Abstract
Menthol is thought to stimulate lacrimation via activation of cold-sensitive primary afferent neurons in the cornea. We evaluated a warm compress containing menthol as a potential treatment for dry eye by examining its effects on the tear film in healthy subjects (n = 20) and dry eye patients (n = 35). Disposable eyelid-warming steamers that either did (MH) or did not (HO) contain menthol were applied to one eye of each subject either once only for 10 min or repeatedly over 2 weeks. Single application of MH significantly increased tear meniscus volume (P = 8.6 × 10−5, P = 1.3 × 10−5) and tear film breakup time (P = 0.006, P = 0.002) as well as improved meibum condition in healthy subjects and dry eye patients, respectively. Repeated application of MH significantly increased tear meniscus volume (P = 0.004, P = 1.7 × 10−4) and tear film breakup time (P = 0.037, P = 0.010) in healthy subjects and dry eye patients, respectively. Repeated application of MH thus induced persistent increases in tear fluid volume and tear film stability in dry eye patients, suggesting that repeated use of a warm compress containing menthol is a potential novel treatment for dry eye disease.
Similar content being viewed by others
Introduction
Menthol is a volatile water-clear organic compound with the structure of a cyclic monoterpene that is incorporated into various consumer products including toothpaste, gum, and medicines such as proprietary eyedrops. It has also been suggested as a possible treatment for dry eye1,2,3,4. Menthol binds to transient receptor potential cation channel subfamily M member 8 (TRPM8)1,2,3,5,6,7 and thereby stimulates lacrimation via activation of cold-sensitive primary afferent neurons in the cornea. The possible effects of menthol on tear volume and tear film stability in humans have remained unknown, however.
Dry eye is characterized by qualitative or quantitative abnormalities of the tear film and is estimated to affect and have a negative impact on the quality of life of ~4.88 million people in the United States8,9,10. If left untreated, dry eye can result in damage to the ocular surface and impair vision. A reduced volume of tear fluid gives rise to aqueous-deficient dry eye (ADDE), whereas impaired tear film stability underlies evaporative dry eye (EDE)11. ADDE is further categorized as Sjӧgren syndrome–type ADDE (SS-ADDE) or non-Sjӧgren ADDE (non-SS-ADDE). The common etiology of SS-ADDE and non-SS-ADDE is dysfunction or hypofunction of lacrimal glands and a consequent deficiency of the aqueous layer of the tear film11. Meibomian gland dysfunction (MGD), a chronic abnormality of meibomian glands characterized by terminal duct obstruction or qualitative or quantitative changes in glandular secretion12, is one of the most important underlying causes of EDE13. Meibomian glands produce meibum, the lipid components of which give rise to the surface lipid layer of the tear film. MGD can thus result in changes to the tear film, symptoms of eye irritation, clinically apparent inflammation, and ocular surface disease12.
Given the difference in the pathophysiologies of ADDE and EDE, the treatment strategies for these conditions are also different. ADDE is managed with punctal plugs and eyedrops such as those containing cyclosporine, artificial tears, hyaluronate, diquafosol sodium chloride, or rebamipide, with the aim of increasing the volume of tear fluid or tear film stability14. The application of a warm compress to the eyelids is a standard treatment for obstructive MGD15. Previous studies have assessed the effects of various warming devices—including infrared devices16,17, a disposable eyelid-warming device18, warm moist air devices19,20,21, an Orgahexa fiber eye mask22, Blephasteam23, MGDRx EyeBag24,25, Azuki-no-chikara26, and LipiFlow27—on tear function and the ocular surface.
The purpose of the present study was to investigate the effects of a disposable eyelid-warming steamer containing menthol (MH) on tear film function, meibomian glands, and the ocular surface in individuals with dry eye. We first examined the effects of a single application of MH and of a similar device without menthol (HO) in healthy subjects and dry eye patients. We then examined the effects of repeated warming with the two devices over a period of 2 weeks.
Results
None of the subjects reported glare, discomfort, or pain during the examinations. Moreover, there were no reports of persistent complications as a result of the procedures.
Single-use evaluation
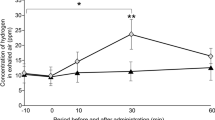
Tear film parameters measured before and immediately after single application of MH (containing menthol) or HO (heat only) devices for 10 min are shown for all the subjects in Table 1. Tear meniscus volume (TMV) was significantly increased after MH application in both healthy subjects and dry eye patients, but it was not increased after HO application in either group. Tear film breakup time (BUT) was also significantly increased only after MH application in both groups. Meibum grade was significantly improved after application of MH or HO in both healthy subjects and dry eye patients. Fluorescein staining score as a measure of ocular surface damage was unaffected by either device in either group of participants. Representative images of the tear meniscus before and after single application of each device are shown in Fig. 1.
Repeated-use evaluation
The Dry Eye–Related Quality-of-Life Score (DEQS) and tear film parameters measured before and at least 8 h after repeated application (10 min twice a day for 2 weeks) of HO or MH are shown for healthy subjects and dry eye patients in Table 2. DEQS was significantly improved after HO or MH application in dry eye patients but not in healthy subjects. TMV and tear film BUT were significantly increased after MH application, but not after HO application, in both groups of participants. Meibum grade was significantly improved after MH application in healthy subjects. Neither device significantly affected fluorescein staining score in either group of participants. Representative images of the tear meniscus before and after repeated application of HO or MH are shown in Fig. 1.
Discussion
We have here shown that single application of a disposable eyelid-warming device containing menthol (MH) increased TMV and prolonged tear film BUT in both dry eye patients and healthy subjects, whereas single application of a similar device without menthol (HO) had no such effects. Furthermore, repeated application of MH, but not that of HO, induced persistent increases in TMV and BUT in dry eye patients as well as normal subjects. Our results thus indicate that single or repeated application of MH improved the condition of the tear film in both the normal and diseased state, suggesting that MH application is a potential novel treatment option for dry eye.
Single application of MH increased TMV and BUT as well as improved meibum condition, whereas HO improved meibum condition alone, in both healthy subjects and dry eye patients. Both menthol and cold temperatures are thought to increase tear secretion as a result of stimulation of TRPM81,2,3,4,5,6. Cooling was thus previously shown to increase tear volume through TRPM8 signaling3, suggesting that warming might be expected to have a negative effect on the production of tear fluid. We have found that the application of eyedrops containing menthol or of chilled saline eyedrops did not increase TMV in healthy subjects (unpublished data). These observations, together with our present finding that only MH increased TMV in healthy subjects and dry eye patients, thus suggest that warming may be necessary for menthol to be able to increase tear fluid volume and that the regulation of TMV by menthol and temperature appears to be complex.
Repeated application of MH induced stable increases in both TMV and BUT in both normal subjects and dry eye patients. Given that tear film parameters were evaluated at least 8 h after the final application of MH, our results suggest that repeated MH use might give rise to a persistent stimulation of tear fluid production by lacrimal glands. The mechanisms of such persistent effects warrant further investigation, especially given that repeated application of menthol might be expected to result in desensitization of the TRPM8 response.
Given that menthol is a ligand of TRPM8, it might be expected to affect the sensory nervous system and thereby influence ocular symptoms. We found that repeated application of MH or HO for 2 weeks improved DEQS in dry eye patients. Although we did not evaluate the effect of repeated application of HO on ocular symptoms in healthy subjects, that of MH did not significantly affect DEQS in healthy subjects. Similar to our results, a recent study found that the application of low-dose menthol ointment improved the ocular symptom score in dry eye patients7; although the symptom score was worsened in healthy subjects, this effect was small and not significant. In the present study, the application of MH did not directly expose the ocular surface to menthol and thus might be considered equivalent to low-dose ointment application. Our results thus suggest that repeated application of MH ameliorated dry eye symptoms.
We would like to emphasize that repeated use of MH over a period of 2 weeks improved TMV and BUT in dry eye patients without the need for administration of any eyedrops or medication. These results indicate that MH application is a potential alternative to eyedrops as a treatment for dry eye patients. Long-term treatment with eyedrops can result in the development of corneal epithelial disorders (toxic keratopathy) and otherwise adversely affect quality of life. Furthermore, dry eye patients with additional ocular diseases such as glaucoma may need to administer multiple types of eyedrops, with the application of those for relief of dry eye symptoms possibly leading to dilution of the drugs contained in the others. Repeated application of MH is thus a candidate novel treatment for individuals with dry eye—including both ADDE and EDE—that would avoid the adverse effects of eyedrop administration. The efficacy of MH for treatment of dry eye thus warrants further evaluation in a multicenter study with a larger number of patients.
Methods
Subjects
This study was approved by the Institutional Review Board of Itoh Clinic, and it adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all subjects before examination. Twenty eyes of 20 healthy subjects (10 men and 10 women; mean age ± SD, 34.9 ± 6.8 years) and 36 eyes of 36 patients with dry eye (16 men and 20 women; mean age ± SD, 30.4 ± 5.7 years) who attended Itoh Clinic between March and December 2015 were enrolled in the study (Table 3). Dry eye was diagnosed on the basis of criteria proposed by the Dry Eye Research Group in Japan28: (1) the presence of dry eye symptoms, (2) abnormal tear production as determined by Schirmer’s test (≤5 mm after 5 min) or abnormal tear film stability as determined by measurement of tear film BUT (≤5 s), and (3) the presence of conjunctival and corneal epithelial damage as evidenced by a fluorescein staining score of ≥3. The fulfillment of at least two of these three criteria was necessary for a diagnosis of dry eye29. Exclusion criteria for all participants included ocular allergies and a history of eye surgery. The healthy subjects had no ocular conditions other than cataract or refractive error. Data were obtained from the left eye of each subject unless this eye did not meet the enrollment criteria, in which case data were obtained from the right eye. One of the 36 patients with dry eye did not undergo single or repeat device application, with the result that the number of such subjects (eyes) was 35 for each protocol.
Protocols
The effects of two types of disposable eyelid-warming steamer (DELW)18 that either contained menthol (MH) (Hogushite-Shaki; Kao, Tokyo, Japan) or did not (HO) (Jo-ki de Hot Eye Mask, Kao) were first evaluated after a single application for 10 min. The two devices were tested on different days with an interval of at least 7 days between each test. The effects of repeated application of MH or HO were then determined after their use for 10 min twice a day for 2 weeks. DELW is an eye mask–shaped device that contains iron powder and water and which provides moist heat through the chemical reaction of iron, water, and atmospheric oxygen when its package is opened. Menthol is volatilized from MH with heat and steam, with the amount of volatilized menthol being ~0.02 mg over 10 min.
Examinations
For the single-use evaluation, examinations were performed sequentially both before (at least 1 day) and immediately after each device application as follows: (1) DEQS30 was determined for assessment of ocular symptoms. (2) TMV was measured over 5 s by strip meniscometry (Echo Electricity, Tokyo, Japan)31. (3) Tear film BUT was measured three times consecutively after the instillation of 1 μl of 1% fluorescein with a micropipette, and the mean value was calculated. (4) Corneal and conjunctival epithelial damage was scored from 0 to 9 on the basis of fluorescein staining29. (5) The morphology of meibomian glands in the upper and lower eyelids was scored (meiboscore) with the use of a noninvasive meibography system (SL-D701 DC4 BG-5; Topcon, Tokyo, Japan)32. (6) Digital pressure was applied to the upper tarsus, and the degree of ease with which meibomian secretion was induced was evaluated semiquantitatively33. (7) A Schirmer strip (Whatman no. 41; Showa, Tokyo, Japan) was inserted over the lower lid margin (midway between the middle and outer thirds) for 5 min without topical anesthesia, with subjects being asked to close their eyes during the measurement. Room temperature (25.3° ± 1.2 °C) and humidity (41.2 ± 6.3%) were maintained relatively constant for all examinations. For the repeated-use evaluation, all of the examinations described above were performed both before (at least 1 day) the initial device application as well as during the daytime at least 8 h (but <16 h) after the final application (in order to avoid immediate effects of warming).
Statistical analysis
Data are presented as means ± s.d. Changes in TMV and BUT between before and after device application were analyzed with Student’s paired t test, whereas those in meibum grade and fluorescein staining score were assessed with Wilcoxon’s signed rank test. A P value of <0.05 was considered statistically significant.
Additional Information
How to cite this article: Arita, R. et al. Effects of a warm compress containing menthol on the tear film in healthy subjects and dry eye patients. Sci. Rep. 7, 45848; doi: 10.1038/srep45848 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Kurose, M. & Meng, I. D. Dry eye modifies the thermal and menthol responses in rat corneal primary afferent cool cells. Journal of neurophysiology 110, 495–504, doi: 10.1152/jn.00222.2013 (2013).
Hirata, H. & Meng, I. D. Cold-sensitive corneal afferents respond to a variety of ocular stimuli central to tear production: implications for dry eye disease. Investigative ophthalmology & visual science 51, 3969–3976, doi: 10.1167/iovs.09-4744 (2010).
Parra, A. et al. Ocular surface wetness is regulated by TRPM8-dependent cold thermoreceptors of the cornea. Nature medicine 16, 1396–1399, doi: 10.1038/nm.2264 (2010).
Robbins, A., Kurose, M., Winterson, B. J. & Meng, I. D. Menthol activation of corneal cool cells induces TRPM8-mediated lacrimation but not nociceptive responses in rodents. Investigative ophthalmology & visual science 53, 7034–7042, doi: 10.1167/iovs.12-10025 (2012).
Belmonte, C. & Gallar, J. Cold thermoreceptors, unexpected players in tear production and ocular dryness sensations. Investigative ophthalmology & visual science 52, 3888–3892, doi: 10.1167/iovs.09-5119 (2011).
Hirata, H. & Oshinsky, M. L. Ocular dryness excites two classes of corneal afferent neurons implicated in basal tearing in rats: involvement of transient receptor potential channels. Journal of neurophysiology 107, 1199–1209, doi: 10.1152/jn.00657.2011 (2012).
Kovacs, I. et al. Abnormal activity of corneal cold thermoreceptors underlies the unpleasant sensations in dry eye disease. Pain, doi: 10.1097/j.pain.0000000000000455 (2015).
Lemp, M. A. Report of the National Eye Institute/Industry workshop on Clinical Trials in Dry Eyes. The CLAO journal: official publication of the Contact Lens Association of Ophthalmologists, Inc 21, 221–232 (1995).
Schaumberg, D. A., Dana, R., Buring, J. E. & Sullivan, D. A. Prevalence of dry eye disease among US men: estimates from the Physicians’ Health Studies. Archives of ophthalmology 127, 763–768, doi: 10.1001/archophthalmol.2009.103 (2009).
Schaumberg, D. A., Sullivan, D. A., Buring, J. E. & Dana, M. R. Prevalence of dry eye syndrome among US women. American journal of ophthalmology 136, 318–326 (2003).
The Definition and Classification of Dry Eye Disease: Report of the Definition and Classification Subcommittee of the International Dry Eye Workshop (2007). Ocular Surface 5, 75–92 (2007).
Nichols, K. K. et al. The international workshop on meibomian gland dysfunction: executive summary. Investigative ophthalmology & visual science 52, 1922–1929, doi: 10.1167/iovs.10-6997a (2011).
Lemp, M. A., Crews, L. A., Bron, A. J., Foulks, G. N. & Sullivan, B. D. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea 31, 472–478, doi: 10.1097/ICO.0b013e318225415a (2012).
Chao, W. et al. Report of the Inaugural Meeting of the TFOS i2 = initiating innovation Series: Targeting the Unmet Need for Dry Eye Treatment (London, United Kingdom, March 21, 2015). The ocular surface, doi: 10.1016/j.jtos.2015.11.003 (2016).
Geerling, G. et al. The international workshop on meibomian gland dysfunction: report of the subcommittee on management and treatment of meibomian gland dysfunction. Investigative ophthalmology & visual science 52, 2050–2064, doi: 10.1167/iovs.10-6997g (2011).
Goto, E. et al. Treatment of non-inflamed obstructive meibomian gland dysfunction by an infrared warm compression device. The British journal of ophthalmology 86, 1403–1407 (2002).
Mori, A. et al. Efficacy and safety of infrared warming of the eyelids. Cornea 18, 188–193 (1999).
Mori, A. et al. Disposable eyelid-warming device for the treatment of meibomian gland dysfunction. Japanese journal of ophthalmology 47, 578–586 (2003).
Matsumoto, Y. et al. Efficacy of a new warm moist air device on tear functions of patients with simple meibomian gland dysfunction. Cornea 25, 644–650, doi: 10.1097/01.ico.0000208822.70732.25 (2006).
Pult, H., Riede-Pult, B. H. & Purslow, C. A comparison of an eyelid-warming device to traditional compress therapy. Optometry and vision science: official publication of the American Academy of Optometry 89, E1035–1041, doi: 10.1097/OPX.0b013e31825c3479 (2012).
Mitra, M. et al. Tear film lipid layer thickness and ocular comfort after meibomian therapy via latent heat with a novel device in normal subjects. Eye 19, 657–660, doi: 10.1038/sj.eye.6701611 (2005).
Ishida, R. et al. Tear film with “Orgahexa EyeMasks” in patients with meibomian gland dysfunction. Optometry and vision science: official publication of the American Academy of Optometry 85, 684–691, doi: 10.1097/OPX.0b013e318181ae83 (2008).
Purslow, C. Evaluation of the ocular tolerance of a novel eyelid-warming device used for meibomian gland dysfunction. Contact lens & anterior eye: the journal of the British Contact Lens Association 36, 226–231, doi: 10.1016/j.clae.2013.02.009 (2013).
Bilkhu, P. S., Naroo, S. A. & Wolffsohn, J. S. Randomised masked clinical trial of the MGDRx EyeBag for the treatment of meibomian gland dysfunction-related evaporative dry eye. The British journal of ophthalmology 98, 1707–1711, doi: 10.1136/bjophthalmol-2014-305220 (2014).
Bilkhu, P. S., Naroo, S. A. & Wolffsohn, J. S. Effect of a commercially available warm compress on eyelid temperature and tear film in healthy eyes. Optometry and vision science: official publication of the American Academy of Optometry 91, 163–170, doi: 10.1097/OPX.0000000000000134 (2014).
Arita, R., Morishige, N., Shirakawa, R., Sato, Y. & Amano, S. Effects of Eyelid Warming Devices on Tear Film Parameters in Normal Subjects and Patients with Meibomian Gland Dysfunction. The ocular surface 13, 321–330, doi: 10.1016/j.jtos.2015.04.005 (2015).
Lane, S. S. et al. A new system, the LipiFlow, for the treatment of meibomian gland dysfunction. Cornea 31, 396–404, doi: 10.1097/ICO.0b013e318239aaea (2012).
Shimazaki, J. Definition and diagnosis of dry eye. Atarashii Ganka (J Eye) 24, 181–184 (2006).
van Bijsterveld, O. P. Diagnostic tests in the Sicca syndrome. Archives of ophthalmology 82, 10–14 (1969).
Sakane, Y. et al. Development and validation of the Dry Eye-Related Quality-of-Life Score questionnaire. JAMA ophthalmology 131, 1331–1338, doi: 10.1001/jamaophthalmol.2013.4503 (2013).
Dogru, M. et al. Strip meniscometry: a new and simple method of tear meniscus evaluation. Investigative ophthalmology & visual science 47, 1895–1901, doi: 10.1167/iovs.05-0802 (2006).
Arita, R., Itoh, K., Inoue, K. & Amano, S. Noncontact infrared meibography to document age-related changes of the meibomian glands in a normal population. Ophthalmology 115, 911–915, doi: 10.1016/j.ophtha.2007.06.031 (2008).
Shimazaki, J., Sakata, M. & Tsubota, K. Ocular surface changes and discomfort in patients with meibomian gland dysfunction. Archives of ophthalmology 113, 1266–1270 (1995).
Acknowledgements
I.S., N.I., Y.S., M.I., and A.S. are employees of Kao Corporation, which markets the eyelid-warming devices evaluated in this study. K.T. is a consultant for Kao Corporation. This study was supported by an intramural research grant (no. T00893-KDE) of Personal Health Care Products Research Laboratories, Kao Corporation. The sponsor had no role in the design and conduct of the study; in collection, management, analysis, and interpretation of the data; in preparation, review, or approval of the manuscript; and in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
R.A. designed the study, conducted data analysis, and wrote the manuscript. N.M. and K.T. contributed to protocol development and writing the manuscript. I.S., N.I., Y.S., A.S. and M.I. contributed to data collection. K.I. independently performed data analysis. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
R.A. holds patents on the noncontact meibography system used in the study (JP patent registration no. 5281846, U.S. patent publication no. 2011-0273550A1, EP patent publication no. 2189108A1) and has applied together with Kao Corporation for a patent on the use of a warming compress containing menthol in dry eye patients. N.M. and K.I. have no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Arita, R., Morishige, N., Sakamoto, I. et al. Effects of a warm compress containing menthol on the tear film in healthy subjects and dry eye patients. Sci Rep 7, 45848 (2017). https://doi.org/10.1038/srep45848
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep45848
This article is cited by
-
Meibomian Gland Dysfunction Clinical Practice Guidelines
Japanese Journal of Ophthalmology (2023)
-
Effects of warm compress on tear film, blink pattern and Meibomian gland function in dry eyes after corneal refractive surgery
BMC Ophthalmology (2021)
-
TheraPearl Eye Mask and Blephasteam for the treatment of meibomian gland dysfunction: a randomized, comparative clinical trial
Scientific Reports (2021)
-
Periocular skin warming promotes body heat loss and sleep onset: a randomized placebo-controlled study
Scientific Reports (2020)
-
Effect of warming eyelids on tear film stability and quality of life in visual display terminal users: a randomized controlled trial
Scientific Reports (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.