Abstract
Clinical studies have shown alterations in metabolic profiles when patients with mild cognitive impairment and Alzheimer’s disease dementia were compared to cognitively normal subjects. Associations between 204 serum metabolites measured at baseline (1987–1989) and cognitive change were investigated in 1035 middle-aged community-dwelling African American participants in the biracial Atherosclerosis Risk in Communities (ARIC) Study. Cognition was evaluated using the Delayed Word Recall Test (DWRT; verbal memory), the Digit Symbol Substitution Test (DSST; processing speed) and the Word Fluency Test (WFT; verbal fluency) at visits 2 (1990–1992) and 4 (1996–1998). In addition, Cox regression was used to analyze the metabolites as predictors of incident hospitalized dementia between baseline and 2011. There were 141 cases among 1534 participants over a median 17.1-year follow-up period. After adjustment for established risk factors, one standard deviation increase in N-acetyl-1-methylhistidine was significantly associated with greater 6-year change in DWRT scores (β=−0.66 words; P=3.65 × 10−4). Two metabolites (one unnamed and a long-chain omega-6 polyunsaturated fatty acid found in vegetable oils (docosapentaenoate (DPA, 22:5 n-6)) were significantly associated with less decline on the DSST (DPA: β=1.25 digit-symbol pairs, P=9.47 × 10−5). Two unnamed compounds and three sex steroid hormones were associated with an increased risk of dementia (all P<3.9 × 10−4). The association of 4-androstene-3beta, 17beta-diol disulfate 1 with dementia was replicated in European Americans. These results demonstrate that screening the metabolome in midlife can detect biologically plausible biomarkers that may improve risk stratification for cognitive impairment at older ages.
Similar content being viewed by others
Introduction
Alzheimer’s disease (AD) is the most common form of dementia1 and is characterized by significant impairment in memory, behavioral changes and gradual loss of functional autonomy. The prevalence of AD dementia is as high as 20–30% in persons aged 75–84 years, and up to 50% in individuals aged ⩾85 years.2 When 2800 subjects who were free of dementia were followed for 29 years in the Framingham Heart Study, the lifetime risk for dementia was reported to be 1 in 5 for women and 1 in 10 for men.3 There is currently no known cure or preventive intervention. Cognitive function, including memory and executive function, is influenced by both genetic and environmental factors.4, 5 The human metabolome is a reflection of the interaction between genes and the environment, and studies examining the relationship between metabolomic profiles and cognitive function may lead to the development of biomarkers used to detect cognitive decline or AD before clinical diagnostic criteria for impairment are met. In this context, Mapstoneet al.6 have recently reported that a set of 10 lipids identified in a metabolomics screen in peripheral blood could be used with 90% accuracy to predict conversion from normal cognitive status to amnestic mild cognitive impairment (MCI) or AD dementia over a 2–3-year period in adults aged ⩾70 years. Several other investigators have also found significant alterations in metabolic profiles in comparisons of patients with MCI and AD dementia to cognitively normal subjects.7, 8, 9, 10, 11, 12, 13, 14 The goal of this study is to determine whether metabolites measured in serum in middle-aged African American adults are associated with cognitive function and cognitive change in the Atherosclerosis Risk in Communities (ARIC) study. African Americans are affected disproportionately with AD dementia;15, 16 therefore, this investigation may also provide insight into the biological basis of this health disparity.
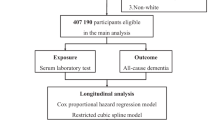
Materials and methods
The ARIC Study
The ARIC Study is a prospective longitudinal investigation of the development of atherosclerosis and its clinical sequelae, in which 15 792 individuals aged 45–64 years were enrolled at the baseline examination. A detailed description of the ARIC study has been reported previously.17 At the inception of the study in 1987–1989, the participants were selected by probability sampling from four communities in the United States: Forsyth County, North Carolina; Jackson, Mississippi (African Americans only); suburbs of Minneapolis, Minnesota; and Washington County, Maryland. Four examinations were carried out at 3-year intervals (examination 1, 1987–1989; examination 2, 1990–1992; examination 3, 1993–1995; examination 4, 1996–1998). Subjects were contacted annually to update their medical histories between examinations. Cognitive testing was performed at examinations 2 and 4. Metabolomics profiles were available for 1977 African American study participants.18 Cognitive function at the baseline examination was examined in 1577 men and women after excluding individuals who had an unknown history of definite or probable stroke or a history of physician-diagnosed stroke prior to visit 2 (n=51), did not attend the second clinical examination (n=297), were missing test scores for all three cognitive tests (n=50) or were missing information on educational attainment (n=2). Among the participants with cognitive test scores obtained at both examinations, individuals were not included in the analysis of 6-year cognitive change if they had an unknown history of definite or probable stroke or a history of physician-diagnosed stroke prior to visit 2 (n=51) or between visits 2 and 4 (n=74), or did not attend the second (n=297) or fourth (n=361) clinical examination. Additional exclusions were made for missing cognitive data for all three neuropsychological tests at either visit 2 (n=45) or visit 4 (n=112), or for missing information concerning the highest level of education attained (n=2); the final study sample consisted of 1035 participants. Individuals hospitalized for dementia through the end of 2011 were identified using ICD-9 codes listed in the hospital discharge record (AD (331.0); vascular dementia (290.4); or other forms of dementia (290.0, 290.1., 290.2, 290.3, 290.9, 294.1, 294.2, 294.8, 294.9, 331.1, 331.2, 331.8, 331.9) after collection of all hospital records of the study participants.19 The study participants were excluded from the analysis of incident hospitalized dementia if they had prevalent stroke at visit 1 (n=67), were missing information about the number of years of education completed (n=5) or if follow-up time was missing (n=371), leaving a total of 1534 individuals. Written informed consent was provided by all study participants, and the study design and methods were approved by the institutional review boards at the four collaborating institutions: University of Mississippi Medical Center Institutional Review Board (Jackson Field Center); Wake Forest University Health Sciences Institutional Review Board (Forsyth County Field Center); University of Minnesota Institutional Review Board (Minnesota Field Center); and the Johns Hopkins School of Public Health Institutional Review Board (Washington County Field Center).
Cognitive tests
Cognitive function was assessed by three neuropsychological tests at the second and fourth clinical examinations that have been described previously:20 (1) the Delayed Word Recall Test (DWRT) is a test of verbal memory requiring recall of a word list after a short delay (score range 0–10);21 (2) the Digit Symbol Substitution Test (DSST) is a subtest of the Wechsler Adult Intelligence Scale-Revised involving timed translation of numbers to symbols in 90 s using a key, and measures psychomotor performance (score range 0–93);22, 23 and (3) the Word Fluency Test (WFT) is a measure of executive function. The score is the combined total of correct words produced beginning with F, A and S.23, 24 For all of the neuropsychological tests, lower scores indicate a lower measure of cognition. Six-year change in cognitive function was analyzed as the difference between the test score obtained at visit 4 and the test score obtained at visit 2 for each test.
Clinical and laboratory measurements
The clinical and laboratory measurements used for this study were assessed during the first clinical examination for the analyses of incident hospitalized dementia, and during the second clinical examination for the analyses of cognitive function with the exception of education and estimated glomerular filtration rate (eGFR), which were evaluated at the first examination. Education was included as a covariate in regression models as an ordinal variable based on the highest level attained (⩽11 years; 12–16 years; >16 years). Serum creatinine was measured using a Jaffe method and calibrated to nationally representative estimates as previously described.25 GFR was estimated based on serum creatinine using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation (eGFRCKD-EPI).26 Plasma total cholesterol, triglycerides and low-density lipoprotein (LDL) cholesterol were measured as previously described.27, 28, 29 Hypertension was defined by diastolic blood pressure ⩾90 mm Hg, systolic blood pressure ⩾140 mm Hg or use of antihypertensive medication. The prevalence of diabetes was defined using a fasting glucose level ⩾7.0 mmol l−1, a nonfasting glucose level ⩾11.1 mmol l−1 and/or self-reported physician diagnosis or treatment for diabetes. Body mass index (BMI) was calculated as weight in kilograms/(height in meters2). Information on cigarette smoking and alcohol consumption was obtained using an interviewer-administered questionnaire, and smoking and drinking status were classified as current, former or never. Usual intake of alcohol in grams/week was calculated for current drinkers;30 the usual weekly intake was set to zero for former or never drinkers. Genotyping of apolipoprotein E (APOE) polymorphisms at codons 112 and 158 (ref. 31) was performed using the TaqMan system (Thermo Fisher Scientific, Waltham, MA, USA) to generate the six APOE genotypes. The genotype call rate, or the percentage of samples to which a genotype was assigned, was determined prior to exclusion of individuals from the analysis and was 92.5%.
Metabolomics
Metabolomic profiles were measured in a subsample of 1977 randomly selected African American study participants from the Jackson, Mississippi field center who had given consent for use of genetic information as previously described.18 Metabolites were detected and quantified by Metabolon (Durham, NC, USA) in serum isolated from individuals who had fasted ⩾8 h before the first clinical examination using an untargeted, gas chromatography/mass spectrometry, and a liquid chromatography–mass spectrometry-based method. Instrument variability was determined by calculating the median relative s.d. for the internal standards that were added to each sample prior to injection into the mass spectrometers. Overall process variability was determined by calculating the median relative s.d. for all endogenous metabolites (that is, non-instrument standards) present in 100% of the technical replicate samples created from a homogeneous pool of human plasma. As the measurements span multiple days, a data-normalization step was performed to correct variation resulting from instrument tuning differences between days. Metabolites were compared to library entries of purified standards that included retention times, molecular weights, preferred adducts, in-source fragments and associated fragmentation spectra of the intact parent ions, or to recurrent unknown compounds. After laboratory quality-control procedures described in detail elsewhere,18 this approach yielded a total of 602 metabolites, including 361 named compounds and 241 unnamed compounds that did not have a chemical standard. The unknown compounds are designated by X followed by numbers (e.g., X-12345) by Metabolon. After conducting a repeatability study to determine the stability of metabolites in two serum samples collected 4–6 weeks apart from 60 individuals, 204 metabolites were selected that met the criteria of a reliability coefficient of ⩾0.6 and <80% of values that were either missing or below the limit of detection.18 The reliability coefficient is an intraclass-correlation coefficient32 calculated as the ratio of between-individual variance and the sum of between-individual variance and within-individual variance over time. Using the intraclass-correlation coefficient, a group of metabolites was defined where the between-person variance accounts for most of the variability in metabolite concentrations, whereas within-person variance is relatively low, thus optimizing their usefulness for risk assessment.33, 34
Statistical analysis
The 204 metabolites described above were divided into two groups for statistical analysis (Supplementary Table S1). The first group was composed of 187 metabolites (108 named and 79 unnamed compounds) that were analyzed as continuous variables and had values above the limit of detection in ⩾50% of samples; values below the limit of detection were assigned the lowest detected value for that metabolite in all samples. The lowest detected values for the metabolites found to be significantly associated with incident hospitalized dementia or interindividual variation in performance on neurocognitive tests in this study are shown in Supplementary Table S2. Each of the 187 metabolites was centered by its mean and scaled by its s.d. prior to the analysis. A second group of 17 metabolites (10 named and 7 unnamed) with 50–80% of values that were below the limit of detection were analyzed as ordinal variables with the levels specified as follows: 1=below the limit of detection; 2=detected values below the median of the detected values; and 3=detected values at or higher than the median. Proportions, means and s.d.s were calculated for clinical and demographic characteristics for individuals categorized by incident dementia case status, and for all individuals for the analyses of cognitive function. Groups were compared using 2-tests for categorical variables and t-tests for continuous variables. Cox proportional hazards models were used to estimate the hazard ratio (HR) for developing hospitalized dementia; the median follow-up period was 17.1 years (25th percentile=10.8 years; 75th percentile=21.2 years). All HRs were calculated and reported per one s.d. increase for continuous variables, and per one category change for the categorical variables. Linear regression models were applied separately for each of the three cognitive tests (DWRT, DSST and WFT) for each metabolite to estimate its association with baseline cognitive function and 6-year cognitive change. Two multivariable models were used to evaluate the relationship between individual metabolites and both incident dementia and cognitive function. Model 1 was adjusted for age, gender, education defined as an ordinal variable (⩽11 years; 12–16 years; >16 years) and eGFR, whereas Model 2 was adjusted for the covariates in Model 1 with the addition of potential confounding variables including diabetes and hypertension case status, BMI, LDL cholesterol, current smoking, alcohol intake and APOE genotype (carriage of at least one ɛ4 allele) after exclusion of individuals with missing data.20, 35 The Dubey/Armitage-Parmar algorithm,36 a modified stepwise Bonferroni procedure, was used to correct for multiple comparisons as previously described,18 and a two-tailed P-value of 3.9 × 10−4 was considered statistically significant for each individual test. A power calculation was performed using the fixed sample size for each analysis and a pre-specified effect size reported from previous studies. For incident hospitalized dementia, more than 90% power will be reached if the sample size is 1534 (141 cases), the HR is 1.7,37, 38 the correlation between metabolites is 0.3 and the alpha level is 3.9 × 10−4. For the tests of association of baseline neurocognitive test scores and 6-year score change, assuming a small effect size of 0.02,39 five predictors (Model 1) and an alpha level of 3.9 × 10−4, there will be more than 90% and 80% power with sample sizes of 1577 and 1035, respectively. All statistical analyses were performed using R.40
Results
The clinical and demographic characteristics of the study sample are summarized in Table 1 for individuals included in the analyses of incident hospitalized dementia who were free of dementia and self-reported stroke or transient ischemic attack at baseline. Among the 1534 participants, 9.2% (n=141) were hospitalized with dementia during a median follow-up period of 17.1 years. Participants who developed dementia were significantly more likely to be older at baseline, have had 11 years or less of formal education, have hypertension or diabetes, have a lower eGFR and to bear at least one copy of the APOE ɛ4 allele that has been reproducibly associated with increased risk of AD41, 42, 43 and variation in cognitive function in non-demented community-dwelling adults35, 44, 45, 46, 47 (P<0.05). Individuals without prevalent stroke at visit 1 or incident clinical stroke between visits 1 and 4 were included in the analyses of baseline cognitive function and 6-year cognitive change, and the characteristics of this study sample are shown in Table 2. As a randomly selected subsample of African American ARIC study participants with metabolomics profiles were included in this analysis, the clinical and demographic characteristics of those with and without available data were compared (Supplementary Table S3). Individuals with metabolomics data were significantly younger and less likely to be male or have diabetes or hypertension, and also had a higher eGFR than ARIC participants who were not chosen for measurements of the metabolome.
Two unnamed compounds (X-11423, X-11491) were significantly associated with incident hospitalized dementia in the minimally adjusted Cox proportional hazards model but were no longer associated with susceptibility to dementia after further adjustment for a panel of established risk factors, whereas another metabolite implicated in sex steroid metabolism (5 alpha-androstan-3 beta, 17 beta-diol disulfate) and an unnamed compound (X-12851) were significantly associated with elevated dementia risk only after adjustment for all covariates (Table 3). Three metabolites were significantly associated with increased hospitalized dementia using both the minimally adjusted and full Cox proportional hazards regression models including two named compounds involved in sex steroid metabolism (pregnen-diol disulfate and 4-androsten-3 beta, 17 beta-diol disulfate 1) and one metabolite with unknown structural identity (X-11440). Secondary analyses stratified by gender revealed that the two androgen sulfates were either significantly or marginally significantly associated with incident dementia in men (Table 4), although there was no association observed in women. The associations appeared to be similar in men and women for pregnen-diol disulfate.
In the analyses of 6-year cognitive change, the N-acetylated amino acid N-acetyl-1-methylhistidine was associated with greater decline in scores on the DWRT, and two metabolites (docosapentaenoate (DPA) and X-12844) were associated with less decline in scores on the DSST only in the fully adjusted models (Table 5). DPA (22:5 n-6) is a long-chain n-6 polyunsaturated fatty acid (PUFA). Long-chain PUFAs are lipids at least 18 carbons in length with two or more double bonds that are categorized as n-3 or n-6 based on the position of the first double bond with respect to the omega or last carbon end of the molecule. Although a significant relationship between five individual metabolites and baseline cognitive function was observed for the DSST using the minimally adjusted model, none remained significant after further adjustment for lifestyle and physiological factors. No metabolites were associated with either performance on the WFT at baseline or with change in scores over the 6-year interval.
Discussion
Associations between the levels of three sulfate-conjugated sex steroid hormones and increased risk of incident hospitalized dementia, the omega-6 fatty acid DPA and less decline in processing speed, and an N-acetylated amino acid and greater decline in verbal memory were identified in a large-scale screen of serum metabolites in middle-aged African American participants in the ARIC study. Although the phenotype examined in this study was incident hospitalized dementia that encompassed AD and vascular dementia as well as other forms of dementia, several investigators have previously observed significant alterations in metabolic profiles in cerebrospinal fluid,7, 8, 48, 49, 50, 51 or blood6, 7, 9, 10, 11, 12, 13, 14 in comparisons of patients with MCI or AD to cognitively normal subjects. Because sample acquisition is less invasive, identification of blood-based biomarkers would be advantageous for clinical diagnosis, AD-screening programs and monitoring of response to therapy. Mapstone et al. recently reported that a set of 10 lipids identified in a metabolomics screen in peripheral blood could be used with 90% accuracy to predict conversion from normal cognitive status to amnestic MCI or AD dementia over a 2–3-year period in 525 community-dwelling adults ⩾70 years.6 Although these findings were not replicated in three independent cohorts including the ARIC study,52, 53 higher concentrations of one of the 10 phospholipids was significantly associated with a decreased prevalence of dementia.54 Alterations in lipid metabolic pathways detected in the blood of patients with AD dementia have also been described by other investigators.9, 10, 11, 12, 13, 14 For example, significantly decreased plasma concentrations of three phosphatidylcholines were observed when individuals with AD dementia were compared to controls from the King’s College London Dementia Case Register and the AddNeuroMed study,12 and six ether-containing phosphatidylcholines and sphingomyelins were associated with abnormal levels of Aβ1–42 in the cerebrospinal fluid in participants in the Alzheimer’s Disease Neuroimaging Initiative-1 cohort.14 A group of 154 metabolites associated with AD dementia was identified in the Mayo Clinic Study of Aging including etiocholanolone sulfate (5-androstan-3-alpha-ol-17-one sulfate) and testosterone sulfate, two metabolites of testosterone.7 Most of the metabolites described in the studies above6, 7, 8, 9, 10, 11, 12, 13, 14, 48, 49, 50, 51 were not included in the panel analyzed in the ARIC study, with the exception of uridine,7, 48 creatine,7 dimethylglycine,7 tryptophan,7, 49 2-hydroxyisobutyrate7 and valine.14 Providing evidence in support of an initial discovery in Alzheimer’s Disease Neuroimaging Initiative-1, higher levels of the branched-chain amino acid valine were significantly positively associated with general cognitive ability and conferred a decreased risk of incident AD dementia over a median 9.7-year follow-up period in 2505 dementia-free participants in the population-based Rotterdam Study.14 However, among these metabolites, only dimethylglycine was nominally associated with incident hospitalized dementia using the fully adjusted Cox regression model (P=0.0252).
In the ARIC study, profiling of serum metabolites by an untargeted mass spectrometry-based method revealed associations between increased risk of incident hospitalized dementia and three metabolites involved in sex steroid metabolism including 4-androsten-3 beta, 17 beta-diol disulfate 1 (sulfate of 4-androsetenediol; HR=1.25, P=1.44 × 10−4), 5 alpha-androstan-3 beta, 17 beta-diol disulfate (HR=1.26, P=1.64 × 10−4) and pregnen-diol disulfate (HR=1.35, P=5.59 × 10−5) and two unnamed metabolites after adjustment for a panel of established risk factors for cognitive function.35 The regression models were also adjusted for eGFR, as the kidney freely filters molecules weighing less than 10 000 Da from the blood that are then reabsorbed, catabolized and/or secreted so that interindividual variation in renal function can influence metabolite concentrations.55 The association with 4-androsten-3 beta, 17 beta-diol disulfate 1 was replicated in European American ARIC study participants, providing stronger evidence that levels of this hormone influence susceptibility to dementia. As both androgens and estrogens have been shown to exert neuroprotective effects including prevention of amyloid beta deposition and tau hyperphosphorylation,56, 57, 58, 59, 60 age-related depletion of sex steroid hormones might be expected to contribute to an increased susceptibility to neurodegenerative diseases. Accordingly, age-related decline in circulating estrogens and testosterone has previously been reported to be a risk factor for AD dementia or MCI in women and men, respectively, in some61, 62, 63, 64, 65, 66, 67 but not all studies.68 The relationship between steroid hormones and AD has also been evaluated directly in samples of neural tissue.69, 70 Although these previous reports provide support for the suggestion that interindividual variation in the levels of the three sex steroid metabolites may be biologically linked to cognitive impairment, important caveats are that dementia as defined in this study was based on hospital ICD-9 codes and was not restricted to AD, and that even many cases of clinically diagnosed dementias including AD show a mixture of AD and vascular neuropathology at autopsy.71, 72, 73
Four-androstenediol is a precursor of both testosterone and estradiol, and is used as a prohormone by men to elevate levels of serum and urinary testosterone.74, 75 5-alpha-androstan-3-beta, 17-beta-diol (3-betaAdiol) is a metabolite of the androgen dihydrotestosterone. Pregnen-diol disulfate has not been well characterized. An increase in the levels of sulfated intermediates in steroid metabolism in individuals with incident hospitalized dementia could reflect alterations in a number of biological processes. The major site of clearance and inactivation of steroids is the liver where conjugation with sulfuric acid is one mechanism whereby the compounds become water-soluble and can be excreted in the urine.76 Changes in the rate of steroid clearance in individuals with dementia may be reflected in the increased levels detectable in the serum. Another possibility is that, as hydrolysis of steroid sulfates by steroid sulfatase in the liver, kidney and other tissues can contribute to the pool of unconjugated androgens,77 as yet undescribed variation in this enzymatic reaction may also be a factor.
To our knowledge, this study is among the first to examine the association between the human metabolome and change in cognitive function among middle-aged adults who are not cognitively impaired using scores on standardized neuropsychological tests. Higher levels of an N-acetylated amino acid previously associated with lower eGFR in African American ARIC study participants were significantly associated with greater decline in scores on the DWRT, a test of verbal declarative memory.55 Although lower eGFR has been shown to be associated with impairment in delayed word recall in patients with chronic kidney disease,78, 79 N-acetyl-1-methylhistidine was significantly associated with memory performance after adjustment for eGFR, suggesting an effect on cognition that is independent of its role in renal function. The DSST is a test widely used to measure information-processing speed while an individual translates numbers to letters on a paper and pencil test. The rate of information-processing speed has been shown to decrease in older individuals,80, 81 and low scores on the DSST indicative of poor performance in this domain have been associated with MCI and early-stage dementia.82, 83 Higher n-6 DPA levels were associated with less decline in DSST scores over a 6-year period in ARIC study participants (β=1.25, P=9.47 × 10−5). DPA is a long-chain n-6 PUFA found in vegetable oil that can also be metabolized from the essential fatty acid linoleic acid (18:2 n-6) or from arachidonic acid (20:4 n-6) by a series of chain elongation and desaturation reactions.84 The higher serum DPA levels may indicate an increased rate of conversion from either linoleic acid or arachidonic acid to n-6 DPA in those with less pronounced DSST score change. Genetic variants in enzymes involved in the n-6 metabolic pathway have been associated with linoleic acid and arachidonic acid levels, and could potentially underlie the observed variation in cognitive status.85, 86
Dietary intake of omega-6 fatty acids has previously been shown to be associated with a lower risk of AD, MCI, cognitive decline and all-cause mortality,87, 88, 89, 90 although increased risk has also been reported.91, 92, 93 For example, intake of omega-6 polyunsaturated fat was inversely associated with incident clinically diagnosed AD in a biracial sample of 815 participants from the Chicago Health and Aging Project,87 and the odds ratio of MCI decreased as intake of omega-6 fatty acids increased in 1233 individuals in the Mayo Clinic Study of Aging.88 In one of the only studies to specifically address the association between n-6 DPA and cognitive status, erythrocyte DPA levels were higher in adults older than 65 years with MCI than in healthy controls.94 Of particular relevance to the results reported here, a higher ratio between total erythrocyte n-6-PUFAs and n3-PUFAs was significantly negatively correlated with baseline DSST scores in the Lothian Birth Cohort 1936 study.95 However, as all n-6 PUFAs were considered as a group, it is possible that individual components such as DPA exerted a range of effects in different directions that could not be distinguished in the assay used. Although there may be many reasons for the inconsistent results reported across studies, many relied on food frequency questionnaires or interviews87, 88, 89, 92, 93 that are subject to recall bias rather than on laboratory measurements of metabolites as reported here. Most importantly, both the neuropsychological test batteries used to evaluate cognition and the individual omega-6 fatty acids chosen for analysis either alone or as components of a composite measure often varied between cohorts, and a large-scale hypothesis-free screen of the metabolome was not undertaken except in the ARIC study. Further research optimally relying on the use of the same cognitive tests to assess change over a similar time period may help to clarify whether increased levels of serum n-6 DPA are consistently associated with less decline in processing speed in early middle age.
Taken together, these results demonstrate that screening the metabolome in midlife can be used to discover and prioritize biologically plausible biomarkers that may improve risk stratification for cognitive impairment at older ages. The strengths of the study include the prospective design and a large deeply phenotyped cohort that allowed the detection of an association between novel biomarkers and incident hospitalized dementia decades before it came to medical attention, as well as early cognitive change in non-demented community-dwelling adults. There are also limitations. Only one cognitive test was used to measure each of three cognitive domains, and cognitive change was analyzed over a short period in middle age when relatively few participants will have undergone substantial decline. Finally, there was only a single measurement of the serum metabolites, although rigorous quality-control procedures were undertaken to assure medium term reliability of the data, and the identity of some of the metabolites significantly associated with both phenotypes is currently unknown. While the association between a sex steroid hormone significantly associated with incident hospitalized dementia in African Americans was replicated in European American study participants, evaluation of the same metabolites in an independent replication sample of African Americans and across different ethnicities to address the generalizability of the findings is warranted.
References
Alzheimer's Association. 2016 Alzheimer's disease facts and figures. Alzheimers Dement 2016; 12: 459–509.
Fitzpatrick AL, Kuller LH, Ives DG, Lopez OL, Jagust W, Breitner JC et al. Incidence and prevalence of dementia in the Cardiovascular Health Study. J Am Geriatr Soc 2004; 52: 195–204.
Seshadri S, Beiser A, Kelly-Hayes M, Kase CS, Au R, Kannel WB et al. The lifetime risk of stroke: estimates from the Framingham Study. Stroke 2006; 37: 345–350.
McClearn GE, Johansson B, Berg S, Pedersen NL, Ahern F, Petrill SA et al. Substantial genetic influence on cognitive abilities in twins 80 or more years old. Science 1997; 276: 1560–1563.
Swan GE, Carmelli D, Reed T, Harshfield GA, Fabsitz RR, Eslinger PJ . Heritability of cognitive performance in aging twins. The National Heart, Lung, and Blood Institute Twin Study. Arch Neurol 1990; 47: 259–262.
Mapstone M, Cheema AK, Fiandaca MS, Zhong X, Mhyre TR, Macarthur LH et al. Plasma phospholipids identify antecedent memory impairment in older adults. Nat Med 2014; 20: 415–418.
Trushina E, Dutta T, Persson XM, Mielke MM, Petersen RC . Identification of altered metabolic pathways in plasma and CSF in mild cognitive impairment and Alzheimer's disease using metabolomics. PLoS ONE 2013; 8: e63644.
Kaddurah-Daouk R, Rozen S, Matson W, Han X, Hulette CM, Burke JR et al. Metabolomic changes in autopsy-confirmed Alzheimer's disease. Alzheimers Dement 2011; 7: 309–317.
Sato Y, Suzuki I, Nakamura T, Bernier F, Aoshima K, Oda Y . Identification of a new plasma biomarker of Alzheimer's disease using metabolomics technology. J Lipid Res 2012; 53: 567–576.
Han X, Rozen S, Boyle SH, Hellegers C, Cheng H, Burke JR et al. Metabolomics in early Alzheimer's disease: identification of altered plasma sphingolipidome using shotgun lipidomics. PLoS ONE 2011; 6: e21643.
Oresic M, Hyotylainen T, Herukka SK, Sysi-Aho M, Mattila I, Seppanan-Laakso T et al. Metabolome in progression to Alzheimer's disease. Transl Psychiatry 2011; 1: e57.
Whiley L, Sen A, Heaton J, Proitsi P, Garcia-Gomez D, Leung R et al. Evidence of altered phosphatidylcholine metabolism in Alzheimer's disease. Neurobiol Aging 2014; 35: 271–278.
Proitsi P, Kim M, Whiley L, Simmons A, Sattlecker M, Velayudhan L et al. Association of blood lipids with Alzheimer's disease: A comprehensive lipidomics analysis. Alzheimers Dement 2017; 13: 140–151.
Toledo JB, Arnold M, Kastenmuller G, Chang R, Baillie RA, Han X et al. Metabolic network failures in Alzheimer's disease-A biochemical road map. Alzheimers Dement 2017 (e-pub ahead of print 21 March 2017).
Tang MX, Cross P, Andrews H, Jacobs DM, Small S, Bell K et al. Incidence of AD in African-Americans, Caribbean Hispanics, and Caucasians in northern Manhattan. Neurology 2001; 56: 49–56.
Demirovic J, Prineas R, Loewenstein D, Bean J, Duara R, Sevush S et al. Prevalence of dementia in three ethnic groups: the South Florida program on aging and health. Ann Epidemiol 2003; 13: 472–478.
The ARIC investigators. The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. Am J Epidemiol 1989; 129: 687–702.
Zheng Y, Yu B, Alexander D, Manolio TA, Aguilar D, Coresh J et al. Associations between metabolomic compounds and incident heart failure among African Americans: the ARIC Study. Am J Epidemiol 2013; 178: 534–542.
Alonso A, Mosley TH Jr., Gottesman RF, Catellier D, Sharrett AR, Coresh J . Risk of dementia hospitalisation associated with cardiovascular risk factors in midlife and older age: the Atherosclerosis Risk in Communities (ARIC) study. J Neurol Neurosurg Psychiatry 2009; 80: 1194–1201.
Cerhan JR, Folsom AR, Mortimer JA, Shahar E, Knopman DS, McGovern PG et al. Correlates of cognitive function in middle-aged adults. Atherosclerosis Risk in Communities (ARIC) Study Investigators. Gerontology 1998; 44: 95–105.
Knopman DS, Ryberg S . A verbal memory test with high predictive accuracy for dementia of the Alzheimer type. Arch Neurol 1989; 46: 141–145.
Wechsler D . The Adult Intelligence Scale - Revised. Psychological Corporation: New York, NY, USA, 1981.
Lezak M . Neuropsychological Assessment. Oxford University Press: Oxford, UK, 1995.
Tombaugh TN, Kozak J, Rees L . Normative data stratified by age and education for two measures of verbal fluency: FAS and animal naming. Arch Clin Neuropsychol 1999; 14: 167–177.
Manjunath G, Tighiouart H, Ibrahim H, MacLeod B, Salem DN, Griffith JL et al. Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community. J Am Coll Cardiol 2003; 41: 47–55.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009; 150: 604–612.
Nagele U, Hagele EO, Sauer G, Wiedemann E, Lehmann P, Wahlefeld AW et al. Reagent for the enzymatic determination of serum total triglycerides with improved lipolytic efficiency. J Clin Chem Clin Biochem 1984; 22: 165–174.
Siedel J, Hagele EO, Ziegenhorn J, Wahlefeld AW . Reagent for the enzymatic determination of serum total cholesterol with improved lipolytic efficiency. Clin Chem 1983; 29: 1075–1080.
Friedewald WT, Levy RI, Fredrickson DS . Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972; 18: 499–502.
Demirovic J, Nabulsi A, Folsom AR, Carpenter MA, Szklo M, Sorlie PD et al. Alcohol consumption and ultrasonographically assessed carotid artery wall thickness and distensibility. The Atherosclerosis Risk in Communities (ARIC) Study Investigators. Circulation 1993; 88: 2787–2793.
Weisgraber KH, Rall SC Jr., Mahley RW . Human E apoprotein heterogeneity. Cysteine-arginine interchanges in the amino acid sequence of the apo-E isoforms. J Biol Chem 1981; 256: 9077–9083.
Fleiss J. Reliability of measurement. In: Fleiss J (ed). The Design and Analysis of Clinical Experiments. Wiley and Sons: New York, NY, USA, 1986, pp 1–32.
Floegel A, Drogan D, Wang-Sattler R, Prehn C, Illig T, Adamski J et al. Reliability of serum metabolite concentrations over a 4-month period using a targeted metabolomic approach. PLoS ONE 2011; 6: e21103.
Zheng Y, Yu B, Alexander D, Couper DJ, Boerwinkle E . Medium-term variability of the human serum metabolome in the Atherosclerosis Risk in Communities (ARIC) study. Omics 2014; 18: 364–373.
Blair CK, Folsom AR, Knopman DS, Bray MS, Mosley TH, Boerwinkle E et al. APOE genotype and cognitive decline in a middle-aged cohort. Neurology 2005; 64: 268–276.
Sankoh AJ, Huque MF, Dubey SD . Some comments on frequently used multiple endpoint adjustment methods in clinical trials. Stat Med 1997; 16: 2529–2542.
van Oijen M, Witteman JC, Hofman A, Koudstaal PJ, Breteler MM . Fibrinogen is associated with an increased risk of Alzheimer disease and vascular dementia. Stroke 2005; 36: 2637–2641.
Beydoun MA, Beydoun HA, Gamaldo AA, Teel A, Zonderman AB, Wang Y . Epidemiologic studies of modifiable factors associated with cognition and dementia: systematic review and meta-analysis. BMC Public Health 2014; 14: 643.
Cohen J . Statistical Power Analysis for the Behavioral Sciences. 2nd edn, Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988.
R Development Core Team R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria, 2014.
Strittmatter WJ, Saunders AM, Schmechel D, Pericak-Vance M, Enghild J, Salvesen GS et al. Apolipoprotein E: high-avidity binding to beta-amyloid and increased frequency of type 4 allele in late-onset familial Alzheimer disease. Proc Natl Acad Sci USA 1993; 90: 1977–1981.
Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer's disease in late onset families. Science 1993; 261: 921–923.
Farrer LA, Cupples LA, Haines JL, Hyman B, Kukull WA, Mayeux R et al. Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer disease. A meta-analysis. APOE and Alzheimer Disease Meta Analysis Consortium. JAMA 1997; 278: 1349–1356.
Kuller LH, Shemanski L, Manolio T, Haan M, Fried L, Bryan N et al. Relationship between ApoE, MRI findings, and cognitive function in the Cardiovascular Health Study. Stroke 1998; 29: 388–398.
Bretsky P, Guralnik JM, Launer L, Albert M, Seeman TE . MacArthur Studies of Successful Aging. The role of APOE-epsilon4 in longitudinal cognitive decline: MacArthur Studies of Successful Aging. Neurology 2003; 60: 1077–1081.
Mayeux R, Small SA, Tang M, Tycko B, Stern Y . Memory performance in healthy elderly without Alzheimer's disease: effects of time and apolipoprotein-E. Neurobiol Aging 2001; 22: 683–689.
Slooter AJ, van Duijn CM, Bots ML, Ott A, Breteler MB, De Voecht J et al. Apolipoprotein E genotype, atherosclerosis, and cognitive decline: the Rotterdam Study. J Neural Trans Suppl 1998; 53: 17–29.
Czech C, Berndt P, Busch K, Schmitz O, Wiemer J, Most V et al. Metabolite profiling of Alzheimer's disease cerebrospinal fluid. PLoS ONE 2012; 7: e31501.
Kaddurah-Daouk R, Zhu H, Sharma S, Bogdanov M, Rozen SG, Matson W et al. Alterations in metabolic pathways and networks in Alzheimer's disease. Transl Psychiatry 2013; 3: e244.
Koal T, Klavins K, Seppi D, Kemmler G, Humpel C . Sphingomyelin SM (d18:1/18:0) is Significantly Enhanced in Cerebrospinal Fluid Samples Dichotomized by Pathological Amyloid-beta42, Tau, and Phospho-Tau-181 Levels. J Alzheim Dis 2014; 44: 1193–1201.
Klavins K, Koal T, Dallmann G, Marksteiner J, Kemmler G, Humpel C . The ratio of phosphatidylcholines to lysophosphatidylcholines in plasma differentiates healthy controls from patients with Alzheimer's disease and mild cognitive impairment. Alzheimers Dement 2015; 1: 295–302.
Casanova R, Varma S, Simpson B, Kim M, An Y, Saldana S et al. Blood metabolite markers of preclinical Alzheimer's disease in two longitudinally followed cohorts of older individuals. Alzheimers Dement 2016; 12: 815–822.
Li D, Misialek JR, Boerwinkle E, Gottesman RF, Sharrett AR, Mosley TH et al. Prospective associations of plasma phospholipids and mild cognitive impairment/dementia among African Americans in the ARIC Neurocognitive Study. Alzheimers Dement 2017; 6: 1–10.
Li D, Misialek JR, Boerwinkle E, Gottesman RF, Sharrett AR, Mosley TH et al. Plasma phospholipids and prevalence of mild cognitive impairment and/or dementia in the ARIC Neurocognitive Study (ARIC-NCS). Alzheimers Dement 2016; 3: 73–82.
Yu B, Zheng Y, Nettleton JA, Alexander D, Coresh J, Boerwinkle E . Serum metabolomic profiling and incident CKD among African Americans. Clin J Am Soc Nephrol 2014; 9: 1410–1417.
Gouras GK, Xu H, Gross RS, Greenfield JP, Hai B, Wang R et al. Testosterone reduces neuronal secretion of Alzheimer's beta-amyloid peptides. Proc Natl Acad Sci USA 2000; 97: 1202–1205.
Gandy S . Estrogen and neurodegeneration. NeurochemRes 2003; 28: 1003–1008.
Pike CJ, Carroll JC, Rosario ER, Barron AM . Protective actions of sex steroid hormones in Alzheimer's disease. Front Neuroendocrinol 2009; 30: 239–258.
Vest RS, Pike CJ . Gender, sex steroid hormones, and Alzheimer's disease. Hormones Behav 2013; 63: 301–307.
Holland J, Bandelow S, Hogervorst E . Testosterone levels and cognition in elderly men: a review. Maturitas 2011; 69: 322–337.
Barron AM, Pike CJ . Sex hormones, aging, and Alzheimer's disease. Front Biosci 2012; 4: 976–997.
Jayaraman A, Pike CJ . Alzheimer's dsease and type 2 diabetes: multiple mechanisms contribute to interactions. Curr Diabetes Rep 2014; 14: 476.
Verdile G, Laws SM, Henley D, Ames D, Bush AI, Ellis KA et al. Associations between gonadotropins, testosterone and beta amyloid in men at risk of Alzheimer's disease. Mol Psychiatry 2014; 19: 69–75.
Manly JJ, Merchant CA, Jacobs DM, Small SA, Bell K, Ferin M et al. Endogenous estrogen levels and Alzheimer's disease among postmenopausal women. Neurology 2000; 54: 833–837.
Hogervorst E, Williams J, Budge M, Barnetson L, Combrinck M, Smith AD . Serum total testosterone is lower in men with Alzheimer's disease. Neuroendocrinol Lett 2001; 22: 163–168.
Hogervorst E, Combrinck M, Smith AD . Testosterone and gonadotropin levels in men with dementia. Neuroendocrinol Lett 2003; 24: 203–208.
Moffat SD, Zonderman AB, Metter EJ, Kawas C, Blackman MR, Harman SM et al. Free testosterone and risk for Alzheimer disease in older men. Neurology 2004; 62: 188–193.
Ponholzer A, Madersbacher S, Rauchenwald M, Jungwirth S, Fischer P, Tragl KH . Serum androgen levels and their association to depression and Alzheimer dementia in a cohort of 75-year-old men over 5 years: results of the VITA study. Int J Impotence Res 2009; 21: 187–191.
Rosario ER, Chang L, Stanczyk FZ, Pike CJ . Age-related testosterone depletion and the development of Alzheimer disease. JAMA 2004; 292: 1431–1432.
Rosario ER, Chang L, Head EH, Stanczyk FZ, Pike CJ . Brain levels of sex steroid hormones in men and women during normal aging and in Alzheimer's disease. Neurobiol Aging 2011; 32: 604–613.
Lopez OL, Kuller LH, Fitzpatrick A, Ives D, Becker JT, Beauchamp N . Evaluation of dementia in the cardiovascular health cognition study. Neuroepidemiology 2003; 22: 1–12.
Fernando MS, Ince PG,, MRC Cognitive Function and Ageing Neuropathology Study Group. Vascular pathologies and cognition in a population-based cohort of elderly people. J Neurol Sci 2004; 226: 13–17.
Schneider JA, Arvanitakis Z, Leurgans SE, Bennett DA . The neuropathology of probable Alzheimer disease and mild cognitive impairment. Ann Neurol 2009; 66: 200–208.
Uralets VP, Gillette PA . Over-the-counter anabolic steroids 4-androsten-3,17-dione; 4-androsten-3beta,17beta-diol; and 19-nor-4-androsten-3,17-dione: excretion studies in men. J Anal Toxicol 1999; 23: 357–366.
Broeder CE . Oral andro-related prohormone supplementation: do the potential risks outweigh the benefits? Can J Appl Physiol 2003; 28: 102–116.
Schanzer W . Metabolism of anabolic androgenic steroids. Clin Chem 1996; 42: 1001–1020.
Reed MJ, Purohit A, Woo LW, Newman SP, Potter BV . Steroid sulfatase: molecular biology, regulation, and inhibition. Endocr Rev 2005; 26: 171–202.
Yaffe K, Ackerson L, Kurella Tamura M, Le Blanc P, Kusek JW, Sehgal AR et al. Chronic kidney disease and cognitive function in older adults: findings from the chronic renal insufficiency cohort cognitive study. J Am Geriatr Soc 2010; 58: 338–345.
Bugnicourt JM, Godefroy O, Chillon JM, Choukroun G, Massy ZA . Cognitive disorders and dementia in CKD: the neglected kidney-brain axis. J Am Soc Nephrol 2013; 24: 353–363.
Salthouse TA . The processing-speed theory of adult age differences in cognition. Psychol Rev 1996; 103: 403–428.
Der G, Deary IJ . Age and sex differences in reaction time in adulthood: results from the United Kingdom Health and Lifestyle Survey. Psychol Aging 2006; 21: 62–73.
Lopez OL, Jagust WJ, Dulberg C, Becker JT, DeKosky ST, Fitzpatrick A et al. Risk factors for mild cognitive impairment in the Cardiovascular Health Study Cognition Study: part 2. Arch Neurol 2003; 60: 1394–1399.
Twamley EW, Ropacki SA, Bondi MW . Neuropsychological and neuroimaging changes in preclinical Alzheimer's disease. J Int NeuropsycholSoc 2006; 12: 707–735.
Sprecher H, Luthria DL, Mohammed BS, Baykousheva SP . Reevaluation of the pathways for the biosynthesis of polyunsaturated fatty acids. J Lipid Res 1995; 36: 2471–2477.
Tanaka T, Shen J, Abecasis GR, Kisialiou A, Ordovas JM, Guralnik JM et al. Genome-wide association study of plasma polyunsaturated fatty acids in the InCHIANTI Study. PLoS Genet 2009; 5: e1000338.
Guan W, Steffen BT, Lemaitre RN, Wu JH, Tanaka T, Manichaikul A et al. Genome-wide association study of plasma N6 polyunsaturated fatty acids within the cohorts for heart and aging research in genomic epidemiology consortium. Circ Cardiovasc Genet 2014; 7: 321–331.
Morris MC, Evans DA, Bienias JL, Tangney CC, Bennett DA, Aggarwal N et al. Dietary fats and the risk of incident Alzheimer disease. Arch Neurol 2003; 60: 194–200.
Roberts RO, Cerhan JR, Geda YE, Knopman DS, Cha RH, Christianson TJ et al. Polyunsaturated fatty acids and reduced odds of MCI: the Mayo Clinic Study of Aging. J Alzheim Dis 2010; 21: 853–865.
Solfrizzi V, Colacicco AM, D'Introno A, Capurso C, Torres F, Rizzo C et al. Dietary intake of unsaturated fatty acids and age-related cognitive decline: a 8.5-year follow-up of the Italian Longitudinal Study on Aging. Neurobiol Aging 2006; 27: 1694–1704.
Wu JH, Lemaitre RN, King IB, Song X, Psaty BM, Siscovick DS et al. Circulating omega-6 polyunsaturated fatty acids and total and cause-specific mortality: the Cardiovascular Health Study. Circulation 2014; 130: 1245–1253.
Heude B, Ducimetiere P, Berr C,, EVA Study. Cognitive decline and fatty acid composition of erythrocyte membranes—The EVA Study. Am J Clin Nutr 2003; 77: 803–808.
Kalmijn S, Feskens EJ, Launer LJ, Kromhout D . Polyunsaturated fatty acids, antioxidants, and cognitive function in very old men. Am J Epidemiol 1997; 145: 33–41.
Barberger-Gateau P, Raffaitin C, Letenneur L, Berr C, Tzourio C, Dartigues JF et al. Dietary patterns and risk of dementia: the Three-City cohort study. Neurology 2007; 69: 1921–1930.
Milte CM, Sinn N, Street SJ, Buckley JD, Coates AM, Howe PR . Erythrocyte polyunsaturated fatty acid status, memory, cognition and mood in older adults with mild cognitive impairment and healthy controls. Prostaglandins Leukot Essent Fatty Acids 2011; 84: 153–161.
Whalley LJ, Fox HC, Wahle KW, Starr JM, Deary IJ . Cognitive aging, childhood intelligence, and the use of food supplements: possible involvement of n-3 fatty acids. Am J Clin Nutr 2004; 80: 1650–1657.
Acknowledgements
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by the National Heart, Lung, and Blood Institute contracts (HHSN2628201100005C, HHSN2628201100006C, HHSN2628201100007C, HHSN2628201100008C, HHSN2628201100009C, HHSN2628201100010C, HHSN2628201100011C and HHSN2628201100012C. We thank the staff and participants of the ARIC study for their important contributions. The metabolomics research was sponsored by the National Human Genome Research Institute (grant 3U01HG004402-02S1).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Knopman served as Deputy Editor for Neurology until October 2015 and received compensation from the American Academy of Neurology. He serves on a Data Safety Monitoring Board for Lundbeck Pharmaceuticals and for the DIAN study, and is an investigator in clinical trials sponsored by TauRX Pharmaceuticals, Lilly Pharmaceuticals and the Alzheimer’s Disease Cooperative Study. The remaining authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Translational Psychiatry website .
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Bressler, J., Yu, B., Mosley, T. et al. Metabolomics and cognition in African American adults in midlife: the atherosclerosis risk in communities study. Transl Psychiatry 7, e1173 (2017). https://doi.org/10.1038/tp.2017.118
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2017.118
This article is cited by
-
Genetic loci of beta-aminoisobutyric acid are associated with aging-related mild cognitive impairment
Translational Psychiatry (2023)
-
Plasma nervonic acid levels were negatively associated with attention levels in community-living older adults in New Zealand
Metabolomics (2022)
-
The Contribution of Kidney Disease to Cognitive Impairment in Patients with Type 2 Diabetes
Current Diabetes Reports (2020)
-
Nutrition and Metabolic Profiles in the Natural History of Dementia: Recent Insights from Systems Biology and Life Course Epidemiology
Current Nutrition Reports (2019)