Abstract
Autoantibodies that bind the N-methyl-D-aspartate receptor (NMDAR) may underlie glutamate receptor hypofunction and related cognitive impairment found in schizophrenia. Exposure to neurotropic pathogens can foster an autoimmune-prone environment and drive systemic inflammation leading to endothelial barrier defects. In mouse model cohorts, we demonstrate that infection with the protozoan parasite, Toxoplasma gondii, caused sustained elevations of IgG class antibodies to the NMDAR in conjunction with compromised blood–gut and blood–brain barriers. In human cohorts, NMDAR IgG and markers of barrier permeability were significantly associated with T. gondii exposure in schizophrenia compared with controls and independently of antipsychotic medication. Combined T. gondii and NMDAR antibody seropositivity in schizophrenia resulted in higher degrees of cognitive impairment as measured by tests of delayed memory. These data underscore the necessity of disentangling the heterogeneous pathophysiology of schizophrenia so that relevant subsets eligible for NMDAR-related treatment can be identified. Our data aid to reconcile conflicting reports regarding a role of pathological NMDAR autoantibodies in this disorder.
Similar content being viewed by others
Introduction
The N-methyl-D-aspartate receptor (NMDAR) is a glutamate receptor that functions in synaptic plasticity and memory formation.1 Altered NMDAR activity has been observed in individuals who exhibit neuropsychiatric symptoms, including those with schizophrenia and mood disorders.2, 3 Although the mechanisms causing NMDAR dysfunction in psychiatric disorders remain unknown, one source may be autoantibodies that target the NMDAR. Anti-NMDAR encephalitis is an autoimmune disorder that involves the production of IgG antibodies directed against the NMDAR.4, 5, 6 Psychosis is a pathological sequela of this condition, thus leading researchers to hypothesize a role for NMDAR autoantibodies in the pathogenesis of psychiatric disorders.4, 5, 6 The examination of NMDAR autoantibodies in case–control cohorts of various psychiatric disorders, however, has produced mixed results, and positive associations of these antibodies with disease have not been uniformly replicated.7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21 The heterogeneous etiology and pathophysiology of polygenic complex brain disorders such as schizophrenia may underlie the failure to detect a straightforward mechanistic contribution of NMDAR autoantibodies to these disorders.
An insult to the blood–brain barrier (BBB) may increase the likelihood that NMDAR autoantibodies produce neuropsychiatric symptoms.21, 22 The experimental infusion of mouse- and human-derived anti-NMDAR antibodies in rodent models leads to hippocampal-dependent memory impairment only once the BBB is perturbed.23, 24 Infectious microbial agents are known to increase BBB permeability in rodents,25, 26 have been associated with elevated NMDAR antibodies in humans with encephalitis22, 27, 28 and are environmental influences that may further tangle the heterogeneity of schizophrenia.29 Exposure to the neurotropic parasitic protozoan, Toxoplasma gondii, in particular, is a putative risk factor for schizophrenia and for the development of cognitive deficits.30, 31 In rodent models, T. gondii infection alters behavior in a parasite strain-dependent manner31, 32, 33, 34, 35, 36 and leads to NMDAR subunit and antibody changes.37, 38
In a parallel examination of mice and humans, our objective was to dissect the NMDAR autoimmune phenotype of schizophrenia in the context of exposure to the infectious parasite, T. gondii. We hypothesized that, as a neurotropic and gut pathogen, T. gondii may promote an inflammatory autoimmune state, which would lead to the production of NMDAR antibodies as well as an avenue of breached cellular barriers via which these autoantibodies would be detrimental to the central nervous system (CNS).
Materials and methods
Study design
The study assessed the inter-relatedness of pathogen antibodies, NMDAR autoantibodies and markers of endothelial barrier permeability as replicated in two rodent models and two human cohorts. The mouse component was composed of one longitudinal cohort of animals infected with two different strains of T. gondii with controls and one cohort infected with activated and inactivated parasites with controls. In these rodent model cohorts, we examined temporal changes in NMDAR autoimmunity and accompanying cellular barrier permeability as generated and replicated by specific strains of T. gondii. The human component was composed of one case–control cohort of individuals with established schizophrenia and controls without a history of psychiatric disorders, and one cohort of individuals with first-episode schizophrenia who were either antipsychotic-naive or had received antipsychotics. In these human psychiatric cohorts, we determined whether the same autoimmune and cellular barrier indices were associated with a schizophrenia diagnosis and whether a combined T. gondii-NMDAR antibody hit led to decreased performance on cognitive tests.
Blood samples from mice and humans were generated from other ongoing studies, and all available samples and related data were included in this investigation to produce the largest possible sample sizes. For mice, prior studies demonstrate very little variance in T. gondii infection status, with designations of positive or negative clearly evident based on antibody levels. Thus, sample sizes of four to five mice screened as positive or negative are routinely adequate for comparisons between infected and uninfected animals. For the human cohort studies, power assessments based on previous case–control comparisons of means and s.d.'s of serum marker levels were undertaken. Cohort 1 had sample sizes that well exceeded minimal power requirements with a power (1−β) of greater than 0.95 and an α of less than 0.001. Cohort 2 had the smallest sample-sized group at n=57, and this size had a sufficient power of 0.80 using an α of less than 0.05.
Mouse experiments
Animals
Male BALB/c mice (Jackson Laboratories, Bar Harbor, ME, USA) were used in these experiments in a controlled laboratory environment. Mice were given free access to food and water for the duration of the experiment and were kept on a 14.5/9.5 h light/dark cycle. Animal protocols were reviewed and approved by the Animal Care and Use Committee at Johns Hopkins University.
Infection
The two T. gondii strains chosen for this study, Prugniaud (PRU) and ME49, are part of the type II genotypic lineage, which is the most common type found in humans in Europe and North America.39 Tachyzoites from PRU and ME49 were maintained and purified as previously described for cohort 1 [ref. 36] and cohort 2.40 Upon arrival at the animal facility, mice were randomly put into one of three cages assigned to be administered either vehicle (control), PRU or ME49 tachyzoites. Cohort 1 mice (4.5 weeks of age) were either mock-infected with Dulbecco's phosphate-buffered saline (DPBS; n=5 mice) or administered 400 purified PRU or ME49 tachyzoites via intraperitoneal injection. One of each of the DPBS- and PRU-infected mice died; final sample sizes were n=4 DPBS, n=4 PRU, n=5 ME49. Cohort 2 mice (5 weeks of age) received either live purified PRU (400 tachyzoites; n=8 mice), 300 000 ultraviolet (UV)-inactivated tachyzoites in alum adjuvant (n=13 mice), alum adjuvant only (n=5 mice) or DPBS only (n=5 mice). Boosters consisting of DPBS, 300 000 UV-inactivated tachyzoites in alum adjuvant, alum adjuvant only or DPBS, respectively, were administered at 12 days post infection.
Serum collection
For cohort 1, blood was collected via tail clip at eight time points—0, 2, 4, 6, 8, 12, 16 and 20 weeks post infection (wpi). For cohort 2, blood was collected at 19 wpi. The blood was centrifuged at 10 000 g to separate the serum. Serum was stored at −80 °C until needed. Serum was coded and further studies were run blinded by separate investigators.
Immunoassays
Using enzyme-linked immunosorbent assays, serum IgG antibodies were measured for T. gondii, NMDAR subunit GLUN2 and gluten.37, 41 Gluten antibodies served as a marker of cytological damage and gut barrier permeability.41, 42, 43 Serum levels of the glial-specific S100B protein served as a marker of CNS barrier dysfunction.44, 45 S100B measurements were carried out according to the manufacturer’s instructions (antibodies-online.com, Atlanta, GA, USA). Each 96-well plate tested contained kit standards as well as study sample replicates for use as internal controls of reproducibility.
Human participants
Human studies were approved by the Institutional Review Boards of the Sheppard Pratt Health System, University of Cologne, Heidelberg University and the Johns Hopkins Medical Institution following established guidelines. All participants provided written informed consent after study procedures were explained. The work was carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
Human cohort 1—Sheppard Pratt, Baltimore, MD, USA
We retrieved available data previously generated for T. gondii IgG, NMDAR IgG, gluten IgG, S100B and cognitive tests for people with schizophrenia and controls in the study cohort. Methods and analyses reporting psychiatric case and control levels of T. gondii IgG, NMDAR IgG and gluten IgG were previously published for subsets of this cohort.14, 46, 47 Cognitive functioning was assessed with the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS).48 This cohort was composed of 899 sample results (n=297 controls, n=602 schizophrenia). S100B data were available for a subset (n=112 controls, n=237 schizophrenia) and measures were derived using a multianalyte immunoassay platform.49
Methods for identifying and characterizing individuals of diagnostic groups according to criteria defined by DSM-IV50 have been previously described.46 To be included in the schizophrenia group, individuals received a DSM-IV diagnosis of schizophrenia, schizophreniform disorder or schizoaffective disorder. Inclusion criteria required an age between 18 and 65 years. Individuals without a history of psychiatric disorder were recruited from posted announcements and were screened to rule out current or past psychiatric disorders with the Structured Clinical Interview for DSM-IV Axis I Disorders Non-Patient Edition.51 Control participants were between the ages of 20 and 60 years, inclusive. Exclusion criteria for all participants included the following: history of intravenous substance abuse; mental retardation; and clinically significant medical disorder that would affect cognitive performance. For psychiatric participants, having a primary diagnosis of substance abuse or dependence was an exclusion criterion. Basic demographic data for this study population are shown in Table 1. The mean±s.e. duration of illness onset for this schizophrenia cohort at the time when blood was drawn was 18.99±0.48 years.
Human cohort 2—University of Cologne/Central Institute of Mental Health
The methods for identifying and characterizing individuals with a first episode of schizophrenia according to criteria defined by DSM-IV were previously described.52 Biomarker data for T. gondii and gluten IgG were obtained from previous analyses of this cohort.53, 54 NMDAR GLUN2 antibodies and S100B levels were measured using commercially available enzyme-linked immunosorbent assay kits (CIS Biotech, Decatur, GA, USA; EMD Millipore, Darmstadt, Germany). Seventy-six of these patients were antipsychotic-naive and 57 were currently receiving antipsychotic medication. Individuals were excluded if they had a relevant comorbidity such as heart disease, liver cirrhosis, known immune-mediated disease (such as multiple sclerosis) or history of substance dependence. Demographic data regarding age and sex are listed in Table 1. The region from which patients were recruited was generally homogenous with respect to socioeconomic characteristics.
Statistical analyses
Data were checked for normality and equal variance, and all subsequent analyses were carried out using STATA version 12 (STATA, College Station, TX, USA). Data analyses were performed blinded to group identities. For quantitative antibody data in mouse cohort 1 kinetic experiments, repeated measures analysis of variance (ANOVAs) were applied to identify significant differences in antibody levels among groups according to time and infection status. Interstrain differences in marker levels at each time point were examined with t-tests. Mouse cohort 2 intergroup data differences were tested with ANOVAs and t-tests.
In the human cohort analyses, absorbance levels were normalized per plate by the mean value of controls, as previously described.55 Parallel analyses of non-normalized data and use of assay plate designations to correct plate-to-plate variation were also evaluated in multivariate analyses. Multiple linear regressions (MLRs) corrected for demographic variables were used to identify significant correlations of T. gondii and NMDAR antibody levels. For cohort 1, multivariate regressions incorporating gluten IgG, S100B and RBANS cognitive scores were applied to confirm significance of all markers within the model. Demographic covariates of age, sex and race were included for cohort 1; age and sex were included for cohort 2.
Dichotomous marker seropositivity was established based on three cutoff values to maximize detection of informative data. For the human cohort 1, cutoff values corresponded to absorbances of 75, 90 and 95% control values, which represented an increasing degree of stringency for demarcating seropositivity. Because there were no control values for human cohort 2, we examined seropositivity based on a combination of control values in cohort 1, a series of s.d.'s above the mean and a visual inspection of cohort 2 data where a natural bifurcation of the data is evident for T. gondii. T-tests were used to detect significant differences between marker levels for those who were seropositive versus those who were seronegative for T. gondii and NMDAR IgG. χ2-tests were used to identify differences in categorical diagnostic and demographic data sets. P-values less than 0.05 were considered statistically significant. One- versus two-tailed t-test results are indicated; one-tailed t-tests were justified because marker elevations with T. gondii seropositivity were expected.
Results
T. gondii infection produced sustained, strain-specific, anti-NMDAR immune responses
Animals infected with either T. gondii strain sustained a parasite-directed immune response for the entire duration of the 20-week study (Figure 1a; repeated measures ANOVA, between infected versus uninfected groups, F=1288.13, P⩽0.0001; time-by-infection group interaction, F=80.74, P⩽0.0001). Over this same time period, both strain types elicited an increase in NMDAR GLUN2 antibodies compared with mock-infected controls, with one peak at 4 wpi and a second at 12 wpi (Figure 1b; repeated measures ANOVA, between groups, F=18.90, P⩽0.0002; time-by-infection group interaction, F=11.17, P⩽0.0001). The early 4-wpi peak in GLUN2 IgG levels was particularly strong for ME49-infected mice, with levels significantly increased compared with the PRU group (Figure 1b; t-test, t=3.58, two-tailed P⩽0.007).
T. gondii infection in mice produces antibodies that react with the GLUN2 subunit of the NMDAR. Infection with PRU and ME49 strains of T. gondii caused significant increases in the mean serum IgG antibody levels to total T. gondii (a) and to NMDAR GLUN2 (b). DPBS, n=4; PRU, n=4; ME49, n=5. Error bars represent s.e.m. A red asterisk (*) indicates significant differences over time according to the infection group in repeated measures ANOVAs. A blue asterisk (*) indicates significant differences in NMDAR antibodies between PRU and ME49 mice at individual time points with t-tests. PRU mice infected with live parasite and inactivated parasite had elevated T. gondii antibodies compared with DPBS and adjuvant controls (c). Only mice infected with live T. gondii had elevated levels of IgG to the NMDAR GLUN2 (d). Dashed line represents the mean antibody levels. A red asterisk (*) indicates significant differences between infection groups in ANOVAs. ANOVA, analysis of variance; DPBS, Dulbecco's phosphate-buffered saline; NMDAR, N-methyl-D-aspartate receptor.
In the second cohort, both live and UV-inactivated parasites potently produced anti-T. gondii IgG (Figure 1c; ANOVA, F=31.70, P⩽0.0001). However, only infection with the live strain resulted in antibodies that recognized the GLUN2 subunit of the NMDAR (Figure 1d; ANOVA, F=12.05, P⩽0.0001).
NMDAR antibody associations with T. gondii in two schizophrenia cohorts
In the first clinical cohort, NMDAR IgG levels in T. gondii-seropositive people with schizophrenia were consistently elevated across three different assay cutoff values compared with seronegative counterparts (Figure 2a; shown are results for the 95% cutoff value, t-test, t=3.84, two-tailed P⩽0.0001). NMDAR IgG levels were also significantly greater in T. gondii-seropositive people with schizophrenia than T. gondii-seropositive controls (75% control cutoff, t-test, t=2.16, two-tailed P⩽0.03). In multivariate regression analyses, quantitative T. gondii and NMDAR IgG levels were significantly correlated in schizophrenia but not in controls (Figure 2b; MLR, age, sex, race-corrected, coefficient=0.73, 95% confidence interval (CI) 0.45–1.01, P⩽0.0001). Separately, T. gondii and NMDAR IgG levels and seropositivity percentages were not significantly different between individuals with schizophrenia compared with controls. Seropositivity estimates for people with schizophrenia corresponding to the 75, 90 and 95% control cutoff values were 24.1, 10.5 and 8.5% for T. gondii IgG and 22, 11.1 and 8.1% for NMDAR IgG, respectively.
NMDA receptor antibodies in T. gondii-seropositive individuals with schizophrenia. Levels of NMDAR IgG were significantly elevated in individuals with schizophrenia who were T. gondii-seropositive (Tg+) compared with those who were T. gondii-seronegative (Tg−) and compared with controls who were Tg+ (a). There were no significant differences between diagnostic groups for individuals who were Tg−. Error bars represent s.e.m. In multiple linear regressions corrected for age, sex and race, T. gondii and NMDAR antibodies were significantly correlated in individuals with schizophrenia, but not controls (b). Levels of NMDAR IgG were also significantly elevated in antipsychotic-naive individuals with first-episode schizophrenia who were Tg+ compared with those who were Tg−. No differences in NMDAR IgG levels were detected between T. gondii seropositivity groups who were medicated (c). T. gondii and NMDAR antibodies were significantly correlated in the antipsychotic-naive, but not medicated, group of first-episode individuals. The correlation became significant (blue dashed line) in the medicated group when one outlier (circled in blue) was removed (d). A red or blue asterisk (*) indicates significant associations of antibody levels or seropositivity in t-tests or multiple linear regressions. NMDAR, N-methyl-D-aspartate receptor.
In the second cohort, T. gondii-seropositive patients with first-episode schizophrenia who were antipsychotic-naive had significantly elevated NMDAR IgG levels compared with those who were T. gondii-seronegative (Figure 2c; t-test, t=2.31, two-tailed P⩽0.02). There were no differences in NMDAR IgG levels between medicated T. gondii-seropositive patients versus medicated seronegative patients. MLRs corrected for age and sex showed significant correlations between T. gondii and NMDAR IgG in the antipsychotic-naive group (Figure 2d; MLRs, AP-naive, coefficient=1.02, 95% CI 0.24–1.80, P⩽0.01). In the medicated group, initial analyses showed no significant correlations between parasite and receptor IgG. To determine whether one extremely high NMDAR IgG value was having a negative impact on the correlation, we re-performed the data analyses with the outlier removed. Although basic differences in the mean levels of NMDAR antibodies between the T. gondii-seropositive and -seronegative medicated subgroups did not significantly change, we found that the correlation between T. gondii IgG and receptor antibody levels in the group receiving medication was now statistically significant (Figure 2d; MLRs, AP+, coefficient=1.35, 95% CI 0.09–2.60, P⩽0.04).
Blood–gut barrier and BBB permeability in T. gondii-exposed mice
To explore the possibility that the mechanisms driving the production of NMDAR autoantibodies require permeability at blood–gut barrier and BBB, we quantified the levels of two surrogate markers of gut and CNS endothelial barrier dysfunction, gluten IgG and S100B, respectively. Both gluten IgG and S100B levels were significantly elevated in infected mice throughout the 20-week study (Figures 3a and b; repeated measures ANOVA, between groups, gluten F=82.51, P⩽0.0001, S100B F=113.75, P⩽0.0001; time-by-infection group interaction, gluten F=3.77, P⩽0.0001, S100B F=3.53, P⩽0.0002). We also found strain-specific differences at individual time points for gluten IgG, with levels significantly elevated in ME49 compared with PRU at 8 wpi (t-test, t=2.04, one-tailed P⩽0.04), and then significantly decreased at the later time points, 16 and 20 wpi (t-test, t=2.69–3.52, two-tailed P⩽0.01–0.03).
Blood–gut barrier and BBB permeability markers in T. gondii-infected mice and in T. gondii-seropositive individuals with schizophrenia. Infection with PRU and ME49 strains of T. gondii caused significant increases in the mean serum IgG antibody levels to gluten (a), and in the mean levels of the glial protein S100B, a marker often used as a measure of blood–brain barrier permeability (b). DPBS, n=4; PRU, n=4; ME49, n=5. Error bars represent s.e.m. A red asterisk (*) indicates significant differences over time and according to the infection group in repeated measures ANOVAs. A blue asterisk (*) indicates significant differences in gluten antibodies between PRU and ME49 mice at individual time points. Levels of gluten IgG were significantly elevated in individuals with schizophrenia who were T. gondii-positive (Tg+) compared with those who were T. gondii-negative (Tg−; c). Levels of S100B were significantly elevated in individuals with schizophrenia who were Tg+ compared with controls who were Tg+ (d). There were no significant differences between diagnostic groups for individuals who were Tg−. Error bars represent s.e.m. A red asterisk (*) indicates significant differences between infection and seropositivity groups in repeated measures ANOVAs and t-tests. ANOVA, analysis of variance; DPBS, Dulbecco's phosphate-buffered saline.
T. gondii exposure and blood–gut barrier and BBB permeability in schizophrenia
Gluten IgG was significantly elevated in T. gondii-seropositive individuals with schizophrenia compared with seronegative ones (Figure 3c; 95% cutoff value shown, t-test, both t=1.79, one-tailed P⩽0.04). For S100B, levels were significantly elevated in T. gondii-seropositive individuals with schizophrenia compared with seropositive controls (Figure 3d; t-test, t=2.23, two-tailed P⩽0.028). In multivariate regression analyses incorporating gluten IgG and S100B in addition to age, sex and race, quantitative T. gondii and NMDAR IgG levels were significantly correlated in schizophrenia but not in controls (MLR, coefficient=0.89 (previously 0.73), 95% CI 0.52–1.27, P⩽0.0001).
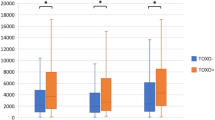
Combined T. gondii and NMDAR seropositivity has an adverse impact on cognitive functioning in schizophrenia
We found significant decreases in scores on the delayed memory index of RBANS for cohort 1 people with schizophrenia who were seropositive for both T. gondii and NMDAR antibodies compared with those who were not seropositive for both antigens (Figure 4; 90% cutoff shown, t-test, t=1.72, one-tailed P⩽0.04). Individuals who were seropositive for only one antibody marker did not yield significant differences in memory scores compared with those who were seronegative. Delayed memory scores were significantly inversely correlated with both T. gondii and NMDAR antibody levels in regressions corrected for age, sex and race (T. gondii: coefficient=−3.69, 95% CI −7.31 to −0.08; NMDAR: coefficient=−1.56, 95% CI −3.07 to −0.05; P⩽0.04).
Combined seropositivity to T. gondii and NMDAR antibodies contributes to decreased memory scores on tests of cognition. Individuals who were seropositive for both T. gondii and NMDAR antibodies (Both+) had decreased performance on the delayed memory module of RBANS compared to individuals who were not seropositive to both (One/none+). Delayed memory scores were not significantly altered between individuals who were T. gondii-seropositive (Tg+) compared with those who were seronegative (Tg−) or between individuals who were NMDAR IgG-seropositive (NMDAR+) compared with those who were seronegative (NMDAR−). A red asterisk (*) indicates significant differences between seropositivity groups. Fourteen individuals positive for both (Both+) were removed from the single marker analyses. NMDAR, N-methyl-D-aspartate receptor; RBANS, Repeatable Battery for the Assessment of Neuropsychological Status.
Discussion
Investigations of NMDAR autoantibodies as agents that suppress glutamatergic function in schizophrenia have yielded mixed results, a phenomenon that likely reflects the complex etiological and pathophysiological heterogeneity of the disorder. In this study, we identified a subgroup of individuals with schizophrenia who had NMDAR autoantibodies that were associated with exposure to the infectious parasite, T. gondii. We further established that the T. gondii-NMDAR antibody correlations were not simply a medication effect attributable to antipsychotics. T. gondii enters the body through the gut and over the course of infection, disseminates into host circulation and eventually travels to the brain where it enters a dormant stage.56 As such, T. gondii has the ability to cross both the blood–gut barrier and BBB, and here we show that these compromised vascular barriers were significantly associated with infection by this parasite in individuals with schizophrenia. Control individuals did not show similar autoantibody or barrier associations with infection, suggesting an inherent predisposition of certain people with schizophrenia to dysfunctions that contribute to an autoimmune state or pathways that have an impact on cellular barrier integrity. Much of the recent genetic evidence points to the human leukocyte antigen region of chromosome 6 as housing immune-related susceptibility loci for schizophrenia.57, 58
The human cohorts examined in the present investigation represented different stages of schizophrenia. Cohort 1 reflects a relatively established disease state with all individuals currently receiving antipsychotic medications and cohort 2 a more recent onset phase of individuals with first-episode schizophrenia including people who were antipsychotic-naive. The cohorts also differed with respect to culture, socioeconomics and geography, with cohort 1 derived from the metropolitan area of Baltimore, MD, USA, and cohort 2 originating from the German cities of Cologne and Mannheim. Technical differences in study design and sample collection and processing at the two sites likely also introduced variability to the measured immunoassay responses. In spite of these differences, we demonstrated in both cohorts an association between pathogen exposure and antibodies that recognize the NMDAR. We would expect that the findings from our analyses of a well-treated chronic disease population such as cohort 1 might be best replicated in the cohort 2 individuals who were receiving antipsychotics. However, this connection was not immediately evident and was only measurable in the medicated first-episode cohort 2 group, when one outlier was removed. Nevertheless, in the cohort 2 antipsychotic-naive group, which arguably represents an early stage, less confounded state of the disease, the association between pathogen exposure and NMDAR antibodies was readily detectable.
In the mouse cohorts, we verified the causality of infection by T. gondii with the sustained production of antibodies against the NMDAR. The presence of such autoantibodies in the CNS would have an obvious impact on NMDAR functioning, and others have shown that high levels of these antibodies lead to neuronal death and cognitive dysfunction in vivo.3, 23, 24 The mechanism of NMDAR antibody pathogenicity presumably occurs via antibody capping and internalization of the receptor.6 Previously, we observed downregulated NMDAR expression in brains of T. gondii-infected juvenile mice, and these expression changes corresponded with increases in serum NMDAR antibodies.37 In the present study, both strains of T. gondii caused NMDAR antibody upregulation during the initial acute phase of infection, and which was maintained across timescales that reflect long-term infection. These data suggest that NMDAR autoantibody pathogenicity could persist significantly after the initial exposure to the parasite. Interestingly, however, we also observed T. gondii strain-specific differences that were consistent with previous findings that ME49, but not PRU, altered aspects of mouse behavior and cognition.31, 36 Here, ME49-infected mice produced a stronger and earlier anti-NMDAR immune response than the PRU-infected mice. Gut barrier permeability also seemed to be achieved earlier with the ME49 strain compared with PRU.
We further found that NMDAR autoantibodies were only generated following infection with live, fully functional parasites, compared with parasites that were UV-inactivated. These results may suggest that the antibodies produced against the parasite itself were not cross-reactive to the receptor. It is possible, however, that an antigenic mimic of NMDAR is expressed by a later stage of the parasite, such as during the dormant cyst phase and that this antigen was not generated by UV-inactivated parasites arrested earlier during the cell cycle.
Our mouse and human data support that T. gondii caused elevations of gluten IgG and S100B, markers that are surrogates for gut–blood barrier and BBB dysfunction, respectively. Infection-related BBB permeability would enable access to the brain where anti-NMDAR antibodies could presumably be generated and act at their final CNS destination. Another interpretation introduces a scenario whereby all of the processes discussed in the paper converge to the intestinal tract. NMDARs are present in the enteric nervous system where the receptors are involved in visceral pain associated with colitis.59 Initial infection with this parasite creates an inflammatory intestinal environment that could expose novel immunogenic triggers composed of enteric NMDARs complexed with other gut cellular, dietary or microbial antigens. Transit of the pathogen to the brain to generate antibodies against the NMDAR, thus, would not be required. Although S100B is often used as a surrogate measure of BBB permeability,44, 45 the gut has its own enteric glial network capable of producing S100B.60, 61 The kinetic profiles from our gluten IgG and S100B kinetic studies may support this proposed mechanism, with S100B peaking earliest of all markers at 2 wpi. A number of disorders of the intestinal tract have an autoimmune component (for example, celiac disease, Crohn’s disease and ulcerative colitis) and increasingly psychiatric symptoms are being reported in a subset of people afflicted with intestinal conditions.62, 63, 64, 65
The extent to which our results can be interpreted are limited by several issues. It is notoriously difficult to reproduce promising biological data generated from human specimens of heterogeneous diseases. Although we included two clinical cohorts, some of our statistical analyses were exploratory and were not subjected to multiple comparison corrections. The main results, however, connecting infection with receptor autoantibodies were strong in the human comparisons especially with the more rigorous multifactorial regressions. Furthermore, our modeling of this connectome in two cohorts of mice produced highly statistically significant results, providing verification of a sound mechanism. Another factor to consider is that the assay used recorded activity only of antibodies that recognize the GLUN2 subunit of the NMDAR. Others have previously proposed that the NMDAR autoantibody response in schizophrenia might be distinct from the classic anti-NMDAR encephalitis due to a disease-specific differential recognition of GLUN1 versus GLUN2.6 It will also be necessary to further study these patterns longitudinally in humans and to do so with a larger array of gut biomarkers, such as with other measures of intestinal inflammation, dietary and microbial translocation and microbiome imbalances. The identification and development of biomarkers of BBB dissolution that do not reflect components of the enteric nervous system are also necessary.
To put these findings into perspective, we envision that the continued identification and use of a combination of serological biomarkers will help define distinct subsets of individuals who may benefit from refined individualized therapeutic strategies. The NMDAR represents an attractive pharmacological treatment target for use in psychiatric disorders because of a well-studied array of receptor agonists, antagonists and modulators available to evaluate its function. The anesthetic ketamine, a receptor antagonist, is currently a hotly evaluated treatment, especially of depression, and it is approved for other indications. It is believed to improve glutamatergic transmission through the increased release of glutamate.66, 67 Hypofunction of the NMDAR in schizophrenia could involve a range of insufficiencies including that of the primary ligand glutamate, its binding partner glycine or D-serine or it may be that densities of actual functional receptors in this disorder are unusually sparse. In order for the correct pharmacological treatment to be clinically tested and developed, however, the appropriate patient population afflicted by an NMDAR pathology needs to be identified. On the basis of our work, the identification of those exposed to T. gondii and possibly other intestinal pathogens is also warranted to further fine-tune treatment strategies.
In conclusion, we provide mechanistic evidence that exposure to the pathogen, T. gondii, produced an anti-NMDAR immune response that was accompanied by endothelial barrier dysfunction in both the gut and the CNS, using biomarkers that were similarly informative in both mouse and human studies. In the subset of patients identified in this study, those who tested positive for both NMDAR and pathogen antibodies had reduced scores on memory modules of the RBANS measures of cognition. Taken together, these data help to further refine proposed inclusion criteria for participation in studies of NMDAR antibodies in schizophrenia, by requiring the identification of past exposures to infectious agents and other causes of endothelial barrier compromise. Our better understanding of NMDAR mechanisms in schizophrenia will in turn lead to more applicable treatments based on this well-studied and modifiable pharmacological target.
References
Stephenson FA, Cousins SL, Kenny AV . Assembly and forward trafficking of NMDA receptors (Review). Mol Membr Biol 2008; 25: 311–320.
Lakhan SE, Caro M, Hadzimichalis N . NMDA receptor activity in neuropsychiatric disorders. Front Psychiatry 2013; 4: 52.
Faust TW, Chang EH, Kowal C, Berlin R, Gazaryan IG, Bertini E et al. Neurotoxic lupus autoantibodies alter brain function through two distinct mechanisms. Proc Natl Acad Sci USA 2010; 107: 18569–18574.
Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 2008; 7: 1091–1098.
Dalmau J, Tuzun E, Wu HY, Masjuan J, Rossi JE, Voloschin A et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol 2007; 61: 25–36.
Kayser MS, Dalmau J . Anti-NMDA receptor encephalitis, autoimmunity, and psychosis. Schizophr Res 2016; 176: 36–40.
Dahm L, Ott C, Steiner J, Stepniak B, Teegen B, Saschenbrecker S et al. Seroprevalence of autoantibodies against brain antigens in health and disease. Ann Neurol 2014; 76: 82–94.
Masdeu JC, Gonzalez-Pinto A, Matute C, Ruiz De Azua S, Palomino A, De Leon J et al. Serum IgG antibodies against the NR1 subunit of the NMDA receptor not detected in schizophrenia. Am J Psychiatry 2012; 169: 1120–1121.
Masopust J, Andrys C, Bazant J, Vysata O, Kuca K, Valis M . Anti-NMDA receptor antibodies in patients with a first episode of schizophrenia. Neuropsychiatr Dis Treat 2015; 11: 619–623.
Pollak TA, McCormack R, Peakman M, Nicholson TR, David AS . Prevalence of anti-N-methyl-D-aspartate (NMDA) receptor [corrected] antibodies in patients with schizophrenia and related psychoses: a systematic review and meta-analysis. Psychol Med 2014; 44: 2475–2487.
Rhoads J, Guirgis H, McKnight C, Duchemin AM . Lack of anti-NMDA receptor autoantibodies in the serum of subjects with schizophrenia. Schizophr Res 2011; 129: 213–214.
Steiner J, Walter M, Glanz W, Sarnyai Z, Bernstein HG, Vielhaber S et al. Increased prevalence of diverse N-methyl-D-aspartate glutamate receptor antibodies in patients with an initial diagnosis of schizophrenia: specific relevance of IgG NR1a antibodies for distinction from N-methyl-D-aspartate glutamate receptor encephalitis. JAMA Psychiatry 2013; 70: 271–278.
Pearlman DM, Najjar S . Meta-analysis of the association between N-methyl-d-aspartate receptor antibodies and schizophrenia, schizoaffective disorder, bipolar disorder, and major depressive disorder. Schizophr Res 2014; 157: 249–258.
Dickerson F, Stallings C, Vaughan C, Origoni A, Khushalani S, Yolken R . Antibodies to the glutamate receptor in mania. Bipolar Disord 2012; 14: 547–553.
Timucin D, Ozdemir O, Parlak M . The role of NMDAR antibody in the etiopathogenesis of schizophrenia. Neuropsychiatr Dis Treat 2016; 12: 2327–2332.
Ando Y, Shimazaki H, Shiota K, Tetsuka S, Nakao K, Shimada T et al. Prevalence of elevated serum anti-N-methyl-D-aspartate receptor antibody titers in patients presenting exclusively with psychiatric symptoms: a comparative follow-up study. BMC Psychiatry 2016; 16: 226.
Haussleiter IS, Emons B, Schaub M, Borowski K, Brune M, Wandinger KP et al. Investigation of antibodies against synaptic proteins in a cross-sectional cohort of psychotic patients. Schizophr Res 2012; 140: 258–259.
Zandi MS, Irani SR, Lang B, Waters P, Jones PB, McKenna P et al. Disease-relevant autoantibodies in first episode schizophrenia. J Neurol 2011; 258: 686–688.
Steiner J, Teegen B, Schiltz K, Bernstein HG, Stoecker W, Bogerts B . Prevalence of N-methyl-D-aspartate receptor autoantibodies in the peripheral blood: healthy control samples revisited. JAMA Psychiatry 2014; 71: 838–839.
de Witte LD, Hoffmann C, van Mierlo HC, Titulaer MJ, Kahn RS, Martinez-Martinez P et al. Absence of N-methyl-D-aspartate receptor igg autoantibodies in schizophrenia: the importance of cross-validation studies. JAMA Psychiatry 2015; 72: 731–733.
Castillo-Gomez E, Oliveira B, Tapken D, Bertrand S, Klein-Schmidt C, Pan H et al. All naturally occurring autoantibodies against the NMDA receptor subunit NR1 have pathogenic potential irrespective of epitope and immunoglobulin class. Mol Psychiatry 2016; e-pub ahead of print 9 August.
Hammer C, Stepniak B, Schneider A, Papiol S, Tantra M, Begemann M et al. Neuropsychiatric disease relevance of circulating anti-NMDA receptor autoantibodies depends on blood-brain barrier integrity. Mol Psychiatry 2014; 19: 1143–1149.
Kowal C, Degiorgio LA, Lee JY, Edgar MA, Huerta PT, Volpe BT et al. Human lupus autoantibodies against NMDA receptors mediate cognitive impairment. Proc Natl Acad Sci USA 2006; 103: 19854–19859.
Kowal C, DeGiorgio LA, Nakaoka T, Hetherington H, Huerta PT, Diamond B et al. Cognition and immunity; antibody impairs memory. Immunity 2004; 21: 179–188.
Chaudhuri JD . Blood brain barrier and infection. Med Sci Monit 2000; 6: 1213–1222.
Chai Q, He WQ, Zhou M, Lu H, Fu ZF . Enhancement of blood-brain barrier permeability and reduction of tight junction protein expression are modulated by chemokines/cytokines induced by rabies virus infection. J Virol 2014; 88: 4698–4710.
Pruss H, Finke C, Holtje M, Hofmann J, Klingbeil C, Probst C et al. N-methyl-D-aspartate receptor antibodies in herpes simplex encephalitis. Ann Neurol 2012; 72: 902–911.
Armangue T, Leypoldt F, Malaga I, Raspall-Chaure M, Marti I, Nichter C et al. Herpes simplex virus encephalitis is a trigger of brain autoimmunity. Ann Neurol 2014; 75: 317–323.
Yolken RH, Torrey EF . Are some cases of psychosis caused by microbial agents? A review of the evidence. Mol Psychiatry 2008; 13: 470–479.
Torrey EF, Bartko JJ, Yolken RH . Toxoplasma gondii and other risk factors for schizophrenia: an update. Schizophr Bull 2012; 38: 642–647.
Kannan G, Pletnikov MV Toxoplasma gondii and cognitive deficits in schizophrenia: an animal model perspective. Schizophr Bull 2012; 38: 1155–1161.
Flegr J . Effects of Toxoplasma on human behavior. Schizophr Bull 2007; 33: 757–760.
Flegr J, Havlicek J, Kodym P, Maly M, Smahel Z . Increased risk of traffic accidents in subjects with latent toxoplasmosis: a retrospective case-control study. BMC Infect Dis 2002; 2: 11.
Flegr J, Zitkova S, Kodym P, Frynta D . Induction of changes in human behaviour by the parasitic protozoan Toxoplasma gondii. Parasitology 1996; 113 (Pt 1): 49–54.
Webster JP . Rats, cats, people and parasites: the impact of latent toxoplasmosis on behaviour. Microbes Infect 2001; 3: 1037–1045.
Kannan G, Moldovan K, Xiao JC, Yolken RH, Jones-Brando L, Pletnikov MV . Toxoplasma gondii strain-dependent effects on mouse behaviour. Folia Parasitol 2010; 57: 151–155.
Kannan G, Crawford JA, Yang C, Gressitt KL, Ihenatu C, Krasnova IN et al. Anti-NMDA receptor autoantibodies and associated neurobehavioral pathology in mice are dependent on age of first exposure to Toxoplasma gondii. Neurobiol Dis 2016; 91: 307–314.
Severance E, Kannan G, Dickerson F, Pletnikov M, Yolken R . Antibodies to food antigens: translational research in psychiatric disorders. Neurol Psychiatr Brain Res 2012; 18: 87–88.
Sibley LD, Ajioka JW . Population structure of Toxoplasma gondii: clonal expansion driven by infrequent recombination and selective sweeps. Annu Rev Microbiol 2008; 62: 329–351.
Kannan G, Prandovszky E, Steinfeldt CB, Gressitt KL, Yang C, Yolken RH et al. One minute ultraviolet exposure inhibits Toxoplasma gondii tachyzoite replication and cyst conversion without diminishing host humoral-mediated immune response. Exp Parasitol 2014; 145: 110–117.
Severance EG, Kannan G, Gressitt KL, Xiao J, Alaedini A, Pletnikov MV et al. Anti-gluten immune response following Toxoplasma gondii infection in mice. PLoS ONE 2012; 7: e50991.
Uhde M, Ajamian M, Caio G, De Giorgio R, Indart A, Green PH et al. Intestinal cell damage and systemic immune activation in individuals reporting sensitivity to wheat in the absence of coeliac disease. Gut 2016; 65: 1930–1937.
Stenberg R, Dahle C, Magnuson A, Hellberg D, Tysk C . Increased prevalence of antibodies against dietary proteins in children and young adults with cerebral palsy. J Pediatr Gastroenterol Nutr 2013; 56: 233–238.
Koh SX, Lee JK . S100B as a marker for brain damage and blood-brain barrier disruption following exercise. Sports Med 2014; 44: 369–385.
Blyth BJ, Farhavar A, Gee C, Hawthorn B, He H, Nayak A et al. Validation of serum markers for blood-brain barrier disruption in traumatic brain injury. J Neurotrauma 2009; 26: 1497–1507.
Dickerson F, Stallings C, Origoni A, Katsafanas E, Schweinfurth L, Savage C et al. Antibodies to Toxoplasma gondii and cognitive functioning in schizophrenia, bipolar disorder, and nonpsychiatric controls. J Nerv Ment Dis 2014; 202: 589–593.
Dickerson F, Stallings C, Origoni A, Vaughan C, Khushalani S, Leister F et al. Markers of gluten sensitivity and celiac disease in recent-onset psychosis and multi-episode schizophrenia. Biol Psychiatry 2010; 68: 100–104.
Randolph C . RBANS Manual - Repeatable Battery for the Assessment of Neuropsychological Status. Psychological Corporation: San Antonio, TX, USA, 1998.
Dickerson F, Schroeder J, Stallings C, Origoni A, Bahn S, Yolken R . Multianalyte markers of schizophrenia and bipolar disorder: a preliminary study. Schizophr Res 2015; 168: 450–455.
DSM-IV Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. 4th edn, American Psychiatric Association: Washington, DC, USA, 1994, xxvii 886.
First MB, Spitzer RL, Gibbon M, Williams JBW . Structured Clinical Interview for DSM-IV Axis I Disorders - Non-patient Edition (SCID I/NP). Biometrics Research, New York State Psychiatric Institute: New York, NY, USA, 1998.
Leweke FM, Gerth CW, Koethe D, Klosterkotter J, Ruslanova I, Krivogorsky B et al. Antibodies to infectious agents in individuals with recent onset schizophrenia. Eur Arch Psychiatry Clin Neurosci 2004; 254: 4–8.
Severance EG, Alaedini A, Yang S, Halling M, Gressitt KL, Stallings CR et al. Gastrointestinal inflammation and associated immune activation in schizophrenia. Schizophr Res 2012; 138: 48–53.
Severance EG, Gressitt KL, Alaedini A, Rohleder C, Enning F, Bumb JM et al. IgG dynamics of dietary antigens point to cerebrospinal fluid barrier or flow dysfunction in first-episode schizophrenia. Brain Behav Immun 2015; 44: 148–158.
Severance EG, Dickerson FB, Halling M, Krivogorsky B, Haile L, Yang S et al. Subunit and whole molecule specificity of the anti-bovine casein immune response in recent onset psychosis and schizophrenia. Schizophr Res 2010; 118: 240–247.
Severance EG, Xiao J, Jones-Brando L, Sabunciyan S, Li Y, Pletnikov M et al. Toxoplasma gondii-A gastrointestinal pathogen associated with human brain diseases. Int Rev Neurobiol 2016; 131: 143–163.
Sekar A, Bialas AR, de Rivera H, Davis A, Hammond TR, Kamitaki N et al. Schizophrenia risk from complex variation of complement component 4. Nature 2016; 530: 177–183.
Consortium SWGotPG. Biological insights from 108 schizophrenia-associated genetic loci. Nature 2014; 511: 421–427.
Zhou Q, Nicholas Verne G . NMDA receptors and colitis: basic science and clinical implications. Rev Analg 2008; 10: 33–43.
Esposito G, Cirillo C, Sarnelli G, De Filippis D, D'Armiento FP, Rocco A et al. Enteric glial-derived S100B protein stimulates nitric oxide production in celiac disease. Gastroenterology 2007; 133: 918–925.
Cirillo C, Sarnelli G, Esposito G, Turco F, Steardo L, Cuomo R . S100B protein in the gut: the evidence for enteroglial-sustained intestinal inflammation. World J Gastroenterol 2011; 17: 1261–1266.
Gupta S, Masand PS, Kaplan D, Bhandary A, Hendricks S . The relationship between schizophrenia and irritable bowel syndrome (IBS). Schizophr Res 1997; 23: 265–268.
Filipovic BR, Filipovic BF . Psychiatric comorbidity in the treatment of patients with inflammatory bowel disease. World J Gastroenterol 2014; 20: 3552–3563.
Vaknin A, Eliakim R, Ackerman Z, Steiner I . Neurological abnormalities associated with celiac disease. J Neurol 2004; 251: 1393–1397.
Lee YT, Hu LY, Shen CC, Huang MW, Tsai SJ, Yang AC et al. Risk of psychiatric disorders following irritable bowel syndrome: a nationwide population-based cohort study. PLoS ONE 2015; 10: e0133283.
Salvadore G, Singh JB . Ketamine as a fast acting antidepressant: current knowledge and open questions. CNS Neurosci Ther 2013; 19: 428–436.
Berman RM, Cappiello A, Anand A, Oren DA, Heninger GR, Charney DS et al. Antidepressant effects of ketamine in depressed patients. Biol Psychiatry 2000; 47: 351–354.
Acknowledgements
This work was supported by a NIMH P50 Silvio O Conte Center at Johns Hopkins (grant# MH-94268) and by the Stanley Medical Research Institute. We thank Drs Cynthia Sears and Vern Carruthers for detailed and constructive comments on earlier versions of this paper. We also thank Chunxia Yang for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Yolken is a member of the Stanley Medical Research Institute Board of Directors and Scientific Advisory Board. The remaining authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Kannan, G., Gressitt, K., Yang, S. et al. Pathogen-mediated NMDA receptor autoimmunity and cellular barrier dysfunction in schizophrenia. Transl Psychiatry 7, e1186 (2017). https://doi.org/10.1038/tp.2017.162
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2017.162
This article is cited by
-
The role of infections and inflammation in schizophrenia: review of the evidence
Middle East Current Psychiatry (2024)
-
Effects of Toxoplasma gondii infection on cognition, symptoms, and response to digital cognitive training in schizophrenia
Schizophrenia (2022)
-
Host cell proteins modulated upon Toxoplasma infection identified using proteomic approaches: a molecular rationale
Parasitology Research (2022)
-
Toxoplasmosis: Targeting neurotransmitter systems in psychiatric disorders
Metabolic Brain Disease (2022)
-
Schizophrenia, the gut microbiota, and new opportunities from optogenetic manipulations of the gut-brain axis
Behavioral and Brain Functions (2021)