Abstract
Poststroke depression (PSD) occurs in approximately one-third of stroke survivors and is one of the serious sequelae of stroke. The onset of PSD causes delayed functional recovery by rehabilitation and also increases cognitive impairment. However, appropriate strategies for the therapy against ischemia-induced depression-like behaviors still remain to be developed. Such behaviors have been associated with a reduced level of brain-derived neurotrophic factor (BDNF). In addition, accumulating evidence indicates the ability of stem cells to improve cerebral ischemia-induced brain injuries. However, it remains to be clarified as to the effect of neural progenitor cells (NPCs) on PSD and the association between BDNF level and PSD. Using NPCs, we investigated the effect of intravenous injection of NPCs on PSD. We showed that injection of NPCs improved ischemia-induced depression-like behaviors in the forced-swimming test and sucrose preference test without having any effect on the viable area between vehicle- and NPC-injected ischemic rats. The injection of NPCs prevented the decrease in the level of BDNF in the ipsilateral hemisphere. The levels of phosphorylated CREB, ERK and Akt, which have been implicated in events downstream of BDNF signaling, were also decreased after cerebral ischemia. NPC injection inhibited these decreases in the phosphorylation of CREB and ERK, but not that of Akt. Our findings provide evidence that injection of NPCs may have therapeutic potential for the improvement of depression-like behaviors after cerebral ischemia and that these effects might be associated with restoring BDNF-ERK-CREB signaling.
Similar content being viewed by others
Introduction
Stroke is the most common severe neurological disorder and a major cause of mortality among adults, followed by cancer and myocardial infarction.1 In addition, stroke survivors suffer severe aftereffects, including motor dysfunction, cognitive impairment and mood disorder. Poststroke depression (PSD), occurring in approximately one-third of stroke survivors, is a serious sequelae of stroke.2 The onset of PSD causes delayed recovery from the cerebral infarction, adversely affects motor function recovery by rehabilitation,3 and increases cognitive impairment4 and the risk of suicide.5 Furthermore, it is likely that stroke patients may have relevant mood disorders despite good functional outcome.6 However, evidence for effective treatments for PSD has not been well developed.
Accumulating evidence has suggested that impaired neurogenesis is linked to affective disorders, including depression.7, 8 Furthermore, several lines of evidence indicate the ability of antidepressants to elicit neurogenesis, thus suggesting the importance of the latter in mediating the therapeutic effect of antidepressants.7, 9, 10 Proliferation of neural progenitor cells (NPCs) is enhanced by cerebral ischemia.11, 12, 13 It was demonstrated that newly generated cells migrate to the site of injury in the brain,14, 15 and that these migrated cells express markers of mature neurons.14, 16 The majority of newly generated endogenous neurons fail to survive, although some of them persist for up to 5 weeks after brain ischemia.14, 16 Therefore, it has been suggested that transplantation of cells would be one potential strategy for the treatment of stroke17, 18 and other progressive neurodegenerative diseases.
It was earlier reported that the transplantation of stem or progenitor cells induces improvement of motor and cognitive functions and neurological deficits. Indeed, we demonstrated previously that the injection of NPCs improves spatial learning and memory dysfunction, which were evaluated by performing a water maze task, after cerebral ischemia.19, 20 However, it remains to be clarified whether transplantation of NPCs can improve PSD.
Several studies have suggested that brain-derived neurotrophic factor (BDNF) is associated with the pathophysiology of depression.21, 22 In this regard, chronic stress reduces the expression of BDNF in the hippocampus,23 whereas chronic administration of an antidepressant increases BDNF expression there.24, 25, 26 Moreover, infusion of BDNF into the hippocampus exerts an antidepressant effect as assessed by the learned helplessness and forced-swimming test (FST) paradigms.22 Despite accumulating data suggesting an association between decreased brain BDNF levels and depression, there are no data regarding the effect of transplantation of NPCs on cerebral ischemia-induced depression or on the level of BDNF in the brain.
The aims of this study were to determine whether intravenous injection of NPCs could improve ischemia-induced depression-like behaviors. We furthermore sought to determine the molecular changes, including those in BDNF levels and ERK/CREB signaling, underlying the pathophysiology of cerebral ischemia-induced depression-like behaviors. As NPCs were prepared from green-fluorescent protein (GFP) transgenic rats by using the neurosphere method, cells derived from these NPCs were also characterized in situ after the intravenous injection of them into ischemic rats.
Materials and methods
NPC cultures
NPCs were prepared from gestational Day 14 fetal GFP transgenic rats as described previously.19, 27, 28 The GFP transgenic rats (Wistar-TgN (CAG-GFP) 184ys) used in this study were provided by National Bio Resource Project for the Rat in Japan (Kyoto, Japan). The origin and characteristics of the transgenic rats were described previously.29 Cells were seeded at a density of 50 000 cells per cm2 into non-treated flasks (Nalge Nunc International, New York, NY, USA) containing N-2 plus medium supplemented with 20 ng ml−1 epidermal growth factor and 20 ng ml−1 basic fibroblast growth factor (growth medium). NPCs were grown in culture as free-floating neurosphere, and 80% of the medium was exchanged for new growth medium on Day 4. For the experiments, neurospheres cultured for 6 days in vitro were used. The protocol was approved by the Committee of Animal Care and Welfare of Tokyo University of Pharmacy and Life Sciences.
For immunostaining of floating cultured neurospheres, they were incubated on poly-L-lysine (Sigma-Aldrich, St Louis, MO, USA)-coated slides for 1 h at 25 °C. The attached neurospheres were fixed for 30 min with 4% paraformaldehyde. The primary antibodies used for neurospheres were mouse monoclonal anti-nestin (BD Bioscience, Franklin, NJ, USA) and rabbit polyclonal anti-musashi-1 (Chemicon, Temecula, CA, USA). Omission of primary antibodies served as negative controls. No immunostaining was detected in the group of negative controls.
For differentiation, neurospheres were cultured for 6 days in vitro, followed by replacement of the medium with Dulbecco's modified Eagle's medium/F12 medium without epidermal growth factor and basic fibroblast growth factor on Day 7. The neurospheres were then cultured for 7 additional days. For immunostaining of differentiated NPCs, the following primary antibodies were used: mouse monoclonal anti-MAP2 (Sigma-Aldrich), detecting neurons; rabbit polyclonal anti-glial fibrillary acidic protein (GFAP) (DAKO, Carpinteria, CA, USA), labeling astrocytes; and mouse monoclonal anti-mouse monoclonal anti-oligodendrocytes (clone RIP) (Chemicon), marking oligodendrocytes.
The secondary antibodies used were as follows: fluorescein isothiocyanate-conjugated donkey anti-mouse immunoglobulin G (IgG) (Jackson Immunoresearch, West Grove, PA, USA) or Cy3-conjugated donkey anti-rabbit IgG (Jackson Immunoresearch). Fluorescence was detected using Olympus fluorescence microscopy (BX-52; Olympus, Tokyo, Japan) or with a KEYENCE BZ-8000 (KEYENCE, Osaka, Japan). Omission of primary antibodies served as negative controls, which showed no immunostaining.
Model of microsphere-induced cerebral embolism in rat
Male wistar rats weighing 220–250 g (Charles River Japan Inc., Atsugi, Japan) were used. The rats were maintained at 23±1 °C in a room with a constant humidity of 55±5% and a light cycle of 12-h light:12-h darkness. The rats had free access to food and water according to the National Institute of Health Guide for the Care and Use of Laboratory Animals and the Guidance for Experimental Animal Care issued by the Prime Minister's Office of Japan. The study was approved by the Committee of Animal Care and Welfare of Tokyo University of Pharmacy and Life Sciences.
Microsphere-induced cerebral embolism was performed by the method described previously.19, 30 After rats had been anesthetized by an intraperitoneal injection of 40 mg kg−1 sodium pentobarbital, the right external carotid and pterygo-palatine arteries were temporarily occluded with strings. Immediately, a needle connected to a polyethylene catheter (3 French Atom, Tokyo, Japan) was inserted into the right common carotid artery, and then 700 microspheres (47.5±0.5 μm in diameter; Perkin-Elmer Life Sciences, Waltham, MA, USA), suspended in 20% dextran solution, were injected into the right internal carotid artery through the cannula. After the injection, the needle was removed, and the puncture wound was repaired with surgical glue. The rats that underwent a sham operation received the same volume of vehicle without microspheres.
Neurological deficits
Neurological deficits of microsphere-embolized rats were scored on the basis of paucity of movement, truncal curvature and forced circling during locomotion according to the criteria described previously.31, 32 The score of each neurological deficit was rated from 3 to 0 (3, very severe; 2, severe; 1, moderate; 0, little or none). The rats with a total score of 7–9 points on Day 1 after cerebral embolism were used in this study.
Administration of NPCs
Neurospheres were dispersed in the enzyme solution and resuspended in N-2 plus medium to a final concentration of 1.0 × 106 cells/100 μl. The cell suspension (100 μl) was administered via the right femoral vein on Day 7 after the cerebral embolism. Vehicle was injected in a similar manner as the NPCs.
Behavioral test
A series of behavioral tests, including motor, sensory, reflex and balance tests, was performed on Days 1, 7, 14, 21 and 28 after cerebral embolism according to the modified Neurological Severity Scores (mNSS)33 by a researcher who was blinded to the experimental groups. The score of mNSS was rated from 0 to 18 (normal score, 0; maximal deficit score, 18). In this scoring system, 1 score point is awarded for the inability to perform the test or for the lack of a tested reflex; thus, the higher the score, the more severe is the injury.
Open-field test
The open-field test was performed on Day 28 after cerebral embolism according to a modified version of the test described previously.34 The open-field apparatus consisted of a square arena with black walls (90 × 90 × 45 cm3). The floor of the apparatus was divided equally into 25 squares marked by white lines. The rats were placed individually into the center of the arena and allowed to explore for 15 min. The locomotor activity was measured by counting the number of crossings (squares crossed with all paws). Before each session, the floor was cleaned.
Sucrose preference test
A battery of the sucrose preference test (SPT) was performed before surgery and on Days 7, 14, 21 and 28 after cerebral embolism. Rats were given access for 12 h (1900 hours until 0700 hours) to two drinking spouts (water and 1% sucrose solution) positioned side by side (1900 hours until 0700 hours) after water deprivation for 6 h. Bottle positions were switched at 6 h after the start of the test. At the end of test, the consumption was noted. Sucrose preference was calculated according to the following ratio: sucrose preference=(sucrose consumption (ml)/(water consumption (ml)+sucrose consumption (ml)) × 100.
Forced-swimming test
The FST was performed at Day 28 after surgery for the induction of cerebral embolism or on the sham animals. Rats were placed in a dark transparent acrylic cylinder (60 cm in height, 20 cm in diameter) filled to 30 cm with water (25±1 °C) and kept there for 15 min. Then, the animals were removed from the water, dried with towels and placed in their cage. The 5-min test session was conducted 24 h later, and the duration of immobility of the rats was recorded. Immobility was defined as the lack of motion of the whole body, except for small movements necessary to keep the rat's head above the water.
Histological assessments
On Day 28 after surgery, cerebral embolism or sham rats were perfused via the heart with 4% paraformaldehyde in 0.1 M phosphate buffer. Their brains were quickly removed and immersed in 30% sucrose in 0.1 M phosphate buffer. The brains were then cut into 5-mm-thick coronal slabs, which were subsequently embedded in Neg50 (Richard-Allan Scientific, Kalamazoo, MI, USA) and cut into 10-μm sections by using a cryostat. For determination of the viable area, coronal sections were stained with hematoxylin and eosin. The viable area in the ipsilateral hemisphere was measured as a percentage of that of the contralateral hemisphere by using NIH Image ver. 1.63.
For immunostaining, sections were incubated overnight with the desired primary antibody at 4 °C, and then with the corresponding secondary antibody for 1 h. In the case of double immunofluorescence staining, after a wash, the same sections were incubated overnight with another primary antibody at 4 °C. Subsequently, they were incubated with the corresponding secondary antibody for 1 h. Omission of primary antibodies served as a negative control. No immunostaining was detected in this group.
The following primary antibodies were used: rat monoclonal anti-GFP (Nacalai Tesque, Kyoto, Japan), mouse monoclonal anti-NeuN (Chemicon), rabbit polyclonal anti-GFAP (DAKO), mouse monoclonal anti-RIP (Chemicon) and rabbit polyclonal anti-musashi-1 (Chemicon) antibodies. The secondary antibodies used were as follows: fluorescein isothiocyanate-conjugated donkey anti-rat IgG (Jackson Immunoresearch), Cy3-conjugated goat anti-mouse IgG (Amersham, Buckinghamshire, UK) and Cy3-conjugated donkey anti-rabbit IgG (Jackson Immunoresearch). Fluorescence was detected by using Olympus fluorescence microscopy (BX-52; Olympus) or with a KEYENCE BZ-8000 (KEYENCE).
Immunoblotting
On Day 28 after surgery, cerebral embolism or sham rats were killed by decapitation. The whole ipsilateral hemisphere was homogenized in ice-cold buffer containing 320 mM sucrose, 20 mM β-glycerophosphate, 20 mM sodium diphosphate, 0.2 mM sodium orthovanadate, 0.1 mM phenylmethyl sulfonyl fluoride, 5 μg ml−1 antipain, 5 μg ml−1 aprotinin and 5 μg ml−1 leupeptin at 4 °C. To determine the level of BDNF proteins, the whole ipsilateral hemisphere was homogenized in ice-cold buffer containing 10% sucrose, 1 mM EDTA, phosphatase inhibitor cocktail (Roche) and protease inhibitor cocktail (Roche, Mannheim, Germany) in 20 mM Tris-HCl (pH 7.4), and then centrifuged at 12 000g for 12 min at 4 °C; and finally the supernatant was collected. Protein concentration was determined by the method of Lowry.35 Western blotting was performed according to standard protocols. The following primary antibodies were used: rabbit polyclonal antibody against BDNF (Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA), phospho-CREB (Cell Signaling Technology Inc., Danvers, MA, USA), CREB (Cell Signaling Technology), phospho-ERK1/2 (Cell Signaling Technology), ERK1/2 (Cell Signaling Technology), phospho-Akt (Cell Signaling Technology), Akt (Cell Signaling Technology) and TrkB (BD Biosciences). Subsequently, the membrane was washed and incubated with secondary antibody. Bound antibody was detected by use of the enhanced chemiluminescence method (Amersham). Quantification was carried out by performing computerized densitometry with an image analyzer (ATTO Co., Tokyo, Japan). To minimize between blot variability, we applied an aliquot of pooled ‘control’ homogenates, which was obtained from naïve control rats, to one lane of every gel and calculated the immunoblotting of samples relative to this standard.
Statistical analysis
The results were expressed as the means±standard error of the mean (s.e.m.). Differences between two groups were evaluated statistically by the unpaired Student's t-test. Statistical comparison among multiple groups was evaluated by analysis of variance, followed by Scheffe's test as a post hoc test or repeated measures analysis of variance. P-values of less than 0.05 were considered significant.
Results
Isolation of NPCs
Figure 1 shows that cells in the neurospheres expressed the neural progenitor markers nestin (Figure 1b) and musashi-1 (Figure 1c) on Day 6 when cultured in vitro. After triggering in vitro differentiation by withdrawal of the growth factors, we confirmed the tripotent nature of the NPCs by their ability to generate differentiated cells expressing neuronal (MAP2; Figure 1e), astrocytic (GFAP; Figure 1f) and oligodendrocytic (RIP; Figure 1g) markers.
Characterization of neural progenitor cells and experimental protocol of this study. Triple staining was carried outwith 4′,6-diamidino-2-phenylindole (DAPI), (a) and for nestin (b) and musashi-1 (c) was merged (d), and indicated that cells in neurospheres, which were prepared from gestational Day 14 fetal rats, expressed the neural progenitor cell markers nestin and musashi-1 on Day 6 when cultured in vitro. The cells in the neurospheres differentiated after the withdrawal of growth factors from the medium into MAP2- (e), glial fibrillary acidic protein (GFAP)- (f) and oligodendrocytes (clone RIP)-positive cells (g). Scale bars represent 50 μm (a–d) and 10 μm (e–g). Experimental protocol in this study was depicted (h). Abbreviations: mNSS, modified Neurological Severity Scores; SPT, sucrose preference test; FST, forced-swimming test; OFT, open-field test; WB: western immunoblotting; and IHC, immunohistochemistry.
Effect of injection of NPCs on body weight and neurological deficits
The time courses of the change in body weight of the vehicle- and NPC-injected ischemic rats are shown in Figure 2a. The body weight of both groups of ischemic rats transiently decreased after the surgery, and there was no significant difference in body weight between the two groups (F(1, 32)=1.72, P=0.20).
Time courses of changes in body weight, neurological deficits and modified Neurological Severity Score (mNSS)- of vehicle- and neural progenitor cell (NPC)-injected ischemic rats. The arrow indicates the time point when NPCs or vehicle was injected. There was no significant difference in body weight between NPC- (open circles) and vehicle-treated (closed circles) groups (a). The score of each neurological deficit was rated from 3 to 0 (from very severe to little or none). There was no significant improvement in the NPC-injected ischemic (closed circles) rats compared with the vehicle-injected ischemic (open circles) ones (b). Determination of mNSS, which is based on a series of behavioral tests, including motor, sensory, reflex and balance tests, was made. There was a significant reduction in the score of NPC-injected ischemic rats (open circles) when these rats were compared with the vehicle-injected ones (closed circles) after the embolism (c). All results are presented as the mean±s.e.m. (n=17 rats per group). #Statistically significant difference from vehicle-injected ischemic rats (P<0.05).
The time courses of the change in neurological deficits of vehicle-treated and NPC-injected ischemic rats are shown in Figure 2b. The neurological deficits of ischemic rats gradually decreased after surgery for microsphere embolism. No significant improvement in the NPC-injected ischemic rats was seen when these rats were compared with the vehicle-treated ones (F(1, 32)=0.58, P=0.45) (Figure 2b).
Effect of injection of NPCs on mNSS
We next examined the time courses of the change in mNSS of the vehicle-treated and NPC-injected ischemic rats (Figure 2c). The score of the vehicle-injected ischemic rats was 13.1±0.2 points on Day 1, dropped to 9.5±0.2 points on Day 7 after microsphere embolism and remained at roughly that value up to Day 28. There were significant differences in the mNSS by group (F(1,32)=161.24, P<0.0001) and by days (F(4,32)=913.29, P<0.0001). The group-by-day interaction was significant. There was a significant improvement in the score of NPC-injected ischemic rats when these rats were compared with the vehicle-injected ones after microsphere embolism (Figure 2c). Sham-operated rats did not reveal any neurological deficits and had no mNSS throughout the examination (data not shown).
Effect of injection of NPCs on the SPT
The time courses of the change in sucrose preference of the vehicle- and NPC-injected ischemic rats are shown in Figure 3a. The percentage of the sucrose preference of vehicle-injected ischemic rats was 71.8±2.9% on Day 7 after the embolism. Then, this percentage remained at about the same value up to Day 28 after the embolism (Figure 3a). The percentage for the sucrose preference score of NPC-injected ischemic rats was 67.3±2.7% on Day 7 and then it gradually increased (Figure 3a). There was a significant difference in the percentage of the sucrose preference by group (F(1,32)=36.54, P<0.0001) and by days (F(4,32)=67.04, P<0.0001). There was a significant improvement in the percentage of sucrose preference of NPC-injected ischemic rats when these rats were compared with the vehicle-injected ones. The sham-operated rats did not reveal any reduction in the sucrose preference throughout the examination (data not shown). There was no significant difference in total consumption between vehicle- and NPC-injected ischemic rats throughout the experiment (Figure 3b).
Effect of injection of neural progenitor cells (NPCs) on sucrose preference, immobility time in the forced-swimming test and locomotor activity. A battery of the sucrose preference test was conducted before microsphere embolism and on Days 7, 14, 21 and 28 after the embolism (a and b). Time courses of changes in sucrose preference of vehicle- (closed circles) and NPC-injected (open circles) ischemic rats are shown (a). The arrows indicate the time point when NPC or vehicle was injected. There was significant improvement in the percentage of the sucrose preference of the NPC-injected ischemic rats when these rats were compared with the vehicle-injected ischemic ones on Days 14, 21 and 28 after the embolism. There was no significant difference in total consumption between vehicle- and NPC-injected ischemic rats throughout the experiment (b). All results in the sucrose preference test are presented as the mean±s.e.m. (n=17 rats per group). The forced-swimming test was performed on Day 28 after the embolism (c). #Statistically significant difference from vehicle-injected ischemic rats (P<0.05). There was a significant increase in the immobility of the vehicle-injected ischemic rats when these rats were compared with the sham-operated ones (c). The immobility time was not increased in NPC-injected ischemic rats (c). The open-field test was performed on Day 28 after the embolism (d). The total locomotor activity was not significantly different among sham-operated, vehicle-injected and NPC-injected ischemic rats (d). All results in the forced-swimming test and the open-field test are presented as the mean±s.e.m. (n=14 rats per group). *Statistically significant difference from sham-operated rats (P<0.05). #Statistically significant difference from vehicle-injected ischemic rats (P<0.05).
Effect of injection of NPCs on the FST
To determine the effect of injection of NPCs on depression-like behavior, we next conducted the FST on Day 28 after microsphere embolism. The immobility time in the FST for the sham-operated rats and the vehicle- and NPC-injected ischemic rats is shown in Figure 3c. There was a significant difference in the mobility time among the three groups (F(2,39)=7.27, P<0.01). The immobility time of vehicle-injected ischemic rats was significantly increased, and this increased time was attenuated by the NPC injection (Figure 3c).
Effect of injection of NPCs on the open-field test
We further examined the effect of NPCs on the locomotor activity of the sham-operated rats and the vehicle- and NPC-injected ischemic ones on Day 28 after the microsphere embolism or sham surgery. As shown in Figure 3d, there was no significant difference in the locomotor activity among these three groups.
Effect of injection of NPCs on the viable area and phenotype of injected NPCs
We examined the effect of injection of NPCs on the viable area of the ipsilateral hemisphere of vehicle-treated (Figures 4a and d) and NPC-injected (Figures 4b and e) ischemic rats on Day 28 after the microsphere embolism. The marked degeneration seen in the vehicle-injected ischemic rats was not attenuated by the injected NPCs (Figures 4c and f). The NPCs, which were identified as GFP-positive cells, were found in the peri-infarct region at 21 days after the injection. Although the injected NPCs (GFP-positive cells) were not positive for RIP (data not shown) after in vivo cerebral ischemia, a few injected NPCs expressed NeuN (Figure 4k) and GFAP (Figure 4l) in the peri-infarct areas at 21 days after the injection of NPCs. Most injected NPCs were still positive for musashi-1 around the infarct areas (Figure 4m).
Histological analysis of the neural progenitor cell (NPC)-injected brain after the embolism. Effect of injection of NPCs on the viable areas after the embolism. On Day 28 after microsphere embolism-induced cerebral ischemia (ME), coronal sections were stained with hematoxylin and eosin. Photographs of hematoxylin- and eosin-stained sections are shown for vehicle-injected (a and d) and NPC-injected (b and e) ischemic rats. Viable areas were estimated by measuring hematoxylin- and eosin-stained sections (c and f) that corresponded to coronal coordinates of bregma from 0.48 to −0.30 mm (striatal region: a–c) and from −3.80 to −4.52 mm (hippocampal region: d–f). All results are presented as the mean percentage of the contralateral hemisphere±s.e.m. (n=8–9 rats per group). There was no significant attenuation of tissue degeneration in the NPC-injected ischemic rats compared with that in the vehicle-injected ischemic rats in both regions (c and f). Green-fluorescent protein (GFP)-positive NPCs were found in the peri-infarct areas (h and j) on Day 28 after the embolism (striatal region: g and h; hippocampal region: i and j). The images (white square) in ‘g’ and ‘i’ are enlarged in ‘h’ and ‘j’, respectively. To determine the effect of injection of NPCs on the phenotype of injected cells, double immunostaining in the peri-infarct areas was conducted on Day 28 after the embolism. Some GFP-positive injected NPCs expressed mature neuronal marker NeuN (k) and astrocyte marker GFAP (l). Most GFP-positive NPCs expressed NPC marker musashi-1 (m). Scale bars represent 1 mm (g and i), 50 μm (h and j) and 10 μm (k–m).
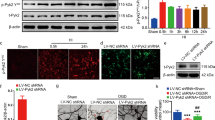
Effect of injection of NPCs on the levels of BDNF, phosphorylated CREB and TrkB
We examined the effect of the NPC injection on the level of BDNF protein (Figure 5a) and phospho-CREB (Figure 5b) in the ipsilateral hemisphere of sham-operated rats and vehicle- or NPCs-injected ischemic rats on Day 28 after microsphere embolism. There were significant differences in the level of BDNF and phospho-CREB proteins among the three groups (BDNF: F(2,24)=37.71, P<0.0001; phospho-CREB: F(2,24)=7.94, P<0.01). The level of BDNF proteins was decreased after the embolism compared with that in the sham-operated rats (Figure 5a). The injection of NPCs significantly lessened this decrease in BDNF level in the ischemic rats (Figure 5a). Phosphorylation of CREB was also decreased on Day 28, and the NPC injection inhibited this decrease without causing any change in the level of CREB (Figure 5b). Furthermore, there was a significant difference in the level of the BDNF receptor TrkB protein among the three groups (F(2, 14)=26.99, P<0.0001). The decreased level of TrkB protein in the ipsilateral hemisphere of the vehicle-injected ischemic rats was attenuated by the injection of the NPCs (Figure 5c).
Effect of neural progenitor cell (NPC) injection on the levels of brain-derived neurotrophic factor (BDNF), phosphorylated CREB, TrkB, phosphorylated ERK and phosphorylated AKT on Day 28 after the embolism. Samples obtained from sham-operated (sham), vehicle-injected ischemic (vehicle) and NPC-injected (NPC) ischemic rats (ME) were solubilized and separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE). Bands corresponding to BDNF (a), phospho-CREB (b), and TrkB (c), phosphorylated ERK (d) and phosphorylated Akt (e) were scanned, and scanned bands were normalized by actin (a and c), total CREB (b), total ERK (d) or total AKT (e) on the same blot. All results are presented as mean percentages of non-operated naïve rats±s.e.m. (BDNF and phospho-CREB: n=9 rats per group; TrkB: n=5–6 rats per group; and phospho-ERK and -AKT: n=6 rats per group). *Statistically significant difference from sham-operated rats (P<0.05). #Statistically significant difference from vehicle-injected ischemic rats (P<0.05).
Effect of NPC injection on the level of phosphorylated ERK and Akt
We next examined the effect of the NPC injection on the phosphorylation of ERK and Akt, which are located upstream of CREB. There were significant differences in the levels of phospho-ERK and phospho-Akt among the three groups (phospho-ERK: F(2,15)=14.74, P<0.001; phospho-Akt: F(2,15)=7.32, P<0.01). The microsphere embolism decreased the level of phospho-ERK on Day 28 (Figure 5d), and this decrease in the phosphorylation of ERK was attenuated by the injection of NPCs without changing the total level of ERK (Figure 5d). Although the level of phosphorylated Akt was significantly decreased after the embolism compared with that for the sham-operated rats, no statistical difference was detected in Akt phosphorylation between vehicle- and NPC-injected ischemic rats (Figure 5e).
Discussion
In this study, NPCs proliferated and formed neurospheres that expressed NPC markers nestin and musashi-1. The cells in the neurospheres differentiated by withdrawal of the growth factors in the medium into neurons, astrocytes and oligodendrocytes in vitro. These results indicate the ability of NPCs isolated from fetal GFP transgenic rats to express the properties of self-renewal and multipotency.
As a transient inflammatory response occurs around the injured region during the acute stage, this time period is not likely to be suitable for therapeutic transplantation of cells.36 We have previously confirmed that the level of an inflammatory cytokine IL-6 was comparable to that of sham-operated control rats and that the body weight of embolized rats was transiently decreased and then returned to baseline on Day 7 after surgery.20, 37 In addition, the infarction had almost completely developed in the ipsilateral hemisphere on Day 7 after surgery. Therefore, we injected NPCs on Day 7 after microsphere embolism in this study, to avoid inappropriate environments for therapeutic NPC injection after cerebral ischemia. We showed that there was no significant difference in the time course of the change in the neurological deficits, regardless of intravenous injection or not of NPCs. As described previously, the neurological deficits seen in microsphere embolism-induced cerebral ischemia in rats can only be useful as stroke-like symptoms to assess the severity of ischemic models during the acute period after surgery.19 Thus, these results imply that the effect of the NPCs on mNSS, sucrose preference and the immobility time in the FST evaluated in this study was not due to alterations of neurological deficits during the acute period after surgery.
In this study, there was a significant group-by-day interaction in the mNSS. Therefore, it was suggested that the intravenous injection of NPCs on Day 7 after the induction of cerebral ischemia improved the results in a series of motor sensory, reflex and balance tests for the mNSS, compared with those for the vehicle-injected ischemic rats. This effect of NPCs is consistent with the finding that intravenous administration of bone marrow stromal cells after transient focal cerebral ischemia reduces functional deficits.38, 39 Accumulating evidence indicates that the recovery of neurological function after cerebral ischemia is mediated by the production of some trophic factors, vascular remodeling and axonal regeneration,40, 41 although it is still not clear why the intravenous injection of NPCs was effective in reducing the mNSS.
We performed the SPT and FST as measures of PSD-like behavior. In this study, the sucrose preference of the ischemic rats decreased at 7 days after surgery and this decrease was sustained at least until Day 28. This result is consistent with the decreased sucrose preference in middle cerebral artery occlusion models with chronic mild stress.42 As a decrease in sucrose consumption indicates a state of anhedonia, a core symptom of depression, which can be evaluated effectively in rodents,43 our results can be used to estimate a mood disturbance of rats after microsphere embolism. We furthermore showed that the immobility time in the FST was prolonged in the vehicle-treated ischemic rats. These results suggest that microsphere embolism-induced cerebral ischemia affected behaviors associated with depression. On the basis of these results, our present study is the first to provide evidence that the intravenous injection of NPCs can improve PSD-like behaviors.
Intravenously injected NPCs homed into the ischemic hemisphere, but not into the contralateral hemisphere, on Day 28 after the embolism. This result raises the possibility that the injected NPCs integrated into the damaged area and might provide growth factors because most of these cells did not undergo differentiation. It was earlier shown that systemically injected endothelial progenitor cells homed into the ischemic regions as early as 24 h after transient middle cerebral artery occlusion.44 In this study, some GFP-positive NPCs became localized in the hippocampus and hypothalamus, which were consistent with lesion sites after the embolism. In addition, the administration of bone marrow stromal cells to rats with middle cerebral artery occlusion enhances axonal plasticity, which is highly and significantly correlated with progressive functional recovery enhanced by these bone marrow stromal cells, whereas no significant difference is found on the ischemic lesion between control and bone marrow stromal cell treatment group.45 Interestingly, we demonstrated that the intravenous injection of NPCs on Day 7 after the embolism improved PSD-like behaviors without having any restorative effect on the damaged areas on Day 28 after the embolism. Although some injected GFP-positive NPCs expressed NeuN and GFAP, most of the injected NPCs did not undergo differentiation in this study. These results imply that injected NPCs may exert several types of cellular responses in the peri-infarct areas. Therefore, these injected NPCs were maintained in an undifferentiated condition morphologically and might not only have functioned as cells producing neurotrophic factors, but also have protected host viable cells and/or achieve an exact reconnection of neural networks. Although the primary mechanism was presently not fully elucidated, the altered expression of trophic factors as well as biochemical responses induced by NPCs may have contributed to the antidepression-like effects of these cells after the embolism.
Among neurotrophic factors, BDNF plays an important role in cellular proliferation and differentiation and contributes to the maintenance of neuronal function and structural integrity of neurons in the CNS. In addition, depressed suicide patients show a decreased level of BDNF in their brain tissue.21 Therefore, we focused on a possible change in the level of BDNF as underlying the PSD-like behaviors. Our results suggest that a properly maintained level of BDNF achieved by the injection of the NPCs was involved in the improvement of PSD-like behaviors after cerebral ischemia. This effect might be associated with the actions of chemical antidepressants in the FST,46 as well as in agreement with the effect of centrally administered BDNF, including infusion of it into the midbrain,47 hippocampus22 and lateral ventricles.48 Furthermore, the anti-depressant-like effects of BDNF in the learned helplessness paradigms are blocked by co-administration of K252a, a broad-spectrum tyrosine kinase inhibitor.22 The effects of antidepressants on the behavioral responses are inhibited in conditional BDNF knockout mice and in transgenic mice expressing a dominant-negative form of the BDNF receptor TrkB.49, 50 These findings raise the possibility of an important role of altered BDNF and/or BDNF receptor TrkB-mediated signaling pathway in PSD-like behaviors.
It was earlier shown that administration of BDNF increases the level of BDNF, and enhances the phosphorylation of ERK as well as that of CREB, which have been implicated in events downstream of BDNF-TrkB signaling.51, 52 BDNF-ERK-CREB signaling has been implicated in antidepressant effects on behavior.51 In this regard, ERK is likely to be required for the effects of BDNF infusion on depression-like behaviors22 or for the antidepressant action.53 Furthermore, CREB expression and its phosphorylation are sufficient for an antidepressant-like effect on behavioral responses.54 These results suggest that BDNF-TrkB-ERK-CREB signaling could be required for an antidepressant response.49, 50 Also, the activation of Akt via TrkB has been implicated in the BDNF-induced survival of neurons.55 Interestingly, we demonstrated that injection of NPCs did not affect the decreased phosphorylation of Akt on Day 28 after the embolism. Although we cannot fully rule out the possibility that Akt phosphorylation might be increased at some different time point by NPC injection and related to antidepressant response, our results suggest that the effect of NPCs on PSD-like behavioral responses may be associated with improvement in the BDNF-ERK-CREB signaling pathway in the viable areas.
In conclusion, the intravenous injection of NPCs improved PSD-like behaviors without having any restorative effect on the degeneration of the brain tissue. We demonstrated that restoring the BDNF-ERK-CREB signaling pathway by NPCs was paralleled with improvement of PSD-like behaviors. Although future studies will be required to explore the mechanisms concerning the source of increased BDNF, this study provides evidence of the therapeutic potential of NPCs for improvement of PSD-like behaviors after cerebral ischemia.
References
Stroke—1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO Task Force on Stroke and other Cerebrovascular Disorders. Stroke 1989; 20: 1407–1431.
Hackett ML, Yapa C, Parag V, Anderson CS . Frequency of depression after stroke: a systematic review of observational studies. Stroke 2005; 36: 1330–1340.
Burvill PW, Johnson GA, Jamrozik KD, Anderson CS, Stewart-Wynne EG, Chakera TM . Prevalence of depression after stroke: the Perth Community Stroke Study. Br J Psychiatry 1995; 166: 320–327.
Austin MP, Mitchell P, Goodwin GM . Cognitive deficits in depression: possible implications for functional neuropathology. Br J Psychiatry 2001; 178: 200–206.
Schulz R, Beach SR, Ives DG, Martire LM, Ariyo AA, Kop WJ . Association between depression and mortality in older adults: the Cardiovascular Health Study. Arch Intern Med 2000; 160: 1761–1768.
Schwab-Malek S, Vatankhah B, Bogdahn U, Horn M, Audebert HJ . Depressive symptoms and quality of life after thrombolysis in stroke: the TEMPiS study. J Neurol 2010; 257: 1848–1854.
Dranovsky A, Hen R . Hippocampal neurogenesis: regulation by stress and antidepressants. Biol Psychiatry 2006; 59: 1136–1143.
Thomas RM, Hotsenpiller G, Peterson DA . Acute psychosocial stress reduces cell survival in adult hippocampal neurogenesis without altering proliferation. J Neurosci 2007; 27: 2734–2743.
Malberg JE, Schechter LE . Increasing hippocampal neurogenesis: a novel mechanism for antidepressant drugs. Curr Pharm Des 2005; 11: 145–155.
David DJ, Samuels BA, Rainer Q, Wang JW, Marsteller D, Mendez I et al. Neurogenesis-dependent and -independent effects of fluoxetine in an animal model of anxiety/depression. Neuron 2009; 62: 479–493.
Jin K, Minami M, Lan JQ, Mao XO, Batteur S, Simon RP et al. Neurogenesis in dentate subgranular zone and rostral subventricular zone after focal cerebral ischemia in the rat. Proc Natl Acad Sci USA 2001; 98: 4710–4715.
Kawai T, Takagi N, Miyake-Takagi K, Okuyama N, Mochizuki N, Takeo S . Characterization of BrdU-positive neurons induced by transient global ischemia in adult hippocampus. J Cereb Blood Flow Metab 2004; 24: 548–555.
Zhang RL, Zhang ZG, Zhang L, Chopp M . Proliferation and differentiation of progenitor cells in the cortex and the subventricular zone in the adult rat after focal cerebral ischemia. Neuroscience 2001; 105: 33–41.
Arvidsson A, Collin T, Kirik D, Kokaia Z, Lindvall O . Neuronal replacement from endogenous precursors in the adult brain after stroke. Nat Med 2002; 8: 963–970.
Goings GE, Sahni V, Szele FG . Migration patterns of subventricular zone cells in adult mice change after cerebral cortex injury. Brain Res 2004; 996: 213–226.
Parent JM, Vexler ZS, Gong C, Derugin N, Ferriero DM . Rat forebrain neurogenesis and striatal neuron replacement after focal stroke. Ann Neurol 2002; 52: 802–813.
Bacigaluppi M, Pluchino S, Martino G, Kilic E, Hermann DM . Neural stem/precursor cells for the treatment of ischemic stroke. J Neurol Sci 2008; 265: 73–77.
Locatelli F, Bersano A, Ballabio E, Lanfranconi S, Papadimitriou D, Strazzer S et al. Stem cell therapy in stroke. Cell Mol Life Sci 2009; 66: 757–772.
Mochizuki N, Takagi N, Kurokawa K, Onozato C, Moriyama Y, Tanonaka K et al. Injection of neural progenitor cells improved learning and memory dysfunction after cerebral ischemia. Exp Neurol 2008; 211: 194–202.
Mochizuki N, Takagi N, Onozato C, Moriyama Y, Takeo S, Tanonaka K . Delayed injection of neural progenitor cells improved spatial learning dysfunction after cerebral ischemia. Biochem Biophys Res Commun 2008; 368: 151–156.
Dwivedi Y, Rizavi HS, Conley RR, Roberts RC, Tamminga CA, Pandey GN . Altered gene expression of brain-derived neurotrophic factor and receptor tyrosine kinase B in postmortem brain of suicide subjects. Arch Gen Psychiatry 2003; 60: 804–815.
Shirayama Y, Chen AC, Nakagawa S, Russell DS, Duman RS . Brain-derived neurotrophic factor produces antidepressant effects in behavioral models of depression. J Neurosci 2002; 22: 3251–3261.
Smith MA, Makino S, Kvetnansky R, Post RM . Stress and glucocorticoids affect the expression of brain-derived neurotrophic factor and neurotrophin-3 mRNAs in the hippocampus. J Neurosci 1995; 15: 1768–1777.
Castren E, Voikar V, Rantamaki T . Role of neurotrophic factors in depression. Curr Opin Pharmacol 2007; 7: 18–21.
Duman RS, Monteggia LM . A neurotrophic model for stress-related mood disorders. Biol Psychiatry 2006; 59: 1116–1127.
Schmidt HD, Duman RS . The role of neurotrophic factors in adult hippocampal neurogenesis, antidepressant treatments and animal models of depressive-like behavior. Behav Pharmacol 2007; 18: 391–418.
Chiasson BJ, Tropepe V, Morshead CM, van der Kooy D . Adult mammalian forebrain ependymal and subependymal cells demonstrate proliferative potential, but only subependymal cells have neural stem cell characteristics. J Neurosci 1999; 19: 4462–4471.
Palmer TD, Markakis EA, Willhoite AR, Safar F, Gage FH . Fibroblast growth factor-2 activates a latent neurogenic program in neural stem cells from diverse regions of the adult CNS. J Neurosci 1999; 19: 8487–8497.
Hakamata Y, Tahara K, Uchida H, Sakuma Y, Nakamura M, Kume A et al. Green fluorescent protein-transgenic rat: a tool for organ transplantation research. Biochem Biophys Res Commun 2001; 286: 779–785.
Miyake K, Takeo S, Kaijihara H . Sustained decrease in brain regional blood flow after microsphere embolism in rats. Stroke 1993; 24: 415–420.
Furlow Jr TW, Bass NH . Arachidonate-induced cerebrovascular occlusion in the rat. The role of platelets and aspirin in stroke. Neurology 1976; 26: 297–304.
McGraw CP . Experimental cerebral infarction effects of pentobarbital in Mongolian gerbils. Arch Neurol 1977; 34: 334–336.
Chen Y, Constantini S, Trembovler V, Weinstock M, Shohami E . An experimental model of closed head injury in mice: pathophysiology, histopathology, and cognitive deficits. J Neurotrauma 1996; 13: 557–568.
Wallace TL, Stellitano KE, Neve RL, Duman RS . Effects of cyclic adenosine monophosphate response element binding protein overexpression in the basolateral amygdala on behavioral models of depression and anxiety. Biol Psychiatry 2004; 56: 151–160.
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ . Protein measurement with the Folin phenol reagent. J Biol Chem 1951; 193: 265–275.
Okano H, Kaneko S, Okada S, Iwanami A, Nakamura M, Toyama Y . Regeneration-based therapies for spinal cord injuries. Neurochem Int 2007; 51: 68–73.
Mochizuki N, Moriyama Y, Takagi N, Takeo S, Tanonaka K . Intravenous injection of neural progenitor cells improves cerebral ischemia-induced learning dysfunction. Biol Pharm Bull 2011; 34: 260–265.
Chen J, Li Y, Wang L, Zhang Z, Lu D, Lu M et al. Therapeutic benefit of intravenous administration of bone marrow stromal cells after cerebral ischemia in rats. Stroke 2001; 32: 1005–1011.
Zacharek A, Shehadah A, Chen J, Cui X, Roberts C, Lu M et al. Comparison of bone marrow stromal cells derived from stroke and normal rats for stroke treatment. Stroke 2010; 41: 524–530.
Zacharek A, Shehadah A, Chen J, Cui X, Roberts C, Lu M et al. Comparison of bone marrow stromal cells derived from stroke and normal rats for stroke treatment. Stroke 2010; 41: 524–530.
Zhang J, Li Y, Chen J, Yang M, Katakowski M, Lu M et al. Expression of insulin-like growth factor 1 and receptor in ischemic rats treated with human marrow stromal cells. Brain Res 2004; 1030: 19–27.
Guo YJ, Zhang ZJ, Wang SH, Sui YX, Sun Y . Notch1 signaling, hippocampal neurogenesis and behavioral responses to chronic unpredicted mild stress in adult ischemic rats. Prog Neuropsychopharmacol Biol Psychiatry 2009; 33: 688–694.
Brenes Saenz JC, Villagra OR, Fornaguera Trias J . Factor analysis of forced swimming test, sucrose preference test and open field test on enriched, social and isolated reared rats. Behav Brain Res 2006; 169: 57–65.
Fan Y, Shen F, Frenzel T, Zhu W, Ye J, Liu J et al. Endothelial progenitor cell transplantation improves long-term stroke outcome in mice. Ann Neurol 2010; 67: 488–497.
Liu Z, Li Y, Zhang ZG, Cui X, Cui Y, Lu M et al. Bone marrow stromal cells enhance inter- and intracortical axonal connections after ischemic stroke in adult rats. J Cereb Blood Flow Metab 2010; 30: 1288–1295.
Cryan JF, Page ME, Lucki I . Differential behavioral effects of the antidepressants reboxetine, fluoxetine, and moclobemide in a modified forced swim test following chronic treatment. Psychopharmacology (Berl) 2005; 182: 335–344.
Siuciak JA, Lewis DR, Wiegand SJ, Lindsay RM . Antidepressant-like effect of brain-derived neurotrophic factor (BDNF). Pharmacol Biochem Behav 1997; 56: 131–137.
Hoshaw BA, Malberg JE, Lucki I . Central administration of IGF-I and BDNF leads to long-lasting antidepressant-like effects. Brain Res 2005; 1037: 204–208.
Monteggia LM, Barrot M, Powell CM, Berton O, Galanis V, Gemelli T et al. Essential role of brain-derived neurotrophic factor in adult hippocampal function. Proc Natl Acad Sci USA 2004; 101: 10827–10832.
Sairanen M, Lucas G, Ernfors P, Castren M, Castren E . Brain-derived neurotrophic factor and antidepressant drugs have different but coordinated effects on neuronal turnover, proliferation, and survival in the adult dentate gyrus. J Neurosci 2005; 25: 1089–1094.
Schmidt HD, Banasr M, Duman RS . Future antidepressant targets: neurotrophic factors and related signaling cascades. Drug Discov Today Ther Strateg 2008; 5: 151–156.
Carlezon Jr WA, Duman RS, Nestler EJ . The many faces of CREB. Trends Neurosci 2005; 28: 436–445.
Gourley SL, Wu FJ, Kiraly DD, Ploski JE, Kedves AT, Duman RS et al. Regionally specific regulation of ERK MAP kinase in a model of antidepressant-sensitive chronic depression. Biol Psychiatry 2008; 63: 353–359.
Nakagawa S, Kim JE, Lee R, Chen J, Fujioka T, Malberg J et al. Localization of phosphorylated cAMP response element-binding protein in immature neurons of adult hippocampus. J Neurosci 2002; 22: 9868–9876.
Reichardt LF . Neurotrophin-regulated signalling pathways. Philos Trans R Soc Lond Ser B 2006; 361: 1545–1564.
Acknowledgements
We thank Chisa Itokawa, Sachiko Tsuru, Kanae Hashimura and Shoko Mizukami for their contribution to the research. This research was supported in part by the Promotion and Mutual Aid Corporation for Private Schools of Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Moriyama, Y., Takagi, N. & Tanonaka, K. Intravenous injection of neural progenitor cells improved depression-like behavior after cerebral ischemia. Transl Psychiatry 1, e29 (2011). https://doi.org/10.1038/tp.2011.32
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/tp.2011.32
Keywords
This article is cited by
-
Possible Involvement of PI3-K/Akt-Dependent GSK-3β Signaling in Proliferation of Neural Progenitor Cells After Hypoxic Exposure
Molecular Neurobiology (2019)
-
Involvement of GSK-3β Phosphorylation Through PI3-K/Akt in Cerebral Ischemia-Induced Neurogenesis in Rats
Molecular Neurobiology (2017)
-
Effects of acute versus post-acute systemic delivery of neural progenitor cells on neurological recovery and brain remodeling after focal cerebral ischemia in mice
Cell Death & Disease (2014)