Key Points
-
Medical imaging via CT can enable detailed virtual case planning of a full arch implant reconstruction.
-
A virtual treatment plan can be translated into a pre-planned surgical outcome using a precise drilling stent.
-
A predictable prosthetic outcome can be achieved using an immediate load procedure after virtual treatment planning and guided implant placement.
Abstract
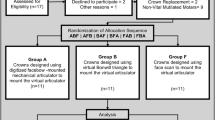
This paper describes a protocol which incorporates the benefits of medical imaging, computerised virtual treatment planning, computer guided surgery, and the fitting and immediate loading of a preformed provisional full arch fixed prosthesis. The protocol can be adapted for use with the implant system of the operator's choosing and a prosthetic carrier presents the immediate load prosthesis to the mouth in its correct three-dimensional inter-occlusal relationship, simplifying the prosthetic stages for immediate load case management. Two case studies are described to illustrate the procedure for both mandibular and maxillary reconstructions.
Similar content being viewed by others
Introduction and background
Previously, in order to achieve osseointegration of dental implants, it has been recommended that implants remain load-free for 3-4 months in the mandible and 6-8 months in the maxillae.1 However, in recent years various studies have reported equally good treatment outcomes when immediate loading of implants has taken place under appropriate clinical conditions.2 Success in such cases is dependent upon control of micro-movement at the bone/implant interface during implant loading. With full arch immediate load prostheses this can be achieved when implants attain adequate primary stability at the time of placement, are subject to rigid inter-implant splinting, and occlusal forces are appropriately controlled during the osseointegration period.3,4,5,6,7
Taking surgical protocols and patient management a step further, there has also been a growing interest in exploring the potential of a flapless surgical approach to minimise post-operative trauma and accelerate postoperative healing.8,9,10 However, this approach can risk significant complications should the operator misinterpret the underlying hard and soft tissue anatomy.
Against this background, it has been shown that implant placement using a computer generated surgical guide based on appropriate medical imaging can dramatically improve the degree of surgical accuracy.11,12
Treatment concept
This report documents a technique to harness the benefits of CT scanning to generate and fit an immediate load full arch temporary prosthesis supported by guided implants fitted with a flapless surgical protocol. The protocol is illustrated with the use of two case presentations – one maxillary, one mandibular.
Guided implant placement is achieved via the use of accurate mucosa-supported CAD/CAM drilling guides. The accuracy of the guides is dependent upon a carefully constructed, well extended and well-fitting scanning stent – the CT denture. The CT denture is cloned from a conventional full denture which has itself been proven to fulfil certain key parameters including the achievement of the patient's aesthetic requirements and the establishment of basic occlusal parameters that will subsequently be replicated on the definitive implant-borne prosthesis. These parameters include the establishment of a centric stop position of appropriate vertical dimension and a satisfactory overall occlusal scheme.
Planning stages
The CT denture is manufactured with radiopaque denture teeth (eg SR Ortho Tac, Vivadent) in a standard acrylic base material which incorporates 10% by weight barium sulphate in order that the base will contrast appropriately when scanned under CT. The base and flanges of the CT denture should be fully extended as far as possible to maximise the data outcome that will be attained during the subsequent scanning phase.
With the patient wearing the CT denture and biting into the established position of centric occlusion, data from a single episode CT scan are collected. The CT data are then reformatted for software analysis.
Manipulation of the reformatted CT data set allows the operator to perform a virtual rehearsal of the implant surgery on the computer screen, thereby establishing optimum orientation of implants which are themselves of determined length and diameter. Soft tissue anatomy is represented on the computer model via the detail of the fitting surface of the CT denture. Since both the patient's anatomy and the ideal position of the teeth of the final prosthesis are apparent on the CT data set, appropriate implant positioning for successful surgical and prosthetic outcomes can be tested and discussed before a final treatment plan is determined.13
Once the treatment plan has been finalised, three or more horizontal positioning bone screws must be added to the virtual plan as a means to the rigid fixation of the surgical guide into its appropriate position during the surgical drilling phase. The completed planning files are forwarded to the manufacturing facility together with the CT denture, the opposing arch model, and an occlusal registration index. A working master model of the soft tissue anatomy can be generated stereolithographically from the computer data. This model incorporates detail of implant orientations allowing construction of a surgical stent which itself incorporates accurately orientated drilling guides.
Furthermore, the CT denture can be seated accurately onto the master model to provide an index and occlusal guide for tooth positions during the construction of an accurate temporary immediate load prosthesis which is built around known implant positions and axes. The temporary prosthesis can be held in its appropriate three dimensional relationship to the master model (and subsequently offered up to the mouth) via the use of a detachable clear acrylic carrier/baseplate.
Case report 1: male aged 52 years; maxillary reconstruction
CT denture construction and scanning phases were completed as described above. Virtual planning of the case and virtual implant placement were undertaken using Simplant software (Materialise, Belgium). Various views can be checked simultaneously in the programme during the planning of implant positions (Fig. 1). An example of a rotated 3D view of the completed case is shown in Figure 2. Various layers of data (teeth/baseplate/bone) can be added or removed with the click of a mouse to allow different views of the developing treatment plan.
Accurate seating of the manufactured components onto the soft tissues was confirmed at a try-in stage. Try-in of the provisional immediate load bridge was aided with the use of a detachable clear acrylic base carrier (Smart Implants UK) (Fig. 3). The carrier holds the prosthesis in its correct three dimensional relationship to the oral tissues allowing confirmation of appropriate aesthetic and occlusal outcomes.
At the surgical visit, the patient was prepared and anaesthetised as per routine dental implant therapy and the surgical guide rigidly fixed into position with the aid of the horizontal bone fixation screws. A soft tissue plug was removed at each drilling site with a soft tissue punch. The drilling guides of the stent accommodate a sequence of steel drilling cylinders which themselves incorporate internal cylinders corresponding to the diameters of the twist drills used for the case (Figs 4, 5). Surgical preparation and implant insertion can all be completed via the drilling guides with the stent in situ. Osteotomy depths are readily calculated since the height of the top of the drilling cylinder above the underlying bony crest is known. Figure 6 illustrates the clinical situation following stent removal. Adequate primary stability for immediate loading was confirmed during implant placement. The immediate load temporary bridge was seated over the implants on its removable carrier and temporary cylinders were sequentially cured into place on the supporting implants with pink acrylic (Fig. 7). Views of the fitted prosthesis immediately after surgery are shown in Figures 8 and 9.
Minor adjustments to the occlusion were performed as required and the occlusal access holes filled with a temporary filling material. The patient was given standard post-operative advice and advised to chew only lightly during the first six weeks after surgery to assure a successful osseointegration phase. No antibiotics were prescribed and standard headache analgesics were advised if required. The patient was kept under review and the temporary prosthesis was removed after three months when impressions for the definitive prosthesis were taken. Radiographic appearance is illustrated on the panoral radiograph which was taken four months after surgery (when other work to the lower arch was underway). The panoral view shows the definitive maxillary prosthesis in situ (Fig. 10).
Case report 2: female aged 70 years; mandibular reconstruction
This lady presented complaining of a troublesome lower denture on a very atrophic mandibular ridge. Following discussion of treatment alternatives it was agreed to provide an immediate load bridge based on CT data. In this instance the case was planned to accommodate up to five implants in the inter-foraminal region (Fig. 11). However, since good primary stability was achieved by all implants at other sites at the time of surgery only four implants were deemed necessary (midline implant not used – Fig. 12). Figure 13 shows the relationship between the inferior dental nerve on the left side and the planned implant sites - confirming a good safety margin between the mental foramen and the distal implant. The drilling stent incorporating steel guides to support the drilling cylinders and bone screw locators is shown in Figure 14.
Correct alignment of implants and temporary prosthesis can be confirmed by fitting guide screws onto implants and seating the bridge (supported by its temporary carrier) over these (Fig. 15).
The lower fixed prosthesis seated in its acrylic carrier following the provisional in situ bonding of all four temporary implant cylinders is shown in Figure 16. The final fitting of the prosthesis on the day of surgery is shown in Figure 17. In this case, a panoral view was taken at three weeks (Fig. 18) and impressions for the definitive prosthesis were taken at three months.
Discussion
Today, many prospective implant patients are aware of the possibility of immediate load restorations for the rehabilitation of edentulous arches. Although the procedure described requires a considerable amount of pre-treatment planning and the need to attend for CT scanning, the possibility of avoiding an inconvenient temporisation phase is a strong incentive for many patients. A somewhat similar technique to that described above using a double CT scan process has also been described in the literature,14,15 but this is currently only available to users of a specific implant manufacturer.
Whilst the use of the Simplant platform for the production of a soft-tissue borne stent has been described previously,13 the protocol described in the current report adds the possibility of presenting a pre-manufactured full arch temporary prosthesis to the mouth in a pre-mounted inter-arch position - provided adequate bone volume is identified following analysis of the CT data. This addition to the treatment protocol can greatly simplify the prosthetic procedures which follow on from the surgical stages.
As with any new treatment protocol, there is a significant learning curve associated with its successful execution. A degree of operator experience is necessary to make appropriate judgements about minor modifications to the protocol for the chosen implant system during placement including under-preparation of sites to attain optimal primary stability and the appropriateness of proceeding with the immediate load restoration in any given situation.10
Many of the procedures undertaken during the surgical phase of the current protocol are fairly standard for implant dentistry. Control of primary stability is essential and sites should not be over-prepared since insertion torques in the region of 45NCm are desirable where immediate loading of microtextured implants is proposed.10
Case selection and accuracy in the construction and management of the CT denture are critical factors in this protocol. The accuracy of the subsequently manufactured stents and prosthetic components are a function of the CT denture. Reproducibility of fit onto soft tissues and control of the way in which the fitting processes relate consistently to the underlying hard tissue are clearly key to the technique. The CT denture differs from the conventional denture in that maximum extension of flanges may be critical to ensure the surgical stent can subsequently be secured accurately in its appropriate location as determined in the computer software. For example, over-extension of the baseplate into areas such as the mylohyoid ridge region may not be particularly comfortable for the patient to wear, but this may be one of the few landmarks that allows firm and repeatable seating of a baseplate onto an atrophic ridge. The use of a labial flange in the upper anterior region will generate data on the CT to allow the subsequent placements of horizontal bone fixation screws, whereas the original denture may be gum-fitted and flangeless.
Seating of the surgical guide can also be complicated by other issues at the time of surgery where the use of a local anaesthetic distends and distorts tissues. Regional block anaesthesia may be advantageous in this respect. Asking the patient to bite down onto the CT denture for some minutes prior to subsequent seating of the surgical stent is also a useful procedure in this respect, and with experience it is possible to check appropriate seating via the blanching of supporting soft tissues underneath the clear acrylic of the stent baseplate.
During the drilling stages, the surgical stent may be subject to high levels of torque and occasionally additional support of the stent provided by an assistant may be of benefit. If implants are inserted sequentially through the guide, their carriers or other components may help with further stabilisation of the drilling stent during the preparation of the subsequent implant sites.14
Conclusion
Prefabricated provisional full arch mandibular and maxillary restorations can be predictably provided and immediately loaded using the CAD/CAM based protocol described in this report provided sufficient bone volume is identified via the CT scan Data. Immediate loading of the temporary prosthesis is simplified via the use of an acrylic detachable mounting system. However, these techniques require a certain degree of clinical experience to ensure that the computer generated virtual treatment outcome is reproduced in situ.
References
Branemark P-I, Hansson B O, Adell R et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-Year Period. Scand J Plast Reconstr Surg 1977: 16 (Suppl): 1–132.
Jokstad A, Carr A B . What is the effect on outcomes of time-to-loading of a fixed or removable prosthesis placed on implant(s)? Int J Oral Maxillofac Implants 2007; 22 (Suppl): 19–48.
Szmukler-Moncler S, Salama H, Reingewirtz Y, Dubruille J H . Timing of loading and effect of micromotion on bone-dental implant interface: review of experimental literature. J Biomed Mater Res 1998: 43: 192–203.
Szmulkler-Monkler S, Piatelli A, Favero G A, Dubruille J-H . Considerations preliminary to the application of early and immediate loading protocols in dental implantology. Clin Oral Implants Res 2000; 11: 12–25.
Gapski R, Wang H-L, Mascarenhas P, Lang N P . Critical review of immediate implant loading. Clin Oral Implants Res 2003; 14: 515–527.
Aparicio C, Rangert B, Sennerby L . Immediate/early loading of dental implants: a report from the Sociedad Espanola de Implantes World Congress Meeting in Barcelona, Spain, 2002. Clin Implant Dent Relat Res 2003; 5: 57–60.
Misch C E, Hahn J, Judy K W, Lemons J E, Linkow L I et al. Immediate function concensus conference. Workshop guidelines on immediate loading in implant dentistry. J Oral Implantol 2004; 30: 283–288.
Campelo D, Dominguez C . Flapless implant surgery: a 10-year clinical retrospective analysis. Int J Oral Maxillofac Implants 2002; 17: 271–276.
Roccii A, Martignoni M, Gottlow J . Immediate loading in the maxilla using flapless surgery, implants placed in predetermined positions, and prefabricated provisional restorations: a retrospective 3-year clinical study. Clin Implant Dent Relat Res 2005; 7 (Suppl 1): 29–36.
Cannizzaro G, Leone M, Esposito M . Immediate functional loading of implants placed with flapless surgery in the edentulous maxilla: 1-year follow-up of a single cohort study. Int J Oral Maxillofac Implants 2007: 22: 87–95.
Sarament D, Sukovic P, Clinthorne N . Accuracy of implant placement with a sterolithographic surgical guide. Int J Oral Maxillofac Implants 2003: 18: 571–577.
Virielinck L, Politis C, Schepers S, Pauwels M, Naert I . Image-based planning and clinical validation of zygoma and pterygoid implant placement in patients with severe atrophy using customised drill guides. Preliminary results from a prospective follow-up study. Int J Oral Maxillofac Surg 2003: 32: 7–14.
Rosenfeld A L, Mandelaris G A, Tardieu P B . Prosthetically directed implant placement using computer software to ensure precise placement and predictable prosthetic outcomes. Part 3: Stereolithographic drilling guides that do not require bone exposure and the immediate delivery of teeth. Int J Periodontics Restorative Dent 2006: 26: 493–499.
Balshi S F, Glenn J W, Balshi T J . Surgical planning and prosthesis construction using computed tomography, CAD/CAM technology, and the Internet for immediate loading of dental implants. J Esthet Restor Dent 2006: 18: 312–325.
Becker W, Goldstein M, Becker B E, Sennerby L . Minimally invasive flapless implant surgery: a prospective multicentre study. Clin Implant Dent Relat Res 2005: 7 (Suppl 1): S111–S120.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Allum, S. Immediately loaded full-arch provisional implant restorations using CAD/CAM and guided placement: maxillary and mandibular case reports. Br Dent J 204, 377–381 (2008). https://doi.org/10.1038/sj.bdj.2008.252
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2008.252