Key Points
-
Respiratory disorders may present with cough, sputum, wheeze or haemoptysis. Differentiation from cardiac disease (which may be concurrent) can be difficult since certain features are common to both. These include dyspnoea, finger clubbing and cyanosis. A thorough history helps in differentiation.
-
Respiratory failure can be precipitated in a patient with respiratory impairment if they have a GA. The impairment may be temporary eg because of infection. An upper respiratory tract infection may progress to the chest and therefore a GA should be postponed in the non-urgent case.
-
Enquiry should be made regarding the efficacy of medication eg inhalers used in the management of asthma and should be available for use if required. The possibility that the patient may be taking (or have taken) steroids should be borne in mind.
-
Patients who are short of breath feel more comfortable in a sitting position rather than supine.
Key Points
General medicine and surgery for dental practitioners:
-
1
Cardiovascular system
-
2
Respiratory system
-
3
Gastrointestinal system
-
4
Neurological disorders
-
5
Liver disease
-
6
The endocrine system
-
7
Renal disorders
-
8
Musculoskeletal system
-
9
Haematology and patients with bleeding problems
-
10
The paediatric patient
Abstract
Respiratory disorders are common and their main significance in dentistry relates to intravenous sedation, general anaesthesia and the unwanted effects of prescribed drugs. The degree of compliance achievable for local analgesia may also be compromised. As with most disorders the history is important in the assessment of such patients.
Similar content being viewed by others
Main
The respiratory system is always affected to some extent by smoking and enquiry should always be made with regard to smoking habits. Cough is a non-specific reaction to irritation anywhere from the pharynx to the lungs. It may produce sputum or be non-productive. Haemoptysis (coughing up of blood) may occur and it is important to differentiate this from haematemesis (vomiting of blood). Large volumes of blood may be coughed up in lung cancer, bronchiectasis and tuberculosis. Lesser amounts may be observed in pneumonia and pulmonary embolism. A summary of specific points to obtain in the history is given in Table 1 and these are discussed further below.
Infections of the respiratory tract may be acute or chronic and may be of the upper (ie vocal cords or above) or lower tract. Infections of either are a contra-indication to GA, which should be deferred until resolution has occurred. An upper respiratory tract infection (URTI) will readily progress to the lower tract if a GA is given. URTIs may occur as part of the common cold, as pharyngitis or tonsillitis and as a laryngotracheitis. The latter in children may cause stridor ('croup').
The paranasal air sinuses may become infected secondary to a viral URTI (a viral cause being most common). In acute sinusitis, the most commonly implicated bacteria are Streptococcus pneumoniae and Haemophilus influenzae. In maxillary sinusitis (which may also occur secondary to periapical infection of intimately related teeth) pain in the cheek and/or upper teeth is worsened by lowering the head and there is a mucopurulent nasal discharge. The maxilla over the antrum is tender to palpation. An occipito-mental radiograph may show increased radiopacity of the antrum but this can often be difficult to assess objectively and may be due to a thickened mucosal lining rather than acute infection (Fig. 1.). Analgesics and antibiotics eg amoxicillin, erythromycin or doxycycline for 2 weeks may be required. In addition a decongestant such as ephedrine may be useful however this should be for short term use (less than 2 weeks). In chronic sinusitis, formal drainage of the antrum may be required.
Lower respiratory tract infections are often viral, but bacterial infection will frequently supervene. There are signs of systemic upset eg fever, pleuritic pain (sharp pain on inspiration), cough, green/yellow sputum and possibly haemoptysis. The patient (especially the elderly) may appear confused and indeed this may be the only sign that something is wrong. There will often be dyspnoea (the subjective feeling of a shortage of breath).
Primary pneumonia occurs in previously healthy individuals and is often caused by pneumococci or 'atypical' organisms. Secondary pneumonias occur in patients with impaired defences eg in malignancy or Chronic Obstructive Airways Disease (COAD) such as chronic bronchitis and emphysema. Atypical pneumonias include Legionella pneumophila and Pneumocystis carinii (a protozoan-like cyst) in AIDS. The former organism causes Legionnaire's Disease and the organism multiplies in stagnant water found in air conditioning systems. It has been isolated from dental units which have been unused over a prolonged period eg weekends or holidays.1 Units such as these should be 'run through' thoroughly before resuming clinical use.
An inadequately treated pneumonia may lead to a lung abscess. Aspiration of a foreign body from the mouth can also be a cause. In dentistry this may occur when a rubber dam is not used when it is indicated leading to inhalation of debris or if an inadequate throat pack or uncuffed endotracheal tube is used for dental procedures under GA. The commonest infecting organisms are Staphylococcus aureus or Klebsiella pneumoniae.
Bronchial asthma is a generalised airways obstruction which in the early stages is paroxysmal and reversible. The obstruction, leading to wheezing, is due to bronchial muscle contraction, mucosal swelling and increased mucus production. Exposure to allergens and/or stress can induce an attack. It is now accepted that inflammation is an important aetiological factor in asthma and this has resulted in the use of anti-inflammatory medication in the management of the condition.2 In terms of management, infrequent attacks can be managed by salbutamol (ventolin) inhalers as needed or prophylactically if an attack might be predicted eg before exercise or prior to a stressful event such as dental treatment. If the attacks are more frequent, the salbutamol should be used regularly. If this is insufficient, inhaled steroids (or cromoglycate in the young) should be used. In severe cases systemic steroids may be prescribed. Enquiry should be directed toward the efficacy of medication, use of steroids and whether there have been episodes of hospitalisation.
COAD comprises chronic bronchitis and emphysema. Chronic bronchitis is said to exist when there is sputum production on most days for 3 months of the year in two successive years. Emphysema is dilatation of airspaces distal to the terminal bronchioles by destruction of their walls. The two co-exist in varying proportions in COAD and smoking is a common predisposing factor.3 Emphysema may rarely be inherited and is then due to Alpha-1-antitrypsin deficiency. Some COAD patients are breathless but not cyanosed ('pink puffers') some are cyanotic and if heart failure supervenes become oedematous or bloated ('blue bloaters'). In these patients the respiratory centres are relatively insensitive to carbon dioxide and they rely on 'hypoxic drive' to maintain respiratory effort. It is dangerous to give high levels of supplemental oxygen for longer than brief periods to these patients as breathing may stop or the patient may begin to hypoventilate.
Treatment of acute exacerbations of COAD involves broad spectrum antibiotics, bronchodilators (inhaled or nebulised) and possibly physiotherapy. Steroids may also be used. Dental treatment should be avoided during an exacerbation and in any event if possible should be carried out under LA.
Tuberculosis caused mainly by Mycobacterium tuberculosis is a disease that has increased in prevalence in recent years, largely caused by the immunocompromised HIV population, in the malnourished eg the materially deprived and in immigrants from underdeveloped countries. It is unlikely to be a great risk to dental staff unless the patient has an active pulmonary type in which case dental treatment is better deferred until control has been achieved. Pulmonary TB is usually spread by inhaling infected sputum and is highly infectious when active. If delayed treatment is not possible aerosols should be reduced to a minimum and it may be useful to carry out treatment under rubber dam. Masks and spectacles are mandatory for all personnel. Most primary infections are subclinical. Haematogenous spread can lead to skeletal or genito-urinary lesions. Widespread lesions give rise to the term 'Miliary TB'. A diagnosis of TB is suggested by chronic cough, haemoptysis, fever, night sweats and weight loss. Confirmatory tests include chest X-ray, sputum examination for acid and alcohol fast bacilli and the skin test or Mantoux test which shows a delayed hypersensitivity to a protein derived from Mycobacterium tuberculosis. Specific chemotherapy is by far the most important measure in the treatment of TB. In the UK, rifampicin, isoniazid, ethambutol, streptomycin and pyrazinamide are considered in the first-line treatment of TB. The majority of patients are treated as outpatients whereas a policy of 'isolation' was followed in the past. Immobilisation of the patient is necessary in some forms of skeletal TB.
Bronchiectasis is a condition where the bronchi are irreversibly dilated and act as stagnation areas for persistently infected mucus. It should be suspected in any persistent or recurrent chest infection. It may be congenital eg in cystic fibrosis or post infection eg TB, measles. Haemoptysis may occur. Intensive physiotherapy, antibiotics and bronchodilators are the mainstays of treatment.
Cystic fibrosis is one of the commonest inherited diseases (1 in 2000 live births) and is autosomal recessive. The cells are relatively impermeable to chloride (hence diagnosis by measuring the chloride concentration of sweat) and thus salt-rich secretions are produced. The mucus is viscid and blocks glands. In the young adult or child recurrent chest infections are seen, bronchiectasis and pancreatic insufficiency also occur.
Lung cancer is usually linked to cigarette smoking and may present in various ways including cough and haemoptysis. The disease may produce cerebral and hepatic metastases. The latter produce hepatomegaly, jaundice or ascites (fluid in the abdomen producing distension). Bone metastases (including the facial bones) may lead to pathological fracture. If the superior vena cava becomes compressed by tumour, facial oedema and cyanosis may occur (the Superior Vena Cava Syndrome). These patients may have muscle weakness (the Eaton-Lambert Syndrome) in which, unlike myaesthenia gravis the use of muscles leads to better function rather than a deterioration. Ectopic hormone production may occur in lung cancer (commonly adrenocorticotrophic hormone — ACTH).
Occupational lung disease is still seen in patients and may lead to significant respiratory impairment. Most inhaled particles cause no damage as they become trapped in the nose or are removed by the muco-ciliary clearance system. Particles may be destroyed by alveolar macrophages. The pneumoconioses are conditions which result from inhalation of various dusts and include asbestosis, silicosis and coal workers' pneumoconiosis. They will all restrict respiratory efficiency to some degree and potentially have a bearing on dental treatment provision.
Sarcoidosis is a multi-system disorder of unknown aetiology and is characterised by non-caseating granulomata. It most commonly affects the lungs of young adults but may occur at any age. Thoracic sarcoidosis classically presents incidentally as bilateral hilar lymphadenopathy on chest X-ray and is often asymptomatic. It may, however, be associated with cough, fever, arthralgia, malaise or erythema nodosum. Erythema nodosum comprises painful, erythematous nodular lesions on the anterior shins, but are not specific for sarcoid, for example they may also be seen in TB. Extra-thoracic manifestations of sarcoidosis are listed in Table 2. Gingival swelling found to be due to sarcoid is shown in Figure 2. The mainstay of diagnosis is a rise in the Serum Angiotensin Converting Enzyme level. Treatment may be carried out using steroids which may have implications for dental treatment as well as potential respiratory impairment.
The Adult Respiratory Distress Syndrome (ARDS) is a progressive respiratory insufficiency which usually follows a major systemic insult eg trauma, infection, and is largely due to interstitial pulmonary oedema arising from leaking capillaries. It is only relevant to mainstream dental practice in that about one third of surviving patients may be left with pulmonary fibrosis. Other causes of pulmonary fibrosis include connective tissue disorders eg rheumatoid arthritis, Sjögren's Syndrome or may be unknown — cryptogenic. Management is difficult and largely relies on immunosuppression eg with prednisolone.
Oral manifestations of respiratory disease • Gingival swelling (sarcoid) • Ulceration (TB) • Hyperpigmentation (lung cancer) • Drug induced xerostomia
Examination
The patient's colour may give an early clue as to their condition eg the pink puffer or blue bloated patient with COAD. The patient may be centrally cyanosed with a bluish hue to the tongue/lips. This is seen when there is a deoxygenated haemoglobin concentration greater than 5 grams per decilitre. Respiratory disease may cause the patient to be short of breath or tachypnoeic (breathing quickly) at rest or on minimal exertion eg walking into the surgery. The patient may be using their accessory muscles of respiration. In patients who retain carbon dioxide, the radial pulse at the wrist may feel very full and 'bounding' and carbon dioxide retainers may also have a flapping tremor of the hands when they are held outstretched.
Intra-oral examination may reveal that patients using corticosteroid inhalers are predisposed to developing oral/pharyngeal candidosis (Fig. 3.) and patients using beta 2 agonists and antimuscarinic agents often will have a dry mouth. More uncommon oral findings on examination may be a hyperpigmentation of the soft palate in lung cancer, or even bony metastases from lung cancer in the jaws. Chronic ulcers of the dorsum of tongue may rarely be an oral manifestation of TB. Cervical lymphadenopathy from TB may also be evident, but the more common lymphadenopathy secondary to a URTI should be considered first, (Table 3).
The pulse oximeter gives a guide to the efficiency of oxygenation of blood (Fig. 4.). It measures the pulse rate and oxygen saturation. The sensor, placed usually on a fingertip contains two Light Emitting Diodes (LEDs), one red measuring the amount of oxygenated haemoglobin, the other infrared, measuring the total haemoglobin. The oxygen saturation is the amount of oxygen carried in the blood relative to the maximum possible amount. There is a linear relationship between oxygen in the blood and the arterial oxygen saturation. Pulse oximetry does not necessarily indicate normal ventilation, since the saturation can appear normal if supplemental oxygen is being used.
Relevance of drugs in respiratory disorders
Corticosteroids
The use of corticosteroids, normally by inhalation, can lead to some problems related to dental management. Firstly, the use of steroid inhalers can lead to localised lowered resistance to opportunistic infections. As a result of this oro-pharyngeal candidal infection may occur.4 In order to avoid this complication patients should be advised to rinse and gargle with water after use of their inhaler. Secondly, regular use of inhaled steroids can lead to adrenal suppression thus the patient may be at risk of an adrenal crisis if they are subjected to stress.
Beta adrenergic agonist bronchodilators
Beta2 adrenergic agonists such as salbutamol and terbutaline can produce dry mouth, taste alteration and discolouration of the teeth. Dry mouth may increase caries incidence and thus a preventive regimen is important. If the dry mouth is severe artificial saliva may be indicated. The hypokalaemia which may result from large doses of beta2 adrenergic agonists may be exacerbated by a reduction in potassium produced by high doses of steroids and by epinephrine in dental local anaesthetics.
Antimuscarinic bronchodilators
Drugs such as ipratropium can produce dry mouth and taste disturbance and may also cause stomatitis. The absorption of the antifungal agent ketoconazole is decreased during combined therapy with ipratropium.
There is an increased chance of arryhthmia with halogenated general anaesthetic agents during combined therapy with theophylline. In addition theophylline decreases the sedative and anxiolytic effects of some benzodiazepines including diazepam. Plasma theophylline levels are reduced by carbamazepine and phenytoin5 and increased by erythromycin.6,7 Theophylline levels may also be affected by corticosteroids. Hydrocortisone and methylprednisolone have been shown to both increase and decrease theophylline levels. Terfenadine decreases the plasma concentration of erythromycin8 and this may be clinically important. Anti-muscarinic effects (such as dry mouth) are increased with concurrent use of tricyclic and mono-amine oxidase inhibitor antidepressant drugs.
Cromoglycate
Dry mouth, burning mouth and taste disturbance may occur during cromoglycate therapy.
Antihistamines
The more modern antihistamines such as terfenadine may produce dry mouth, but this is less common compared with older antihistamines. Stevens-Johnson syndrome may occur. Tricyclic and mono-amine oxidase inhibitor antidepressants increase anti-muscarinic effects such as dry mouth when used concurrently.
Among the many drugs which may produce dangerous arrythmias when combined with terfenadine are erythromycin,8 the anti fungal drugs, miconazole, fluconazole, itraconazole and ketoconazole9 and the antiviral agents efavirenz, indinavir, nelfinavir, ritonavir and saquinavir. Grapefruit juice must be avoided during therapy with terfenadine to avoid arrhythmias.
The antihistamines have an enhanced sedative effect when combined with anxiolytic and hypnotic drugs.
Cough suppressants and decongestants
Occasionally cough suppressants such as codeine may be used by patients and the additive effect of this should be considered when prescribing opioid analgesics (such as paracetamol/codeine compound drugs). There is a theoretical possibility that the adrenergic effects of epinephrine in dental local anaesthetics will be enhanced by ephedrine so dose reduction should be considered. Ephedrine may increase the chance of arrhythmia with halogenated general anaesthetic agents.
Relevance of respiratory disorders in the provision of local anaesthesia, sedation, general anaesthesia and management in dental practice
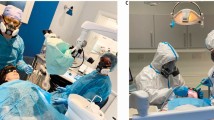
The relevant drug interactions and adverse effects of medication used to treat respiratory disorders have been discussed above. Other effects of respiratory disease on management are considered here. In the presence of respiratory impairment, general anaesthesia can be potentially dangerous since respiratory failure may be precipitated. If infection is temporary then resolution should be awaited. If GA is unavoidable and the condition is chronic eg in cases of COAD or bronchiectasis, then the condition of the patient should be optimised eg using preoperative physiotherapy, sometimes antibiotics, bronchodilators such as salbutamol and antimuscarinics such as ipratropium (sometimes nebulised). Even when treated using LA, these patients may become dyspnoeic, especially when supine. As part of any pre-operative work up, benefit can be gained by stopping smoking. The use of rubber dam may be unacceptable in patients with COAD because of further compromise of the airway. If rubber dam is necessary supplemental oxygen via a nasal cannula may be required but low concentrations should be used. Figure 5. shows a patient receiving supplemental oxygen via a nasal cannula.
In cases of active TB, a GA is contra-indicated, both due to impaired respiratory function or contamination of anaesthetic machine circuits.
Asthmatic patients should have treatment carried out using LA if possible. Effort should be made to allay anxiety as far as possible and treatment should not be carried out if the patient has not brought their normal medication and such medication is otherwise unavailable. Relative analgesia using nitrous oxide and oxygen is preferred to intravenous sedation since the former can be rapidly controlled. GA can be complicated by hypoxia and increased carbon dioxide which can lead to pulmonary oedema even if cardiac function is normal.
As mentioned above patients may not be comfortable in the supine position if they have respiratory problems. If the patient suffers from asthma then aspirin-like compounds should not be prescribed as many asthmatic patients are allergic to these analgesics.10 Similarly, sulphite-containing compounds (such as preservatives in some epinephrine-containing local anaesthetics) can produce allergy in asthmatic patients.11
A severe asthmatic attack can be life-threatening and as stress may contribute to the onset of such a condition the dentist should have the equipment to deal with such an emergency at hand. A salbutamol inhaler or nebulised salbutamol are useful. In extremis the administration of epinephrine as for the management of anaphylactic shock (that is an intramuscular dose of 0.5 ml increments of 1:1000) should be performed. Intravenous hydrocortisone (200–500 mg) should be administered to all severely ill patients. Intravenous aminophylline is reserved for patients who do not respond quickly to nebulised bronchodilator therapy. Care is needed with patients already taking theophylline preparations and this step is best left until medical assistance is available.
Adrenal crisis An adrenal crisis may occur if there is a lack of circulating catcholamines. This is unlikely during routine dentistry but blood pressure monitoring of 'at risk' patients is recommended
The use of supplemental steroids prior to dental surgery in patients at risk of an 'adrenal crisis' is a contentious issue. The rationale for steroid supplementation is as follows. Corticosteroids are critical in the body's response to trauma (including operative trauma). A normal response is to increase corticosteroid production in response to stress. If this response is absent, hypotension, collapse and death will occur. The hypothalamo-pituitary-adrenal axis will fail to function if either pituitary or adrenal cortex ceases to function eg administration of corticosteroids leads to negative feedback to the hypothalamus causing decreased ACTH production and adrenocortical atrophy. This atrophy means that an endogenous steroid boost cannot be produced in response to stress. Recent studies have suggested that dental surgery may not require supplementation.12 More invasive procedures however, such as third molar surgery or the treatment of very apprehensive patients may still require cover. It is wise, even if supplementary steroids have not been used, to monitor the blood pressure of patients taking steroids. If the diastolic pressure falls by more than 25% then an intravenous steroid injection (100 mg hydrocortisone) is indicated. Patients who may require supplementation are those who are currently taking corticosteroids or have done so in the last month. A supplement may also be required if steroid therapy has been used for more than one month in the previous year. If the patient is receiving the equivalent of 20 mg prednisolone daily then extra supplementation is not required.
Summary
Respiratory problems affect many aspects of dental treatment. Eliciting a proper history from the patient with respiratory disease will help prevent serious problems and alert the dentist to oro-facial conditions which may result from the use of appropriate medication. Patients with significant respiratory problems, particularly if they need extensive treatment are best treated in the hospital setting.
References
Scully C, Cawson RA, Griffiths M . Occupational hazards to dental staff. BDJ publication 1990; 178–179.
Randall T . International consensus report urges sweeping reform in asthma treatment. JAMA 1992; 267: 2153–2154.
Lee PN, Fry JS, Forey BA . Trends in lung cancer, chronic obstructive lung disease, and emphysema death rates for England and Wales 1941-1985 and their relation to trends in cigarette smoking. Thorax 1990; 45: 657–665.
McAllen MK, Kochanowski SJ, Shaw KM . Steroid aerosols in asthma: an assessment of betamethasone valerate and a 12-month study of patients on maintenance treatment. Br Med J 1974; i: 171.
Reed RC, Schwartz HJ . Phenytoin-theophylline-quinidine interaction. New Engl J Med 1983; 308: 724–725.
Reisz G, Pingleton SK, Melethil S, Ryan P . The effect of erythromycin on theophylline pharmacokinetics in chronic bronchitis. Am Rev Resp Dis 1983; 127: 581–584.
Paulsen O, Hoglund P, Nilsson L-G, Bengtsson H-I . The interaction of erythromycin with theophylline. Eur J Clin Pharmacol 1987; 32: 493–498.
Honig PK, Woosley RL, Zamani K, Conner DP, Cantilena LR . Changes in the pharmacokinetics and electrocardiographic pharmacodynamics of terfenadine with concomitant adminstration of erythromycin. Clin Pharmacol Ther 1992; 52: 231–238.
Eller MG, Okerholm RA . Pharmacokinetic interaction between terfenadine and ketoconazole. Clin Pharmacol Ther 1991; 49: 130.
Szczeklik A . The cyclo-oxygenase theory of aspirin-induced asthma. Eur Resp J 1990; 3: 588–593.
Seng GF, Gay BJ . Dangers of sulfites in dental local anesthetic solutions: warning and recommendations. J Am Dent Assoc 1986; 113: 769–770.
Thomason JM, Girdler NM, Kendall-Taylor P, Wastell H, Weddell A., Seymour R A . An investigation into the need for supplementary steroids in organ transplant patients undergoing gingival surgery. J Clin Period 1999; 26: 577–582.
Acknowledgements
The authors would like to thank Professor J. V. Soames for some of the photographs used in this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Greenwood, M., Meechan, J. General medicine and surgery for dental practitioners Part 2: Respiratory system. Br Dent J 194, 593–598 (2003). https://doi.org/10.1038/sj.bdj.4810230
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4810230
This article is cited by
-
General medicine and surgery for dental practitioners. Part 1 – the older patient
British Dental Journal (2010)