Key Points
-
Orthodontic treatment can often assist the restorative treatment of patients with congenital hypodontia
-
Orthodontics can help with problems such as unfavourable space distribution, tooth alignment and deep overbite
-
The principles of orthodontic management of hypodontia are discussed
-
Stability of the orthodontic result can be a problem and retention needs careful management
Key Points
The Interdisciplinary management of hypodontia:
-
1
Paediatric dentistry
-
2
Restorative dentistry
-
3
Orthodontics
-
4
Oral surgery
-
5
The relationship between an interdisciplinary team and the general dental practitioner
Abstract
Orthodontic treatment can greatly facilitate any restorative treatment or sometimes even eliminate the need for it. There are several issues that commonly arise in the orthodontic management of patients with hypodontia. These include: space management; uprighting and aligning teeth; and management of deep overbite and retention and stability. The following paper discusses these aspects of orthodontic management.
Similar content being viewed by others
Main
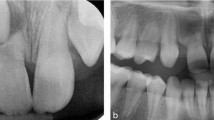
The restorative management of spacing which results from congenital absence of teeth is often hampered by unfavourable positions of the teeth that are present and the result can therefore be compromised (Fig. 1). In many cases of hypodontia, orthodontic treatment can greatly facilitate any restorative treatment, or sometimes even eliminate the need for it.
Patients with hypodontia often present with a number of associated traits that should be considered prior to determining the definitive orthodontic treatment plan.1 In most patients there is a tendency to a reduced mandibular planes angle, associated with a reduced lower facial height and lip protrusion, which becomes more marked with increasing severity of the hypodontia.2 Intra-orally, retroclined lower incisors, increased interincisal angle and over-eruption of the lower incisors also frequently contribute to an increased overbite. There is often a fairly flat palatal vault which results in reduced anchorage capacity of upper removable appliances. Increased rotations of teeth, both adjacent and non-adjacent to missing permanent teeth3 and an increased prevalence of ectopic maxillary canine teeth4 may also complicate management.
The range of problems that can present in patients with hypodontia is enormous and each case should be considered on its own merits and discussed fully within the interdisciplinary team. Patients' concerns and attitude to treatment can also vary hugely and, as always when formulating a treatment plan, these must be taken fully into consideration. However, there are several issues that commonly arise in the orthodontic management of patients with hypodontia. These include:
-
Space management
-
Uprighting and aligning teeth
-
Management of deep overbite
-
Retention and stability.
Space management
The decision on whether to open or close space depends upon:
-
The age of the patient
-
The severity of the hypodontia.
-
The degree of inherent crowding.
Age of the patient
In young patients, the possibility should be considered of carrying out interceptive measures to simplify later orthodontic treatment. Where there is mild crowding, selective extraction of primary teeth in the early mixed dentition may be of advantage to allow some favourable, spontaneous tooth movement. Joondeph5 found that extracting second primary molars at the appropriate time often led to some relief of anterior crowding and spontaneous space closure. Similarly, where upper lateral incisors are absent in an otherwise crowded arch, extraction of the primary lateral incisors may encourage mesial migration of permanent canines. This results in a more adjacent position between the permanent central incisor and canine as the latter erupts. However, as discussed below the indication for these early extractions depends very much on the degree of crowding present.
Space management Whether to open or close space depends on the number of teeth missing, the degree of crowding and the type of malocclusion. Judicious extraction of primary teeth can sometimes help encourage more favourable eruption of the permanent teeth
Patients with absent or diminutive permanent lateral incisor teeth have been shown to have an increased prevalence of ectopic maxillary canines.6 Where a canine appears to be ectopic, extraction of its primary predecessor should be considered as this has been shown to lead to an improvement in canine position in the majority of cases7 provided that the degree of displacement of the canine is not too severe.8
The ideal time for definitive orthodontic treatment of patients with hypodontia is very often early adolescence, when most of those permanent teeth that have developed are erupting. At this stage the greater part of facial growth has taken place, but such growth as does remain facilitates overbite reduction and spontaneous tooth movements.
Space closure and improvement in alignment are very often incomplete following these interceptive measures, and patients and parents should be warned that further restorative or orthodontic intervention may well be necessary.
At the other end of the age range, there has been a steady increase in adults seeking orthodontic treatments. The management of adults is often complicated by the effects of caries and periodontal disease, and by the lack of facial growth potential which reduces the ability to adapt to occlusal disturbance. The ideal goals of orthodontics — aesthetics, function and stability - are not always achievable and a degree of compromise may have to be accepted.9
Severity of the hypodontia
The presentation of hypodontia may vary from a single tooth to multiple missing teeth. As the number of absent teeth increases, the tendency for permanent tooth displacement increases, the overbite tends to become more severe1,2 and overall the treatment need for such cases tends to increase.10 The treatment option of space closure becomes unrealistic and instead orthodontic treatment aims to provide space distribution and tooth positions which are optimal to facilitate restoration of the spaces.11
Degree of crowding
No crowding. Where there is no crowding and the extent of the hypodontia is limited, it is often best not to close the space but either restore it prosthetically or leave the primary tooth in situ if its condition is satisfactory. The option of retaining a good primary tooth should always be considered, and is particularly appropriate where a permanent premolar is absent from an otherwise uncrowded arch. Preservation of the primary tooth has the added benefit of preserving alveolar bone which would be invaluable if an implant were to be placed at a later stage.
Moderate crowding. In a crowded arch, the degree of crowding should be assessed as if all permanent teeth were present, and then any congenitally absent permanent teeth considered as 'extractions' to relieve the crowding. However, where the crowding is mild or moderate, extraction of the retained primary tooth may well provide too much space and it is in these cases that early extraction of the primary tooth may be of help. Fig. 2 shows diagrammatically such a situation where the crowding is mild and a lower second premolar is absent. The extraction of the lower E could easily provide too much space, but removing it early has two beneficial effects:
-
It allows the lower 6 to drift mesially and take up some of the excess space, thereby simplifying subsequent orthodontic space closure,
-
It often allows some spontaneous improvement in the alignment of the anterior teeth.
Severe crowding. Where the orthodontic treatment is going to need a lot of space and a second premolar is absent, it is prudent to delay the extraction, keeping the primary molar as a natural space maintainer until enough of the permanent teeth have erupted to allow orthodontic treatment to begin. In cases where space is at a premium and a primary second molar has to be lost, for example because of caries or severe infra-occlusion, provision of a space maintainer should be considered.
Space Closure — advantages and disadvantages
Where space closure is possible in mild hypodontia cases, the need for a prosthesis, with its associated long-term maintenance, is avoided. In hypodontia cases however, space closure may be slower than normal and it may not be possible to close the space completely. Possible explanations include reduced alveolar bone mass, generally smaller teeth and anchor units which are weaker because of the reduced size and number of teeth.11
Attempts to close substantial amounts of space will tend to retract the anterior teeth, which may or may not be desirable. Space closure in the upper arch may well assist with reduction of an increased overjet, but unwanted retraction of the anterior teeth can affect the incisor relationship adversely. For example, in a Class 1 occlusion, where there is no scope to use some of the space to correct the incisor relationship, attempts to close space in one arch could easily spoil the incisor relationship by over-retracting incisors. The use of protraction headgear to the upper arch may be necessary where the overjet is tenuous. There may also be concerns about aesthetics and function where space is closed in the anterior part of the upper arch.12 Closure of the space from a missing upper lateral incisor results in the canine tooth being moved mesially into contact with the central incisor, and the first premolar being positioned in what was the canine position.
The resulting appearance varies enormously and often is satisfactory, but potentially this situation does have some disadvantages. Firstly, the canine is more pointed, wider and darker than the lateral incisor it replaces. This appearance can be improved by selective grinding of the cusp tip, by the addition of composite material, and by bleaching13 without any adverse long term reactions clinically or radiographically.14,15 Secondly, the important question of symmetry and centre lines must be considered. Where there is crowding or an increased overjet, extraction of the contralateral lateral incisor may help preserve symmetry and keep the dental midline correct within the face. Fig. 3 illustrates a satisfactory appearance following closure of both upper lateral incisor spaces.
Finally, placing the first premolar in what was the canine position means that a canine protected occlusion is not feasible and lateral occlusal forces are applied to the smaller and thinner roots of the first premolar.16 Although some workers fear this may lead to periodontal breakdown, long term periodontal studies suggest that space closure is preferable to orthodontic space opening.17
Space opening and redistribution — advantages and disadvantages
Space opening or re-creation is usually the best option where there is little or no crowding, especially where orthodontic treatment does not need to make use of the space and attempts to close it could result in the undesirable effects described above. Indeed, space opening is considered by some authors to be advantageous both functionally and occlusally, favouring good intercuspation in the buccal segments,18 but its major disadvantage is that it commits the patient to a permanent prosthesis.
Interdisciplinary planning Decisions about space management must be made by the interdisciplinary team, taking into account the risks and benefits of all options
The space required for the prosthesis is usually determined by two factors. The first is the aesthetics: for example an upper lateral incisor should be two thirds of the width of the upper central incisor.19 The second factor is the occlusion. Ideally, at the end of treatment there should be a good Class I occlusion, with coincident centre lines and optimal overbite and overjet. However this may be difficult in hypodontia cases because of unusual tooth form and the anchorage problems associated with reduced numbers of teeth, which are often of smaller size. Fig. 4 shows a patient with absent UR2(12) and diminutive UL2(22) treated with a fixed appliance to recreate the space to allow replacement of UR2(12) and enlargement of UL2(22).
Congenital absence of UR2 (12) and diminutive UL2 (22) in an uncrowded, Class I occlusion; 4b) Upper fixed appliance to reopen UR2 (12) space, showing also the Class I buccal segment interdigitation; 4c) Upper removable retainer with spurs to ensure maintenance of the mesio-distal tooth movements and an anterior bite plane to reduce the overbite and facilitate the placement of the bridge; and 4d) The final acid etch retained bridge at UR2 (12) and composite veneer at UL2 (22)
Where the hypodontia is extensive, or early loss of retained primary teeth has resulted in alveolar atrophy, complete space closure will not be possible. In these situations the final distribution of teeth and spaces must be agreed by the interdisciplinary team at the planning stage, so that tooth positions can be optimised for the definitive restoration of the remaining space.
If implants or autogenous transplants are being considered, not only must adequate space be created for replacement of the tooth crown but the roots of adjacent teeth should be parallel or slightly divergent to give adequate space for implant placement. The position of the roots of the adjacent teeth should therefore be evaluated radiographically before the appliances are removed.18
Uprighting and aligning teeth
As well as closing space or optimising its distribution in the arch, orthodontic treatment can also improve the alignment of the teeth to facilitate the provision of prostheses.
Many of these procedures, rather than being described as definitive orthodontic treatment, fit more closely into the adjunctive category with limited orthodontic goals. Common examples are uprighting tilted teeth, correction of rotated teeth and forced tooth eruption (extrusion) to improve crown length prior to restoration.Uprighting molars can aid preparation of abutment teeth, improve distribution of occlusal forces and re-establish marginal ridge relations.20 Important considerations prior to uprighting include:
-
Is space required distal to the tooth to be uprighted?
-
Should the tooth be uprighted by crown movement, root movement or a combination of both?
-
Should extrusion of the tooth be permitted with the uprighting procedure?
-
Does the tooth at the other side of the space require any tooth movement?
Appliance selection
The appliance selected for space management depends upon the type of tooth movement required. Active removable appliances produce mainly tipping movements and, although indicated occasionally (Fig. 5), their application for space creation or closure is very limited. However, as will be discussed below, removable appliances are very useful for three specific purposes:
-
For overbite reduction,
-
For space maintenance in the upper arch,
-
As retainers.
Appliance selection Fixed appliances are otherwise almost always the appliance of choice as they allow greater control of tooth movement. Patients with hypodontia do, however, present particular difficulties for fixed appliances. Altered tooth morphology, with altered enamel structure and microdontia, adversely affects both the etch patterns and the fit of the bracket base to the tooth surface when bonding with resin cements. Resin-modified glass-ionomer bonding cements, which allow both chemical and mechanical adhesion even in the presence of moisture, may be beneficial in these situations. Long spans of unsupported arch wire can also be a problem, particularly when using flexible aligning wires which are easily distorted and displaced out of molar tubes, resulting in soft tissue trauma. The recently introduced thermally active nickel titanium wires have an advantage in this respect, in that heavy, rectangular wires may be placed even in the early stages of alignment and are large enough to be adequately robust while at the same time producing a low, constant force.
Fixed orthodontic appliances have been shown to lead to difficulties with oral hygiene21 and predispose to plaque accumulation22 with consequent demineralisation, especially on teeth with small clinical crowns.23 Patients with hypodontia, with their tendency to microdontia, may be more at risk of plaque accumulation between bracket and gingiva caused by their close proximity, and may need specific oral hygiene advice and preventive measures to avoid these undesirable sequelae.
Patients with moderate to severe hypodontia have also been shown to be more susceptible to apical root resorption. Whether this is because of their unusual root morphology or to the extensive tooth movements required is unknown, but it is likely24 that both contribute. Where resorption is thought to be a potential hazard, anterior intra-oral radiographs should be taken before treatment to determine root morphology, with a follow up radiograph after 6—9 months of active treatment to try to identify problems early in treatment.25
Overbite
An increased overbite is often marked in patients with hypodontia, especially where the degree of hypodontia is significant.1,2 Reduction of the overbite must be taken into account in the overall treatment plan when restoration of spaces is required anteriorly or when overjet reduction is required. In hypodontia cases, the deep overbite often results in an opposing tooth occupying the space to be restored, so preventing provision of a prosthesis (Fig. 1). Reduction of overbite is best carried out in growing patients,26 when dentoalveolar and skeletal adaptation is at its most accommodating. One of the most effective methods of overbite reduction in growing patients is to use an upper removable appliance with an anterior bite plane. This allows eruption of the posterior segments whilst restraining eruption of the lower anterior teeth. Where an upper removable appliance is being used for active tooth movement it can incorporate a bite plane, but hypodontia cases nearly always require fixed appliances. Unfortunately, overbite reduction with these appliances can be difficult where the number of permanent teeth is significantly reduced. In this situation, management of the overbite can often be left until the end of fixed appliance treatment and then dealt with by incorporating a bite plane into the retainer (Fig. 4c). In general, slight over correction is favoured due to its relapse potential.
Functional appliances are particularly useful for reducing an increased overjet in a patient who is growing. They can be very useful even where the degree of hypodontia is severe, as it is often possible to construct a functional appliance even if only a few teeth are present, and many designs of functional appliance are also effective for controlling the overbite. Their effects are largely dentoalveolar, with incisor tipping and molar eruption.27
In adults, the management of overbite is much more difficult. Removable appliances with bite planes are not very well tolerated and Dahl et al.28 described an appliance which is essentially a small anterior bite plane made of cobalt-chromium, with minimal bulk to make it better tolerated. These appliances can be either removable or cemented to the anterior teeth, and are now often made of acrylic rather than cast metal. Small amounts of inter-occlusal space may be created in this way to facilitate restorative work and, fortunately, with modern restorative materials and techniques the space required to accommodate the definitive restorations is usually quite slight, with 0.5–0.75 mm of space being adequate.29,30
Where significant overbite reduction is required in an adult patient, intrusion mechanics with fixed appliances are usually the favoured option,31 although the ability to truly intrude labial segments is probably limited.32 Correction of skeletal discrepancies in an adult patient will require orthognathic surgery.
Retention and stability
Retention is that phase of orthodontic treatment during which a passive appliance is used to counteract relapse and thus maintain the changes achieved by orthodontic treatment. Many of the orthodontic movements required in the orthodontic treatment of hypodontia patients are inherently unstable and are prone to some extent to relapse unless retention is maintained long-term. Examples of these unstable changes include:
-
Space closure in the absence of crowding
-
Space redistribution and creation
-
Correction of rotations
-
Overbite reduction in the absence of a stable occlusal stop.
Space closure, particularly when associated with either minimal or no crowding, is particularly prone to relapse, as is closure of an upper midline diastema. The options for retention are either a removable retainer or, in the anterior part of the mouth, a semi-permanent bonded retainer on the palatal or lingual surface. Bonded retainers are usually made of flexible orthodontic wire bonded with a light-cured composite, and can be successful where they do not interfere with the occlusion. Where the occlusion is a problem, such as in the upper anterior region, a cast metal Maryland design can be considered but the clinical success of these is very variable, the chances of failure increasing as more teeth are involved in the retainer. In the early stages of retention, the bonded retainer may be supplemented with a removable retainer for full time wear for 6 months followed by night time wear for at least a further 6 months. This allows not only the anterior but also the posterior occlusion to be adequately retained and also acts as a safe-guard should the bonded retainer become detached during the first year. If a bonded retainer is unsuccessful, long term part-time wear of a removable retainer may be the only solution. Unfortunately, wearing a removable prosthesis increases plaque retention33 and compliance is likely to be less.34
Where space has been opened or redistributed it must be retained for a period prior to provision of the definitive restoration. Single tooth spaces may be retained by an immediate adhesive bridge,35 but much more commonly a removable retainer is fitted which carries acrylic teeth and wire stops (Fig. 4c). The wire stops are essential to prevent loss of space should the acrylic teeth become detached. The retainer can also conveniently include a flat anterior bite plane to encourage further overbite reduction and increase the inter-occlusal space to facilitate the provision of the definitive restoration. This type of appliance must be worn full time for a minimum of 6 months, allowing dentoalveolar remodelling in the saddle areas prior to restoration, following which it can be worn part time. When the definitive restoration is designed it should take into account the need to permanently retain the orthodontic changes, ideally with a fixed-fixed bridge design with attachment of the pontic to the teeth on either side of the space. Alternatively, it may be possible to prevent mesio-distal drifting of a single abutment tooth by creating a broad contact area between the pontic and the adjacent tooth, but this does have potential adverse implications for oral hygiene and dental health.
Teeth which have been derotated are particularly prone to relapse, and strategies to reduce this include over rotation, prolonged retention and flattening the contact points. Pericision, that is the division of the supracrestal gingival fibre network after correction of the rotation, may also have a place in reducing rotational relapse although it is unlikely to eliminate it.36 If a rotated tooth is to be used as an abutment, either a second abutment must be included in the bridge to prevent rotational relapse or the tooth must be left in its rotated position.
From an orthodontic point of view, it would often be desirable to include multiple teeth as bridge abutments to prevent the undesirable drifting and relapse that may occur if a single cantilevered pontic is used (Fig. 6). However, fixed-fixed or double-abutment designs of bridgework have a significantly poorer long term prognosis35 and there is often a conflict between the orthodontist's desire for the restorative work to provide maximum orthodontic retention and the restorative dentist's concerns about the longevity of the restoration. In some cases, the patient may have to accept long-term part-time wear of a removable retainer.
References
Ogaard B, Krogstad 0 . Craniofacial structure and soft tissue profile in patients with severe hypodontia. Am J Orthodontics Dentofac Orthop 1995; 108: 472–477.
Chung LK, Hobson RS, Nunn JH, Gordon PH, Carter NE . An analysis of skeletal relationships in a group of young people with hypodontia. J Orthod 2000; 27: 315–318.
Baccetti T . Tooth rotation associated with aplasia of nonadjacent teeth. Angle Orthod 1998; 68: 471–474.
Pirinen S, Arte S, Apajalahti S . Palatal displacement of canine is genetic and related to congenital absence of teeth. J Dent Res 1996; 75: 1742–1746.
Joondeph DR, McNeil RW . Congenitally absent second premolars: an interceptive approach. Am J Orthod 1971; 59: 50–66.
Peck S, Peck L, Kataja M . Site specificity of tooth agenesis in subjects with maxillary canine malpositions. Angle Othod 1996; 66: 473–476.
Ericson S, Kurol J . Early treatment of palatally erupting maxillary canines by extraction of the primary canines. Eur J Orthod 1988; 10: 283–295.
Power SM, Short MB . An investigation into the response of palatally displaced canines to the removal of deciduous canines and an assessment of factors contributing to favourable eruption. Br J Orthod 1993; 20: 215–23.
Schroff B, Siegel SM, Feldman S, Siegel SC . Combined orthodontic and prosthetic therapy. Dent Clin NAm 1996; 40: 911–943.
Hobkirk JA, King PA, Goodman JR, Jones SP . Hypodontia: 2. The management of severe hypodontia. Dent Update 1995; 22: 8–11.
Bergendal B, Bergendal T, Hallonsten A-L, Koch G . Kurol J, Kvint S . A multidisciplinary approach to oral rehabilitation with osseointegrated implants in children and adolescents with multiple aplasia. Eur J Orthod 1996; 18: 119–129.
Dietschi J, Schatz JP . Current restorative modalities for the young patient with missing anterior teeth. Quint Int 1997; 28: 231–240.
Thordarson A, Zachrisson BU, Mjor IA . Remodelling of canines to the shape of lateral incisors by grinding: A long term evaluation. Am J Orthod Dentofacial Orthop 1991; 100: 123–132.
Millar BJ, Taylor NG . Lateral thinking: the management of missing lateral incisors. Br Dent J 1995; 178: 99–106.
Sabri R . Management of missing lateral incisors. J Am Dent Ass 1999; 130: 80–84.
Senty EL . The maxillary cuspid and missing lateral incisors: Aesthetics and Occlusion. Angle Orthod 1976; 46: 365–371.
Robertsson S, Mohlin B . The congenitally missing upper lateral incisor. A retrospective study of orthodontic space closure versus restorative treatment. EurJOrthod 2000; 22: 697–710.
Balshi TJ . Osseointegration and orthodontics: modern treatment for congenitally missing teeth. Int J Perio Rest Dent 1993; 13: 494–505.
Levin HI . Dental aesthetics and the golden proportion. J Pros Dent 1978; 40: 244–252.
Ceen RF, Rubler CG . Orthodontic Intervention as an aid in restorative dentistry. Dent Clin N Am 1985; 29: 279–291.
Gwinnett AJ, Ceen RF . Plaque distribution on bonded brackets: a scanning microscope study. Am J Orthod 1979: 75: 667–677.
Gorelick L, Geiger AM, Gwinnett AJ . Incidence of white spot formation after bonding and banding. Am J Orthod 1982; 81: 92–98.
Levander E, Malmgren 0, Stenback K . Apical resorption during orthodontic treatment of patients with multiple aplasia: a study of maxillary incisors. Eur J Orthod 1998; 20: 427–434.
Levander E, Malmgren 0, Stenback K . Apical root resorption during orthodontic treatment of patients with multiple aplasia: a study of maxillary incisors. Eur J Orthod 1998; 20: 427–434.
Isaacson KG, Thom AR . Guidelines for the use of radiographs in clinical orthodontics. London: British Orthodontic Society, 2001.
McDowell EH, Baker IM . The skeletal adaptions in the deep bite correction. Am J Orthod Dentofac Orthop 1991; 100: 370–375.
Ball JV, Hunt NP . The effect of Andresen, Harvold and Begg treatment on overbite and molar eruption. Eur J Orth 1991; 13: 53–58.
Dahl KL, Krogstad O, Karlsen K . Conservative treatment in cases with advanced localised attrition. J Oral Rehab 1975; 2: 209–214.
Beckett CA, Evans RD . The interface between orthodontics and restorative dentistry in the management of anterior tooth surface loss. Br J Orthod 1994; 21: 231–237.
Nanda R . Correction of deep overbites in adults. Dent Clin N Am 1997; 41: 67–87.
Dake ML, Sinclair PM . A comparison of Ricketts and Tweed-type arch levelling techniques. Am J Orthod Dentofac Orthop 1989; 95: 72–78.
Heasman PA, Millett DT, Chapple IL . The periodontium and orthodontics in health and disease. Oxford: Oxford University Press 1996.
Bates JF . Partial denture design: Modern Concepts. Dent Update 1986; 13: 90–95.
Aftun J, Zachrisson BU . New techniques for semi-permanent replacement of missing incisors. Am J Orthod 1984; 85: 367–375.
Hussey DL, Pagni C, Linden GJ . Performance of 400 adhesive bridges fitted in a restorative dentistry department. J Dent 1991; 19: 221–225.
Edwards JG . A long-term prospective evaluation of CSF in alleviating rotational. Am J Orthod 1988; 93: 380–387.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carter, N., Gillgrass, T., Hobson, R. et al. The interdisciplinary management of hypodontia: orthodontics. Br Dent J 194, 361–366 (2003). https://doi.org/10.1038/sj.bdj.4809995
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4809995
This article is cited by
-
Restorative dentistry clinical decision-making for hypodontia: managing missing premolar teeth
British Dental Journal (2023)
-
Aesthetic evaluation of the labiolingual position of maxillary lateral incisors by orthodontists and laypersons
BMC Oral Health (2021)
-
Quality of occlusal outcome following space closure in cases of lower second premolar aplasia using lingual orthodontic molar mesialization without maxillary counterbalancing extraction
Head & Face Medicine (2018)
-
The interdisciplinary management of hypodontia patients in the UK: a national service evaluation
British Dental Journal (2017)
-
The restorative management of microdontia
British Dental Journal (2016)