Abstract
Four VD receptor (VDR) gene polymorphisms (TaqI, ApaI, FokI and BsmI) have been reported to influence Hashimoto’s thyroiditis (HT) risk. However, individual studies have produced inconsistent results. We conducted a comprehensive meta-analysis of eleven case-control studies to better understand roles of the four polymorphisms in HT development. The results showed only FokI polymorphism was significantly associated with the risk of HT (F vs f: OR = 1.44, 95% CI = 1.09–1.91, P = 0.010; FF vs Ff + ff: OR = 1.72, 95% CI = 1.09–2.70, P = 0.019). Subgroup analyses demonstrated the significant effect was only present in Asian population (F vs f: OR = 1.45, 95% CI = 1.07–1.95, P = 0.016; FF vs ff: OR = 1.64, 95% CI = 1.03–2.59, P = 0.036; FF + Ff vs ff: OR = 1.34, 95% CI = 1.00–1.80, P = 0.047; FF vs Ff + ff: OR = 1.64, 95% CI = 1.03–2.64, P = 0.039), but not in Caucasian. For TaqI, ApaI and BsmI polymorphisms, no significant association was found in any model comparison. Based on the current literature, it appears that only VDR FokI polymorphism is associated with HT risk in Asian population, but not in Caucasians; and the TaqI, ApaI and BsmI polymorphisms have not positive association neither in the overall population, nor when stratified by ethnicity. Further well-designed studies with larger sample sizes and different ethnic population are needed to clarify the present findings.
Similar content being viewed by others
Introduction
Hashimoto’s thyroiditis (HT) is an autoimmune thyroid disease (AITD), which has been reported to lead hypothyroidism in up to 5% of population1,2,3. It is characterized by diffuse infiltration of chronic lymphocytic cells and presence of high serum thyroid antibodies concentrations4,5,6. Accumulating evidence has demonstrated that HT may be an autoimmune disease triggered by both genetic and environmental factors7,8,9. Data on twins studies showed the concordance rates for HT were significantly higher among monozygotic twins than dizygotic twins10,11, which suggests that patients with HT have a substantial inherited susceptibility. Moreover, a number of studies have reported certain immunomodulatory genes polymorphisms, such as fork head box P3 (FOXP3), cytotoxic T-lymphocyte-associated protein-4 (CTLA-4) and human leukocyte antigen (HLA) family, were involved in the susceptibility to HT12,13,14,15. Thus, HT seems to be a polygenic disease with a complex mode of inheritance. However, the precise gene factors inciting the condition remain not fully comprehended.
Vitamin D receptor (VDR) is a ligand inducible transcription factor, which is harbored on many human immune cells16,17,18. The active vitamin D, an important immunomodulator, exerts its biological effects through binding to the VDR, and in this way to modulate immune cells activity, triggering innate and adaptive immune responses19,20,21. Certain single nucleotide polymorphisms (SNPs) of the VDR gene may modify vitamin D function. More than sixty SNPs of human VDR gene have been reported22,23. Among them, four common VDR SNPs: TaqI (rs731236, exon 9, +65058 T > C), ApaI (rs7975232, intron 8, +64978 C > A), FokI (rs2228570, exon 2, +30920 C > T) and BsmI (rs1544410, intron 8, + 63980 G > A), were studied intensively for association with various human traits. They were reported to affect the risk of several autoimmune disorders, including rheumatoid arthritis, systemic lupus erythematosus, inflammatory bowel disease, diabetes mellitus and the other AITD (Graves’ diseases, GD)21,24,25,26,27. Recently, several studies have also investigated the association of the four VDR SNPs and HT susceptibility28,29,30,31,32,33,34,35,36,37,38, but their results were inconsistent.
Therefore, it is necessary to carry out a meta-analysis of the available evidence to clarify this inconsistency and provide a much comprehensive and quantitative understanding of the association of VDR gene polymorphisms with HT risk.
Results
Study characteristics
As shown in Fig. 1, the search strategy retrieved 136 articles. After further evaluation, only eleven relevant studies28,29,30,31,32,33,34,35,36,37,38 finally fulfilled the inclusion criteria, including 1338 cases and 1303 controls. All were case-control studies. Nine studies published in English and two in Chinese. There were six studies involving Asians28,29,31,32,34,36, and the other five studies involving Caucasians30,33,35,37,38. The VDR gene was genotyped by polymerase chain reaction–restriction fragment length polymorphism (PCR-RFLP) in all studies, excepting one study used Matrix assisted laser desorption ionization-time of flight mass spectrometer (MALDI-TOF-MS)36. The NOS scores of included studies ranged from 6 to 9 stars, with a median 7 stars. All studies but two28,36 was scored as high quality studies (≥7 stars). Table 1 summaries the characteristics of these studies. The following 4 VDR SNPs were studied: TaqI (rs731236, alleles T/t), ApaI (rs7975232, alleles A/a), FokI (rs2228570, alleles F/f), and BsmI (rs1544410, alleles B/b). Genotypes are designated conventionally by the first letter of the name of restriction enzymes, with a lower case indicating the presence of restriction site, whereas an upper-case letter indicating its absence. Table 2 shows the genotype distribution in the cases and controls, along with the P-value of chi square test for genotype distribution and HWE in control group. HT is often diagnosed mainly on the basis of laboratory and ultrasonographic features, such as positive serum anti-thyroid antibodies, heterogeneous echo-structure with diffuse or patchy hypoechogenicity at ultrasonography, with hypothyroid or euthyroid metabolic state.
Meta-analysis results
Table 3 provides the pooled results regarding the association of the four VDR gene polymorphisms and HT risk under five different genetic models, along with the P-value of Egger’s test for publication bias.
FokI polymorphism
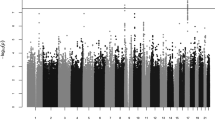
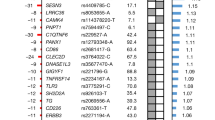
Eight studies including 978 cases and 938 controls examined the association of FokI polymorphism and HT risk. Pooled analyses showed a significant association in the allele model (F vs f: OR = 1.44, 95% CI = 1.09–1.91, P = 0.010) and the dominant model (FF vs Ff + ff: OR = 1.72, 95% CI = 1.09–2.70, P = 0.019), but not in the other models (Table 3, Fig. 2). Significant heterogeneity existed in these two models (I2 = 69.2%, and P = 0.002 for allele model; I2 = 75.7%, and P = 0.000 for dominant model). Then, Galbraith plot analyses were performed to further explore the sources of heterogeneity. As shown in Fig. 3A and C, the studies performed by Guleryuz et al.38 and Meng et al.36 might mainly contribute to the heterogeneity. With exclusion of these studies, the heterogeneity decreased significantly (I2 = 0% and P = 0.760 for F vs f; I2 = 0% and P = 0.738 for FF vs Ff + ff) while the overall association remained significant in these two models (F vs f: OR = 1.72, 95% CI = 1.42–2.07, P = 0.000; FF vs Ff + ff: OR = 2.32, 95% CI = 1.79–3.02, P = 0.000) (Fig. 3B and D). There was one study35 the genotype distributions in controls departed from HWE. Sensitivity analyses by excluding this study did not change the pooled result of allele model (F vs f: OR = 1.37, 95% CI = 1.03–1.82, P = 0.030), but the P value of the dominant model was borderline (FF vs Ff + ff: OR = 1.54, 95% CI = 0.98–2.43, P = 0.060). Subgroup analyses by ethnicity indicated that the FokI F allele or FF genotype significantly increased the risk of HT in Asians (F vs f: OR = 1.45, 95% CI = 1.07–1.95, P = 0.016; FF vs ff: OR = 1.64, 95% CI = 1.03–2.59, P = 0.036; FF + Ff vs ff: OR = 1.34, 95% CI = 1.00–1.80, P = 0.047; FF vs Ff + ff: OR = 1.64, 95% CI = 1.03–2.64, P = 0.039), but the positive association was not found in Caucasians. However, significant heterogeneity were also detected in two models among studies with Asian population (F vs f: I2 = 63.4% and P = 0.027; FF vs Ff + ff: I2 = 65.7% and P = 0.020) (Table 4). Galbraith plot analyses indicated that Meng et al.36 might be the source of heterogeneity. With exclusion of this study, the pooled results remain significant (F vs F: OR = 1.64, 95% CI = 1.31–2.04, P = 0.000; FF vs Ff + ff: OR = 2.07, 95% CI = 1.50–2.86, P = 0.000), with no significant heterogeneity (F vs F: I2 = 0% and P = 0.718; FF vs Ff + ff: I2 = 0% and P = 0.940). Subgroup analyses by study quality suggested that this positive association only existed in pooled analyses of high-quality studies (F vs f: OR = 1.58, 95% CI = 1.10–2.26, P = 0.013; FF vs Ff + ff: OR = 1.92, 95% CI = 1.09–3.40, P = 0.025).
BsmI polymorphism
Six studies including 837 cases and 901 controls evaluated the association of BsmI polymorphism and HT risk. Pooled results indicated that there was no significant correlation between BsmI polymorphism and HT risk in all genetic models (B vs b: OR = 0.95, 95% CI = 0.72–1.26, P = 0.727; BB vs bb: OR = 0.84, 95% CI = 0.46–1.52, P = 0.554; Bb vs bb: OR = 0.99, 95% CI = 0.76–1.29, P = 0.930; BB + Bb vs bb: OR = 0.96, 95% CI = 0.73–1.27, P = 0.764; BB vs Bb + bb: OR = 0.84, 95% CI = 0.49–1.45, P = 0.538) in the overall population (Table 3). Similar results were also observed in the subgroup analyses by ethnicity (Table 4). Moreover, sensitivity analyses showed the results did not change meaningfully by excluding two studies31,34 departed from HWE or one study with low-quality36. There was no significant heterogeneity for all models except the allele model (I2 = 52.1% and P = 0.064). A Galbraith plot analysis suggested that Stefanic et al.30 might be the source of heterogeneity for the allele model. Omitting this study, the pooled result was still not statistically significant (B vs b: OR = 1.06, 95% CI = 0.85–1.31, P = 0.615), with no significant heterogeneity (I2 = 0% and P = 0.621).
ApaI polymorphism
Six studies including 766 cases and 813 controls evaluated the association of ApaI polymorphism and HT risk. The meta-analyses demonstrated no positive relationship of ApaI polymorphism and HT risk in the overall population (A vs a: OR = 0.98, 95% CI = 0.82–1.19, P = 0.869; AA vs aa: OR = 0.90, 95% CI = 0.60–1.36, P = 0.615; Aa vs aa: OR = 1.06, 95% CI = 0.82–1.36, P = 0.670; AA + Aa vs aa: OR = 1.01, 95% CI = 0.78–1.32, P = 0.916; AA vs Aa + aa: OR = 0.92, 95% CI = 0.65–1.29, P = 0.620). No significant heterogeneity was found in all the comparisons (all P > 0.05, Table 3). Similar results were found in the subgroup analyses by ethnicity; ApaI polymorphism was not associated with HT risk in Asian or Caucasian populations (Table 3). Sensitivity analyses, by excluding these two studies33,35 not in HWE or one study with low-quality36, suggested that the results were consistent with those of the primary analyses (all P > 0.05).
TaqI polymorphism
A total of 902 cases and 863 controls from seven studies investigated the relationship between TaqI polymorphism and HT risk. The genotype distribution was consistent with HWE in the controls of all studies (all P > 0.05, Table 2). The pooled results showed that the TaqI polymorphism wasn’t significantly associated with HT risk (T vs t: OR = 1.16, 95% CI = 0.83–1.62, P = 0.372; TT vs tt: OR = 1.55, 95% CI = 0.87–2.76, P = 0.139; Tt vs tt: OR = 1.19, 95% CI = 0.79–1.81, P = 0.386; TT + Tt vs tt: OR = 1.42, 95% CI = 0.98–2.04, P = 0.064; TT vs Tt + tt: OR = 1.23, 95% CI = 0.77–1.96, P = 0.379, Table 3). There was significant heterogeneity for comparison of T vs t and TT vs Tt + tt (I2 = 70.8%, P = 0.002 and I2 = 75.4%, P = 0.000, respectively). In the Galbraith plots, two studies33,35 were outside of the 95%CI from the log OR, causing the heterogeneity in the results. When these two studies were excluded, the heterogeneity decreased significantly, but the pooled results were not changed significantly (T vs t: OR = 1.16, 95% CI = 0.95–1.41, P = 0.147; I2 = 0% and P = 0.635 for heterogeneity; TT vs Tt + tt: OR = 1.16, 95% CI = 0.90–1.50, P = 0.262; I2 = 0% and P = 0.788 for heterogeneity). Subgroup analyses by ethnicity found the similar results in Caucasian or in Asian (all P > 0.05) (Table 4).
Publication bias
No evidence of publication bias was detected by visual inspections of these funnel plots and Egger’s test in all the models regarding the FokI, TaqI and ApaI polymorphism (all PEgger’s > 0.05). However, significant publication bias was detected in two models regarding BsmI polymorphism (PEgger’s = 0.001 for Bb vs bb and PEgger’s = 0.005 for BB + Bb vs bb) (Table 3, Fig. 4A and C). We used the trim and fill method incorporating the hypothetical studies to recalculate the pooled risk estimate. The pooled analyses continued to show no significant association between BsmI polymorphism and HT risk (Bb vs bb: OR = 0.90, 95% CI = 0.71–1.15, P = 0.397; and BB + Bb vs bb: OR = 0.80, 95% CI = 0.59–1.08, P = 0.141). The imputed studies produced symmetrical funnel plots (Fig. 4B and D).
Discussion
To our knowledge, this is the first meta-analysis specially focused on the association of VDR polymorphism with HT risk. A significant association between the BsmI and TaqI polymorphisms and AITD risk has been reported by a previous meta-analysis39. However, in that study, the AITD, including GD and HT, was regarded as an entirety to analyze and only two studies29,30 concentrated on HT alone among all the contained studies. Although GD and HT shared similar immune-mediated mechanisms characterized by the production of thyroid autoantibodies and by thyroid lymphocytic infiltration, a number of studies has indicated that the two diseases might harbor different susceptibility genes5,34,40. Thus, it is necessary to perform a meta-analysis specially focused on HT. Recently, several individual studies33,34,35,36,37 have been conducted to investigate the association between the VDR gene polymorphisms and HT risk, but results from these studies remain conflictive and inconclusive. The reasons for this discrepancy may be small sample size, extensive geographic variations and difference in lifestyle and ethnicities. Therefore, in order to overcome the potential limitations of individual studies, we performed a meta-analysis and found that VDR FokI but not TaqI, ApaI and BsmI polymorphism was significantly associated with the risk of HT. Furthermore, the positive association of FokI polymorphism was only detected in Asians, not in Caucasians by subgroup analyses based on ethnicity.
Polymorphism FokI (rs2228570), located in the translational initiation site of VDR, which is the only known VDR gene polymorphism that results in the generation of an altered protein41,42,43. It can produce two structurally distinct isoforms: a shorter F-VDR or a longer f-VDR protein. The shorter F-VDR protein variant has been reported to be more active than the longer protein variant44,45. Transfection experiments showed the presence of short F-VDR resulted in a higher NF-kB- and NFAT-driven transcription capacity compared to the longer f-VDR. Concordantly, human monocytes and dendritic cells with a homozygous FF VDR genotype show higher expression of IL-12 (mRNA and protein) compared to the cells with an ff VDR genotype46. Therefore, individual with FF genotype may have a more active immune system and an increased risk to immune-mediated diseases. Eight previous studies investigated the distributional difference of FokI polymorphism in patients with HT and controls, and six found a positive association, but another two studies36,38 did not. By pooling these results, our meta-analysis demonstrated that the F allele might be a risk factor for susceptibility of HT (OR = 1.44, P = 0.010) and the incidence of HT was significantly higher in FF genotype individuals than that of Ff + ff genotype individuals in overall population (OR = 1.72, P = 0.019). In addition, results from subgroup analyses stratified by ethnicity indicated that HT risk was increased in Asians with FF genotype (OR = 1.64, P = 0.039), but not in Caucasians. This inconsistent result in these two ethnicities may be due to the influence of different genetic backgrounds, lifestyle and environment factors (such as sunlight exposure and diet). In addition, an insufficient number of samples for analysis might lead to unreliable conclusions with deviation in Caucasians.
BsmI (rs1544410), ApaI (rs7975232), and TaqI (rs731236) SNPs, located near the 3′ end of the VDR gene, are in strong linkage disequilibrium (LD) with each other. These three SNPs don’t change the amino acid sequence of the encoded protein but have been shown to affect gene expression through regulation of mRNA stability47. Three studies30,33,38 indicated TaqI polymorphism was associated with risk of HT in Croatian and Turkish population, but four other studies34,35,36,37 from China, Japan, Italy and Serbia showed no association. ApaI polymorphism was reported no association with HT risk in previous studies with consistent results. Regarding BsmI polymorphism, the study conduct by Stefanic et al.30 demonstrated B variant was apparently associated with decreased risk for HT in comparison to the reference b allele, but five other studies didn’t find this association. In present meta-analysis, pooled results showed no significant association between HT disease and TaqI, ApaI or BsmI polymorphism. Furthermore, subgroup analyses found similar results, and sensitivity analyses did not change the orientation of pooled results.
VDR 3′-RFLP haplotypes have been positioned within the regulatory element spanning-3′- untranslated region which contains polymorphic sequences affecting either VDR mRNA stability or VDR transcriptional activity22,48. Thus, BsmI, ApaI and TaqI, although functionally most likely anonymous, have been associated with total and allele-specific VDR mRNA expression22. Given these three variants strong LD with each other, it is rational to assess the haplotypes effects of VDR polymorphism on HT risk. Meng et al.36 reported three common haplotypes (ab, Ab and AB) of ApaI-BsmI LD block were not associated with Chinese patients with HT (P > 0.05). Giovinazzo et al.37 found the distribution of Bat and baT, the two most common BsmI–ApaI–TaqI haplotypes, was not significantly different in HT patients and controls from Italy. In another study30 conducted in Croatia, the bT and BT of BsmI-TaqI haplotypes were found to be the predisposing and protective haplotypes, respectively. Similarly, common baT as well as the rare BaT haplotypes was associated with increased and decreased risk, respectively. However, we couldn’t do meta-analysis due to insufficient published data in these studies. These effects, including effects associated with rare variants or specific stimuli need further research.
Vitamin D, well-known for its role in calcium and bone metabolism, has important effects on immune regulation by binding to the VDR localized in T lymphocytes and macrophages49,50. A number of studies37,38,51,52,53,54 have found the serum vitamin D level was lower in subjects with HT than that of healthy controls. This inverse association indicated that vitamin D deficiency might be a causal factor leading to HT. Therefore, vitamin D level might be a significant confounder which should be considered when analyzing the association of VDR and HT risk. However, a different point of view has also been postulated, which suggested that the low level of serum vitamin D seen in disease is a secondary phenomenon of VDR dysfunction rather than the reason for autoimmunity55. Although vitamin D level is seen as playing an important role, it is VDR dysfunction that is proposed to be the key factor in the autoimmune diseases process56. Because VDR is key to innate immune response which is important in the pathogenesis of autoimmune diseases57,58, VDR dysregulation greatly compromises the innate immune response. The 25-hydroxyvitamin D3 (25-OHD) level is a reliable parameter reflecting the vitamin D level of the body and usually measured as the level of vitamin D. When VDR dysregulation, the expression of CYP24A1, an enzyme that inactivating 1,25-dihydroxyvitamin D (1,25-OHD) was inhibited. Increased 1,25-OHD will decrease 25-OHD by reducing gene expression and inhibiting expression of CYP27A1 which is an enzyme involved in conversion of vitamin D into 25-OHD55,59. Among our included studies, only two studies concurrently provided the information on vitamin D levels and VDR in patients with HT. One study37 found that the prevalence of vitamin D deficiency in HT patients was significantly higher than that in the control group (70% vs 18.2%; P = 0.0001), but VDR BsmI, ApaI, and TaqI polymorphisms were not associated with HT risk. The other38 indicated that the prevalence of vitamin D insufficiency in HT cases was significantly higher than controls (P = 0.02) while VDR TaqI, but not FokI polymorphisms is associated with HT. It is unfortunate that neither study analyzed the distributional difference of VDR polymorphisms stratified by vitamin D levels. Therefore, the mechanism and effect for the interaction of vitamin D and VDR in patients with HT need further investigations.
Several limitations should be discussed when explaining the results of our meta-analysis. First, lack of adjustments for some factors, such as age, gender, thyroid functional status, circulating vitamin D levels, or dietary vitamin D intake, which may influence the association between VDR variants and risk of HT, might bias the present results. Second, because of unpublished data or limited number of studies, significant publication bias was found in two models regarding BsmI polymorphism, which might have some impact on the final outcome. However, we used trim and fill method to assess the influence of publication bias and found that the results were not significantly changed with or without the addition of hypothetical missing studies. Heterogeneity among studies was also detected in some analyses due to ethnic difference, geographic characteristics and lifestyle. However, our sensitivity analysis showed that studies that contribute to heterogeneity did not significantly alter the conclusions of the overall OR. Third, the statistical power to detect the association may be lower because number of studies included in our meta-analysis is relatively small. However, Ioannidis et al.60 estimated the median sample size required to detect the observed summary effects in each population addressed in 752 studies is 3,535, which is 13.3-fold more subjects than in each original study. These sample size requirements can be inflated considerably if trying to account for potential bias or heterogeneity. These estimates may be difficult to address even by very large biobanks and observational cohorts. Therefore, meta-analysis is an effective way to explore the truth before the emergence of large sample data. Further studies should be focusing on innovative study designs and strong collaborative efforts.
In conclusion, our meta-analysis suggests that the VDR FokI polymorphism is associated with HT risk in overall population or in Asians, but not in Caucasians. The TaqI, ApaI and BsmI polymorphisms are not associated with HT risk. Further well-designed studies with larger sample sizes and different ethnic population are needed to clarify the present findings. Furthermore, the exact causality and mechanism for the interaction of VDR and HT development need further experimental or animal mechanism studies.
Methods
Search strategy
We identified all the studies regarding the relationship of VDR gene polymorphisms and HT by searching PubMed, Embase, China National Knowledge Internet (CNKI), and Wan fang databases without language restrictions (the last search update performed on September 30, 2016). The following key words and search terms were used to identify relative publications: “Vitamin D receptor”, “VDR”, “ApaI”, “BsmI”, “FokI”, “TaqI” and “hashimoto’s thyroiditis”. The reference lists of identified articles and related reviews were reviewed for additional studies.
Inclusion and exclusion criteria
Studies meeting all of the following inclusion criteria were included: (1) case-control study or cohort study; (2) investigating the association between VDR gene polymorphisms (ApaI, BsmI, FokI and TaqI) and HT risk; and (3) providing the frequencies of the variants in cases and controls or providing sufficient data to calculate the estimation of odds ratios (ORs) with 95% confidence interval (95% CI). Exclusion criteria were as follows: (1) overlapping data; (2) studies without genotype frequency and genotype distribution or insufficient information for data extraction; (3) family-based study design; and (4) abstracts, reviews, comments or editorial articles lack of necessary raw data. In the case of overlapping data, only the study with the largest population was selected for this meta-analysis.
Data extraction
Two investigators (XF Wang and WL Cheng) extracted data independently. Any disagreement was resolved through discussion. The extracted data included: name of the first author, year of publication, country, ethnicity, number of cases and controls, genotyping method, control sources, and genotype distribution in cases and controls.
Quality Assessment
The quality of included studies was assessed by two independent reviewers (XF Wang and Y Ma) using the Newcastle-Ottawa Scale (NOS)61. The NOS judged a study based on three perspectives: selection, comparability and exposure/outcome. The full score was 9 stars. Study that scored above six stars was considered as high quality.
Statistical analysis
A random-effects model was used to incorporate within- and between-study heterogeneity as this can provide more conservative result than a fixed effects model62. Pooled ORs and their respective 95% CIs were calculated to evaluate the association between the four VDR SNPs and HT risk under five genetic models: the allele model (eg, A vs a), the homozygous model (eg, AA vs aa), the heterozygous model (eg, Aa vs aa), the recessive model (eg, AA + Aa vs aa), and the dominant model (eg, AA vs Aa + aa). The Hardy-Weinberg equilibrium (HWE) in controls was tested using the goodness-of-fit χ2 statistic with one degree of freedom63. Cochrane’s Q test and I2 test were used to assess heterogeneity among trials. Q-test reported a P value < 0.1 or I2 > 50% was defined as significant heterogeneity64. In case of substantial heterogeneity, a Galbraith plot was created to graphically identify the potential outlier studies that might cause the heterogeneity. Then, a meta-analysis was rerun after excluding the outlier studies65. Subgroup analyses were performed based on ethnicity and quality of included studies to avoid the potential bias influence. Sensitivity analyses were performed by excluding each individual study or the studies with controls inconsistent with HWE to evaluate the impact of individual study on the pooled risk estimate. Publication bias was evaluated by a visual inspection of funnel plot and Egger’s test66. If publication bias was indicated, the “trim and fill” method which conservatively imputes hypothetical negative unpublished studies to mirror the positive studies that cause funnel plot asymmetry was performed to further assess the possible effect of publication bias67. All P-values were two-tailed. All analyses were performed using Stata 11.0 (Stata Corporation, College Station, TX, USA). This article follows the PRISMA statement68 and the Cochrane Collaboration guidelines for reporting meta-analysis.
Additional Information
How to cite this article: Wang, X. et al. Vitamin D receptor gene FokI but not TaqI, ApaI, BsmI polymorphism is associated with Hashimoto’s thyroiditis: a meta-analysis. Sci. Rep. 7, 41540; doi: 10.1038/srep41540 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Hollowell, J. G. et al. Serum TSH, T(4), and thyroid antibodies in the United States population (1988 to 1994): National Health and Nutrition Examination Survey (NHANES III). The Journal of clinical endocrinology and metabolism 87, 489–499, doi: 10.1210/jcem.87.2.8182 (2002).
Vanderpump, M. P. et al. The incidence of thyroid disorders in the community: a twenty-year follow-up of the Whickham Survey. Clinical endocrinology 43, 55–68 (1995).
Lorini, R., Gastaldi, R., Traggiai, C. & Perucchin, P. P. Hashimoto’s Thyroiditis. Pediatr. Endocrinol. Rev. 1 Suppl 2, 205–211, discussion 211 (2003).
Brown, R. S. Autoimmune thyroid disease: unlocking a complex puzzle. Curr. Opin. Pediatr. 21, 523–528, doi: 10.1097/MOP.0b013e32832cf824 (2009).
Lee, H. J., Li, C. W., Hammerstad, S. S., Stefan, M. & Tomer, Y. Immunogenetics of autoimmune thyroid diseases: A comprehensive review. J. Autoimmun. 64, 82–90, doi: 10.1016/j.jaut.2015.07.009 (2015).
Pearce, E. N., Farwell, A. P. & Braverman, L. E. Thyroiditis. N. Engl. J. Med. 348, 2646–2655, doi: 10.1056/NEJMra021194 (2003).
Guarneri, F. & Benvenga, S. Environmental factors and genetic background that interact to cause autoimmune thyroid disease. Curr. Opin. Endocrinol. Diabetes Obes. 14, 398–409, doi: 10.1097/MED.0b013e3282ef1c48 (2007).
Hasham, A. & Tomer, Y. Genetic and epigenetic mechanisms in thyroid autoimmunity. Immunol. Res. 54, 204–213, doi: 10.1007/s12026-012-8302-x (2012).
Roberts, C. G. & Ladenson, P. W. Hypothyroidism. Lancet 363, 793–803, doi: 10.1016/S0140-6736(04)15696-1 (2004).
Brix, T. H., Kyvik, K. O. & Hegedus, L. A population-based study of chronic autoimmune hypothyroidism in Danish twins. The Journal of clinical endocrinology and metabolism 85, 536–539, doi: 10.1210/jcem.85.2.6385 (2000).
Ringold, D. A. et al. Further evidence for a strong genetic influence on the development of autoimmune thyroid disease: the California twin study. Thyroid: official journal of the American Thyroid Association 12, 647–653, doi: 10.1089/105072502760258613 (2002).
Ramesh, B. G. et al. Genomics and phenomics of Hashimoto’s thyroiditis in children and adolescents: a prospective study from Southern India. Annals of translational medicine 3, 280, doi: 10.3978/j.issn.2305-5839.2015.10.46 (2015).
Tomer, Y. Genetic susceptibility to autoimmune thyroid disease: past, present, and future. Thyroid: official journal of the American Thyroid Association 20, 715–725, doi: 10.1089/thy.2010.1644 (2010).
Nithiyananthan, R., Heward, J. M., Allahabadia, A., Franklyn, J. A. & Gough, S. C. Polymorphism of the CTLA-4 gene is associated with autoimmune hypothyroidism in the United Kingdom. Thyroid: official journal of the American Thyroid Association 12, 3–6, doi: 10.1089/105072502753451896 (2002).
Tomer, Y. et al. Common and unique susceptibility loci in Graves and Hashimoto diseases: results of whole-genome screening in a data set of 102 multiplex families. Am. J. Hum. Genet. 73, 736–747, doi: 10.1086/378588 (2003).
Lemire, J. M., Adams, J. S., Sakai, R. & Jordan, S. C. 1 alpha, 25-dihydroxyvitamin D3 suppresses proliferation and immunoglobulin production by normal human peripheral blood mononuclear cells. J. Clin. Invest. 74, 657–661, doi: 10.1172/JCI111465 (1984).
Mahon, B. D., Wittke, A., Weaver, V. & Cantorna, M. T. The targets of vitamin D depend on the differentiation and activation status of CD4 positive T cells. J. Cell. Biochem. 89, 922–932, doi: 10.1002/jcb.10580 (2003).
Provvedini, D. M., Tsoukas, C. D., Deftos, L. J. & Manolagas, S. C. 1, 25-dihydroxyvitamin D3 receptors in human leukocytes. Science 221, 1181–1183 (1983).
Boonstra, A. et al. 1alpha, 25-Dihydroxyvitamin d3 has a direct effect on naive CD4(+) T cells to enhance the development of Th2 cells. J. Immunol. 167, 4974–4980 (2001).
Chen, S. et al. Modulatory effects of 1, 25-dihydroxyvitamin D3 on human B cell differentiation. J. Immunol. 179, 1634–1647 (2007).
Adorini, L. & Penna, G. Control of autoimmune diseases by the vitamin D endocrine system. Nat. Clin. Pract. Rheumatol. 4, 404–412, doi: 10.1038/ncprheum0855 (2008).
Fang, Y. et al. Promoter and 3′-untranslated-region haplotypes in the vitamin d receptor gene predispose to osteoporotic fracture: the rotterdam study. Am. J. Hum. Genet. 77, 807–823, doi: 10.1086/497438 (2005).
Uitterlinden, A. G., Fang, Y., Van Meurs, J. B., Pols, H. A. & Van Leeuwen, J. P. Genetics and biology of vitamin D receptor polymorphisms. Gene 338, 143–156, doi: 10.1016/j.gene.2004.05.014 (2004).
Abd-Allah, S. H., Pasha, H. F., Hagrass, H. A. & Alghobashy, A. A. Vitamin D status and vitamin D receptor gene polymorphisms and susceptibility to type 1 diabetes in Egyptian children. Gene 536, 430–434, doi: 10.1016/j.gene.2013.12.032 (2014).
Prietl, B., Treiber, G., Pieber, T. R. & Amrein, K. Vitamin D and immune function. Nutrients 5, 2502–2521, doi: 10.3390/nu5072502 (2013).
Xia, S. L. et al. Association of vitamin D receptor gene polymorphisms and serum 25-hydroxyvitamin D levels with Crohn’s disease in Chinese patients. J. Gastroenterol. Hepatol. 31, 795–801, doi: 10.1111/jgh.13221 (2016).
Yu, F. et al. Study and Evaluation the Impact of VDR Variants on the Risk of T2DM in Han Chinese. Journal of diabetes, doi: 10.1111/1753-0407.12413 (2016).
Ban, Y., Taniyama, M. & Ban, Y. Vitamin D receptor gene polymorphisms in Hashimoto’s thyroiditis. Thyroid: official journal of the American Thyroid Association 11, 607–608, doi: 10.1089/105072501750302967 (2001).
Lin, W. Y. et al. Vitamin D receptor gene polymorphisms are associated with risk of Hashimoto’s thyroiditis in Chinese patients in Taiwan. J. Clin. Lab. Anal. 20, 109–112, doi: 10.1002/jcla.20110 (2006).
Stefanic, M., Papic, S., Suver, M., Glavas-Obrovac, L. & Karner, I. Association of vitamin D receptor gene 3′-variants with Hashimoto’s thyroiditis in the Croatian population. Int. J. Immunogenet. 35, 125–131, doi: 10.1111/j.1744-313X.2008.00748.x (2008).
Huo, X. J. et al. Association of VitaminD Receptor Gene-BsmI Polymorphism with Autoimmune Thyroid Disease in Innermongolia People of the Han Nationality. J of Radioimmunology 23, 72–74 (2010).
Hong, L. H. Association of vitamin D receptor gene polymorphisms and Hashimoto’s thyroiditis Medical Information 07, 2963–2964 (2011).
Yazici, D. et al. Vitamin D receptor gene ApaI, TaqI, FokI and BsmI polymorphisms in a group of Turkish patients with Hashimoto’s thyroiditis. Minerva Endocrinol. 38, 195–201 (2013).
Inoue, N. et al. The functional polymorphisms of VDR, GC and CYP2R1 are involved in the pathogenesis of autoimmune thyroid diseases. Clin. Exp. Immunol. 178, 262–269, doi: 10.1111/cei.12420 (2014).
Djurovic, J. et al. Association between FokI, ApaI and TaqI RFLP polymorphisms in VDR gene and Hashimoto’s thyroiditis: preliminary data from female patients in Serbia. Int. J. Immunogenet. 42, 190–194, doi: 10.1111/iji.12199 (2015).
Meng, S. et al. Genetic susceptibility to autoimmune thyroid diseases in a Chinese Han population: Role of vitamin D receptor gene polymorphisms. Ann. Endocrinol. (Paris) 76, 684–689, doi: 10.1016/j.ando.2015.01.003 (2015).
Giovinazzo, S. et al. Vitamin D receptor gene polymorphisms/haplotypes and serum 25(OH)D levels in Hashimoto’s thyroiditis. Endocrine, doi: 10.1007/s12020-016-0942-5 (2016).
Guleryuz, B., Akin, F., Ata, M. T., Dalyanoglu, M. M. & Turgut, S. Vitamin-D Receptor (VDR) Gene Polymorphisms (TaqI, FokI) in Turkish Patients with Hashimoto’s Thyroiditis: Relationship to the levels of Vit-D and Cytokines. Endocr. Metab. Immune Disord. Drug Targets (2016).
Feng, M., Li, H., Chen, S. F., Li, W. F. & Zhang, F. B. Polymorphisms in the vitamin D receptor gene and risk of autoimmune thyroid diseases: a meta-analysis. Endocrine 43, 318–326, doi: 10.1007/s12020-012-9812-y (2013).
Inoue, N. et al. Associations between autoimmune thyroid disease prognosis and functional polymorphisms of susceptibility genes, CTLA4, PTPN22, CD40, FCRL3, and ZFAT, previously revealed in genome-wide association studies. J. Clin. Immunol. 32, 1243–1252, doi: 10.1007/s10875-012-9721-0 (2012).
Whitfield, G. K. et al. Functionally relevant polymorphisms in the human nuclear vitamin D receptor gene. Mol. Cell. Endocrinol. 177, 145–159 (2001).
Kanan, R. M., Varanasi, S. S., Francis, R. M., Parker, L. & Datta, H. K. Vitamin D receptor gene start codon polymorphism (FokI) and bone mineral density in healthy male subjects. Clinical endocrinology 53, 93–98 (2000).
Jurutka, P. W. et al. The polymorphic N terminus in human vitamin D receptor isoforms influences transcriptional activity by modulating interaction with transcription factor IIB. Mol. Endocrinol. 14, 401–420, doi: 10.1210/mend.14.3.0435 (2000).
Colin, E. M. et al. Consequences of vitamin D receptor gene polymorphisms for growth inhibition of cultured human peripheral blood mononuclear cells by 1, 25-dihydroxyvitamin D3. Clinical endocrinology 52, 211–216 (2000).
Saijo, T. et al. A unique mutation in the vitamin D receptor gene in three Japanese patients with vitamin D-dependent rickets type II: utility of single-strand conformation polymorphism analysis for heterozygous carrier detection. Am. J. Hum. Genet. 49, 668–673 (1991).
van Etten, E. et al. The vitamin D receptor gene FokI polymorphism: functional impact on the immune system. Eur. J. Immunol. 37, 395–405, doi: 10.1002/eji.200636043 (2007).
Jurutka, P. W. et al. Molecular nature of the vitamin D receptor and its role in regulation of gene expression. Rev. Endocr. Metab. Disord. 2, 203–216 (2001).
Pastinen, T. et al. Mapping common regulatory variants to human haplotypes. Hum. Mol. Genet. 14, 3963–3971, doi: 10.1093/hmg/ddi420 (2005).
DeLuca, H. F. Overview of general physiologic features and functions of vitamin D. Am. J. Clin. Nutr. 80, 1689S–1696S (2004).
Deluca, H. F. & Cantorna, M. T. Vitamin D: its role and uses in immunology. FASEB J. 15, 2579–2585, doi: 10.1096/fj.01-0433rev (2001).
Bozkurt, N. C. et al. The association between severity of vitamin D deficiency and Hashimoto’s thyroiditis. Endocr. Pract. 19, 479–484, doi: 10.4158/EP12376.OR (2013).
Mansournia, N., Mansournia, M. A., Saeedi, S. & Dehghan, J. The association between serum 25OHD levels and hypothyroid Hashimoto’s thyroiditis. Journal of endocrinological investigation 37, 473–476, doi: 10.1007/s40618-014-0064-y (2014).
Mazokopakis, E. E. et al. Is vitamin D related to pathogenesis and treatment of Hashimoto’s thyroiditis? Hell. J. Nucl. Med. 18, 222–227 (2015).
Wang, J. et al. Meta-analysis of the association between vitamin D and autoimmune thyroid disease. Nutrients 7, 2485–2498, doi: 10.3390/nu7042485 (2015).
Proal, A. D., Albert, P. J. & Marshall, T. G. Dysregulation of the vitamin D nuclear receptor may contribute to the higher prevalence of some autoimmune diseases in women. Ann. N. Y. Acad. Sci. 1173, 252–259, doi: 10.1111/j.1749-6632.2009.04672.x (2009).
Waterhouse, J. C., Perez, T. H. & Albert, P. J. Reversing bacteria-induced vitamin D receptor dysfunction is key to autoimmune disease. Ann. N. Y. Acad. Sci. 1173, 757–765, doi: 10.1111/j.1749-6632.2009.04637.x (2009).
Marshall, T. G. Vitamin D discovery outpaces FDA decision making. Bioessays 30, 173–182, doi: 10.1002/bies.20708 (2008).
Wen, L. & Wong, F. S. How can the innate immune system influence autoimmunity in type 1 diabetes and other autoimmune disorders? Crit. Rev. Immunol. 25, 225–250 (2005).
Yoshizawa, T. et al. Mice lacking the vitamin D receptor exhibit impaired bone formation, uterine hypoplasia and growth retardation after weaning. Nature genetics 16, 391–396, doi: 10.1038/ng0897-391 (1997).
Ioannidis, J. P., Trikalinos, T. A. & Khoury, M. J. Implications of small effect sizes of individual genetic variants on the design and interpretation of genetic association studies of complex diseases. American journal of epidemiology 164, 609–614, doi: 10.1093/aje/kwj259 (2006).
Wells, G. A., D O’Connell, B. S., Peterson, J., Welch, V., Losos, M. & Tugwell, P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (2012).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Controlled clinical trials 7, 177–188 (1986).
Emigh, T. H. A comparison of tests for Hardy-Weinberg equilibrium. Biometrics 36, 627–642 (1980).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Statistics in medicine 21, 1539–1558, doi: 10.1002/sim.1186 (2002).
Bax, L. et al. More than numbers: the power of graphs in meta-analysis. American journal of epidemiology 169, 249–255, doi: 10.1093/aje/kwn340 (2009).
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. Bmj 315, 629–634 (1997).
Duval, S. & Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56, 455–463 (2000).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Bmj 339, b2535, doi: 10.1136/bmj.b2535 (2009).
Acknowledgements
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Author information
Authors and Affiliations
Contributions
X.F. Wang, W.L. Cheng, Y. Ma and J.Q. Zhu were responsible for the conception and design, acquisition of data, analysis and interpretation of data, drafting the initial manuscript and revising it critically for important intellectual content. X.F. Wang wrote the final draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Wang, X., Cheng, W., Ma, Y. et al. Vitamin D receptor gene FokI but not TaqI, ApaI, BsmI polymorphism is associated with Hashimoto’s thyroiditis: a meta-analysis. Sci Rep 7, 41540 (2017). https://doi.org/10.1038/srep41540
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep41540
This article is cited by
-
Role of Preoperative Calcium and Vitamin D Supplementation in Preventing Post-total Thyroidectomy Hypocalcemia: a Systematic Review and Meta-analysis
Indian Journal of Surgery (2023)
-
Vitamin D receptor, vitamin D binding protein and CYP27B1 single nucleotide polymorphisms and susceptibility to viral infections in infants
Scientific Reports (2021)
-
Vitamin D Receptor gene polymorphisms and susceptibility to type 2 diabetes: evidence from a meta-regression and meta-analysis based on 47 studies
Journal of Diabetes & Metabolic Disorders (2021)
-
Three polymorphisms of renin-angiotensin system and preeclampsia risk
Journal of Assisted Reproduction and Genetics (2020)
-
Immunomodulatory effect of vitamin D and its potential role in the prevention and treatment of thyroid autoimmunity: a narrative review
Journal of Endocrinological Investigation (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.