YearNum=2000&Type=backissue&ArticleID=306
Lorefält B, Granénis A, Unosson M . Avoidance of solid food in weight losing older patients with Parkinson's disease. J Clin Nurs 2006; 15: 1404–1412.
Zarb G A . Oral motor patterns and their relation to oral prostheses. J Prosthet Dent 1982: 47: 472–478.
Heckmann S M, Heckmann J G, Weber H P . Clinical outcomes of three Parkinson's disease patients treated with mandibular implant overdentures. Clin Oral Implants Res 2000: 11: 566–571.
Chu F, Deng F, Siu A, Chow T W . Implant-tissue supported, magnet retained mandibular overdenture for an edentulous patient with Parkinson's disease: a clinical report. J Prosthet Dent 2004; 91: 219–222.
Packer M, Nikitin V, Coward T, Davis D M, Fiske J . The potential benefits of dental implants on the oral health quality of life of people with Parkinson's disease. Gerodontology 2008; in press.
Finnerty J . Parkinson's and dental health. London: Parkinson's Disease Society, 1996. Code B045
Jolly D, Paulson R, Paulson G, Pike J . Parkinson's disease: a review and recommendations for dental management. Spec Care Dentist 1989; 9: 74–78.
Ettinger R L. Dental management of patients with Alzheimer's disease and other dementias. Gerodontology 2000; 17: 8–16.
Alzheimer's Society. Dementia UK. The full report. London: Alzheimer's Society, 2007.
Fiske J, Frenkel H, Griffiths J, Jones V . Guidelines for the development of local standards of oral health care for people with dementia. Gerodontology 2006; 23 (Suppl 1): 5–32.
Lewis D, Fiske J, Dougall A . Access to special care dentistry, part 7. Special care dentistry services: seamless care for people in their middle years – part 1. Br Dent J 2008; 205: 305–317.
Ritchie K, Lovestone S . The dementias. Lancet 2002; 360 (9347): 1759–1766.
Kennedy M . Profile: Terry Pratchett. The Guardian 2008 March 14.
Alzheimers Society website. 2008. http://www.alzheimers.org.uk
Warren J, Chalmers J, Levy S, Blanco V L, Ettinger R L . Oral health of persons with and without dementia attending a geriatric clinic. Spec Care Dentist 1997; 17: 47–53.
Chalmers J, Carter K D, Spencer A J . Caries incidence and increments in community-living older adults with and without dementia. Gerodontology 2002; 19: 80–94.
Henry R, Wekstein D . Providing dental care for patients diagnosed with Alzheimer's disease. Dent Clin North Am 1997; 41: 915–942.
Avlund K, Holm-Pedersen P, Morse D, Vitanen M, Winbland B . Tooth loss and caries experience in very old Swedish people: the relationship to cognitive function and functional ability. Gerodontology 2004; 21: 17–26.
Ellefsen B, Holm-Pedersen P, Morse D, Schroll M, Andersen B, Waldemar G . Caries prevalence in older persons with and without dementia. J Am Geriatr Soc 2008; 56: 59–67.
Whittle J, Sarll D, Grant A, Worthington H . The dental health of the elderly mentally ill: preliminary report. Br Dent J 1987; 162: 381–383.
Ship J, DeCarli C, Friedland R, Baum B J . Diminished submandibular salivary flow in dementia of the Alzheimer's type. J Gerontol 1990; 45: 61–66.
Ship J . Oral health of patients with Alzheimer's disease. J Am Dent Assoc 1992; 123: 53–58.
Jones J A, Lavallee N, Alman J, Sinclair C, Garcia R I . Caries incidence in patients with dementia. Gerodontology 1993; 10: 76–82.
Adam H, Preston A . The oral health of individuals with dementia in nursing homes. Gerodontology 2006; 23: 99–105.
Rejnefelt I, Andersson P, Renvert S . Oral health status in individuals with dementia living in special facilities. Int J Dent Hyg 2006; 4: 67–71.
Dougall A, Fiske J . Access to special care dentistry, part 3. Consent and capacity. Br Dent J 2008; 205: 71–81.
Gitto C, Moroni M, Terezhalmy G, Sandu S . The patient with Alzheimer's disease. Quintessence Int 2001; 32: 221–231.
Cowen H, Cowen P . Elder mistreatment: dental assessment and intervention. Spec Care Dentist 2002; 22: 23–32.
Watanabe Y . Supporting independent oral health care among the home-care elderly – the influence of dementia. Kokubyo Gakkai Zasshi 2006; 73: 53–61.
Hugo F, Hilgert J, Bertuzzi D, Padilha D, De Marchi R . Oral health behaviour and socio-demographic profile of subjects with Alzheimer's disease as reported by their family caregivers. Gerodontology 2007; 24: 36–40.
Alzheimer's Society. Dental care and dementia. London: Alzheimer's Society, 2008. Factsheet 448. http://www.alzheimers.org.uk/factsheet/448
Fiske J, Lewis D . The development of standards for domiciliary dental care services: guidelines and recommendations. British Society for Disability and Oral Health, 2000. http://www.bsdh.org.uk/guidelines/domicil.pdf
O'Keefe M, Hills A, Doyle M et al. UK study of abuse and neglect of older people. Prevalence survey report. London: Comic Relief/Department of Health, 2007. http://www.comicrelief.com/docs/elder-abuse/ComicRelief-ElderAbuse-Full.pdf
Action on Elder Abuse. What is elder abuse? webpage. http://www.elderabuse.org.uk/What%20is%20abuse/what_is_abuse%20define.htm (accessed 19 September 2008).
Neissen L C, Jones J A, Zocchi M, Gurian B . Dental care for the patient with Alzheimer's disease. J Am Dent Assoc 1985; 110: 207–209.
Acknowledgements
The illustrative material used in Figure 7 is credited to http://www.JohnBirdsall.co.uk.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dougall, A., Fiske, J. Access to special care dentistry, part 9. Special care dentistry services for older people. Br Dent J 205, 421–434 (2008). https://doi.org/10.1038/sj.bdj.2008.891
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2008.891
This article is cited by
-
Clinicians’ view on the management of oral health in Parkinson’s disease patients: a qualitative study
BDJ Open (2023)
-
A rapid review of barriers to oral healthcare for vulnerable people
British Dental Journal (2019)
-
Dementia friendly dentistry for the periodontal patient. Part 1: recognising and assessing patients with dementia
British Dental Journal (2019)
-
Dementia friendly dentistry for the periodontal patient. Part 2: ethical treatment planning and management
British Dental Journal (2019)
-
The new heterologous fibrin sealant in combination with low-level laser therapy (LLLT) in the repair of the buccal branch of the facial nerve
Lasers in Medical Science (2016)