Key Points
-
Patients are becoming more aware of newer technologies and treatment modalities, and are increasingly requesting metal-free restorations
-
A novel method of producing aesthetic, anterior and posterior metal-free all-ceramic crowns is described
-
Increasing use of computer-aided design and computer-aided milling (CAD/CAM)
-
Aesthetics and strength for restorations are no longer mutually exclusive.
Abstract
Increasing patient expectations regarding the appearance of restorations continue to test the ingenuity and skill of the dental team. To this end the quest for sufficiently strong, metal-free, all-ceramic restorations to function in all areas of the mouth continues apace. We report on a possible solution to this problem that uses computer-aided design/computer-aided milling (CAD/CAM) technology coupled with a novel, densely sintered, ceramic material. In this article we offer suggestions for case selection, preparation design, and luting procedures, and in addition illustrate these with a number of completed cases.
Similar content being viewed by others
Main
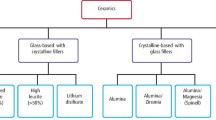
Patients continue to demand aesthetic, tooth-coloured restorations, which are free of metal.1 The absence of a metal substructure has the potential to produce a restoration with superior aesthetics, and enhanced biocompatability. Traditionally however, metal-free restorations have been relatively weak and prone to fracture in service. Improvements in materials during the past 10 years have been such that several metal-free systems, suitable for the construction of single crowns for anterior and posterior use, are now available to the practitioner (Table 1).
A new ceramic material, Procera AllCeram, with universal anterior and posterior applications has recently been introduced to the UK by Nobel Biocare (Sweden). This type of restoration has a densely sintered, high purity, alumina core and was first described in 1993.1 These restorations are produced in a unique manner using technology initially developed to produce titanium copings for implant abutments by spark erosion. The ceramic core is milled and sintered in Sweden at the 'hub' laboratory using a digital prescription transmitted, by modem, from a 'spoke' laboratory in the UK (fig. 1). The coping is then returned to the 'spoke' laboratory for conventional build-up with specially developed dental porcelains (AllCeram Porcelain, Ducera).
Preliminary research has shown that the strength of these restorations is sufficiently high to withstand functional and parafunctional loading, without fracturing, in both anterior and posterior situations.2 Restorations produced in this manner have also been shown to have a precise fit with marginal openings of less than 70 μm and to produce minimal wear of the opposing dentition even, if the core material is exposed, provided the material is suitably polished.3,4,5 Concurrent studies have also shown the excellent colour stability and masking effect of this restorative material.
Requirements
There are no special clinical requirements over and above the use of a specially manufactured bur set. Access to a 'spoke' laboratory, however, with the necessary scanning equipment and modem link to Gothenburg in Sweden is necessary, and at the present time a limited number of laboratories in the UK have this facility.
Case selection
The technique is considered to have universal applicability and may be used for the restoration of molar, premolar and anterior teeth. The presence of metal posts and cores is not a contra-indication and does not adversely affect the aesthetic outcome. As with similar techniques (Table 1) poor oral hygiene, atypical occlusal loading such as nocturnal bruxism or other grinding habits and insufficient coronal tooth tissue for retention and resistance form are contra-indications.
Tooth preparation
In principle, an axial and occlusal reduction of 0.8–1.0 and 2.0 mm respectively is required. To minimise stress concentration within the ultimate restoration and facilitate digitisation of the preparation, the use of sharp line angles, boxes, grooves and 'butt' type shoulders is contra-indicated and a medium, chamfered, axial reduction is required. For similar reasons it is important to round off all surface transitions and there must be no residual sharp edges to the preparation. To facilitate appropriate tooth preparation a set of customised diamond burs is available (fig. 2). Preparation margins should be placed supragingivally wherever possible. The use of subgingival margins, eg for aesthetic reasons, should be restricted to the labial aspect of upper anterior teeth. This will not only simplify impression procedures but it will also help to maintain optimal periodontal health. Impressions, shade selection and occlusal registration require no special considerations for restorations of this type and do not differ from those required for any other indirect tooth-coloured restoration.
Laboratory procedures
In the laboratory a conventional die stone model with high abrasion (wear) resistance is produced and trimmed. The die stump must have sides parallel to the long axis of the preparation, and the preparation margin should be clearly defined. To enhance marginal definition and ensure accurate digitisation, the die is 'guttered' immediately below the finish line (fig. 3).
The trimmed die is mounted, on a rotating platform, in a digital scanner device that is attached to a personal computer (PC) and modem (fig. 4). The die rotates at high speed and a scanning probe, which incorporates a sapphire stylus, approaches the die at a 45° angle. The stylus is held against the die with a light pressure of 20 g to ensure close contact during the scanning process. At each angle of rotation the position of the sapphire stylus is recorded, therefore for each rotation 360 recordings are registered, and following each complete rotation the stylus is elevated by 200 μm and another circle of recordings taken until the entire preparation has been digitised.6 The average preparation will require around 50,000 readings for accurate digitisation, and this method of scanning has been shown to be extremely accurate with maximum shape-related errors of ± 10 μm. The scanning process is surprisingly fast and the scanning of one preparation takes around 30 seconds.
Following digitisation, the coping is designed on the PC; a suitable coping thickness (usually 600 μm) and an appropriate emergence profile are selected (fig. 5). The finishing line is further refined manually at 10° intervals around the finishing line of the preparation. The computer extrapolates this information to determine the definitive finishing line, calculates the relief space required for the luting agent and stores this information as a digital prescription. This information (a PC datafile) is transmitted by modem to the 'hub' laboratory in Gothenburg, Sweden. This is very rapid and several prescriptions for the same and/or different patients can be transmitted simultaneously.
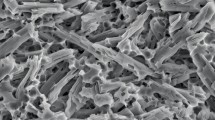
In Sweden, the data file is received by a computer-controlled milling machine, which has a milling tool of exactly the same dimensions and angle of approach as that of the sapphire stylus in the 'spoke' laboratory. This reduces any transcription errors between reading and milling to zero and enables restorations to be produced with great accuracy.7 The milling machine creates a duplicate of the preparation in the 'hub' laboratory onto which aluminum oxide is densely packed. To allow for sintering shrinkage the milling machine automatically enlarges the duplicate preparation by a factor of 0.2 (20%). The aluminum oxide is machined to the proportions requested in the digital prescription and sintered to full density. The resultant coping is checked for any inaccuracies and defects and then returned to the 'spoke' laboratory for build-up with veneering porcelains. The coping arrives back in the 'spoke' laboratory within 2 days of transmission of the digital prescription.
In the 'spoke' laboratory the technician may adjust the thickness of the coping for occlusal or aesthetic considerations but a minimum thickness of 300–400 μm is required, as further reduction significantly reduces the strength of the restoration.8 Special porcelains (AllCeram Porcelain, Ducera), which have a coefficient of thermal expansion (7×10−6 C°) equal to that of the aluminum oxide coping material, have been developed to veneer the coping. A significant reported advantage of the veneering porcelain are its fluorescent properties which are similar to that of the natural dentition and thought to reduce problems with metamerism whereby a crown shade varies in different lighting conditions.6 Crown build-up, incorporation of stains and translucency, characterisation and glazing procedures require no special consideration and do not differ markedly from other systems.
Luting procedures
The fit of crowns, produced in this manner, has been reported to be excellent with the manufacturing process producing a uniform cement space between the crown and residual tooth structure.3,4 It is recommended that the crown is tried in with water or a thin alginate mixture while fit, aesthetics and the occlusion are checked.
The operator has a choice of the following for cementation of the restoration:
-
Zinc phosphate cement
-
Glass-ionomer cement
-
A chemically-cured resin cement such as Panavia 21 (Kuraray Co Ltd, Japan).
As the fit surface of the aluminum oxide (Al2O3) coping is microscopically rough there is little to be gained by acid etching; surface treatment of the fit surface is therefore usually restricted to sandblasting and the application of a silane-coupling agent. It is suggested that Panavia 21 is the cement of choice. This is supplied with a priming agent and the use of this coupled with a total etch procedure is recommended. Glass-ionomer cement has been advocated for use when moisture control is not optimal.
Clinical studies to date
To date there is very little information regarding the long-term clinical performance of these restorations with most published data being restricted to laboratory based studies of the material's physical properties. In a well conducted prospective study of 100 crowns (55 molars, 28 premolars, 17 incisors/canines), placed in 58 patients, monitored over a period of 5 years, only three restorations fractured, two suffered infractions of the veneering porcelains, and one required replacement owing to recurrent caries. It is important to note, however, that the veneering porcelain used in this study was Vitadur N (Panadent Ltd, UK) and not AllCeram Porcelain, Ducera (Nobel Biocare Ltd, Sweden) as currently used. The effect this may have had on porcelain fracture has yet to be established. The remaining crowns were rated as excellent or satisfactory for colour, anatomic form and marginal integrity using the California Dental Association's quality evaluation guidelines.9 These initial results would suggest that single crowns produced with this novel ceramic material can be expected to give acceptable clinical service for at least 5 years and that the technique has universal applicability. However further research is required in this area with respect to longevity.
Clinical experience with the technique
To date 14 patients have been provided with Procera all-ceramic crowns at the University Dental Hospital of Manchester. The first two cases treated are reported here:
Case report 1
A 23-year-old man, requested replacement of a porcelain fused to the metal crown (fig. 6). This crown had been placed some years previously, following trauma to the upper incisors, and the patient was unhappy with the appearance. The tooth was root treated and a replacement crown placed (fig. 7).
Case report 2
A 53-year-old lady, attended with a fractured premolar tooth (fig. 8). As there was insufficient coronal tooth tissue to support an intracoronal restoration and the tooth had been root-treated previously an all-ceramic crown was placed (fig. 9).
Conclusion
It is concluded that this recent development provides practitioners with a novel way of providing high strength, durable, metal-free, aesthetic tooth coloured restorations. Further research, however, is still required to explore other possible applications for this technology, which could include the use of optical impressions directly transmitted to the milling machine and the production of multiple crown units and fixed prostheses.
References
Andersson M and Odén A . A new all-ceramic crown. A dense-sintered, high-purity alumina coping with porcelain. Acta Odontol Scand 1993; 51: 59–64.
Wagner W C, Chu T M . Biaxial flexural strength and indentation fracture toughness of three new dental core ceramics. J Prosthet Dent 1996; 76: 140–144.
May K B, Russell M M, Razzoog M E, Lang B R . Precision fit: The Procera AllCeram crown. J Prosthet Dent 1998; 80: 394–404.
Andersson M, Carlsson L, Persson M, Bergman B . Accuracy of machine milling and spark erosion with a CAD/CAM system. J Prosthet Dent 1996; 76: 187–193.
Hacker C H, Wagner W C, Razzoog M E . An in vitro investigation of the wear of enamel on porcelain and gold in saliva. J Prosthet Dent 1996; 75: 14–17.
Andersson M, Razzoog M E, Odén A, Hegenbarth E A, Lang B R . Procera: A new way to achieve an all-ceramic crown. Quintessence Int 1998; 29: 285–296.
Persson M, Andersson M, Bergman B . Accuracy of a high precision digitizer for CAD/CAM of crowns. J Prosthet Dent 1995; 74: 222–229.
White S N, Caputo A A, Li Z C, Zhao X Y . Modulus of rupture of the Procera all-ceramic system. J Esthetic Dent 1996; 8: 120–126.
Odén, Andersson M, Krystek-Ondracek I, Magnusson D . Five-year clinical evaluation of Procera All Ceram crowns. J Prosthet Dent 1998; 80: 450–456.
Acknowledgements
The authors gratefully thank Bolton Dental Laboratory, specifically Messrs C. Lee and C. Dean, for their technical support of this project and Mr C. Atack, Department of Medical Illustration, University Dental Hospital of Manchester for the illustrations.
Author information
Authors and Affiliations
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Brunton, P., Smith, P., McCord, J. et al. Procera all-ceramic crowns: a new approach to an old problem?. Br Dent J 186, 430–434 (1999). https://doi.org/10.1038/sj.bdj.4800134
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800134
This article is cited by
-
Crowns and extra-coronal restorations: Materials selection
British Dental Journal (2002)