Abstract
Control of occlusal contacts is important to the success of restorative dentistry. Tooth surface loss can contribute to a loss of stability in the occlusion. An occlusal splint is often part of pre-restorative management and can also have a valuable role in protecting both teeth and restorations from excessive loads and further wear.
Similar content being viewed by others
Main
The first two articles in the series concentrated on the aetiology and presentation of tooth surface loss. This paper begins to look at its consequences. Tooth wear can be considered pathological if the degree of wear exceeds the level expected at any particular age. Tooth surface loss affecting the functional surfaces creates difficulties for the restorative dentist and may affect the stability of the occlusion. The first part of this article discusses the importance of occlusal stability and the possible consequences when it is lost. The second part is devoted to the role of occlusal appliances in protecting teeth from wear and in some aspects of the pre-restorative management of tooth surface loss.
The occlusion
Most functional (chewing) and parafunctional (bruxing and clenching) movements of the mandible take place around the intercuspal position (ICP). This is defined as the mandibular position in which maximum intercuspation of the teeth occurs. Functional movements result in brief contacts between maxillary and mandibular teeth, usually toward the end of the masticatory cycle. However, parafunctional activity may produce prolonged periods of forceful tooth contact.
In 90% of the population maximum intercuspation occurs slightly forward from the retruded position of the mandible to the maxilla. However, contact between opposing teeth and the resultant proprioceptive response guides the mandible repeatedly into the habitual ICP, wherever it may be.
Should a patient exhibit parafunctional activity, it becomes increasingly important that there are enough opposing posterior teeth to provide stable ICP contacts, so that the forces produced during parafunction are distributed over a wide area and in the most favourable direction.
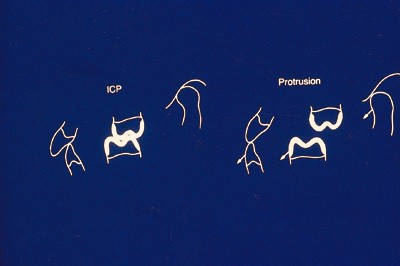
Stable ICP contacts are provided by natural or restored surfaces which have appropriately steep cuspal anatomy (fig. 1). Contact either between the tips of supporting cusps and opposing fossae, or three points surrounding each supporting cusp tip and the ridges surrounding the opposing fossa (tripodisation), provide stable ICP contacts which direct occlusal forces axially.
They will also, in conjunction with the proximal contacts of adjacent teeth, stabilise the positions of individual teeth and also of the mandible in ICP. If ICP contacts are unstable, tilting and tipping of teeth are more likely particularly in the absence of an intact arch. This will cause further loss of stable ICP contacts and increase the likelihood of interferences occurring between the posterior teeth during lateral and protrusive movements.
In order to reduce the potentially harmful lateral forces produced by bruxing on interferences between posterior teeth, it is desirable for a patient to possess adequate anterior guidance. Contact between opposing teeth, preferably the canines in lateral excursion and the central incisors in protrusion, discludes the posterior teeth as soon as the mandible moves from ICP (fig. 1). This occlusal scheme most importantly reduces the number of tooth contacts occurring outside ICP. There is some evidence that this alters the proprioceptive feedback to the central nervous system which in turn reduces the level of activity in the masticatory muscles,1,2 although this view is hard to support on scientific grounds. However, in simple practical terms it is very much easier to make restorations in the presence of an adequately steep, immediate disclusion, provided by a small number of teeth near the front of the mouth.3
How may occlusal stability be maintained or lost?
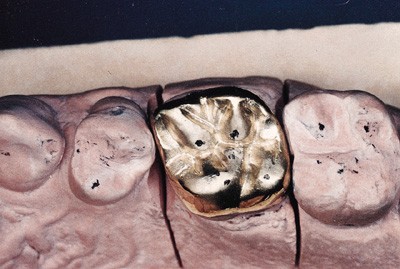
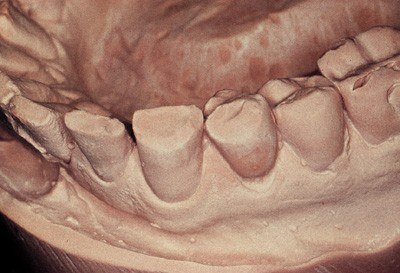
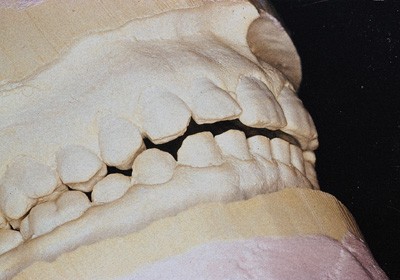
Most restorations are made to conform to a patient's existing ICP. For this to be an appropriate form of treatment ICP must be stable and the occlusal anatomy of all restorations must be carefully shaped to reproduce correct contacts. In addition, the restorative materials used should be easy to manipulate to produce the necessary occlusal contacts, and exhibit similar wear characteristics to enamel or to opposing restorations. This will reduce the chance of differential wear and increase the likelihood of stable contacts being maintained long-term. Gold (fig. 2) is still the most suitable material based upon these criteria, while amalgam remains the plastic material of choice for posterior teeth. The use of composite resin (direct or indirect) or occlusal porcelain to restore large areas of multiple occlusal surfaces should be avoided in patients prone to parafunction and those with restricted anterior guidance. The difficulty in providing stable contacts and the surface hardness of these materials may result in increased tooth surface loss in the opposing arch (fig. 3, 4). The careful use of occlusal porcelain and composite resin is less harmful in individuals who possess immediate disclusion of their posterior teeth and do not parafunction.
Loss of stable contacts may also occur because of tooth surface loss caused by acid erosion or parafunction between unrestored or similarly restored surfaces. Loss of cusp height and definition, broadening areas of ICP contact, combined with a shallowing of the anterior guidance, reduces stability and increases the chances of interferences in lateral or protrusive movements, causing increased and less favourable stress distribution in the teeth affected.
Loss of occlusal stability may result in the repeated fracture of restorations and teeth, increased mobility and drifting, particularly of the upper anterior segment. Traditionally, it has also been held to potentially have other long-term effects on the structure and function of the temporomandibular joints,4,5 although such assertions are increasingly open to question. In the presence of any of these signs of loss of occlusal stability, it sometimes becomes necessary to reorganise the patient's occlusion creating a new and stable ICP at the retruded position of the mandible. There is little reason to choose the retruded position other than because of 'prosthetic convenience'. In the absence of a stable ICP, the retruded position is the only relationship of mandible to maxilla which can be repeatedly and consistently recorded and has been shown to be physiologically acceptable. It is also the maxillo-mandibular relationship to which the mandible will return when not prevented from doing so by interfering tooth contacts. It may therefore be used as the reference position in which the new restorations will intercuspate when re-organising the occlusion.
The rationale and indications for occlusal splints
An occlusal splint is a removable appliance covering some or all of the occlusal surfaces of the teeth in either the maxillary or mandibular arches. The ideal occlusal splint is made from laboratory-processed acrylic resin which should cover the occlusal surfaces of all the teeth in one arch. It should provide even simultaneous contacts on closure on the retruded axis with all opposing teeth and anterior guidance causing immediate disclusion of the posterior teeth and splint surface outside ICP.
The splint provides the patient with an ideal occlusion with posterior stability and anterior guidance. It will disrupt the habitual path of closure into ICP by separating the teeth and removing the guiding effect of the cuspal inclines. It causes an immediate and pronounced relaxation in the masticatory muscles,6 which will eventually result in the mandible repositioning and closing in the retruded position uninterfered with by the teeth.
In order to achieve this muscle relaxation and mandibular repositioning the occlusal surface of the splint is flat and without indentations so as not to hold or guide the mandible into any predetermined position. The only exception to this is the area lateral to the canine and anterior to the incisor ICP contacts which is gently ramped to provide anterior guidance. To achieve muscle relaxation and repositioning of the mandible, the splint ideally must be worn continuously, failure to do so will result in an increase in masticatory muscle activity.7,8 As the mandible repositions it is necessary to adjust the splint frequently to maintain even contact and disclusion.9 However, continuous wear is often not compatible with the patient's daily activities. Wear at night and also if possible in the evenings will achieve the same result but more slowly.
Uses of splints
The use of an appropriate occlusal splint may be indicated in the following circumstances:
Prevention of tooth surface loss
Patients who are prone to nocturnal bruxism should routinely wear occlusal splints at night. The splint may reduce their parafunctional activity while it is being worn but as soon as it is removed masticatory muscle activity will resume its increased levels.6 Whether or not bruxing is continuing can be monitored by observing wear facets created on the splint surface. Even if parafunction continues the intervening splint will prevent damage to the teeth. It is important to motivate patients to wear their splints by stressing the long-term consequences of them not doing so.
Management of mandibular dysfunction
Many studies have shown that an occlusal splint may be beneficial in reducing the pain experienced in mandibular dysfunction.8 Various theories have been put forward to explain the mechanism involved. One of the more common theories is that in lowering masticatory muscle activity, a splint will effectively reduce the build-up of metabolic waste products which may result in restricting muscle pain and spasm. While there is no doubt that many patients suffering from dysfunction who are treated with occlusal splints, do show a significant decrease in pain levels, it is far from clear that the therapeutic effect of the splint is responsible.10 It is possible that a significant part of this improvement is achieved through the placebo effect (although there is some evidence that occlusal treatment with a splint does have a truly therapeutic effect11,12). Because of the difficulties dentists may experience in diagnosing the source of a patient's facial pain and the doubts which exist over the therapeutic effect of occlusal treatment, it is advisable to carry out only reversible occlusal treatment on such patients (splint therapy, not occlusal equilibration).
Pre-restorative stabilisation
The first part of this paper described the importance of occlusal stability and introduced the concept of reorganising the occlusion to create a new and stable ICP at the retruded position when stability is absent. When conforming to the existing ICP the maxillo-mandibular relationship to which restorations are made is easily and accurately determined by the intercuspation of the teeth. When reorganising it is necessary to locate and record the retruded position of the mandible and then mount both diagnostic and working casts on an articulator in this relationship. In the absence of stable ICP contacts this position is determined solely by the temporomandibular joints and associated neuromuscular system. It is essential that the patient's masticatory system is free from dysfunction, either internal derangement or extra-capsular muscle dysfunction, in order that a correct and reproducible retruded position can be recorded. A consistent position must be recorded before embarking upon restorative treatment. If not, it is likely that changes in the occlusal relationship may occur following tooth preparation and temporisation, or cementation of the new restorations. When reorganising the occlusion it is essential to precede restorative procedures with a period of splint therapy to ensure that a stable relationship has been achieved.
Creating space to restore worn anterior teeth
Figures 5 and 6 show a patient before and after splint therapy. At initial examination (fig. 5) the patient requested restoration of severely worn mandibular anterior teeth. It appeared that both ICP and the retruded position were coincident and that no space was available to correctly restore these teeth. After 1 month of wearing an occlusal splint (fig. 6), the mandible had repositioned posteriorly into a stable retruded position. This created space to enable the worn teeth to be properly restored. This repositioning occurred because the pre-existing discrepancy between RCP and ICP had been hidden by the patient's neuromuscular system.
Protection of new restorations from parafunction
The aetiology of parafunction is largely stress-related. It is likely that patients will continue to brux and clench after restoration of worn teeth. It is highly advisable for them to wear a post-restorative splint to protect their new restorations from damage. This should be made clear to the patient before treatment begins.
Types of occlusal splint — advantages and disadvantages
Many types of occlusal splint have been advocated. They may be full or partial occlusal coverage, maxillary or mandibular, repositioning or stabilising, and made from a variety of different materials.
Choice of materials
The material of choice is laboratory-processed acrylic resin. It is a reasonably hard material which may be easily adjusted and is durable enough to serve as a protective nightguard. Resilient vacuformed vinyl splints are of limited use. Although quick and economic to make they are soon destroyed by determined bruxers. Their resilient surface is not amenable to the production and maintenance of the stable occlusion necessary to achieve muscle relaxation.13 The use of hard metal alloys such as cobalt/chrome to cover occlusal surfaces is highly inadvisable as it will result in increased wear of the opposing teeth.
Partial coverage splints
Occlusal splints must be worn continually, often for considerable periods of time to be effective. If a splint does not cover all the occlusal surfaces in an arch, unopposed teeth will continue to erupt creating an iatrogenic malocclusion. This applies to both anterior and posterior partial coverage splints and their use cannot therefore be recommended.
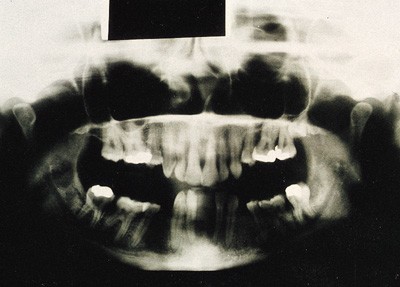
Figure 7 shows a radiograph of a patient who had worn a posterior onlay splint for about 1 year. When she closed into ICP, the posterior teeth were several millimetres apart (the thickness of the splint). The appliance provided no anterior coverage but had permitted the incisors and canines to supra-erupt, and led to intrusion of the posterior segments. An anterior splint would permit the posterior teeth to erupt, so that when the splint was removed the anterior teeth would be apart and anterior guidance would have been lost. In this series a technique will be described where a form of anterior splint (Dahl appliance) is used to gain space to restore worn anterior teeth. This is entirely different as it is a carefully planned procedure in which the anterior space created is filled and guidance restored with restorations placed on the severely worn teeth.
Maxillary or mandibular splints?
Providing the requirements of full occlusal coverage, posterior stability, anterior guidance and use of an appropriate material are met, it matters little whether a splint is made on the maxillary or mandibular arch. In Class I and II incisor relationships it is easier to produce an ideal occlusion on a maxillary appliance while the converse is true in Class III situations.
Stabilisation versus repositioning splints
Ramjford and Ash originally described the stabilisation or Michigan-type splint for which detailed fabrication and use will be covered in the final section of the paper. It is a full coverage maxillary splint made from laboratory processed acrylic resin which provides anterior disclusion and stable ICP contacts between a generally flat surface and the opposing teeth. It does not seek to actively reposition the mandible into a predetermined position. It is impossible at the outset to predict the extent and direction of mandibular repositioning, and any attempt to guide the mandible more actively with the splint may actually prevent stabilisation of the retruded position.
Stabilisation splints, through causing muscle relaxation, may also aid the repositioning of a displaced meniscus providing the displacement is neither too severe nor too longstanding.
The use of splints which seek to reposition the mandible in a predetermined position has been advocated, particularly in cases of internal derangement where some studies have shown them to be more effective than stabilisation splints.14 They possess occlusal surfaces with well-defined fossae into which the opposing teeth locate with the mandible in the desired position. The problem with the use of such splints is that they may not achieve the desired masticatory muscle relaxation: also it is exceptionally difficult if not impossible to predict exactly the position in which the mandible should be located. This position is generally downward and forward from the habitual ICP, the rationale being that the stress on the disrupted joint components will be relieved, permitting them to gradually realign.15 They also have the considerable disadvantage that following repositioning of the meniscus the patient may be left with a posterior open bite. If this occurs occlusal contacts may gradually re-establish through supra-eruption. Sometimes orthodontic treatment may be necessary to re-establish occlusal stability.
Because of the difficulties in use and the possible irreversible changes which may be caused to the patient's occlusion, the use of these appliances in general practice is recommended only with caution and in experienced hands.
Fabrication, fitting, adjusting and monitoring a Michigan splint
Fabrication
Maxillary and mandibular full arch alginate impressions are made in metal rimlock trays. The impressions should be quickly poured with the occlusal surfaces downward to ensure accurate reproduction of surface detail. While the stone is setting the poured impressions must be stored in a humid atmosphere. A Tupperware box containing moist paper towels is ideal. When the impressions are removed, the casts should be left to dry for 24 hours; if articulated too soon, the damp stone surfaces will be abraded and rendered inaccurate.
The casts should be mounted in a semi-adjustable articulator using a facebow record to mount the maxillary cast and an interocclusal record taken on the retruded axis to establish the maxillo-mandibular relation. The interocclusal registration is a pre-contact record using a rim of extra hard wax which fits accurately over the maxillary teeth without contacting the soft tissues. A fluid recording medium (Kerrs Tempbond) is applied to the lower surface to register the cusp tips of the mandibular teeth on closure. Control of the mandible is improved by means of a traditional anterior jig which prevents the teeth from coming into contact making manipulation of the mandible easier and determining the vertical dimension of the record.
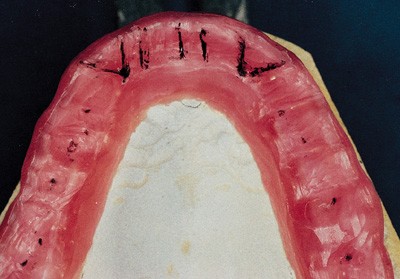
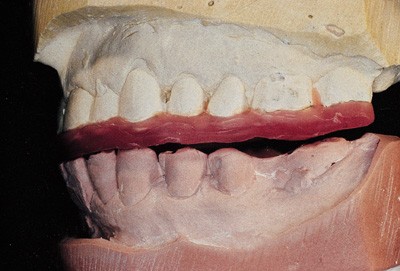
The incisal pin of the articulator is adjusted to provide a space of a roughly 2 mm between the most posterior teeth, and the outline of the splint drawn on the maxillary cast in pencil. It should extend about 3 mm onto the palatal soft tissues and wrap just over the buccal cusps and incisal edges. The splint will be retained by clipping into proximal, buccal and lingual undercuts and so these should not be blocked out prior to waxing. Two thicknesses of pink baseplate wax are softened and adapted over the cast and then trimmed to the pencil outline. The articulator is closed together until the incisal pin contacts the incisal table, establishing the vertical dimension of occlusion of the splint. The wax is then trimmed and the occlusion adjusted (articulating paper can be used on the wax) to establish the desired occlusion (fig. 8). Contacts are established between the flat surface of the splint and all opposing teeth while a shallow, smooth concave ramp is built up in the anterior region to provide immediate, but smooth, disclusion of the posterior teeth on mandibular movement (fig. 9).
Once complete, the maxillary cast is removed from the articulator invested in a flask, the wax boiled out, and then the mould packed with clear acrylic resin which is then processed. The splint is devested, cleaned, trimmed and polished and is then ready for fitting.
Fitting and adjustment
To fit and adjust an occlusal splint will take about 30 minutes. Firstly, the retention is tested and if too tight, acrylic resin is removed with a laboratory carbide bur from the undercut areas around the teeth until the splint seats fully and is adequately retentive. Should the splint exhibit any rocking or lack of seating despite adjustment, it is likely that the casts were inaccurate and new impressions should be made.
Accurate occlusal adjustment requires the use of very thin articulating paper held taut in Millers forceps to ensure that only the actual areas of occlusal contact are marked. The adjustment of the splint is carried out using a large laboratory carbide bur which will adjust the contacts while maintaining a flat occlusal surface. The use of too small a bur will produce indentations in the splint which are undesirable.
Adjustment is carried out with the dental nurse holding two pieces of articulating paper in the patient's mouth and the dentist providing light guidance to the patient's chin with the patient being asked to 'rub forward and back' on the splint. This will guide the mandible toward the retruded position. After marking, the splint is removed and the contacts adjusted until all mandibular teeth make even contact on the splint surface with the mandible in the retruded position. It will probably be impossible at this stage to obtain the correct retruded position because of the state of the patient's neuromuscular system and TMJ's.
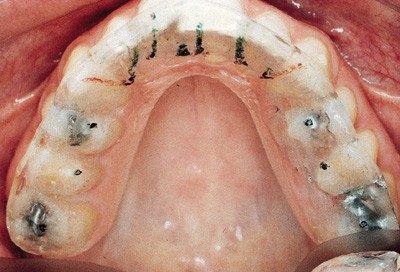
Following establishment of these contacts, the splint is adjusted in lateral and protrusive movements. In lateral movements, the guidance is provided by contact between the mandibular canines and the splint surface (fig. 10), which separates all the other teeth. In protrusive movements, disclusion is provided by even contact between the mandibular incisors and the splint (fig. 10). No other teeth should make contact outside ICP.
Once adjustment is complete, the patient is instructed in how to look after the splint and to wear it as much as possible.
Monitoring splint therapy
If an occlusal splint is being used only as a night guard to protect teeth or restorations it is advisable to review the patient after 7 days to check whether their occlusion has remained stable and to readjust if necessary. After this the splint should be checked at each routine examination.
If the splint is being used to treat mandibular dysfunction or for pre-restorative stabilisation the patient must be reviewed and the splint re-adjusted at weekly intervals for as long as is necessary to achieve a stable retruded position. The time necessary for this to occur may vary from a couple of weeks to several months.
At each adjustment the occlusion is re-examined and the splint readjusted to re-establish even contact and to eliminate excursive interferences. A stable relationship has been achieved when the occlusal contacts marked on the splint remain unchanged for two successive appointments.
If splint therapy were initiated to treat mandibular dysfunction no irreversible alteration to the patient's occlusion (equilibration) is generally needed. The patient may be gradually weaned off the splint but told to wear it if their discomfort returns which is often at times of stress.
If the aim of splint therapy was to stabilise the mandible prior to re-organised restorative treatment, stabilisation of the occlusion on the splint must be followed by an accurate mounting of diagnostic casts in the new maxillo-mandibular relationship. Monitoring the progress of splint therapy is usually carried out by observation of the occlusal contacts on the splint at each adjustment appointment. Prior to more complex restorative procedures and for the purposes of research, the effect the splint has on the stability of the retruded position and other mandibular border movements may be followed very precisely using pantographic tracings of mandibular border movements.3,8,9
The casts, once re-mounted, can then be used to plan and rehearse the restorative procedures. This may necessitate adjustment but will certainly involve diagnostic waxing.
Conclusions
Patients affected by tooth surface loss need protective management. This is based on the elimination, where possible, of the primary cause with careful selection and use of restorative materials to improve or preserve occlusal stability. Where loads on teeth are high, an occlusal splint can be a very effective way of limiting further wear. If preventive strategies have either not been introduced or not complied with, the dentition may be very worn and fixed restorations impossible to provide. Consequently, removable prostheses are frequently used to restore those severely affected by tooth surface loss, Part 4 of the series discusses the principles of their use.
References
Schaerer P, Stallard R E, Zander H A, Occlusal interferences and mastication; an electromyographic study. J Prosthet Dent 1967; 17: 438–449.
Rankow K, Carlsson K, Edlund J, Oberg T . The effect of an occlusal interference on the masticatory system. Odont Revy 1976; 27: 245–256.
Howat A P, Capp N J, Barrett N V J . A colour atlas of occlusion and malocclusion. London: Wolfe Publishing Ltd, 1991. Chapters 2,4,10,11.
Furstman L . The effect of loss of occlusion upon the mandibular joint. Am J Orthod 1965; 51: 1245.
Ramjford S P, Walden J M, Enlow R D . Unilateral function and the temporomandibular joint in Rhesus Monkeys. Oral surg 1971; 32: 237.
Solberg W K, Clark G T, Rugh J D . Nocturnal electromyographic evaluation of bruxism patients undergoing short-term splint therapy. J Oral Rehab 1975; 12: 215–223.
Beard C C, Clayton J A . Effects of occlusal splint therapy on TMJ dysfunctions. J Prosthet Dent 1980; 44: 324.
Shields J M, Clayton J A, Sindledecker L D . Using pantographic tracings to detect TM J and muscle dysfunctions. J Prosthet Dent 1978; 39: 80.
Crispin B J, Myers G E, Clayton J A . Effects of occlusal therapy on pantographic reproducibility of mandibular border movements. J Prosthet Dent 1978; 40: 29–34.
Feinmann C, Harris M . Psychogenic facial pain — Parts I & II. Br Dent J 1984; 156: 165,205.
Forsell H, Kirveskari P, Kangasniemi P . Changes in headache after treatment of mandibular dysfunction Cephalagia. 1985 5: 229–36.
Forsell H, Kirveskari P, Kangasniemi P . Response to occlusal treatment in headache patients previously treated by mock occlusal adjustment. Acta Odont Scand 1987; 45: 77–80.
Nevarro E, Barghi N, Rej R . Clinical evaluation of maxillary hard and resilient occlusal splints. J Dent Res Abstract 1246. Special Issue March 1985.
Anderson G, Schulte J, Goodkind R . Comparative study of two treatment methods for internal derangement of the temporomandibular joint. J Prosthet Dent 1985; 53: 392–397.
Solberg W. K . Temporomandibular disorders. London: BDJ Handbook, 1986, p96.
Capp N J . Temporomandibular joint dysfunction — its relevance to restorative dentistry. Part 2: splint therapy and restorative considerations. Rest Dent 1986: 2; 62–68.
Acknowledgements
The author is most grateful to Mosby-Year Book Europe Ltd for permission to use the illustrations in Figures 1, 2, 8 and 9. This article is based on a presentation at The Medical Society of London on 2 November 1994 as part of the Alpha Omega lecture programme.
The Series Editors are Richard Ibbetson and Andrew Eder of the Eastman Dental Institute for Oral Healthcare Sciences and the Eastman Dental Hospital
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Capp, N. Occlusion and splint therapy. Br Dent J 186, 217–222 (1999). https://doi.org/10.1038/sj.bdj.4800069
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800069
This article is cited by
-
The management of tooth wear with crowns and indirect restorations
British Dental Journal (2018)
-
Unintended changes to the occlusion following the provision of night guards
British Dental Journal (2018)
-
The occlusal splint therapy
international journal of stomatology & occlusion medicine (2009)
-
Patient responses to vacuum formed splints compared to heat cured acrylic splints: pilot study
Journal of Maxillofacial and Oral Surgery (2009)
-
Fitting acrylic occlusal splints and an experimental laminated appliance used in migraine prevention therapy
British Dental Journal (2006)