Key Points
-
This technique makes anaesthesia of the anterior palatal area less painful for the patient.
-
The technique of anaesthetising the anterior hard palate will be more easy for dental students to learn.
-
The injection site is more accessible and the risk of injection necrosis of the palatal mucosa is omitted.
Abstract
Background and aim The conventional nasopalatine nerve block is commonly used to obtain anaesthesia in the anterior portion of the palate. The painful nature of this approach, however, has led investigators to seek alternative methods to obtain anaesthesia. Labial infiltration of the maxillary central incisors can be considered an effective anaesthetic approach for the anterior palate. Our study aimed to assess the anaesthetic effect of a modified labial infiltration method on the nasopalatine nerve.
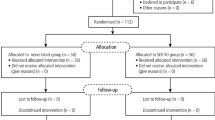
Materials and method A case-control clinical trial was done on 60 patients referring for extraction of maxillary incisors (mean age 44 years). The patients were divided into two groups of 30 people. For the first group, a primary conventional infiltration was given to each patient from a point between the maxillary canine and the lateral to obtain preliminary anaesthesia for the maxillary anterior labial area. The second or the control group was anaesthetised by conventional injection into incisive papilla. Two to three minutes afterwards, a labial infiltration approach was done and the amount of pain determined by OPS (objective pain score) was assessed. After five to six minutes the level of anaesthesia in the anterior palate was assessed in both groups by an explorer and recorded as pain-free, mild pain or severe pain. The sign test was used to statistically analyse the data (p <0.001).
Results Total, moderate and no anaesthesia were observed in 76.7%, 13.3%, and 10% of the patients receiving anesthetic injection at the labial side. For the control group, these results were 83%, 17% and 0% respectively.
Conclusion This method of labial infiltration may be an effective alternative to the painful conventional palatine nerve block to obtain efficient anaesthesia of the anterior palate (p <0.001).
Similar content being viewed by others
Introduction
The importance of pain management during dental procedures cannot be over-emphasised. Without proper anaesthesia, the treatment planned may result in potential harm to the patient. Anaesthetic injections should be as painless as possible, especially in the palate which is the most sensitive area of the oral cavity for injection.1 Anaesthesia of the nasopalatine nerve is mandatory to perform surgical procedures on the soft and hard tissues of the anterior palate and extraction of upper anterior teeth.1 The nasopalatine nerve passes through the anterior nasal spine and innervates the anterior portion of palate, maxillary central incisors and nasal floor and finally enters the oral cavity via the incisal foramen (Fig. 1).1,2,3
Labial tissues are anaesthetised by labial infiltration. Obtaining anaesthesia for the relevant palatal soft tissue is however, impossible this way and necessitates direct injection of an anaesthetic agent in the palatal area. Palatal soft tissues, especially in the vicinity of the hard palate, are tightly attached to the underlying bone and injection in this area is painful when the conventional method for injecting the anaesthetic agent directly beside the incisive papilla on the palatal aspect of the maxillary central incisor is used. Results have shown that needle penetration in the anterior hard palate was more uncomfortable than in the posterior palate.4
However, permanent removal of maxillary teeth without a palatal injection has been possible.1 We assessed this less painful approach to obtain anaesthesia in the anterior palate and aimed to determine the anaesthetic efficiency of our method on the nasopalatine nerve in patients referred for extraction of maxillary anterior incisor teeth to our department.
Materials and method
This clinical trial included 60 patients referring for the extraction of maxillary incisors. The patients were divided into two groups of 30 people. For the first group, after clinical and radiographic examinations, anaesthesia of the maxillary labial area was obtained by infiltration of 1.8 cc of local anaesthetic agent through a point 5 mm above the midpoint between the apices of left/right maxillary canine and lateral incisor (Fig. 2). The second or control group was anaesthetised by conventional injection into the incisive papilla. After 2-3 minutes and relative anaesthesia of the labial area, infiltration was administered via a needle inserted superior to the apices of central incisors in the vicinity of the superior border of the base of the anterior nasal spine near the nasal floor, to obtain anaesthesia in the anterior palate.
Needle positioning: for the case group, the needle was inserted with a 45° angle to the maxillary midline and labial fraenum with the bevel facing the bone. 1.8 cc of lidocaine anaesthetic with 1/80,000 adrenalin was injected within 30-40 seconds. The control group received their incisive papilla injection as normal.
Anaesthesia of the upper lip and anterior palate was assessed and patients' comfort during the operation and the amount of pain experienced by them were evaluated by OPS (objective pain score). Five to six minutes following the second injection, the extension and efficiency of anaesthesia in the anterior palate was examined by an explorer or periosteal elevator. Based on the verbal descriptor scale (VDS), patients were asked to express their perception as painless, mild pain, or severe pain.
Pain-free indicated complete anaesthesia of the nasopalatine nerve and no need for another injection for extraction. In the case of mild pain, severe pain, moderate pain or no anaesthesia, a complementary conventional injection in the palate was needed. Patient age, gender, level of anesthesia, and frequency of injections were recorded in datasheets. Data was assessed via SPSS software and classified. Statistical analysis was performed using the sign test.
Results
Our experimental group of 30 patients (16 females and 14 males) with a mean age of 44.2 years for which extraction of the maxillary anterior incisor was indicated had complete anaesthesia of the maxillary anterior area of the palate in 23 patients (76.7%) using our method. The sign test revealed this to be statistically significant (p <0.001). The other 7 patients (23.3%) needed a conventional nasopalatine nerve block to complement the effect of anaesthesia required for extraction. Moderate and no anaesthesia were observed in 13.3%, and 10% of the cases respectively. Age and gender did not influence the level of anaesthesia obtained by our method. No complications or post-injection complaints were found following this method.
For those patients in the control group, 83% had complete and 17% had moderate numbness at their anterior palate. We did not face any case of anaesthesia failure with the conventional group.
Discussion
This study revealed that the level of anaesthesia obtained by our method in the anterior palate was satisfactory. The labial infiltration method resulted in total anaesthesia in the majority of the cases. Failures may be the result of anatomic and physiologic variations in different people. An eight minute wait might have been more effective than five minutes following the second injection. Some state that epinephrine in lidocaine cartridges when administered into the maxillary vestibule causes moderate pain during this injection. However, palatal injection discomfort does not differ between solutions.2
Lidocaine with epinephrine produces longer-lasting soft tissue anaesthesia than plain lidocaine following palatal infiltration.3 However, no correlations were found between these issues or gender and levels of obtained anaesthesia in our study. The amount of pain experienced by the patients during the injection in the labial infiltration approach was less than the conventional approach in most of our cases and no complications relevant to extractions or anaesthesia were encountered in this study.
References
Uckan S, Dayangac E, Araz K . Is permanent maxillary tooth removal without palatal injection possible? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 102: 733–735.
Meechan J G, Day P F . A comparison of intraoral injection discomfort produced by plain and epinephrine-containing lidocaine local anesthetic solutions: a randomized, double-blind, split-mouth, volunteer investigation. Anesth Prog 2002; 49: 44–48.
Meechan J G, Day P F, McMillan A S . Local anesthesia in the palate: a comparison of techniques and solutions. Anesth Prog 2000; 47: 139–142.
Meechan J G, Howlett P C, Smith B D . Factors influencing the discomfort of intraoral needle penetration. Anesth Prog 2005; 52: 91–94.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Lassemi, E., Motamedi, M., Jafari, S. et al. Anaesthetic efficacy of a labial infiltration method on the nasopalatine nerve. Br Dent J 205, E21 (2008). https://doi.org/10.1038/sj.bdj.2008.872
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2008.872
This article is cited by
-
Comparative study of articaine and lidocaine without palatal injection for maxillary teeth extraction
Clinical Oral Investigations (2019)