Abstract
Nontuberculous mycobacteria (NTM)-lung disease (LD) is an increasing health problem worldwide. The diagnosis of this disease remains difficult, however the application of placenta growth factor (PlGF) and vascular endothelial growth factor (VEGF) has not yet been studied. We screened patients with Mycobacterium avium complex or M. abscessus isolated from sputum, and enrolled 32 patients with NTM-LD and 93 with NTM pulmonary colonization. The NTM-LD group had a lower body mass index, higher proportion of bronchiectasis, more respiratory symptoms and pulmonary lesions, and higher titers of sputum acid-fast stain than the NTM pulmonary colonization group. The plasma level of PlGF was lower in the NTM-LD group than in the NTM colonization group, whereas the level of VEGF was higher in the NTM-LD group. In multivariable logistic regression analysis excluding NTM cultures, the predictive model for NTM-LD included sputum AFS titer, a nodular-bronchiectasis radiographic pattern, plasma VEGF/PlGF ratio, and chest radiographic score (VEGF/P1GF ratio became not significant as a factor in multivariable generalized linear model). The four-factor predictive index had good positive likelihood ratio and negative likelihood ratio for predicting NTM-LD in the patients with NTM in their sputum.
Similar content being viewed by others
Introduction
The incidence of nontuberculous mycobacteria (NTM)-lung disease (LD) has been reported to be increased even in subjects without human immunodeficiency virus infection1,2,3,4, and it has become a health problem worldwide5,6. The American Thoracic Society (ATS) guidelines5 require multiple criteria to diagnose NTM-LD, including clinical and radiographic findings and microbiology, including two or more sets of sputum positive samples for the same NTM infection within 1 year. This process takes time and is inefficient because cultures are time-consuming7.
In addition, the clinical relevance of NTM growth in a sputum culture is much less than 100%, because NTM exists ubiquitously in the environment. The relevance of Mycobacterium avium complex (MAC) in a sputum culture has been reported to be only 35–42%8,9, and 33% for M. abscessus (MAB)9. Making an early diagnosis and treatment are important because NTM-LD can be fatal in critically ill patients and in those who do not receive appropriate treatment10,11,12. Thus, predictors for the clinical diagnosis of NTM-LD are needed, especially when waiting for confirmatory mycobacterial cultures.
Microbiological findings of smear positivity and NTM species have been reported to be predictors for NTM-LD9, in addition to a radiographic bronchiectasis pattern13. Due to low specificity with a single parameter, combining these factors with biomarkers may be more useful. However, systemic inflammatory molecules in the blood such as interferon-gamma and C-reactive protein have been reported to be poorly associated with making a diagnosis, indicating that host cellular immunity may not be adequately responding to a NTM infection14. Local pulmonary biomarkers may be better predictors. Of these markers, vascular endothelial growth factor (VEGF) is responsible for angiogenesis in granulomatous inflammation and is produced by macrophages to induce an immune recruitment response when mycobacteria enter the airway15,16. Higher levels of VEGF have been reported in patients with pulmonary Mycobacteria infections17,18,19. Placenta growth factor (PlGF) is produced from bronchial epithelial cells and is a biomarker that shares significant sequence homology with VEGF at an amino acid level. It can inhibit proliferation, promote cell death, and it has been reported to potentially represent local inflammation20,21,22. Angiogenesis of granuloma and local responses from macrophages and bronchia epithelial cells play important roles in NTM-LD, however VEGF and PlGF have rarely been investigated. The aim of this prospective study, therefore, was to investigate dynamic changes in PlGF and VEGF between NTM-LD and pulmonary colonization, and analyze the potential diagnostic value of these biomarkers.
Materials and Methods
Patient enrollment
This prospective study was conducted at National Taiwan University Hospital from October 2012 to September 2015. The research ethics committee of National Taiwan University Hospital approved the study, which was conducted in accordance with the approved guidelines. All of he enrolled participants provided written informed consent.
Patients aged ≥20 years who had respiratory sample(s) culture-positive for MAC or MAB in the past 12 months were identified, as these two species are most commonly responsible for NTM-LD1,23,24. Patients were recruited consecutively when they visited our chest or infection clinic and were diagnosed with NTM-LD or NTM pulmonary colonization based on the ATS diagnostic guideline5. Briefly, NTM-LD was diagnosed if all of the following were met: (1) two or more sputum culture-positive specimens for the same NTM species; (2) chest images (radiography or computed tomography [CT]) demonstrating lesions compatible with NTM-LD (i.e., fibro-cavitary lesions or multi-focal bronchiectasis; (3) presence of respiratory symptoms; and (4) no obvious alternative diagnosis at that time.
A patient with a positive sputum culture for MAC or MAB but who did not fulfill all of these criteria was defined as having MAC or MAB pulmonary colonization. We enrolled a control group from July 2015 to June 2016 in the same study hospital with the same number of participants as those with NTM-LD. All of the control group had negative chest radiographic images or were sputum-negative for NTM. Patients were excluded if they had human immuno-deficiency virus infection, had received anti-NTM treatment for more than 1 week, or had acute illnesses which caused systemic inflammatory response syndrome.
PlGF and VEGF measurements
Peripheral blood samples were obtained from all participants using heparinized tubes. Plasma was immediately collected and stored at −20 °C. The samples were examined in random order by a technician blinded to the patient’s clinical status. Plasma PlGF and VEGF were measured using an enzyme immunoassay kit (R&D Systems, MN, USA) according to the manufacturer’s instructions.
Data collection
Clinical data, including age, sex, body mass index (BMI), smoking status, co-morbidities, prior pulmonary tuberculosis (TB), symptoms, laboratory data, and radiographic findings upon enrollment were recorded in a standardized case report form with default selection. Current smokers were defined as those who had smoked >100 cigarettes, with the last time of smoking within 1 month prior to the study25.
Symptoms were reviewed according to the patients’ history. Cough ≥3 weeks was defined as chronic cough. Symptom duration was defined as the period prior to the date of the first confirmed positive culture before enrollment. Co-morbidities and prior TB were recorded from medical records. A chest specialist and a radiologist interpreted the chest images. The extent of lung lesions was scored as in a previous study (details in the Supplement File)26,27, and radiographic patterns of the main pulmonary lesions were categorized as fibro-cavitary, nodular-bronchiectasis, and others. Sputum-positive samples for acid fast bacilli in fluorescent staining were then confirmed by Ziehl Neelsen stain. Acid fast smears (AFS) were interpreted as 0, scanty, 1, 2, 3, and 428. Mycobacterial cultures were performed as previously described10.
Statistical analysis
Inter-group differences were analyzed using the Student’s t test for numerical variables and the chi-square test for categorical variables. Relative risks were analyzed using a generalized linear model with Poisson regression. Multivariable logistic regression was used to identify factors associated with NTM-LD in the patients who were sputum-positive for NTM. In stepwise forward variable selection, all potential predictors were included. Statistical significance was set at a two-sided p value of less than 0.05.
The discriminative power of each significant predictor between those with NTM-LD and colonization was compared using receiver operating characteristic (ROC) curve analysis, and the area under the curve (AUC). Optimal values were calculated using the Youden index. All analyses were performed using SPSS software version 19.0 (SPSS, Chicago, IL).
Results
Thirty-two patients with NTM-LD (19 MAC and 13 MAB) and 93 with NTM pulmonary colonization (68 MAC and 25 MAB) during the study period were enrolled (Fig. 1). All of the patients in the colonization group had ≥2 sputum samples cultured for mycobacterium except for one. Thirty-two participants were also enrolled in the control group. The mean age and number of male patients in each group were similar (NTM-LD group: 63 years, 41% male; NTM colonization group: 67.4 years, 44%; and control group: 59.8 years, 41%) (Table 1). In terms of clinical characteristics, the NTM-LD group had lower BMI, higher rate of bronchiectasis, and more symptoms, especially chronic cough, than those with NTM pulmonary colonization. Other underlying co-morbidities and smoking status were comparable.
Flow chart of screening and enrolling participants with sputum positive for nontuberculous mycobacteria (NTM).
Because enrolling period and parent population of the control group are not the same as participants with NTM in sputum. We did not describe the control group in the flow chart. LD, lung disease.
Regarding radiographic findings, 74% of the participants had chest CT, with more in the NTM-LD group (91% vs. 68%, p = 0.011). In the patients with NTM-LD, typical fibro-cavitary and nodular-bronchiectasis patterns accounted for 31% and 53% of the findings, respectively, compared to 0%and 33% in those with NTM colonization. The extent of pulmonary lesions by radiographic score (maximum score 18) was higher in the NTM-LD group (mean ± standard deviation: 3.5 ± 1.6) than in the colonization group (1.9 ± 2.0).
Respiratory specimens were AFB-positive in 21 (66%) and 13 (14%) of the NTM-LD and NTM colonization groups, respectively (p < 0.001). Among them, 13 with NTM-LD and 3 with NTM pulmonary colonization had high-grade (3+ ~ 4+) AFS positivity, with average AFS titers of 1.8 vs. 0.2 (p < 0.001), and 2.5 vs. 0.2 (p < 0.001) AFS-positive specimens per patient. Mycobacterial cultures for the same NTM in the NTM-LD group were positive in 4.1 sets, compared to 1.3 sets of the NTM colonization group (p < 0.001).
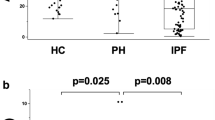
The plasma level of PlGF was higher in the NTM colonization group than in the NTM-LD group (45.0 vs. 13.4 pg/ml, p = 0.019), and the PlGF level in the NTM-LD group was lower than in the control group (13.4 vs. 26.18 pg/ml, p = 0.040) (Fig. 2). However, the plasma level of VEGF was higher in the NTM-LD group than in the NTM pulmonary colonization group (24.1 vs. 14.7 pg/ml, p = 0.035). The ratio of VEGF divided by PlGF was higher in the NTM-LD group than in the colonization group (2.7 vs. 1.6, p = 0.042).
Plasma levels of (A) placenta growth factor (PlGF), (B) vascular endothelial growth factor (VEGF), and (C) their ratio according to nontuberculous mycobacteria (NTM)-lung disease (LD), pulmonary colonization (col), and control group. The cross lines are mean value and error bars are standard error of the mean. ns, not statistically significant.
In terms of clinical presentations, PlGF was correlated with dyspnea (Pearson correlation: 0.249, p = 0.05) and underlying asthma (Pearson correlation: 0.508, p < 0.001). There was no significant difference in PlGF level between those with and without COPD (84 ± 258.1 vs. 40.9 ± 116.7 pg/ml, p = 0.443). VEGF was positively correlated with old age, lower BMI, underlying malignancy, and high number of cultures positive for NTM (Pearson correlation: 0.209, −0.202, 0.188, and 0.211, p = 0.019, 0.024, 0.036 and 0.018, respectively). The AFS-positive grade and radiographic score had borderline significant correlations with VEGF (Pearson correlation: 0.167 and 0.153, p = 0.063 and 0.091, respectively).
The relative risks for the outcome of NTM-LD according to PlGF, VEGF, and the ratio of VEGF/PlGF using the generalized linear model were 0.994 (95% CI: 0.987–0.999, p = 0.049), 1.108 (95% CI: 1.007–1.029, p = 0.001), and 1.136 (95% CI: 1.007–1.280, p = 0.038), respectively. There was a linear relationship between the biomarkers and NTM-LD. We performed multivariable logistic regression analysis for predictors of NTM-LD in the patients who were sputum-positive for NTM. Factors entered into the regression analysis included age, sex, NTM species, and all significant factors in univariable analysis, including BMI, radiographic pattern and score, chronic cough, AFS titer, mycobacterial species, plasma PlGF, plasma VEGF, and VEGF/PlGF ratio. Because more than two sets of positive NTM sputum cultures were required according to the diagnostic criteria, and because that data could not be obtained at baseline, the number of positive NTM cultures was not included in the regression model. In the final model by forward factor selection (Table 2), the AFS titer in the sputum (odds ratio [OR]: 2.007, 95% CI: 1.181–3.411), nodular-bronchiectasis radiographic pattern (OR: 8.580, 95% CI: 2.069–35.575), and plasma VEGF/PlGF ratio (OR: 1.372, 95% CI: 1.068–1.761) were independent predictors of NTM-LD. Radiographic score had borderline significance (OR: 1.272, 95% CI: 0.964–1.680). Multivariable analysis using the generalized linear model with Poisson regression was performed (Table 3), and the relative risks for NTM-LD were 1.636 (1.295–2.068) by sputum AFS titer (per 1 grade increment), 1.189 (1.010–1.399) by radiographic score (per 1 score increment), 1.048 (0.923–1.189) by VEGF/PlGF ratio (per 1 unit increment), and 2.212 (1.049–4.651) by the presence of a nodular-bronchiectasis pattern. The relative risks were smaller than odds ratios for the same factors.
ROC curve analysis for NTM-LD among the patients with NTM in their sputum (Fig. 3) revealed AUC values of 0.764 (95% CI: 0.650–0.875) for AFS titer in the sputum, 0.785 (95% CI: 0.688–0.873) for radiographic score, 0.623 (95% CI: 0.511–0.741) for VEGF/PlGF ratio, and 0.600 (95% CI: 0.481–0.719) for a nodular-bronchiectasis pattern, all of which were lower than that for the number of sputum cultures positive for NTM (AUC = 0.968, 95% CI: 0.941–0.995). Using the probability developed from the multivariable regression model (AUC = 0.899, 95% CI: 0.828–0.969), the predicting AUC value was similar to that by the number of sputum cultures positive for NTM (Fig. 3B). The probability equation is described in the Supplement File.
Receiver operating characteristic (ROC) curves for predicting nontuberculous mycobacteria (NTM)-lung disease in patients with sputum positive for NTM by (A) the four significant factors in the multivariable regression and by (B) the numbers of sputum culture positive for NTM, the probability (ǂ) from the multivariable logistc regression analysis, and the predictive index score (*) by the four factors. The four factors using for the predictive index score were ratio of plasma vascular endothelial growth factor (VEGF)/placenta growth factor (PlGF) >1.8, positive sputum acid fast smear (AFS), radiographic pattern of nodular-bronchiectasis (NB) pattern, and radiographic (chest X film, CXR) score >2. One point was given for each factor and the sum was the predictive index score.
Using the Youden index to identify the optimal cut-off values of continuous independent factors, we defined one point each for sputum AFS titer >0, radiographic score >2, VEGF/PlGF ratio >1.8, or the presence of a nodular-bronchiectasis pattern. The predictive index from this four-factor model was then obtained with a range from 0 to 4. The AUC for NTM-LD with this four-factor model (Fig. 3B) was 0.878 (95% CI: 0.809–0.947), which was similar to that with the probability from the regression model. If the VEGF/PlGF ratio was excluded, the AUC decreased to 0.857 (95% CI: 0.785–0.929) with the remaining three factors and was inferior to the AUC with the number of sputum-positive cultures for NTM.
We then compared the performance of different combinations of the predictors (Table 4). The predictive index with a four-factor model score >2 had 50% sensitivity, 94% specificity, 8.3 positive likelihood ratio (LR), and 0.53 negative LR, compared to 94% sensitivity, 75% specificity, 3.76 positive LR, and 0.08 negative LR for a score >1.
Discussion
In the present study, the plasma level of VEGF was higher in the patients with NTM-LD than in those with NTM pulmonary colonization, while the plasma PlGF level had an opposite trend. A radiographic nodular-bronchiectasis pattern, sputum AFS titer, radiographic score, and VEGF/PlGF ratio were correlated with NTM-LD status when blinded to data from a second set or later of sputum microbiology for NTM. The predictive index using the four-factor model could be used to screen for NTM-LD. In the clinical application of the predictive index, a score >2 favored the diagnosis of NTM-LD, whereas a score <2 excluded NTM-LD.
NTM-LD and colonization are currently differentiated according to the ATS guidelines. Although the clinical significance of NTM pulmonary colonization is not clear and may be a mild form of lung disease, we investigated ATS-defined NTM-LD in the present study for its greater clinical concern. Compared to the patients with NTM pulmonary colonization, those with NTM-LD had higher levels of circulating VEGF, which has been reported to contribute to an alveolar macrophage response to NTM and the formation of granuloma and inflammation15,17. In this study, although VEGF was not correlated with radiographic score, the clinical factors that were correlated with VEGF were also all associated with NTM-LD. These included low BMI, high AFS, and high number of positive cultures for NTM, indicating that the level of VEGF indirectly increased with the severity of NTM-LD.
In contrast, a decreased level of circulating PlGF was noted in the patients with NTM-LD. This may have been due to down-regulation by VEGF22. In addition, PlGF may induce cell apoptosis of type 2 pneumocytes and play a role in the chronic fibrosis phase. Structural lung diseases such as bronchiectasis and COPD, which involve a higher PlGF level, have also frequently been reported in patients with NTM pulmonary colonization20. This may explain the trend of an increase in VEGF/PlGF ratio in the patients with NTM-LD compared to those with NTM colonization. Although the ratio of VEGF/PlGF has not been reported before, this may be useful for discriminating between lung disease of NTM and airway colonization. In particular, the ratio could lead to a bigger difference between NTM-LD and colonization than VEGF or PlGF alone. The ratio was a significant factor in the multivariable logistic regression model and univariable generalized linear model. But it became not significant in multivariable generalized linear model and could be explained by small sample size and the influence from other factors. The real impact of VEGF/PlGF requires further large scale study. For clinical use, the relative risk for NTM-D became smaller and may be more appropriate than the odds ratio which would be over-estimated because the outcome is common29.
The VEGF/PlGF ratio was not a good predictor for NTM-LD by itself, and the predictive model included the clinical factors of sputum AFS titer and radiographic findings. Sputum microbiology is one of the most important factors when diagnosing NTM-LD. The AFS titer has been reported to be higher in patients with NTM-LD than in those with NTM pulmonary colonization14. After rapidly excluding M. tuberculosis in AFS-positive sputum using nucleic acid amplification, the positivity of AFS may be indicative of NTM-LD although AFS titer is not included in the updated NTM-LD guidelines5. Previous studies have reported that different NTM species have different levels of clinical relevance, and that this affects the identification of NTM-LD9,10. However, the NTM species did not affect the prediction of NTM-LD in the present study, which may be because we only recruited patients who were sputum-positive for MAC or MAB species, both of which have a relatively higher clinical relevance than other NTM species8.
With regards to radiographic pattern, fibro-cavitary and nodular-bronchiectasis patterns are typically found in patients with NTM-LD30,31,32. However, the pattern is not always specific and it can be biased by other lung diseases such as fungal or M. tuberculosis infections30,33,34. In the present study, 33% of the NTM colonization group also had a nodular-bronchiectasis pattern. Specific signs such as feeding bronchus or tree-in-buds may be limited due to the facility of CT31,32. Thus, combining microbiologic and radiologic factors and biomarkers such as VEGF/PlGF may be a better index for predicting disease status while NTM is being isolated from set of sputum.
This study has several limitations. First, the patients were enrolled from a single medical center, and they had a high rate of underlying co-morbidities, which may have influenced the levels of the biomarkers. Second, more than half of the patients with NTM isolated from sputum were not recruited due to the absence of follow-up. In addition, the control group was enrolled in a different period. Case selection bias may therefore exist. Third, one case in the NTM pulmonary colonization group only had one sputum sample for mycobacterium culture, and this may have led to classification bias. Fourth, CT imaging was not routinely performed, which may have caused interpretation bias in lung imaging.
In conclusion, the rate of NTM-LD was far lower than 100% in the patients with NTM isolated in their sputum. The diagnosis requires multiple factors and can be delayed by the turn-around time of mycobacterial cultures. Before obtaining more than one set of positive sputum cultures for NTM, our proposed predictive index including ratio of circulating VEGF/PlGF, presence of a nodular-bronchiectasis pattern, positive sputum AFS, and score of radiographic extent may be helpful for favoring or excluding NTM-LD in clinical practice.
Additional Information
How to cite this article: Lin, C.-H. et al. The trend and the disease prediction of vascular endothelial growth factor and placenta growth factor in nontuberculous mycobacterial lung disease. Sci. Rep. 6, 37266; doi: 10.1038/srep37266 (2016).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Lai, C. C. et al. Increasing incidence of nontuberculous mycobacteria, Taiwan, 2000–2008. Emerg Infect Dis 16, 294–296 (2010).
Field, S. K. & Cowie, R. L. Lung disease due to the more common nontuberculous mycobacteria. Chest 129, 1653–1672 (2006).
Adjemian, J., Olivier, K. N., Seitz, A. E., Holland, S. M. & Prevots, D. R. Prevalence of nontuberculous mycobacterial lung disease in US Medicare beneficiaries. Am J Respir Crit Care Med 185, 881–886 (2012).
Prevots, D. R. & Marras, T. K. Epidemiology of human pulmonary infection with nontuberculous mycobacteria: a review. Clin Chest Med 36, 13–34 (2015).
Griffith, D. E. et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med 175, 367–416 (2007).
Menzies, D. & Nahid, P. Update in tuberculosis and nontuberculous mycobacterial disease 2012. Am J Respir Crit Care Med 188, 923–927 (2013).
Lu, D., Heeren, B. & Dunne, W. M. Comparison of the Automated Mycobacteria Growth Indicator Tube System (BACTEC 960/MGIT) with Lowenstein-Jensen medium for recovery of mycobacteria from clinical specimens. Am J Clin Pathol 118, 542–545 (2002).
Koh, W. J. et al. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens in Korea. Chest 129, 341–348 (2006).
van Ingen, J. et al. Clinical relevance of non-tuberculous mycobacteria isolated in the Nijmegen-Arnhem region, The Netherlands. Thorax 64, 502–506 (2009).
Shu, C. C. et al. Nontuberculous mycobacteria pulmonary infection in medical intensive care unit: the incidence, patient characteristics, and clinical significance. Intensive Care Med 34, 2194–2201 (2008).
Ito, Y. et al. Predictors of 5-year mortality in pulmonary Mycobacterium avium-intracellulare complex disease. Int J Tuberc Lung Dis 16, 408–414 (2012).
Kitada, S. et al. Long-term radiographic outcome of nodular bronchiectatic Mycobacterium avium complex pulmonary disease. Int J Tuberc Lung Dis 16, 660–664 (2012).
Lee, M. R. et al. Factors associated with subsequent nontuberculous mycobacterial lung disease in patients with a single sputum isolate on initial examination. Clinical microbiology and infection: the official publication of the European Society of Clinical Microbiology and Infectious Diseases 21, 250 e251–257 (2015).
Shu, C. C. et al. Use of soluble triggering receptor expressed on myeloid cells-1 in non-tuberculous mycobacterial lung disease. Int J Tuberc Lung Dis 15, 1415–1420 (2011).
Barleon, B. et al. Migration of human monocytes in response to vascular endothelial growth factor (VEGF) is mediated via the VEGF receptor flt-1. Blood 87, 3336–3343 (1996).
Berse, B., Brown, L. F., Van de Water, L., Dvorak, H. F. & Senger, D. R. Vascular permeability factor (vascular endothelial growth factor) gene is expressed differentially in normal tissues, macrophages, and tumors. Mol Biol Cell 3, 211–220 (1992).
Datta, M. et al. Anti-vascular endothelial growth factor treatment normalizes tuberculosis granuloma vasculature and improves small molecule delivery. Proceedings of the National Academy of Sciences of the United States of America 112, 1827–1832 (2015).
Alatas, F. et al. Vascular endothelial growth factor levels in active pulmonary tuberculosis. Chest 125, 2156–2159 (2004).
Nishigaki, Y. et al. Increased serum level of vascular endothelial growth factor in Mycobacterium avium complex infection. Respirology 11, 407–413 (2006).
Cheng, S. L., Wang, H. C., Yu, C. J. & Yang, P. C. Increased expression of placenta growth factor in COPD. Thorax 63, 500–506 (2008).
Cheng, S. L., Wang, H. C., Cheng, S. J. & Yu, C. J. Elevated placenta growth factor predicts pneumonia in patients with chronic obstructive pulmonary disease under inhaled corticosteroids therapy. BMC pulmonary medicine 11, 46 (2011).
Tsao, P. N. et al. Overexpression of placenta growth factor contributes to the pathogenesis of pulmonary emphysema. Am J Respir Crit Care Med 169, 505–511 (2004).
Shu, C. C. et al. Clinical characteristics and prognosis of nontuberculous mycobacterial lung disease with different radiographic patterns. Lung 189, 467–474 (2011).
Hoefsloot, W. et al. The geographic diversity of nontuberculous mycobacteria isolated from pulmonary samples: an NTM-NET collaborative study. Eur Respir J 42, 1604–1613 (2013).
Lin, H. H., Ezzati, M., Chang, H. Y. & Murray, M. Association between tobacco smoking and active tuberculosis in Taiwan: prospective cohort study. Am J Respir Crit Care Med 180, 475–480 (2009).
Snider, G. L., Doctor, L., Demas, T. A. & Shaw, A. R. Obstructive airway disease in patients with treated pulmonary tuberculosis. Am Rev Respir Dis 103, 625–640 (1971).
Shu, C. C. et al. Hepatotoxicity due to first-line anti-tuberculosis drugs: a five-year experience in a Taiwan medical centre. Int J Tuberc Lung Dis 17, 934–939 (2013).
Society, A. T. Diagnostic standards and classification of tuberculosis and other mycobacterial diseases. Am Rev Respir Dis 123, 343–358 (1981).
Zhang, J. & Yu, K. F. What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 280, 1690–1691 (1998).
Rozenshtein, A., Hao, F., Starc, M. T. & Pearson, G. D. Radiographic appearance of pulmonary tuberculosis: dogma disproved. AJR Am J Roentgenol 204, 974–978 (2015).
Han, D. et al. Radiographic and CT findings of nontuberculous mycobacterial pulmonary infection caused by Mycobacterium abscessus. AJR Am J Roentgenol 181, 513–517 (2003).
Jeong, Y. J. et al. Nontuberculous mycobacterial pulmonary infection in immunocompetent patients: comparison of thin-section CT and histopathologic findings. Radiology 231, 880–886 (2004).
Cornillet, A. et al. Comparison of epidemiological, clinical, and biological features of invasive aspergillosis in neutropenic and nonneutropenic patients: a 6-year survey. Clin Infect Dis 43, 577–584 (2006).
Hwang, J. H. et al. Pulmonary nocardiosis with multiple cavitary nodules in a HIV-negative immunocompromised patient. Intern Med 43, 852–854 (2004).
Acknowledgements
The authors thank the staff of the Eighth Core Lab of the Department of Medical Research of National Taiwan University Hospital for their technical support. The study was supported in part by grants from the Far Eastern Memorial Hospital National Taiwan University Hospital Joint Research Program (104-FTN22) and the Ministry of Science and Technology Taiwan (MOST 104-2314-B-002-079-MY3 and 103-2314-B-002-152-MY2). The funders had no role in this manuscript.
Author information
Authors and Affiliations
Contributions
Drs. Shu C.C. and Cheng S.L. designed the study. Drs. Lin C.H., Hsu C.L., Shu C.C. and Cheng S.L. performed sample collection, experiment and manuscript writing. Profs. Wang J.Y., Yu C.J. and Lee L.N. were involved in manuscript writing and data analysis.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Lin, CH., Shu, CC., Hsu, CL. et al. The trend and the disease prediction of vascular endothelial growth factor and placenta growth factor in nontuberculous mycobacterial lung disease. Sci Rep 6, 37266 (2016). https://doi.org/10.1038/srep37266
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep37266
This article is cited by
-
Peritonitis due to Mycobacterium abscessus in peritoneal dialysis patients: case presentation and mini-review
Renal Replacement Therapy (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.