Abstract
PSN-357, an effective glycogen phosphorylase (GP) inhibitor for the treatment for type 2 diabetics, is hampered in its clinical use by the poor selectivity between the GP isoforms in liver and in skeletal muscle. In this study, by the introduction of cholic acid, 9 novel potent and liver-targeted conjugates of PSN-357 were obtained. Among these conjugates, conjugate 6 exhibited slight GP inhibitory activity (IC50 = 31.17 μM), good cellular efficacy (IC50 = 13.39 μM) and suitable stability under various conditions. The distribution and pharmacokinetic studies revealed that conjugate 6 could redistribute from plasma to liver resulting in a considerable higher exposure of PSN-357 metabolizing from 6 in liver (AUCliver/AUCplasma ratio was 18.74) vs that of PSN-357 (AUCliver/AUCplasma ratio was 10.06). In the in vivo animal study of hypoglycemia under the same dose of 50 mg/kg, conjugate 6 exhibited a small but significant hypoglycemic effects in longer-acting manners, that the hypoglycemic effects of 6 is somewhat weaker than PSN-357 from administration up to 6 h, and then became higher than PSN-357 for the rest time of the test. Those results indicate that the liver-targeted glycogen phosphorylase inhibitor may hold utility in the treatment of type 2 diabetes.
Similar content being viewed by others
Introduction
Type 2 diabetes mellitus (T2DM) continue to expand at epidemic rates and new medicines targeting novel mechanisms are urgently needed. Glycogen phosphorylase (GP) is the key enzyme that catalyzes glycogenolysis, leading to the release of glucose from glycogen1. Three isoforms of GP have been identified that located within different metabolically active tissues for different physiological functions2. The muscle isoform provides energy for muscle contraction, the brain isoform provides an emergency supply of glucose during periods of anoxia or severe hypoglycemia, and the liver isoform regulates glucose release from hepatic glycogen stores3. In addition, it has been demonstrated that the inhibition of GP is involved in the promoting of glycogen synthesis in liver. Thus, GP, especially, the isoform in liver has received great recent interest as potential target for T2DM4. Although liver GP inhibition is regarded as an excellent therapeutic target for the treatment of diabetes, one very important factor relating to the relevance and importance of isoform specificity with this new therapeutic remains to be proven. As previously stated, brain, liver and skeletal muscle isoforms demonstrate 80% homology in their structures5, thus finding 100% specific inhibitors of the liver isoforms has proved difficult. Therefore, drug development programmes must consider the potential side effects of such compounds in relevant models. For example, inhibition of skeletal muscle GP when the liver isoform is the primary target could have devastating effects on maintaining muscle function. Since many type 2 diabetics are overweight and advised to increase their level of exercise as part of a treatment regimen, adverse effects on skeletal muscle function during exercise would severely limit the utility of a GP inhibitor6.
Effects of pharmacologic GP inhibition on skeletal muscle function after both acute and prolonged muscle contraction in a perfused rat hindlimb model have been reported. For example, the potent GP inhibitor CP316819, inhibition of GP during prolonged (60 min) muscle contraction resulted in a 35% greater muscle fatigue than the control group7,8. OSI Pharmaceuticals, Inc. have previously patented compound structures relating to pyrroloprridine-2-carboxylic acid amides and in early 2006 launched a Phase II clinical study of their promising GP inhibitor PSN-357 for the treatment of diabetes and obesity, but development was discontinued for its side effects. The study was a combined single and multiple dose escalation program that is designed to determine the safety and tolerability of PSN-357, including appropriate exercise tolerance tests to evaluate the potential to compromise recommended positive life changes9,10.
Since the amino acid sequence homology among the GP isoforms is very high, the development of liver isoform-selective GP inhibitors may be a big challenge. And then, we thought about cholic acid, one of the “primary” bile acids formed from cholesterol in the liver, is tightly constrained within the enterohepatic loop through the action of a series of transporter proteins11. The highly efficient enteric and hepatic uptake mechanism ensures that less than 2% of cholic acid pool is excreted daily, even as it makes 10 or more passes through the intestine, portal vein, liver, and bile duct12. A cholic acid conjugate that retained these properties would be expected to have exceptionally substantial hepatic levels and a high liver-to-plasma ratio13. A series of works revealed that hybrid molecules formed by covalent linkage of a drug to cholic acid are recognized by the bile acid uptake systems in the liver and the ileum14,15,16. All the facts definitely indicate that cholic acid-drug conjugates should be considered as the solution to enhance the efficiency of liver-specific of PSN-357.
According to the previous primary structure-activity relationship of PSN-357, the hydroxyl of piperidine is not an essential group for the GP inhibitory activity that modification of it would not drastically decrease the hypoglycemic potency except for a few derivatives17. However, the molecular size of cholic acid is not so small as compared with PSN-357, it’s not hard to speculate that sterically hindrance might be occurred to interfering the interaction between PSN-357 and GP when cholic acid is introduced to the hydroxyl directly, therefore, appropriate linkages such as amino acid, dipeptide or azo linkages were designed to providing enough space between PSN-357 and cholic acid. 9 novel (PSN-357)-cholic acid conjugates were designed (Fig. 1) and synthesized, and the GP inhibition, hypoglycemic effects, biodistributionand pharmacokinetic studies were performed to evaluate the hypoglycemic activity and liver-targeting efficiency of the compounds. To the best of our knowledge, this is the first time to develop cholic acid-based conjugates as liver-specific derivatives of GP inhibitors.
Results and Discussion
Chemistry
The GP inhibitor PSN-357 was obtained according to the method previously described, with some modifications, as outlined in Fig. 218. Commercially available 2-chloro-4-methyl-5-nitropyridine (10) was reacted with diethyl oxalate using potassium ethoxide as the base to give the corresponding derivative 11. Derivative 11 was reduced with iron in saturated aqueous NH4Cl followed by cyclization to give pyrrolopyridine ester 12. Hydrolyzed of 12 with NaOH afforded the carboxylic acid derivative 13 in excellent yield. On the other hand, for segment coupling, (S)-N-Boc-4-fluorophenylalanine (14) coupled to the 4-hydroxypiperidine in the presence of HATU and DIPEA to give 15 in 98% yield. Deprotection of the N-Boc group from 15 with HCl gave the amine hydrochloride salt 16. Reaction of 16 with the carboxylic acid derivative 13 in the presence of HATU and DIPEA furnished PSN-357 in 69% yield (Fig. 2).
The synthesis of cholate conjugate 1 and 2 are shown in Fig. 3. Reaction of cholic acid (17) with glycine methyl ester provided amide derivative 18 in 63% yield. Hydrolyzed of 18 with LiOH afforded the glycine conjugate 19 in 76% yield. Compound 19 was treated with PSN-357 in the presence of DCC and DMAP to obtain conjugate 1. In the same fashion, conjugate 2 was prepared from cholic acid and sarcosine methyl ester.
The synthesis of conjugates 3–6 was carried out starting from PSN-357 (Fig. 4). Reaction of PSN-357 with various protected amino acids (N-Boc-L-Ala-OH, N-Boc-L-Val-OH, N-Boc-O-TBS-L-Ser-OH, Boc-Asp(OtBu)-OH) produced intermediates 22–25. Cleavage of the protecting groups in intermediates 22–25 afforded hydrochloride salts 26–29. Direct coupling of 26–29 with cholic acid in the presence of HATU and DIPEA gave the expected conjugates 3–6.
Reagents and conditions: (a) Boc-NH-CHR-COOH, DCC, DMAP, CH2Cl2, 0 °C to rt; (b) HCl/EtOAc, 0 °C to rt, 2 steps 40% yield for 26, 2 steps 44% yield for 27, 2 steps 70% yield for 28, 67.2% yield for 29; (c) Cholic acid, HATU, DIPEA, DMF, rt, 30.7% yield for 3, 29.2% yield for 4, 20% yield for 5, 15.8% yield for 6.
As shown in Fig. 5, the preparation of conjugate 7 via a multistep process by modifying the well-known synthesis method reported in the literature19. Coupling of N-Boc-L-Val-OH with L-alanine methyl ester hydrochloride yielded N-protected dipeptide ester 31. Hydrolyzed of 31 with LiOH provided Boc-val-ala-OH 32. The dipeptide derivative 32 was treated with PSN-357 to obtain compound 33 in 52% yield. Subsequent deprotection of compound 33 using TFA gave compound 34, which was reacted with cholic acid through the action of HATU and Et3N to give the conjugate 7.
Conjugate 8 was obtained in a similar manner using dipeptide linkage prepared from the protected lysine ester (Fig. 6). Treatment of N6-Cbz-L-lysine methyl ester 35 with Boc-L-phenylalanine in the presence of EDCI in DMF at room temperature afforded dipeptide ester 36. Hydrolyzed of 36 with NaOH in MeOH/H2O gave dipeptide derivative 37 in 79% yield. Hydrogenolysis of 37 over Pd/C in MeOH furnished 38, followed by protection of the resulting amine with FmocCl produced dipeptide intermediate 39. Conjugation of 39 with PSN-357 in the presence of 1-propanephosphonic acid cyclic anhydride (T3P) gave the compound 40. Removal of the protected group from 40 with TFA furnished intermediate 41, which was directly reacted with cholic acid to give the intermediate 42 in a similar reaction pattern as conjugate 7. Deprotection of the Fmoc group of 42 with piperidine afforded the target conjugate 8.
Reagents and conditions: (a) Boc-L-phenylalanine, EDCI, HOBt, DIPEA, DMF, rt, 73%; (b) NaOH, MeOH/H2O, rt, 79%; (c) H2, Pd/C, CH3OH, rt,; (d) FmocCl, NaHCO3, 1,4-dioxane, 0 °C; (e) PSN-357, T3P, CH2Cl2, rt, 3 steps 19.2% yield for 40; (f) TFA, CH2Cl2, 0 °C; (g) Cholic acid, HATU, Et3N, DMF, rt, 2 steps 48.5% yield for 42; (h) Piperidine, CH3CN, rt, 45%.
The complete synthesis of conjugate 9 containing an aromatic azo-linkage is depicted in Fig. 7. Reduction of o-nitrocinnamic acid 43 under H2 atmosphere with Pd/C in aqueous NaOH gave the amine intermediate 44. It was necessary to perform the reduction under basic condition in order to inhibit cyclization of itself. Intermediate 44 was oxidized using Oxone to give nitroso acid intermediate 45. The condensation between intermediate 45 and tert-butyl 4-aminobenzoate was performed in glacial acetic acid at room temperature to give the compound 46. Treatment of 46 with PSN-357 using the Steglich reaction afforded compound 47. Deprotection of the tert-butyl group from 47 using TFA gave the intermediate carboxylic acid 48 in high yield. On the other hand, coupling of cholic acid with N-Boc-ethylenediamine in the presence of DEPC and Et3N in DMF gave compound 49 in 74% yield. Deprotection of the Boc group was performed with 6 M methanolic HCl to yield the cholic acid derivative 50. Compound 50 was attached to the corresponding carboxylic acid 48 under amide-bond-forming condition in the presence of HATU to give the conjugate 9.
Reagents and conditions: (a) H2, Pd/C, NaOH, rt; (b) Oxone, H2O/CH2Cl2; rt; (c) tert-Butyl 4-aminobenzoate, AcOH, 80 °C, 3 steps 17.4% yield for 46; (d) PSN-357, DCC, DMAP, CH2Cl2, rt, 82.9%; (e) TFA, CH2Cl2, rt, 79.5%; (f) N-Boc-ethylenediamine, DEPC, Et3N, DMF, 0 °C to rt, 74%; (g) HCl/MeOH, 0 °C to rt, 97%; (h) 48, HATU, DIPEA, DMF, rt, 10.4%.
Enzyme Assay and SAR Analysis
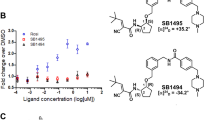
All the compounds were evaluated for their inhibitory activity against rabbit muscle GPa (RMGPa). The activity of RMGPa was measured through detecting the release of phosphate from glucose-1-phosphate in the direction of glycogen synthesis20. CP-91149, a well-known allosteric GP inhibitor, which shares the same binding site with PSN-357, was used as the positive control and the results are summarized in Table 121. The assay results showed that most of the synthesized compounds exhibited moderate to good inhibitory activities against RMGPa. Compared to PSN-357 (IC50 = 0.42 μM), introduction of cholic acid group to PSN-357 resulted in a great loss of activity (1–3, 5–9) or no activity (4). This remarkable loss of activity was probably due to the direct steric interference by such bulky substituent of cholic acid group. Among the compounds, conjugate 1 (IC50 = 5.9 μM) displayed the most efficient inhibition. While the GP inhibition of the intermediates (e.g. 25–28, 33, 40, 42, 48) seemed much acceptable, indicating that introduction of different substitutions in small size on the hydroxyl moiety of PSN-357 resulted in a slight loss of potency. The results is consistent with the SARs of PSN-357 that the hydroxyl of piperidine is not an essential group for the GP inhibitory activity that could be modified slightly9. In general, the L-serine derivative 28 (IC50 = 0.52 μM) was the most active of the series, being approximately 1.25-fold less potent than that of PSN-357.
Cell Assay and SAR Analysis
To evaluate the effects of all compounds in cells, the glycogenolysis assays were established in both rat and human liver cells based on the published method20. These results are summarized in Table 2. Two of the conjugates revealed excellent inhibitory activity in the cellular assays. Of these, conjugate 9 showed the best activity in isolated rat hepatocytes and HepG2 cells, with IC50 value of 12.3 μM and 6.4 μM, respectively. Likewise, conjugate 6 showed IC50 value of 13.4 μM in isolated rat hepatocytes and 6.1 μM in HepG2 cells, respectively. The inhibitory activities of the derivatives of PSN-357 (e.g. 25–28) were also explored. It is not surprising that the derivatives still retained micromolar inhibitory activities. Introduction of steric bulks to the hydroxyl group (e.g. 33, 40, 42, 48) led to a complete loss of activity. Data analysis indicated no clear SAR for the substitutents in the cell-based assays.
In Vitro Stability studies
All the conjugates were tested for their chemical and metabolic stability in multiple assays, including simulated gastric fluid (SGF), simulated interstinal fluid (SIF), mouse plasma, and mouse liver microsome (MLM).
For the stability in SGF (Fig. 8) and SIF (Fig. 9), the conjugates could be divided into three groups: (1) stable conjugates 2, 6 and 9. All of them were stable in SGF for 24 h with almost no detectable PSN-357, but in SIF, conjugate 6, being stable up to 24 h, were much more stable than 2 and 9. Still, 2 and 9 were relatively stable than other conjugates that no more than 20% of the two compounds were degraded during the 24 h incubation in SIF; (2) unstable conjugates 1 and 7. The two conjugates were degraded within 6 h and 1 h in SGF and SIF, respectively, with alomost no conjugates at the end of the 24 h incubation in both SGF and SIF; (3) complicated conjugates 3, 4, 5 and 8. They were relatively stable in SGF over 24 h of incubation, but degraded rapidly in SIF within 1 h.
As shown in Fig. 10, PSN-357 was relatively stable in mouse plasma within the 120-min test, while the conjugates degraded and declined in a mono-exponential model, except conjugates 4 and 6. Conjugates 4 and 6 exhibited considerable stablity in mouse plasma as PSN-357 with approximately 4% and 12% degradation, respectively.
Additionally, the compounds’ stability in microsome were evaluated by measuring the rate of compounds consumpation in MLM and the results are shown in Table 3. PSN-357 demonstrated good metabolic stability in MLM with longer half life (t1/2 > 145 min) and slower elimination rate (CLint < 9.6 μL/min/mg protein, CL < 38.0 μL/min/mg protein). Conjugates 6, 8 and 9 showed considerable metabolic stability with t1/2 over a range of 84.5 to 91.2 min and CLint over a range of 15.2 to 16.4 μL/min/mg protein. Conjugates 1–5, exhibited poor metabolic stability resulting in a short elimination half-life and a high systemic clearance relative to conjugates 6, 8 and 9. In addition, conjugate 7, it metabolized fastest in MLM, with a t1/2 of 4.7 min and displayed very high intrinsic hepatic clearance (CLint of 297.4 μl/min/mg), suggesting the potential for unacceptably high hepatic clearance. Those results indicate that the release of PSN-357 from the conjugates were greatly affecting by the linkers.
Biodistribution and Pharmacokinetic Studies for Compound PSN-357 and Conjugate 6 in Mice
Based on the results of the potency and in vitro stability studies, conjugate 6 was selected for in vivo pharmacokinetic analysis following a single intravenous injection of 5 mg/kg in male C57 BL/6. Doses of PSN-357 intravenous were used as standard regimens for comparison. The results are shown in Table 4 and Fig. 11. In plasma, the concentration of PSN-357 reached the Cmax of 628 ng/mL at 5 min and then sharply decreased during 30 min after dosing, but it gradually increased to reach a secondary peak at 60 min perhaps due to enterohepatic circulation, and the value of AUC0-t is 965 ng/mL.h. For conjugate 6, the concentration reached the Cmax of 726 ng/mL at 5 min and then rapidly decreased to 97 ng/mL at 240 min after dosing. In addition, the concentration of major metabolite PSN-357 released from 6 reached the Cmax of 98 ng/mL at 120 min with the AUC0-t of 691.67 ng/mL.h, about 6 and 1.4-fold lower than that of PSN-357, respectively. On the other hand, in livers, conjugate 6 did not show the highest concentration at 5 min after administration as compared with PSN-357. The concentration of 6 is dramatically increased to reaching a mean Cmax of 3094.55 ng/mL at about 15 min after dosing, suggesting the redistribution from plasma or other tissues to livers may have happened, then 6 was eliminated during 30–240 min. For PSN-357 released from conjugate 6, the value of Cmax is 1023 ng/mL, about 6-fold lower than that of PSN-357, but the value of AUC0-t is 12960 ng/mL.h, about 1.4-fold higher than that of PSN-357 (9711 ng/mL.h), further, (AUCliver/AUCplasma) of PSN-357 metaboliting from 6 is 18.74, about 2-fold higher than that of PSN-357 (10.06). Those results suggested that conjugate 6 exhibited some targeting effect to liver that might enrich and display a longer duration of action in liver in comparison with PSN-357.
In Vivo Efficacy of Compound PSN-357 and Conjugate 6
In vivo efficacy of compound PSN-357 and conjugate 6 were studied on leptin-deficient ob/ob mice. Metformin was chosen as a positive control. Figure 12 showed that treatment with PSN-357 (50 mg/kg) could significantly reduc the blood glucose (BG) to a nadir of 6.36 ± 1.46 mg/dl at 1 h min vs 12.80 ± 1.58 in control ob/ob mice (p < 0.005), with significant effects also being evident at 2 h (p < 0.005) and 3 h (p < 0.005) vs controls. A similar but somewhat weaker hypoglycemic effect was observed for the conjugate 6 under the same dosage. Glucose lowering was statistically significant at 1 (p < 0.01), 2 (p < 0.005), 3 (p < 0.005), 6 (p < 0.005) and 24 h (p < 0.05), with the largest drop (BG level is around 7.79 mmol/L) occurring at 3 h. Especially, there was still significant decrease in BG levels by conjugate 6 up to 6 h after administration. The effect might be due to the fact that 6 acts in a sustained release and longer acting manners. It is noteworthy that the findings are highly consistent with the results from in vivo pharmacokinetic studies.
Conclusions
In summary, though a strategy of bile acid conjugation, it has been found possible to prepare liver-selective conjugates of PSN-357. The in vitro biological and stability studies of these conjugates were evaluated to supporting the selection of a conjugate candidate for in vivo pharmacokinetics and pharmacological evaluation. Among the conjugates, conjugate 6 exhibited moderate enzyme inhibitory activity, suitable cellular activity and acceptable stability in various biological fluids. This compound is preferentially distributed into liver and possesses a longer duration of action than PSN-357 at the same dose. Moreover, conjugate 6 was able to maintain acceptable antidiabetic effects relative to PSN-357. These results implied that the development of liver-selective conjugates might offer a potential opportunity to overcome the muscles side-effects caused by sequence homology of three GP isoforms.
Materials and General Methods
Chemistry section
(The detailed information is in Supplementary information).
Enzyme Kinetics
The inhibitory activity of the test compounds against rabbit muscle glycogen phosphorylase a (GPa) was monitored using microplate reader (BIO-RAD) based on the published method20. In brief, GPa activity was measured in the direction of glycogen synthesis by the release of phosphate from glucose-1-phosphate. Each test compound was dissolved in DMSO and diluted at different concentrations for IC50 determination. The enzyme was added into 100 μL of buffer containing 50 mM Hepes (pH = 7.2), 100 mM KCl, 2.5 mM MgCl2, 0.5 mM glucose-1-phosphate, 1 mg/mL glycogen and the test compound in 96-well microplates (Costar). After the addition of 150 μL of 1 M HCl containing 10 mg/mL ammonium molybdate and 0.38 mg/mL malachite green, reactions were run at 22 °C for 25 min, and then the phosphate absorbance was measured at 655 nm. The IC50 values were estimated by fitting the inhibition data to a dose-dependent curve using a logistic derivative equation.
Glycogenolysis Inhibition in Rat Hepatocytes and HepG2 cells
The inhibition of hepatic glycogenolysis was monitored by the measurement of liver glycogen, which was done quantitatively by the anthrone reagent (Sigma) colorimetric method based on the published method20. Isolated rat hepatocytes or HepG2 cells (Sigma) were treated with the test compound or DMSO solvent (final concentration, 0.10%), followed by 60-min incubation with 0.3 nM glucagon (GGN). Assays were terminated by centrifugation, and cells were digested with 30% KOH followed by glycogen determination. The IC50 values were estimated by fitting the inhibition data to a dose-dependent curve using a logistic derivative equation.
Stability Tests of the Conjugates
Stability in Simulated Gastrointestinal Fluids
The simulated gastrointestinal fluids were prepared according to USP specifications. For SGF, NaCl (0.12 g) and pepsin (0.18 g, from porcine stomach mucosa) was dissolved in HCl (0.42 mL) and sufficient H2O was added to make 60 mL. The pH of the test solution was determined as 1.21 by pH meter. For the SIF, KH2PO4 (0.408 g) and pancreatin (0.6 g, from porcine pancreas) was dissolved in H2O (60 mL). The pH of the test solution was determined as 6.79 by pH meter. Each test compound was dissolved in DMSO and diluted to a final concentration of 2 μM in SIF and SGF. The final concentrations of DMSO and CH3CN in the incubation mixture were 0.2% and 0.45%. Aliquots of these solutions were pipetted into glass tubes, and placed in a 37 °C shaking water bath. Test samples at corresponding time point (1, 2, 6, 24 h) were removed at the end of incubation time and immediately mixed with 800 μL of cold acetonitrile containing 500 ng/mL tolbutamide (internal standard). Samples were subjected to centrifuge at 4000 rpm, 4 °C for 20 min. Aliquots 60 μL of supernatant was combined with 120 μL water for LC-MS/MS analysis.
Stability in Plasma
Frozen plasma from male C57 BL/6 mice was incubated for 5 min at 37 °C before the addition of the test compound. Then prepared 2 μM incubation sample, and aliquots of the incubation mixtures (100 μL) were taken at predetermined time points (10, 30, 60, 120 min) at 37 °C. After incubation, the mixtures was added 400 μL of 50% ACN/50% MeOH containing internal standard (IS, 200 ng/mL Tolbutamide and 20 ng/mL Buspirone) to each sample tube and then centrifuged at 13000 rpm for 8 min. Blank incubations in the absence of the test compound were also performed. The analyses of test compounds were performed by LC-MS/MS analysis.
Stability in Liver Microsomes
The microsomal pellet was suspended in potassium phosphate buffer (100 mM, pH 7.4), 10 μM test compound or positive control (diclofenac) was added. Liver microsomes from C57BL/6 mice (BD Gentest) were pooled. The mixture of microsome solution and compound was incubated at 37 °C for about 10 min in the presence of a NADPH-regenerating system, consisting of 0.02 M DL-isocitric acid (trisodium salt), 0.1 mg/mL isocitrate dehydrogenase and 1 mM NADPH. The addition of ice-cold CH3CN (including 100 ng/mL tolbutamide as internal standard) terminated the reaction. The mixture was vortexed for approx (30 s), centrifuged (20 min, 4000 rpm) and the supernatant was collected and analysed by LC-MS/MS method.
Tissue Distribution and Pharmacokinetic Parameters for Compound PSN-357 and Conjugate 6
The in vivo experiments of compound PSN-357 and conjugate 6 were determined as described below. The animals were housed and cared for in accordance with the guidelines established by the National Science Council of Republic China. All experimental protocols were approved by Animal Care and Use Committee of Chengde Medical University, and all experiments were performed in accordance with the approved guidelines.
Male C57 BL/6 mice (18–20 g, 5–6 weeks old) were provided by the Laboratory Animal Center of Academy of Military Medical Science of People’s Liberation Army, and were reared in standard rodent cages in animal house of Chengde Medical University, under the condition of a constant temperature of 24 °C (±2 °C) and a 12 h light/dark cycle. PSN-357 and conjugate 6 were injected through the caudal vein. For each sampling time point, three mice were treated with a single dose of either PSN-357 or conjugate 6 at 5 mg/kg in 10% DMSO/saline solutions. Blood and liver samples were taken at 0.0833, 0.25, 0.5, 1, 2, 4, 6 and 24 h following intravenous administration, and stored at −80 °C until analysis. Aliquots of all biological matrixes were deproteinized with a mixture of methanol/acetonitrile (1:1). The suspension was vortexed, mixed, and centrifuged at 13000 rpm for 10 min. The organic phase was injected into the LC-MS/MS system. PK calculations and statistical comparisons on PK data were performed according to a non-compartmental kinetic model with validated software (Kinetica™ version 5.1, Thermo Electron Corporation, USA).
Glucose Lowering in Vivo
Five- to six-week old obese, diabetic ob/ob mice (male C57BL/6 J) and their lean, nondiabetic male C57BL/6 J littermates were provided by the Model Animal Research Center of Nanjing University, and housed under standard animal care practices with ad libitum access to food and water throughout the procedures. After 1 week acclimation, blood was collected from the retroorbital sinus for plasma glucose determination, and mice were randomized to groups with similar mean ± SD. Mice were then dosed p.o. daily for 4 days with vehicle consisting of DMSO/PEG400/H-β-CD (1:3:6, v/v/v). On day 5, mice were treated p.o. with PSN-357 (50 mg/kg) or conjugate 6 (50 mg/kg) or vehicle, then bled at 0, 1, 2, 3, 6 and 24 h post-dose for plasma glucose determination. Statistical analysis of the hypoglycemic effect was determined by unpaired t test with the ob/ob mice vehicle treated group.
Additional Information
How to cite this article: Zhang, L. et al. Novel Liver-targeted conjugates of Glycogen Phosphorylase Inhibitor PSN-357 for the Treatment of Diabetes: Design, Synthesis, Pharmacokinetic and Pharmacological Evaluations. Sci. Rep. 7, 42251; doi: 10.1038/srep42251 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Henke, B. R. & Sparks, S. M. Glycogen phosphorylase inhibitors. Mini-Rev. Med. Chem. 6, 845–857 (2006).
Newgard, C. B., Hwang, P. K. & Fletterick, R. J. The family of glycogen phosphorylases: Structure and function. Crit. Rev. Biochem. Mol. Biol. 24, 69–99 (1989).
Rath, V. L. et al. Activation of human liver glycogen phosphorylase by alteration of the secondary structure and packing of the catalytic core. Mol. Cell. 6, 139–148 (2000).
Loughlin, W. A. Recent Advances in the Allosteric Inhibition of Glycogen Phosphorylase. Mini-Rev. Med. Chem. 10, 1139–1155 (2010). (b) Donnier-Marechal, M.; Vidal, S. Glycogen phosphorylase inhibitors: a patent review (2013–2015). Expert. Opin. Ther. Pat. 26, 199–212 (2016).
Baker, D. J., Greenhaff, P. L. & Timmons, J. A. Glycogen phosphorylase inhibition as a therapeutic target: a review of the recent patent literature. Expert. Opin. Ther. Pat. 16, 459–466 (2006).
Casey, A., Short, A. H., Curtis, S. & Greenhaff, P. L. The effect of glycogen availability on power output and the metabolic response to repeated bouts of maximal, isokinetic exercise in man. Eur. J. Appl. Physiol. Occup. Physiol. 72, 249–255 (1996).
Baker, D. J., Timmons, J. A. & Greenhaff, P. L. Glycogen phosphorylase inhibition in type 2 diabetes therapy: a systematic evaluation of metabolic and functional effects in rat skeletal muscle. Diabetes, 54, 2453–2459 (2005).
Baker, D. J., Greenhaff, P. L., MacInnes, A. & Timmons, J. A. The experimental type 2 diabetes therapy glycogen phosphorylase inhibition can impair aerobic muscle function during prolonged contraction. Diabetes, 55, 1855–1861 (2006).
Habash, M. & Taha, M. O. Ligand-based modelling followed by synthetic exploration unveil novel glycogen phosphorylase inhibitory leads. Bioorg. Med. Chem. 19, 4746–4771 (2011).
Sievanen, E. Exploitation of bile acid transport systems in prodrug design. Molecules. 12, 1859–1889 (2007).
Mukhopadhyay, S. & Maitra, U. Chemistry and biology of bile acids. Curr. Sci. 87, 1666–1683 (2004).
Khandare, J. & Minko, T. Polymer-drug conjugates: progress in polymeric prodrugs. Prog. Polym. Sci. 31, 359–397 (2006).
Wu, D., Ji, S., Wu, Y., Ju, Y. & Zhao, Y. Design, synthesis, and antitumor activity of bile acid-polyamine-nucleoside conjugates. Bioorg. Med. Chem. Lett. 17, 2983–2986 (2007).
Geldern, T. W. et al. Liver-selective glucocorticoid antagonists: a novel treatment for type 2 diabetes. J. Med. Chem. 47, 4213–4230 (2004).
Pore, V. S., Aher, N. G., Kumar, M. & Shukla, P. K. Design and synthesis of fluconazole/bile acid conjugate using click reaction. Tetrhedron. 62, 11178–11186 (2006).
Bradley, S. E. et al. Pyrrolopyridine-2-carboxylic acid amide inhibitors of glycogen phosphorylase. PCT patent application : WO2004104001A2 (2004).
Repasi, J. & Szabo, A. Pyrrolopyridine-2-carboxylic acid amide derivative useful as inhibitor of glycogen phosphorylase. US patent application : US8664397 (2014).
Hochdorffer, K., Ajaj, K. A., Schafer-Obodozie, C. & Kratz, F. Development of novel bisphosphonate prodrugs of doxorubicin for targeting bone metastases that are cleaved pH dependently or by cathepsin B: synthesis, cleavage properties, and binding properties to hydroxyapatite as well as bone matrix. J. Med. Chem. 55, 7502–7515 (2012).
Martin, W. H. et al. Discovery of a human liver glycogen phosphorylase inhibitor that lowers blood glucose in vivo . Proc. Natl. Acad. Sci. 95, 1776–1781 (1998).
Wright, S. W. et al. 5-Chloroindoloyl glycine amide inhibitors of glycogen phosphorylase: synthesis, in vitro, in vivo, and X-ray crystallographic characterization. Bioorg. Med. Chem. Lett. 15, 459–465 (2005).
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 81473101 and 81001401), the Natural Science Foundation of Hebei Province (No. H2012406011), the Science Foundation for Excellent Youth Scholars of Education Department of Hebei Province (No. Y2012026), and the Pearl River Nova Program of Guangzhou (No. 2013J2200).
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: L.Z. and C.S. Performed the experiments: L.Z., C.S., G.M., L.Z., Z.Y., J.L. and Y.W. Analyzed the data: G.M., Z.Y. and Y.W. Contributed reagents/materials/analysis tools: L.Z., C.S., G.M., L.Z., Z.Y., J.L. and Y.W. Wrote the manuscript: L.Z.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhang, L., Song, C., Miao, G. et al. Novel Liver-targeted conjugates of Glycogen Phosphorylase Inhibitor PSN-357 for the Treatment of Diabetes: Design, Synthesis, Pharmacokinetic and Pharmacological Evaluations. Sci Rep 7, 42251 (2017). https://doi.org/10.1038/srep42251
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep42251
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.