Key Points
-
Existing research suggests that 30-50% of patients who are prescribed an RPD never or only occasionally wear the prosthesis.
-
This study has identified key factors that influence professional provision and patient use of RPDs.
-
For patients, wearing an RPD is not simply a matter of aesthetics, but of avoiding the social stigma associated with tooth loss.
Abstract
Objective To identify factors that influence Removable Partial Denture (RPD) provision, and patient use of RPDs in the UK.
Design Exploratory qualitative interview study.
Subjects and methods Subjects There were two sample groups. A purposive sample of 16 male and female dentists was categorised in terms of level of RPD provision, experience, and practice characteristics. A purposive sample of 17 male and female partially dentate patients was categorised in terms of RPD use and demographic characteristics. Data collection Semi-structured in-depth interviews.
Results For dentists, RPD provision was indicated by patient demand and physical function of the remaining teeth, but was mediated by NHS fee structures and professional satisfaction. For patients, RPD use was influenced by the trade-off between improved appearance and the unpalatable presence of an RPD in their mouth. The location of the gap(s) was important, but other issues were relevant such as ability to 'manage' without the RPD.
Conclusion When defining 'need' for an RPD, dentists focused on physical function of the teeth whereas patients focused on social meanings of the mouth. These differing priorities may improve understandings of patient non-compliance in RPD use. Further research on the relationship between denture use and social identity could be beneficial.
Similar content being viewed by others
Introduction
The UK is currently characterised by an ageing population,1,2 in which both the number and proportion of the population who are partially dentate is increasing.3 Limited public funding for oral healthcare and the political popularity of evidence-based dentistry mean that there is a need to re-evaluate the management of the partially dentate adult to meet demands for more cost-efficient health care provision. Fifteen million British adults have some natural teeth but have been provided with RPDs or bridges to replace those that are missing.3 RPDs are the simplest and the most common method of replacing missing teeth, and they are provided for approximately 30% of adults of middle age and older3 at a cost to the NHS of some £50 million annually.4 Clearly RPDs are a popular treatment option, but despite the intended benefit to appearance and function they appear to be accepted poorly by patients themselves. Some 30-50% of patients never or only occasionally wear their denture.5,6 This represents a significant discrepancy between professionally assessed need and patient expressed demand and, together with their potential to generate an additional long-term treatment need,7,10 a considerable potential waste of resources within the NHS.
The reasons for this discrepancy between clinical intent and treatment outcome are unclear but may reflect the attitudes and expectations of patients, the clinical knowledge and technique of dentists, and/or administrative and financial restrictions. The present study aimed to explore this discrepancy by identifying factors that influence practitioners' decisions around provision of RPDs, and factors that influence patients' decisions around whether to wear them. A better understanding of these factors could inform practical guidelines to target RPD treatment more effectively.
Method
The qualitative study design adopted an exploratory, descriptive approach to data collection, and a generative thematic approach to data analysis, reflecting the aim of gaining a deeper understanding of practitioner and patient attitudes toward RPDs.
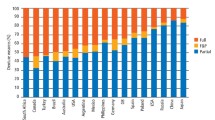
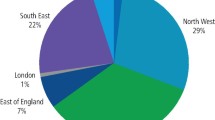
Using the payment database for dental services under the UK's NHS, the Dental Practice Board (DPB) undertook a secondary analysis of its data to our prescription for 2000-2001, relating the pattern of RPD provision to characteristics of practitioner and practice. Based on the findings of this secondary analysis, practitioner samples for interview were identified representing different frequency of RPD prescription (high, medium, low) and experience (time since qualification). We adopted a purposive sampling strategy to identify dentists working in the north and south of England with a variety of practice characteristics such as location in affluent and deprived areas, population density and dentist:population ratio. Patient samples were drawn by the DPB through the patient lists of the practitioner interviewees and with the practitioner's agreement. These patients were at least 45 years old and were sent a validated, self-completion tooth counting questionnaire relating to their dental status.11 Responses provided reliable information about the number and distribution of remaining natural teeth, partial denture provision and denture wearing habits. This information was used to select a purposive sample of patients representing variation in the number and distribution of missing teeth; denture use; denture design; sex; and age (between 52 and 82 years). The participants were selected to represent diversity among patients and dentists. The purposive sampling process did not produce statistically representative samples; rather, it generated sample groups that included the range of opinion that exists within the broader population of dentists, and the broader population of partially dentate patients.
Semi-structured, in-depth interviews were conducted with practitioners and partially dentate patients. The interviews were based on a pre-developed topic guide, but participants were actively encouraged to raise and discuss further issues where relevant. As a result, the topic guide was amended throughout the study, to highlight emerging areas of interest, and to indicate when data saturation had occurred (ie when new themes of interest were no longer apparent. For the dentist sample, an initial purposive sample of 44 yielded 23 potential interviewees; data saturation occurred at n = 16 for practitioners. For the patient sample, the participating dentists were asked (via the DPB) to identify eight suitable patients; this process elicited 54 returned tooth counting questionnaires, 40 of which indicated willingness to be interviewed; data saturation occurred at n = 17 for patients. The interviews were transcribed verbatim, and then analysed using a generative thematic approach, aided by qualitative analysis software packages (Atlas.ti and N.Vivo). The interviews were analysed by RG (dentist data) and SM (patient data) to identify emerging themes; one in three interviews were analysed independently by SB to provide inter-rater reliability for the themes identified. The verified themes were used to code each transcript, identifying relevant statements made by participants under the thematic headings. The analyses of patient and dentist data were then integrated by the research team, working within the framework of thematic headings.
Results
Factors that influence professionally assessed need for an RPD
Dentists' decisions about whether or not to provide an RPD to replace missing teeth were usually initiated by the patient. The dentists understood the importance of dental appearance to patients, and recognised that patients were more likely to demand a new denture or replacement of an old denture, if an anterior tooth/teeth and/or an upper tooth/teeth was missing. If a patient presented with missing posterior, lower teeth, dentists would tend to recommend an RPD only where physical function would be affected, or if the patient requested one. Decisions between an RPD and fixed bridgework were influenced primarily by oral health status and affordability. Dentists were much more likely to recommend bridges for patients with 'clean' mouths (ie good oral hygiene), and RPDs for 'dirty' mouths. In this sense, patient compliance had an influence on dentists' decision making processes. The status of the patients' mouth was also important for the type of RPD provided. For example, some dentists conceptualised 'dirty mouths' as in a downward spiral of decay; the likelihood of further tooth loss often prompted the provision of an acrylic resin based RPD (rather than a cobalt-chromium based denture), because the prosthesis could be altered easily should further tooth loss occur. This rationale was also evident in less affluent areas where dentists were more likely to provide acrylic resin based RPDs than cobalt-chromium based RPDs, because they felt that they were more affordable for patients:
'...on a number of occasions I've advised a chrome and they just can't afford it so they end up with an acrylic.'
'...you could pay a huge amount of money for a chrome and then can't get used to it, pay a little bit for an acrylic and can't get used to it, well [the patients] haven't lost as much [money]'. (ID Dent 9688.)
Factors that influence professional provision of RPDs
A dominant theme emerged related to issues of cost effective work strategies in NHS dentistry. Dentists' experience with the different treatments for the partially dentate was important, but for cost effective reasons. For example, those with less experience of providing cobalt-chromium based RPDs were generally less willing to provide this type of prosthesis; however, more experienced dentists also echoed their concerns. Cobalt-chromium based RPDs were seen as harder to get right first time, and more expensive to get wrong. This was particularly apparent for those who were conscious of the NHS fee structure for each treatment they provided, such as staff affiliated to a practice, rather than partner/s in a practice. The profit margin (which may absorb any additional costs in provision, such as adjustments for an ill fitting RPD) was seen as negligible or non existent. Dentists who were more comfortable with providing RPDs tended to be more experienced, to calculate their cost-effectiveness per month or per year (rather than per intervention), and to have good relationships with the technicians at a local dental laboratory or have a laboratory on-site.
An additional theme emerged around professional satisfaction and quality of workmanship with concerns about the ability to provide a 'good' RPD that extended beyond issues of cost effectiveness, even in private practice. In general, dentists' opinions of the RPD were negative:
'...the dentures are a last resort, there is no doubt, no matter how well made they are.' (ID Dent 2047.)
'Even a good RPD was seen as an inherently bad thing, because many patients don't like them, and because they can cause damage to the remaining teeth.'
Factors that influence patients' use of their RPD
The partially dentate patients with an RPD were categorised into three groups: regular users, occasional users and non-users. For regular and occasional users alike, a dominant influence on RPD use is the aesthetic improvement an RPD offers. Similar to the dentists' perceptions, patients felt more motivated to wear their RPD if it filled an upper, anterior gap, because they felt the gap would be obvious to others. Related factors were also influential, for example those in regular contact with others (eg at work) were more motivated to wear their RPD. RPDs were also perceived as helping to support the shape of the face, and for smiling. However, some patients also stated that they felt 'vain' to care about their appearance, and this demonstrates the taken-for-granted nature of a most important and fundamental aspect of human social communication:
'[when wearing the RPD]... you are a little bit more confident, you smile more...when you've got teeth missing you tend not to smile so you walk around and you look as if you are miserable all the time.' (ID Patient 1006.)
Similarly, those who felt they had 'ugly' natural teeth, found that the aesthetic improvement of an RPD, compared to their natural teeth, was a motivational factor for wearing them. However, the appearance of an RPD was also a reason for concern; those wearing their RPD talked about the aesthetic problems such as the pink plastic on acrylic resin based dentures being the wrong colour, or the metal on a cobalt-chromium based denture being visible when they smiled.
Similar to the dentists, the patients recognised physical function as an important issue but, for most patients, this was of secondary importance to appearance. Some made very positive comments about their improved physical function; but many comments indicated a negative impact. Patients described a number of problems related to eating, such as lack of sensation of food in the mouth, the inconvenience of having to apply denture fixative regularly and rinsing dentures after eating. For example:
'I just don't like the feel of having a mouth full of plastic...if I eat I prefer to take them out because with the palate on the top I can't taste the food properly...' (ID PatientH1.)
Other negative impacts on physical function were the instability of the denture in the mouth (such as 'flipping'), problems with speech, and the feeling of having something in the mouth — this could include gagging, pain, soreness and bulkiness. These factors outweighed any potential aesthetic benefit for those who did not use or only occasionally used their denture.
Patients made relatively sophisticated cost-benefit calculations based on a number of factors when deciding whether or not to use their RPD. For example, cobalt-chromium based dentures are generally viewed more positively than acrylic resin based dentures, because they are perceived to be a tighter fit in the mouth, less likely to fall out, and less likely to break. Similarly, RPDs were generally viewed more positively than no teeth, especially for those with anterior teeth missing. Upper RPDs were seen as better than lowers, because they were felt to be more stable and less likely to move about in the mouth. But the key issue here relates to comparison: if patients felt they could 'manage' without their RPD, ie their RPD offered relatively little improvement on their partially dentate state, then motivation to wear the RPD tended to be lower. However, there are differences amongst patients about what counts as 'managing', and also between patients and practitioners about whether people can 'manage'.
Discussion
When considering the cost effectiveness of dental treatment, the key factors are those that influence dentists' decision making, and those that influence how patients use dental services. These issues are not new; there is some research evidence available to inform discussion in these areas. For example, McGrath and Bedi12 have demonstrated that social class, gender and age are all significant factors for whether or not patients use dental services to obtain dentures. In the US, research indicates that for dentists deciding between providing a fixed bridge or a removable partial denture, technical concerns took priority over patient concerns.13 For patients, psychosocial factors related to the interaction between clinician and patient have been identified as important for patient satisfaction and therefore compliance with treatment.14,15 Several different topics have been researched in attempts to understand patients' dissatisfaction with dentures, such as patients' psychological characteristics,16 functional issues such as eating17 or social factors.12 While these studies have been important for understanding some aspects of professional decision making and patient compliance, an in-depth understanding of how dentists and patients perceive 'the denture' (whether partial or full) remains elusive. This study focused on such perceptions of RPDs, and how those perceptions can help us to understand the discrepancy between professionally assessed need expressed by provision, and patient defined need expressed through (non) use of their RPD.
Some of the patients interviewed were very happy with their RPD, and some dentists felt that the RPD was a well received quality product and service. It is important to note that the RPD can be considered a good thing in its own right. However, for many patients and dentists, the RPD is a 'last resort'. But for a more effective use of resources, the important aspect is why RPDs are provided for patients who do not wear them. When asked what could be done to reduce the discrepancy between professionally assessed need and patient expressed need, the dentists found it difficult to comment on possible solutions.
The principal suggestions were around structural factors such as improving the NHS fee structure to enable the provision of better quality RPDs, or around improved patient selection. Tackling the fee structures for RPDs might address the profit risk that dentists currently face in providing this treatment option, but there is an additional factor that helps to explain why many patients do not regularly wear their RPD. For the dentist, there appeared to be an emphasis on the need for adequate physical function of the teeth, raising issues such as tooth wear, ability to chew food, and the load on the remaining natural teeth. However, this conceptualisation of need was not necessarily shared by patients. Patients' understandings of physical function centred on the mouth rather than the teeth, and the RPD can actually impede the physical function of the mouth in terms of eating (eg tasting, feeling the food, emptying the mouth of food). Many activities associated with RPD use, such as the use of denture fixative and the need for regular rinsing throughout the day, are inconvenient and disruptive to their social persona. For many patients, the perceived benefits of RPD use were simply not sufficient to tolerate the presence of the denture in the mouth.
Nevertheless, physical function remained secondary to appearance as a motivation for RPD use amongst patients. But it may be problematic to characterise patients' concerns with appearance as merely 'aesthetic'. This is an unfortunate term because of the connotations that cosmetic/aesthetic health care interventions seem to attract in the wider social sphere, such as vanity, and are therefore perceived as less legitimate interventions. Patients' understandings of appearance suggested a rather different interpretation of factors normally understood as 'aesthetic'. For patients, the mouth performed essential social functions when interacting with others (such as smiling and talking), and concerns about social communication and social identity often took precedence over the physical function of the teeth. For example, one patient described feelings about the need for an RPD:
'...if you smile and you wear a denture all the time...the next time your denture is in for repair say and you smile they go, “what happened to all your teeth?” You know...it's a thing because you are silly getting all your teeth out when you are younger and...you think “What an idiot to do that, if I had just looked after my teeth” or even had them repaired instead...' (Patient ID 1006.)
Although the patients talked about their feelings that a gap would look bad, this quote suggests that these feelings may not be just about how they look, but also how a gap reflects on their social identity. The issue was not so much one of looking pretty, or being vain, but about avoiding social stigma;18 the RPD allowed the partially dentate individuals to 'pass as normal' in a society that has ever increasing expectations of what constitutes a normal dental appearance. RPDs therefore had a significant social function that went beyond what we term aesthetics: it allowed the patients to participate (as normal) in everyday, taken-for-granted micro-social interactions such as smiling, and therefore worked against the social exclusion that those with gaps appear to face. This cannot be dismissed as mere vanity, but rather should be seen as a key contributing factor to how individuals presented themselves to others and formed their social identity.
In conclusion, the study has demonstrated that many factors influence the discrepancy between professionally assessed need for RPDs and patient expressed need. Although dentists are primarily led by patient demand and physical function of the teeth, the perceived need to work cost-effectively within the NHS fee structure and notions of professional satisfaction are also important in their decision making process. For patients, two key issues have been identified. First, physical function is an issue of not just the teeth, but the entire mouth. From this perspective, RPDs may be more hindrance than help for physical function. Second, the motivation for RPD use often centres on patients' concerns about appearance. The analysis suggests that it may be more appropriate to conceptualise these concerns as issues of patients' social function and social identity, rather than vanity and aesthetics. Additional research into the relationship between dental care, denture use and social identity could potentially improve further our understandings of patient non-compliance.
References
Hargreaves S . Burden of ageing population may be greater than anticipated. Lancet 2000; 355: 2146.
Watson R . European countries face similar problems of demographic ageing and higher patient expectations. Br Med J 2001; 323: 1388.
Kelly M, Steele J, Nuttal N et al. Adult dental health survey: Oral health in the United Kingdom 1998. London: the Stationary Office, 2000.
Board DP . Digest of statistics 2002-2003. Eastbourne: Dental Practice Board, 2003.
Jepson NJA, Thomason JM, Steele JG . The influence of denture design on patient acceptance of partial dentures. Br Dent J 1995; 178: 296–300.
Steele JG, Walls AW, Ayatollahi SM, Murray JJ . Major clinical findings from a dental survey of elderly people in three different English communities. Br Dent J 1996; 180: 17–23.
Budtz-Jorgensen E, Isidor F . A 5-year longitudinal study of cantilevered fixed partial dentures compared with removable partial dentures in a geriatric population. J Prosthet Dent 1990; 64: 42–47.
Drake CW, Beck JD . The oral status of elderly removable partial denture wearers. J Oral Rehabil 1993; 20: 53–60.
Steele JG, Walls AW, Murray JJ . Partial dentures as an independent indicator of root caries risk in a group of older adults. Gerodontology 1997; 14: 67–74.
Jepson NJ, Moynihan PJ, Kelly PJ et al. Caries incidence following restoration of shortened lower dental arches in a randomized controlled trial. Br Dent J 2001; 191: 140–144.
Allen PF, Jepson NJA, Burke FM . Development and evaluation of a self-report tooth counting questionnaire. Int Dent J 2005. 55: 13–16.
McGrath C, Bedi R . Severe tooth loss among UK adults — who goes for oral rehabilitation? J Oral Rehabil 2002; 29: 240–244.
Grembowski D, Milgrom P, Fiset L . Factors influencing dental decision making. J Public Health Dent 1988; 48: 159–167.
Redford M, Gift HC . Dentist-patient interactions in treatment decision-making: a qualitative study. J Dent Educ 1997; 61: 16–21.
Gale EN, Carlsson SG, Eriksson A, Jontell M . Effect of dentists' behaviour on patients' attitudes. J Am Dent Assoc 1984; 109: 444–446.
Moltzer G, Van der Meulen MJ, Verheij H . Psychological characteristics of dissatisfied denture patients. Comm Dent Oral Epidemiol 1996; 24: 52–55.
Obrez A, Grussing PG . Opinions and feelings on eating with complete dentures: a qualitative inquiry. Spec Care Dentist 1999; 19: 225–229.
Scambler G . Deviance, sick role and stigma. In Scamber G (Ed). Sociology as applied to medicine. 5th Ed. Edinburgh: Saunders and Elsevier, 2004.
Acknowledgements
This study was funded by the NHS Executive Regional R&D with assistance from the Dental Practice Board for England and Wales. Many thanks to the dentists and patients who participated in the study, and also to Dr Julie Birch for assistance in project development.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Graham, R., Mihaylov, S., Jepson, N. et al. Determining 'need' for a Removable Partial Denture: a qualitative study of factors that influence dentist provision and patient use. Br Dent J 200, 155–158 (2006). https://doi.org/10.1038/sj.bdj.4813193
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4813193
This article is cited by
-
Top tips for removable partial dentures: Part 1 - fundamentals of success
British Dental Journal (2023)
-
Factors affecting dental self-confidence and satisfaction with dental appearance among adolescents in Saudi Arabia: a cross sectional study
BMC Oral Health (2021)
-
Social determinants of denture/bridge use: Japan gerontological evaluation study project cross-sectional study in older Japanese
BMC Oral Health (2014)
-
The psychosocial impacts of implantation on the dental aesthetics of missing anterior teeth patients
British Dental Journal (2012)
-
Risk management in clinical practice. Part 6b. Identifying and avoiding medico-legal risks in removable dentures
British Dental Journal (2010)