Abstract
Early identification of Alzheimer’s disease (AD) risk factors would aid development of interventions to delay the onset of dementia, but current biomarkers are invasive and/or costly to assess. Validated plasma biomarkers would circumvent these challenges. We previously identified the kinase DYRK1A in plasma. To validate DYRK1A as a biomarker for AD diagnosis, we assessed the levels of DYRK1A and the related markers brain-derived neurotrophic factor (BDNF) and homocysteine in two unrelated AD patient cohorts with age-matched controls. Receiver-operating characteristic curves and logistic regression analyses showed that combined assessment of DYRK1A, BDNF and homocysteine has a sensitivity of 0.952, a specificity of 0.889 and an accuracy of 0.933 in testing for AD. The blood levels of these markers provide a diagnosis assessment profile. Combined assessment of these three markers outperforms most of the previous markers and could become a useful substitute to the current panel of AD biomarkers. These results associate a decreased level of DYRK1A with AD and challenge the use of DYRK1A inhibitors in peripheral tissues as treatment. These measures will be useful for diagnosis purposes.
Similar content being viewed by others
Introduction
The development of neuropathological changes associated with Alzheimer’s disease (AD) precedes the onset of dementia by many years.1 Studies in transgenic mouse models of AD suggest that the majority of disease-modifying drugs are most effective in the early stages of AD development and not in later disease stages characterized by severe neurodegeneration.2 Currently established neurochemical and imaging AD biomarkers require invasive procedures such as lumbar puncture or the use of sophisticated technical equipment only available at specialized research centers. New, less invasive, less expensive and reliable markers of AD are urgently needed.
Recently, DYRK1A, a serine threonine kinase with multiple targets, has attracted interest as a candidate AD biomarker. DYRK1A is involved in the control of excitation/inhibition balance,3 anti-inflammatory processes4, 5 and over-phosphorylation of tau protein.6 It is also associated with the dysregulation of neurotrophic pathways,7 particularly at the level of the brain-derived neurotrophic factor (BDNF),8 which has several roles in synaptic plasticity and neuronal survival. We have also previously shown a negative correlation between DYRK1A level and homocysteine (Hcy) level9 in liver from mice models. Moreover, DYRK1A regulation, synthesis and degradation are complex and tissue specific; for instance, in a mouse model of genetic hyperhomocysteinemia, less DYRK1A protein is detected in the liver and more is detected in the brain.9, 10, 11
We recently showed in a well-characterized cohort of AD and age-matched controls (cohort P, Paris) that plasma DYRK1A levels were reduced in individuals with oligosymptomatic AD and with dementia due to AD.12 Interestingly, lymphoblastoid cells from diploid individuals revealed a positive correlation between DYRK1A and BDNF levels.13 BDNF levels are reported to be lower in the platelet-rich plasma of AD patients at moderate-to-severe stages of dementia compared with normal controls.14 A meta-analysis of results obtained from AD cohorts reported a significant positive association between serum Hcy and the incidence of dementia.15
With the hopes of expanding upon these results, we sought to assess the utility of DYRK1A as a biomarker of AD. We measured the DYRK1A plasma levels in a new cohort (cohort M, Munich) using a different method (enzyme-linked immunosorbent assay, ELISA) from that of the first study, as well as a new antibody. Blood markers were measured in biologically and clinically defined AD patients along with age-matched controls from two cohorts (cohorts M and P).
As DYRK1A, like many other kinases, is involved in controlling numerous pathways, we also measured markers linked to these pathways to investigate possible correlations between DYRK1A, BDNF, Hcy and soluble amyloid precursor protein β (sAPPβ), an upstream product of the amyloid cascade leading to the production of amyloid β, a central constituent of amyloid plaques. We further investigated whether Hcy, BDNF and DYRK1A could function as composite biomarkers of AD.
Materials and methods
Clinical research
Cohort M (Munich): The controls (n=20) were individuals without subjective memory complaints and without neuropsychiatric disorders. They had normal cerebrospinal fluid concentration of Amyloid β 42, total tau and tau phosphorylated at threonine 181, measured in duplicate with commercially available ELISA kits (Table 1). Thus, preclinical AD was precluded.16 Recruitment and inclusion criteria of the patient sample have been described.17 Outpatients (n=69) were recruited at the Department of Psychiatry and Psychotherapy, Klinikum Rechts der Isar, Technical University of Munich. Patients had been referred by general practitioners, psychiatrists, other institutions or were self-referred. Controls and patients were Caucasian. Patients with oligosymptomatic AD fulfilled the National Institute on Aging-Alzheimer Association diagnostic guidelines for mild cognitive impairment,18 while patients with dementia met the National Institute on Aging-Alzheimer Association criteria for dementia due to AD.19 All the participants provided written informed consent and all clinical investigations were conducted in accordance with the principles of the Declaration of Helsinki, sixth revision.
Cohort P (Table 1): recruitment and inclusion criteria of 25 controls and 26 patients, have been described previously.12 Twenty-five controls and 25 patients were Caucasian; one AD patient was African.
Cohorts M and P did not include subjects with severe cortical or subcortical vascular lesions. Average duration of the disease was similar in the two cohorts M and P (that is, 1–4 years for mild cognitive impairment, 3–8 years for AD). ApoE genotyping was described previously.20
The blood samples were collected from participants into citrate containers, and the containers were immediately placed on ice until processed. Plasma was obtained by centrifugation of containers for 15 min at 2000 g at 4 °C, then rapidly frozen and stored at −80 °C until analysis. The plasma and serum aliquots were thawed on the same day of the experiment. The plasma was diluted at 1:20 in 1 × phosphate-buffered saline.
Experimental mice
We conducted experimental animal study using mice carrying a murine BAC clone containing the entire Dyrk1a gene (maintained on a C57BL/6J background)21 and Dyrk1a(+/−) mice maintained on a CD1 background.22 Dyrk1a(+/−) and mBACtgDyrk1a mice were genotyped by PCR.21, 22 All the experimental procedures were carried out in accordance with the European Union guidelines (Directive 2010/63/EU) and the followed protocols were approved by the ethics committee of the Parc Científic de Barcelona (PCB). Official authorization from the French Ministry of Agriculture was granted to carry out research and experiments on animals (authorization number 75–369) with approval by local ethical committee (Université Paris Diderot). In this study, we have used embryos of Dyrk1a(−/−) mice, Dyrk1a(+/−) mice and their wild-type littermates. The day of the vaginal plug was defined as E0.5. The proteins were prepared from E11 to E12 embryo heads.
Adult mice were anesthetized and blood was collected through retro-orbital sinus sampling into tubes containing a 1/10 volume of 3.8% sodium citrate. The plasma was isolated by centrifugation (2500 g).
Immunochemistry
Immunogen preparation: the DNA sequence encoding human DYRK1A protein deleted in its C terminus (Δ502–763 further named Dyrk1AΔC) has been previously cloned and was used to prepare the protein.23
Production of monoclonal antibodies: monoclonal antibodies (mAbs) were produced in ascitic fluid in BALB/C mice and further purified using caproic acid precipitation.24 The concentration and purity of mAbs were then assessed by measuring absorbance at 280 nm and by sodium dodecyl sulfate-polyacrylamide gel electrophoresis Coomassie blue staining in reducing and non-reducing conditions.
Evaluation of polyclonal response and screening of mAbs in hybridoma supernatants was performed following standard protocols (see Supplementary Methods).25, 26
Immunoblotting
After transfer, the membranes were saturated by incubation in 5% w/v nonfat milk powder in Tris-saline buffer (1.5 mm Tris base pH 8; 5 mm NaCl; 0.1% Tween-20) and incubated overnight at 4 °C with M01 antibody (1/250, Abnova, Tebu, France) and N6 antibody (1/2000) against DYRK1A. Binding of the primary antibody was detected by incubation with horse radish peroxidase-conjugated secondary antibody using Western Blotting Luminol Reagent (Santa Cruz Biotechnology, Tebu, France). Ponceau-S coloration was used as a loading control. Digitized images (LAS-3000 imaging system (Fuji Photo Film, Tokyo, Japan)) were used for densitometric measurements with an image analyzer (UnScan-It software, Silk Scientific, Orem, UT, USA).
Immunometric tests
The DYRK1A levels were assessed by a solid phase immobilized epitope-immunoassay set up for antibody M01 (Abnova; clone 7D10; immunogen: 674 aa~763 aa) and antibody N6.27 BDNF was assessed using sandwich ELISA (ELISA E-Max, Promega, Madison, WI, USA). After removal of unbound conjugates, bound enzyme activity was assessed by use of a chromogenic substrate for measurement at 450 nm by a microplate reader (Flex Station 3, Molecular Device, San Diego, CA, USA). All the assays were performed in duplicate.
Homocysteine assay
Plasma total (tHcy), defined as the total concentration of Hcy after quantitative reductive cleavage of all disulfide bonds, was assayed by using fluorimetric high-performance liquid chromatography as previously described.28
Statistical analysis
The results are presented as mean±s.d. in all the tables. The normality of data distribution was tested with a Kolmogorov–Smirnov test. Statistical comparisons were performed with an unpaired t-test and two-tailed P-values for the comparison of means between two groups, which calculates the exact P-value and accounts for ties among values. Statistical significance was set at P<0.05.
Multivariate data analysis was performed through a principal component analysis (PCA), which helps the visualization of the association between biomarkers and patient status (control or AD). A PCA projects the standardized data, that is, the biomarker descriptors, into a subspace made of orthogonal linear axis, so-called principal components. Data may then be explored in a smaller dimensional space spanning the most informative view according to data variability.
The analysis of the biomarkers of AD using a protein profile was first performed using different thresholds. We computed receiver–operating characteristic curves to evaluate the capacity of each plasma biomarker to discriminate subjects with AD from those without AD, using area under the curves.
Biomarkers significantly associated to AD were then tested using models and cross-validation approaches based on the protein/Hcy profile data. Logistic regression (LR), which is a method adapted to test association between a binomial outcome and covariates, was used to build a diagnostic model for the status of the patients. Linear combination of selected biomarkers was performed using the following model:

The biomarkers were selected through stepwise selection. The final regression model was selected based on optimizing the balance between its sensitivity (the percentage of predicted AD patients among observed AD patients) and specificity (here, the percentage of predicted controls among observed control patients) on both training and validation sets obtained by cross-validation.
The goal of cross-validation is to limit overfitting, and to give an insight on how the model will generalize to an independent. It is a powerful general technique to test the stability of regression model and its robustness particularly adapted in case of few data. We had used a fivefold cross-validation to partition the initial plasma sample into five parts (fold).29 Each fold serves in turn as a validation sample of the model established on the remaining fourfold (training sample). We then had five models, allowing to calculate, in the case of a logistic regression model, the classical parameters, accuracy, sensitivity and specificity, and to deduce the average and the standard deviation of each one.
Final LR model could thereafter be used to assess the risk for any given patient according to its protein profile variables. Analyses were done using GraphPad Prism v6.07 (San Diego, CA, USA) and R software.
Results
Development of novel anti-DYRK1A monoclonal antibodies and validation in mouse models and plasma
Monoclonal antibodies recognizing DYRK1A were raised in Swiss mice by immunization with purified N-terminally His-tagged DYRK1AΔC (Δ502–763 C-terminal deleted DYRK1A protein). Seven monoclonal antibodies (mAbs) were produced and named N1 to N7.
All mAbs appeared to be good capture antibodies. N6 gave the strongest signal on western blot. M01 (Abnova) and N6 patterns were compared using samples from mouse embryos (E15; −/− mice are not viable) with 0, 1 and 2 copies of Dyrk1a. (Figure 1a).
Characterization of a new monoclonal antibody against DYRK1A. (a) Western blots of heads from mouse embryos; lane 1: 0 copies of DYRK1A, lane 2: 1 copy, lane 3: 2 copies; protein marker sizes (kDa): 95, 70, 62, 51, 42; left panel: M01 antibody (7D10), right panel: N6 antibody; loading control: Ponceau staining. (b) Quantification of DYRK1A content in plasma from adult mice with 1 Dyrk1a (+/−), 2 (2N) or 3 (mBACtgDyrk1a) copies of the Dyrk1a gene, with N6 antibody.
An immunoassay (solid phase immobilized epitope-immunoassay) was designed using the M01 and N6 antibodies with methods described previously.27 Signals obtained from plasma samples from mice with 1, 2 or 3 copies of Dyrk1a were compared with the gene copy number showing a good correlation between DYRK1A level and gene copy number (N6: Figure 1b). The concentration of DYRK1A ranged between 8 and 10 ng ml−1 in mouse plasma and between 1.8 and 2.2 ng ml−1 in human plasma.
As DYRK1A is a constituent of plasma, quantification of DYRK1A in such a matrix is not possible (as no ‘blank plasma’ is available and plasma from a Dyrk1a knockout animals is not available), DYRK1A plasma levels can only be compared between different populations.
Plasma DYRK1A decreases in AD patients from cohort M
Using the same solid phase immobilized epitope-immunoassay method described in 'supplementary of Materials and methods' section (Table 1), we assessed the levels of DYRK1A in human plasma using antibody M01 (Figure 2a) and antibody N6 (Figure 2b). Both the experiments showed a similar decrease in DYRK1A in AD patients, whereas no difference was found between patients with oligosymptomatic AD and patients with dementia due to AD. Consequently, these two groups were not treated as separate, but as one group designated as AD. Mean DYRK1A level was significantly lower in AD patients compared with controls (P<0.0001) and these results were observed with both antibodies M01 and N6.
DYRK1A protein levels in plasma from control (CTRL) individuals and Alzheimer’s disease (AD) patients from cohort M (Munich). SPIE-IA ELISA was used to detect expression of DYRK1A in CTRL and AD (a) with N6 antibody; (b) with M01 antibody; white box: controls; red box: AD patients. (c) DYRK1A protein levels stratified according to APOE genotype with ‘no ApoE4’ for APOE2 or APOE3 genotypes and ‘ApoE4’ for one or two APOE4 alleles: white dots: controls; red dots: AD patients. (d) sAPPbeta protein levels: white box: controls; red box: AD patients. Bars indicate mean±s.e.m, ****P<0.0001, ***P<0.001. ELISA, enzyme-linked immunosorbent assay; SPIE-IA, solid phase immobilized epitope-immunoassay.
The results were the same when stratified by sex, therefore results for both sexes are presented jointly. DYRK1A protein levels did not correlate with Mini-Mental State Examination scores. When stratified by APOE genotype, controls and AD patients were distributed similarly among genotypes and the average level of DYRK1A was similar in individuals with and without the APOE4 genotype (Figure 2c). We also analyzed the levels of sAPPbeta, which were significantly lower in cohort M AD patients (Figure 2d). DYRK1A levels did not correlate with sAPPbeta levels (P=0.79).
DYRK1A and markers from associated pathways are altered in AD patients
The relative decrease in plasma DYRK1A observed in the Munich cohort (ELISA method) and in the Paris cohort (slot blot method) compared to controls was statistically similar. Therefore, we pooled results from the two cohorts. We detected a significant difference in DYRK1A levels between controls and AD patients (decrease of −24%, P<10−14; Table 2). Plasma BDNF was positively correlated with DYRK1A (P<0.05) and was lower in the plasma of AD patients; pooled results are shown in Table 2 (decrease of −37%, P<10−9). We previously showed a negative correlation between liver DYRK1A and plasma homocysteine (Hcy), a known risk factor for AD.30 Plasma levels of homocysteine were assessed with HPLC and were higher in individuals with AD compared with controls (increase of +28%, P<10−6). Glutathione is a major antioxidant byproduct of Hcy and glutathione levels were similar in the control group (26.8) and AD group (26.9; P=0.9, data not shown). There was no relationship between APOE genotype and BDNF or Hcy level.
The diagnostic accuracy (area under the curve) of the three biomarkers in differentiating patients with AD from controls (Figure 3a) showed significant relationships between each biomarker and the AD group. The mean areas under the curves were 0.847 for DYRK1A, 0.793 for BDNF, and 0.754 for Hcy, indicating that DYRK1A was the most accurate of the markers.
(a) Diagnostic accuracy of DYRK1A, BDNF and Hcy markers. (b) Correlation between descriptors and the first principal plane (PC1 + PC2). The closer the descriptors are to the correlation circle, the more they contribute to explaining the variability captured by the corresponding principal components. As indicated by the projection of the biomarker variable descriptors close to the PCA correlation circle, the DYRK1A and BDNF descriptors are strongly correlated and capture the majority of the variability of the data (more than 47.60%) on PC1 while Hcy is negatively correlated with these two first descriptors and is associated with 35.9% of the variability. (c) Distribution of Munich and Paris cohorts showing good overlap between the two control groups and the two AD groups. AD, Alzheimer's disease; AUC, area under the curve; BDNF, brain-derived neurotrophic factor; Hcy, homocysteine; PCA, principal component analysis.
Efficiency analyses
PCA performed on the three biomarker descriptors enabled (i) an in-depth study of their correlation, (ii) a direct visualization of the similarity shared by the two cohorts and (iii) trend biomarker values of control versus AD groups. The first PCA plane in Figure 3b captures more than 83.58% of the marker variability and as such provides an efficient visualization of the data. Figure 3c illustrates the distribution of AD patients from both cohorts on PCA. The two cohorts can be observed (depicted in full or empty circles) as well mixed with no specific biomarker characteristics, confirming that these two cohorts can be merged to build predictive models.
The visualization of patient status illustrates controls gathered in the right PCA space, corresponding to high values of PC1, while AD patients are located on the small values of PC1. This indicates that AD patients exhibit small values of DYRK1A (rel) and BDNF (ng ml−1) and rather large values of Hcy related to controls and that these biomarkers are diagnostic and potentially promising predictors of patient status.
AD diagnostic models were built using statistical learning methods. Only LR models are presented (Table 3), as they resulted in better accuracy by five cross-validation of 0.937±0.013 than CART models (which had an accuracy of 0.881±0.024). LR was selected as an optimal combination of the predictive power of DYRK1A, BDNF and Hcy markers. Parameters for the LR have been calculated independently of age, sex and apoE genotype:

On the pooled cohorts, age, sex and apoE were not significantly different between control and AD groups (P=0.54), but biomarker differences were significant (P<10−6).
Adjusting for age, sex and apoE genotype were then assessed showing nonsignificant effect in LR model for age (P=0.78), for sex (P=0.53) and for ApoE genotype (P=0.54).
The odds ratios for the model are presented in Table 4. We obtained odds ratios of 0.787 for DYRK1A, 0.20 for BDNF and 1.45 for Hcy, indicating that increased DYRK1A (relative) by one unit decreases the AD risk for a patient (risk multiplied by 0.787).
DYRK1A was found to be the most predictive marker of AD and on its own has a high accuracy rate of 0.84±0.05 on five validation sets (Table 3). Combining DYRK1A with BDNF leads to more than a 5% accuracy increase on the validation sets, specifically the specificity (ability to predict control patients), while combining DYRK1A, BDNF and Hcy allows for more than a 3% accuracy increase.
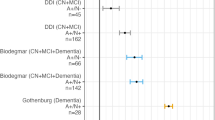
Three PCA figures (Figure 4) illustrate patients accurately or falsely predicted as AD using logistic regressions (LR1, LR2, LR3) obtained using one, two or three markers (DYRK1A, DYRK1A+BDNF, DYRK1A+BDNF+Hcy) showing which patients were predicted as having AD by adding BDNF or Hcy biomarkers. PCA.A illustrates the LR1 performance, which accurately predicted 77/84 AD patients and 25/36 control patients. PCA.B illustrates LR2, which predicted seven supplementary individuals (two AD and five controls) due to their high BDNF values. PCA.C illustrates LR3, which predicted four supplementary patients due to their specific values of Hcy (two AD due to high Hcy values and two control due to low Hcy values).
Diagnostic efficiency for each patient LR1: using one (DYRK1A), LR2: two (DYRK1A+BDNF) or LR3: three (DYRK1A+BDNF+Hcy) biomarkers; red dots: correctly diagnosed AD; black dots: correctly diagnosed control; blue cross: false diagnostic. AD, Alzheimer's disease; BDNF, brain-derived neurotrophic factor; Hcy, homocysteine; PC, principal component.
Discussion
Characteristic features of AD are memory loss, plaques resulting from abnormal processing of amyloid precursor protein, presence of neurofibrillary tangles and dystrophic neurites containing hyperphosphorylated tau and signs of inflammation.
DYRK1A kinase is a multifunctional enzyme known to have a role in dendrite morphogenesis31 and in the control of excitation/inhibition balance.3, 32 It is also involved in tau phosphorylation (ser 212)6 and control of inflammation through NF-kappa B and NFAT-related mechanisms.4, 5, 33 DYRK1A contains a PEST sequence, which, after calpain action, removes the C-terminal part and may contribute to the decrease of native DYRK1A level.
We used two antibodies to measure DYRK1A protein in plasma of AD patients and healthy controls. The M01 antibody recognized a Cter epitope (674–763 aa) and allowed for the quantification of the 95 kDa protein. The second antibody, N6, was raised against the active site (amino acids 1–562). We observed lower levels of DYRK1A in AD in two different cohorts (Munich and Paris) with two different techniques, slot blot12 and ELISA (solid phase immobilized epitope-immunoassay), using the two different antibodies. These results validate the association of a low level of the long forms of DYRK1A (triplet around 95 kDa on western blots) in plasma from patients with AD. A reduction in this long form and an increase in truncation have been reported in brain samples from AD patients versus controls.34 As we observed a decrease with an antibody recognizing the C terminus (long form) and with an antibody recognizing the N terminus (short and long form), our results indicate that the long form is the main form present in the plasma of both controls and patients and that plasma level of this long form correlates with its level in AD brain.
Stratification according to APOE genotype confirmed previous observations12 that DYRK1A levels are not linked to APOE genotype. In AD patients, sAPPbeta was found to be significantly lower, but there was no correlation between sAPPbeta and DYRK1A levels. This finding possibly indicates that the observed decrease in DYRK1A plasma concentration in AD may not be directly related to amyloid precursor protein catabolism and subsequently to the amyloid cascade.
BDNF is essential for brain development, neuroplasticity and neuronal survival. Decreased levels of BDNF and decreased CREB phosphorylation have been linked to depression.35 BDNF has been implicated in a number of neuropsychiatric disorders, including affective disorders, schizophrenia, addiction, eating disorders and neurodevelopmental disorders.36, 37, 38, 39 There is solid evidence demonstrating a reduction in BDNF mRNA and protein levels in AD cortex and hippocampus.40, 41, 42 Given its central role in synaptic plasticity, learning and memory formation,42 it is likely that a decrease in BDNF levels further contributes to cognitive dysfunction in AD. There is also evidence linking changes in BDNF to core psychopathological features of AD.43 Recent data suggest that plasma BDNF is a biomarker of impaired memory and general cognitive function in aging women,44 and a significant decrease in BDNF serum concentration has been found in AD patients compared with healthy controls.45 We found a decrease in BDNF both in oligosymptomatic AD and in dementia due to AD. Interestingly, this decrease was similar in the two studied cohorts M and showing consistency in results obtained with the same technical approach.
Hyperhomocysteinemia, in NPC cultures or induced by direct injection of Hcy into adult mouse brain, reduces neurogenesis46 through a mechanism involving the fibroblast growth factor receptor–Erk1/2–cyclin E signaling pathway. In addition, it leads to a decrease in DYRK1A and increases PP2A in the hippocampus.46 Moderately elevated plasma tHcy is a strong risk factor for vascular dementia and AD.15 Prospectively, elevated tHcy is associated with cognitive decline, white matter damage, brain atrophy, neurofibrillary tangles and dementia. Many studies have reported this association: a landmark study47 including 1092 elderly participants in the Framingham cohort who were free from cognitive impairment at baseline revealed a strong concentration-related effect of baseline tHcy, with no obvious threshold, with the risk of incident dementia up to 11 years later. In the Prospective Population Study of Women in Gothenburg,48 tHcy concentrations in 1368 middle-aged women were related to incident dementia up to 35 years later. In our cohorts, we found an increase of 35% in plasma Hcy in AD patients compared with controls. The Hcy level of our control group was below the 14–15 μmol l−1 critical threshold reported by previous studies47 and the Hcy level of most of AD patients stay close to this critical value (one patient above 25 μmol l−1 in cohort P and 3 in cohort M) in agreement with the absence of severe vascular lesions in the two cohorts.
As area under the curve values for these three markers were significant, we analyzed their respective efficiency and the accuracy of a composite marker. DYRK1A performed the best of the group, but the addition of BDNF and Hcy improves the efficiency of the association. For chronic diseases that may require long-term medications, accurate diagnosis is important, especially when serious adverse effects are expected from the treatment. In these cases, biomarkers are increasingly important, because they can confirm a difficult diagnosis or even make it possible in the first place. It is largely accepted that AD begins with an early, symptom-free phase. In such symptom-free patients there may be more or less probability of actually developing symptoms. In these cases, biomarkers help to identify high-risk individuals reliably and in a timely manner so that they can either be treated before onset of the disease or as soon as possible thereafter. These results, obtained with two cohorts, which have been extensively characterised, are highly significant: however, these cohorts are of limited size and it will be necessary to further confirm these results on larger cohorts.
Mechanisms involved in the differences observed for these markers are still under investigation. For DYRK1A, a link with Hcy level has been previously described as involving a calpain-related pathway either in mouse liver,49 in brains from AD patients34 or through transcription-linked mechanisms.50, 51 However, polymorphism-based mechanisms can also modify DYRK1A levels through changes in the efficiency of transcriptional factors like p53 or REST.52 We previously reported a positive correlation between DYRK1A and BDNF levels in lymphoblastoid cell lines derived from diploid individuals13 suggesting a genetic component to explain variability of these markers. These results associate a decreased level of DYRK1A with AD and challenge the use of DYRK1A inhibitors in peripheral tissues as treatment.
In conclusion, the blood levels of these markers offer diagnosis assessment utility. To assess the value of their addition to the current panel of AD biomarkers would need the use of larger cohorts. The identification of oligosymptomatic or even preclinical AD is crucial to the initiation of preventative strategies. Longitudinal studies will be necessary to decide whether the use of these biomarkers may also allow the prediction of future cognitive decline in cognitively normal individuals.
References
Ballard C, Gauthier S, Corbett A, Brayne C, Aarsland D, Jones E . Alzheimer's disease. Lancet 2011; 377: 1019–1031.
Golde TE, Schneider LS, Koo EH . Anti-abeta therapeutics in Alzheimer's disease: the need for a paradigm shift. Neuron 2011; 69: 203–213.
Souchet B, Guedj F, Sahun I, Duchon A, Daubigney F, Badel A et al. Excitation/inhibition balance and learning are modified by Dyrk1a gene dosage. Neurobiol Dis 2014; 69: 65–75.
Hamelet J, Noll C, Ripoll C, Paul JL, Janel N, Delabar JM . Effect of hyperhomocysteinemia on the protein kinase DYRK1A in liver of mice. Biochem Biophys Res Commun 2009; 378: 673–677.
Khor B, Gagnon JD, Goel G, Roche MI, Conway KL, Tran K et al. The kinase DYRK1A reciprocally regulates the differentiation of Th17 and regulatory T cells. Elife 2015; 4: 05920.
Kimura R, Kamino K, Yamamoto M, Nuripa A, Kida T, Kazui H et al. The DYRK1A gene, encoded in chromosome 21 Down syndrome critical region, bridges between beta-amyloid production and tau phosphorylation in Alzheimer disease. Hum Mol Genet 2007; 16: 15–23.
Guedj F, Sebrie C, Rivals I, Ledru A, Paly E, Bizot JC et al. Green tea polyphenols rescue of brain defects induced by overexpression of DYRK1A. PLoS ONE 2009; 4: e4606.
Toiber D, Azkona G, Ben-Ari S, Toran N, Soreq H, Dierssen M . Engineering DYRK1A overdosage yields Down syndrome-characteristic cortical splicing aberrations. Neurobiol Dis 2010; 40: 348–359.
Noll C, Planque C, Ripoll C, Guedj F, Diez A, Ducros V et al. DYRK1A, a novel determinant of the methionine-homocysteine cycle in different mouse models overexpressing this Down-syndrome-associated kinase. PLoS ONE 2009; 4: e7540.
Planque C, Dairou J, Noll C, Bui LC, Ripoll C, Guedj F et al. Mice deficient in cystathionine beta synthase display increased Dyrk1A and SAHH activities in brain. J Mol Neurosci 2013; 50: 1–6.
Abekhoukh S, Planque C, Ripoll C, Urbaniak P, Paul JL, Delabar JM et al. Dyrk1A, a serine/threonine kinase, is involved in ERK and Akt activation in the brain of hyperhomocysteinemic mice. Mol Neurobiol 2013; 47: 105–116.
Janel N, Sarazin M, Corlier F, Corne H, de Souza LC, Hamelin L et al. Plasma DYRK1A as a novel risk factor for Alzheimer's disease. Transl Psychiatry 2014; 4: e425.
Tlili A, Hoischen A, Ripoll C, Benabou E, Badel A, Ronan A et al. BDNF and DYRK1A are variable and inversely correlated in lymphoblastoid cell lines from Down syndrome patients. Mol Neurobiol 2012; 46: 297–303.
Platenik J, Fisar Z, Buchal R, Jirak R, Kitzlerova E, Zverova M et al. GSK3beta, CREB, and BDNF in peripheral blood of patients with Alzheimer's disease and depression. Prog Neuropsychopharmacol Biol Psychiatry 2014; 50: 83–93.
Wald DS, Kasturiratne A, Simmonds M . Serum homocysteine and dementia: meta-analysis of eight cohort studies including 8669 participants. Alzheimers Dement 2011; 7: 412–417.
Sperling RA, Aisen PS, Beckett LA, Bennett DA, Craft S, Fagan AM et al. Toward defining the preclinical stages of Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011; 7: 280–292.
Grimmer T, Wutz C, Drzezga A, Forster S, Forstl H, Ortner M et al. The usefulness of amyloid imaging in predicting the clinical outcome after two years in subjects with mild cognitive impairment. Curr Alzheimer Res 2013; 10: 82–85.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011; 7: 270–279.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH et al. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement 2011; 7: 263–269.
Lazar AN, Bich C, Panchal M, Desbenoit N, Petit VW, Touboul D et al. Time-of-flight secondary ion mass spectrometry (TOF-SIMS) imaging reveals cholesterol overload in the cerebral cortex of Alzheimer disease patients. Acta Neuropathol 2013; 125: 133–144.
Guedj F, Pereira PL, Najas S, Barallobre MJ, Chabert C, Souchet B et al. DYRK1A: a master regulatory protein controlling brain growth. Neurobiol Dis 2012; 46: 190–203.
Fotaki V, Dierssen M, Alcantara S, Martinez S, Marti E, Casas C et al. Dyrk1A haploinsufficiency affects viability and causes developmental delay and abnormal brain morphology in mice. Mol Cell Biol 2002; 22: 6636–6647.
Bui LC, Tabouy L, Busi F, Dupret JM, Janel N, Planque C et al. A high-performance liquid chromatography assay for Dyrk1a, a Down syndrome-associated kinase. Anal Biochem 2014; 449: 172–178.
Reik LM, Maines SL, Ryan DE, Levin W, Bandiera S, Thomas PE . A simple, non-chromatographic purification procedure for monoclonal antibodies. Isolation of monoclonal antibodies against cytochrome P450 isozymes. J Immunol Methods 1987; 100: 123–130.
Ellman GL, Courtney KD, Andres V Jr, Feather-Stone RM . A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem Pharmacol 1961; 7: 88–95.
Grassi J, Frobert Y, Pradelles P, Chercuitte F, Gruaz D, Dayer JM et al. Production of monoclonal antibodies against interleukin-1 alpha and -1 beta. Development of two enzyme immunometric assays (EIA) using acetylcholinesterase and their application to biological media. J Immunol Methods 1989; 123: 193–210.
Volland H, Vulliez Le Normand B, Mamas S, Grassi J, Creminon C, Ezan E et al. Enzyme immunometric assay for leukotriene C4. J Immunol Methods 1994; 175: 97–105.
Ducros V, Demuth K, Sauvant MP, Quillard M, Causse E, Candito M et al. Methods for homocysteine analysis and biological relevance of the results. J Chromatogr B Analyt Technol Biomed Life Sci 2002; 781: 207–226.
Neto E, Biessmann F, Aurlien H, Nordby H, Eichele T . Regularized linear discriminant analysis of EEG features in dementia patients. Front Aging Neurosci 2016; 8: 273.
Smith AD, Refsum H . Homocysteine, B vitamins, and cognitive impairment. Annu Rev Nutr 2016; 36: 211–239.
Ori-McKenney KM, McKenney RJ, Huang HH, Li T, Meltzer S, Jan LY et al. Phosphorylation of beta-tubulin by the Down syndrome kinase, minibrain/DYRK1a, regulates microtubule dynamics and dendrite morphogenesis. Neuron 2016; 90: 551–563.
Ruiz-Mejias M, Martinez de Lagran M, Mattia M, Castano-Prat P, Perez-Mendez L, Ciria-Suarez L et al. Overexpression of Dyrk1A, a Down syndrome candidate, decreases excitability and impairs gamma oscillations in the prefrontal cortex. J Neurosci 2016; 36: 3648–3659.
Lee Y, Ha J, Kim HJ, Kim YS, Chang EJ, Song WJ et al. Negative feedback Inhibition of NFATc1 by DYRK1A regulates bone homeostasis. J Biol Chem 2009; 284: 33343–33351.
Jin N, Yin X, Gu J, Zhang X, Shi J, Qian W et al. Truncation and activation of dual specificity tyrosine phosphorylation-regulated kinase 1A by Calpain I: a molecular mechanism linked to tau pathology in Alzheimer disease. J Biol Chem 2015; 290: 15219–15237.
Duman RS, Aghajanian GK, Sanacora G, Krystal JH . Synaptic plasticity and depression: new insights from stress and rapid-acting antidepressants. Nat Med 2016; 22: 238–249.
Autry AE, Monteggia LM . Brain-derived neurotrophic factor and neuropsychiatric disorders. Pharmacol Rev 2012; 64: 238–258.
Carrard A, Salzmann A, Perroud N, Gafner J, Malafosse A, Karege F . Genetic association of the Phosphoinositide-3 kinase in schizophrenia and bipolar disorder and interaction with a BDNF gene polymorphism. Brain Behav 2011; 1: 119–124.
Niitsu T, Shirayama Y, Matsuzawa D, Hasegawa T, Kanahara N, Hashimoto T et al. Associations of serum brain-derived neurotrophic factor with cognitive impairments and negative symptoms in schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry 2011; 35: 1836–1840.
Koenigsberg HW, Yuan P, Diaz GA, Guerreri S, Dorantes C, Mayson S et al. Platelet protein kinase C and brain-derived neurotrophic factor levels in borderline personality disorder patients. Psychiatry Res 2012; 199: 92–97.
Phillips HS, Hains JM, Armanini M, Laramee GR, Johnson SA, Winslow JW . BDNF mRNA is decreased in the hippocampus of individuals with Alzheimer's disease. Neuron 1991; 7: 695–702.
Ferrer I, Marin C, Rey MJ, Ribalta T, Goutan E, Blanco R et al. BDNF and full-length and truncated TrkB expression in Alzheimer disease. Implications in therapeutic strategies. J Neuropathol Exp Neurol 1999; 58: 729–739.
Lu Y, Christian K, Lu B . BDNF: a key regulator for protein synthesis-dependent LTP and long-term memory? Neurobiol Learn Mem 2008; 89: 312–323.
Diniz BS, Teixeira AL . Brain-derived neurotrophic factor and Alzheimer's disease: physiopathology and beyond. Neuromol Med 2011; 13: 217–222.
Komulainen P, Pedersen M, Hanninen T, Bruunsgaard H, Lakka TA, Kivipelto M et al. BDNF is a novel marker of cognitive function in ageing women: the DR's EXTRA Study. Neurobiol Learn Mem 2008; 90: 596–603.
Forlenza OV, Diniz BS, Teixeira AL, Ojopi EB, Talib LL, Mendonca VA et al. Effect of brain-derived neurotrophic factor Val66Met polymorphism and serum levels on the progression of mild cognitive impairment. World J Biol Psychiatry 2010; 11: 774–780.
Rabaneda LG, Geribaldi-Doldan N, Murillo-Carretero M, Carrasco M, Martinez-Salas JM, Verastegui C et al. Altered regulation of the Spry2/Dyrk1A/PP2A triad by homocysteine impairs neural progenitor cell proliferation. Biochim Biophys Acta 2016; 1863: 3015–3026.
Seshadri S, Beiser A, Selhub J, Jacques PF, Rosenberg IH, D'Agostino RB et al. Plasma homocysteine as a risk factor for dementia and Alzheimer's disease. N Engl J Med 2002; 346: 476–483.
Zylberstein DE, Lissner L, Bjorkelund C, Mehlig K, Thelle DS, Gustafson D et al. Midlife homocysteine and late-life dementia in women. A prospective population study. Neurobiol Aging 2011; 32: 380–386.
Hamelet J, Couty JP, Crain AM, Noll C, Postic C, Paul JL et al. Calpain activation is required for homocysteine-mediated hepatic degradation of inhibitor I kappa B alpha. Mol Genet Metab 2009; 97: 114–120.
Jang Y, Kim J, Ko JW, Kwon YH . Homocysteine induces PUMA-mediated mitochondrial apoptosis in SH-SY5Y cells. Amino Acids 2016; 48: 2559–2569.
Zhang Y, Liao JM, Zeng SX, Lu H . p53 downregulates Down syndrome-associated DYRK1A through miR-1246. EMBO Rep 2011; 12: 811–817.
Lu M, Zheng L, Han B, Wang L, Wang P, Liu H et al. REST regulates DYRK1A transcription in a negative feedback loop. J Biol Chem 2011; 286: 10755–10763.
Acknowledgements
This work was supported by the FEANS. We acknowledge the platform accommodation and animal testing of the animal facility at the Institute Jacques-Monod (University Paris Diderot) and the FlexStation3 facility of the Functional and Adaptive Biology (BFA) Laboratory.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Translational Psychiatry website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Janel, N., Alexopoulos, P., Badel, A. et al. Combined assessment of DYRK1A, BDNF and homocysteine levels as diagnostic marker for Alzheimer’s disease. Transl Psychiatry 7, e1154 (2017). https://doi.org/10.1038/tp.2017.123
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2017.123
This article is cited by
-
Increased plasma DYRK1A with aging may protect against neurodegenerative diseases
Translational Psychiatry (2023)
-
Brain-derived neurotrophic factor in Alzheimer’s disease and its pharmaceutical potential
Translational Neurodegeneration (2022)
-
Do serum GDNF levels correlate with severity of Alzheimer’s disease?
Neurological Sciences (2021)
-
Peripheral Blood Brain-Derived Neurotrophic Factor as a Biomarker of Alzheimer’s Disease: Are There Methodological Biases?
Molecular Neurobiology (2018)